Abstract
Background:
India has been at the forefront of designing adolescent health (AH) policies. The National Adolescent Reproductive and Sexual Health policy (2006), the Reproductive, Maternal, Newborn Child, and AH strategy (2013), and the “Rashtriya Kishor Swasthya Karyakram (RKSK)” (2014) have been the critical milestones in this direction. However, despite policies being available, the AH outcomes need improvement through operationalization of focused and need-based AH interventions.
Objectives:
The objectives of this study were to improve services for RKSK interventions across select geographies of India.
Materials and Methods:
USAID's VRIDDHI Project has been providing technical support at the national level and in six focus states to improve uptake of evidence-based high-impact reproductive, maternal, newborn, child, and AH interventions. To improve AH services and outcomes, two approaches were implemented, namely (a) strengthen the functioning of adolescent-friendly health clinics in 95 high caseload health facilities in 26 high priority districts across six states and (b) demonstrate other operational strategies outlined in RKSK program including strengthening of district committees on AH, undertaking formative research for developing adolescent-focused communication strategy, and operationalizing weekly iron and folic acid supplementation program.
Results:
As a result of ongoing technical support over 2-year period (January 2016–December 2017), improvements were noted across multiple AH indicators. In addition, evidence-based learnings were also generated from the demonstration models for potential scale up to other geographies.
Conclusion:
The project was successful in improving AH services in the intervention facilities through an integrated approach which is replicable, sustainable, and scalable for driving the AH program in India.
Keywords: Adolescent friendly health clinics, adolescent health, Rashtriya Kishor Swasthya Karyakram, reproductive maternal newborn child and adolescent health
INTRODUCTION
The “Global Strategy for Women's, Children's and Adolescents' Health” (2015–2030) has recognized adolescence as a critical life stage with its own unique health challenges. The strategy recommends for investments in right policies and programs for adolescents to institutionalize integrated solutions for addressing adolescent health (AH) issues.[1] Subsequently, the “Global Accelerated Action for the Health of Adolescents,” launched in 2017, provides an action framework to assist national governments in deciding what they plan to do, and how they plan to do it – as they respond to the health needs of adolescents in their countries.[2]
India comprises of nearly 243 million adolescents and has led efforts in designing and implementing AH policies and programs.[3] The last decade has seen multiple initiatives for improving AH services with the Ministry of Health and Family Welfare (MoHFW), Government of India (GOI) launching the “Adolescent Reproductive and Sexual Health (ARSH) Policy” in 2006, followed by the “Reproductive Maternal Newborn Child and AH (RMNCH + A) Strategy” in 2013, and the “Rashtriya Kishor Swasthya Karyakram” (RKSK), the national program on AH in 2014. RKSK has imparted momentum to ongoing AH-related interventions and has resulted in a realignment of the traditional approach to address AH with a renewed focus on community-based activities for health promotion and prevention, and strengthening of clinic-based, preventive, diagnostic, and curative services across various levels of care [Figure 1].
Figure 1.
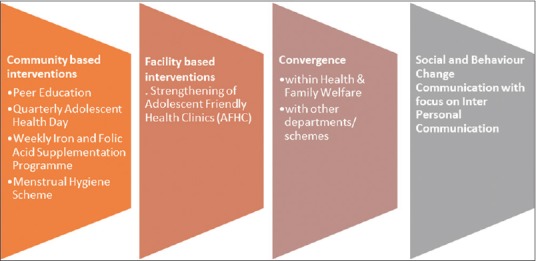
Rashtriya Kishor Swasthya Karyakram interventions
However, despite the policy initiatives undertaken by GOI for improving AH in India, traditional challenges such as early marriages, teenage pregnancy, anemia, and high incidence of maternal mortality among young mothers continue to persist, with upcoming issues such as those of noncommunicable diseases, injuries, and substance abuse further compounding the situation. One of the main underlying factors behind limited success of AH interventions is lack of evidence on functionality of these interventions and level of integration of ongoing programs within the broader RMNCH + A context.
USAID-VRIDDHI (Scaling up RMNCH + A Interventions Project) (hereafter referred to as the “project”) provides technical assistance to the national government and state governments in six focus states (Delhi, Haryana, Himachal Pradesh, Jharkhand, Punjab, and Uttarakhand) for scaling up RMNCH + A interventions. Under this project, four different models based on the operational strategies and approaches of RKSK program for strengthening AH service delivery were conceptualized and piloted. The current paper highlights the process and learnings from these four pilot interventions and discusses their feasibility for scale up and potential for larger impact.
Objectives
To design and pilot RKSK-based intervention models in selected high priority districts (HPDs) of six focus states
Demonstrate and document learnings and efficacy of these models to improve AH service delivery and outcomes.
MATERIALS AND METHODS
Development of models
A consultative process was adopted to identify gaps and critical areas encompassing AH service delivery involving officials from MoHFW, State National Health Missions (NHMs), development partners, and other stakeholders. Published and unpublished literature, reports, and studies were also reviewed to explore and list gaps and challenges. Major gaps included inadequate institutional support system to guide and monitor AH programs and services; deficient or poor-quality services at the government health facility-based “Adolescent Friendly Health Clinics” (AFHC); and lack of adolescent-focused communication material to address their specific needs.
An expert team comprising of senior government officials and the project's technical team reviewed the findings and following a series of discussions figured out four models to address the systemic gaps and positively influence AH services and its delivery. Implemented between October 2015 and December 2017, the following section outlines the implementation frameworks adopted for the interventions.
Implementation frameworks
Model 1: Strengthening of adolescent-friendly health clinics at L2 and L3 health facilities
At the outset, a baseline assessment was conducted in 95 AFHCs located across high caseload L3 and L2 government health facilities in 26 projects HPDs (January–February 2016), with an objective to identify areas that needed strengthening for optimization of service delivery.[4] Based on the findings, an implementation framework was developed through a consultative process to inform decision-making for reorganization of institutional processes at AFHC, training and mentoring of service providers through onsite visits, concurrent monitoring of service delivery quality, and establishing review mechanisms [Figure 2]. After the baseline, the project team engaged in a training, mentorship, and quality improvement framework to improve the functioning of the AFHCs. As an initial step, the trainings were cofacilitated for AFHC counselors through the state annual program implementation plans that potentiated capacity enhancement of the service providers. Subsequently, mentoring visits were made at all AFHCs every month during the intervention period to provide supportive supervision (SS) to the AFHC staff and facilitate required actions related to dedicated space, privacy, signage, clinic branding, availability of commodities, equipment and communication materials, and institutionalization of recording and reporting mechanisms. Specific emphasis was put on developing interpersonal communication skills of the staff providers to ensure a friendly and nonjudgmental attitude toward the adolescents. The mentoring visits were integrated with another intervention at the same L3 and L2 facilities which focused on improving the quality of care during the intrapartum and immediate postpartum periods.[5] Thus, not only was an AH intervention integrated with a maternal and newborn health intervention, the results and achievements of both were entwined with each other. AFHC improvement plans were developed at all intervention facilities to establish review mechanisms, track progress, and enhance ownership and engagement of the concerned staff. Postintervention an end-line assessment was conducted to measure progress made and understand beneficiary perspective (November–December 2017).
Figure 2.
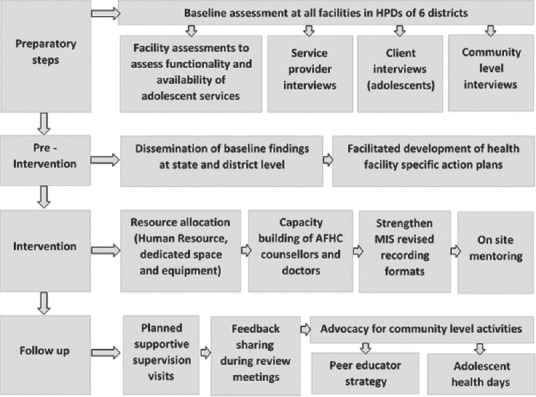
Operational framework for strengthening AFHCs
Model 2: Leveraging “district committees on adolescent health” to enhance coordination and communication between related departments for adolescent health interventions
District committees on adolescent health (DCAH) have been identified as the fulcrum for AH interventions at the district level. Constituted under the chairmanship of the District Magistrate, the DCAH brings together all relevant stakeholders to improve AH outcomes. The district RKSK nodal officer is the designated convener of the DCAH, and the committees are mandated to meet every 3–4 months for discussing the progress and developing action plans.
The functioning and implementation of DCAH have, however, been variable and the project team collaborated with NHM, Government of Jharkhand to strengthen functioning of DCAHs across 7 HPDs. The support framework included formation of state committee on AH (SCAH) to review and monitor functioning of DCAH. State level workshops were organized by NHM to sensitize state/district officials on expected roles and responsibilities of various departments toward achieving AH outcomes. The project cofacilitated quarterly DCAH meetings in the intervention districts, provided technical assistance to the nodal officer by analyzing reports and monitoring data to generate feedback, and institutionalized a structured review mechanism for timely follow-up, improved decision-making and action. Joint supervisory visits were conducted by SCAH members and the project's technical team to monitor AH interventions and regular review meetings including video conferencing were also facilitated to track status and progress.
Model 3: Formative research for developing communication plan on adolescent health
RKSK guidelines focus on social and behavior change communication (SBCC) and improved health-seeking behavior as critical for achieving the targets. The development of such adolescent-focused communication plans need insights into the awareness levels, behavioral practices, and media habits (use of mobile phones and social media) among the target group. To understand these aspects and other related factors, the project collaborated with NHM, Government of Haryana, to undertake a cross-sectional study among school-going adolescent boys and girls in 6 HPDs of the state. According to an earlier study, the prevalence of tobacco use among school-going students is 3.7%; based on this indicator, a sample size of 3600 was calculated for the current study (precision of ± 0.02).[6] Subsequently, in the study districts, lists of government intermediate schools, that is, those up to 12th standard, were collected from the education department and schools were sampled using “Probability Proportionate to Size” technique based on the number of students enrolled. For ensuring appropriate rural–urban representations, 70% schools were selected from rural and remaining 30% from the urban areas. Study participants were identified through gender-stratified multistage cluster sampling technique, and five boys and five girls were randomly selected from each class between 7th and 12th standard in the selected schools. Thus, 60 participants were included in the study from 60 schools (42 rural and 18 urban). The participants were oriented on the study objectives and post informed consent they filled out a self-administered questionnaire adapted from the WHO Global School Student Health Survey 2013 module.[7] Conducted between October 2015 and February 2016, the study was collated and analyzed using Microsoft Excel software. The findings were documented and shared with NHM to guide the development of an AH communication plan.
Model 4: Strengthening the weekly iron and folic acid supplementation program
The weekly iron and folic acid supplementation (WIFS) program is an important intervention aimed at addressing adolescent anemia. In spite of existing guidelines, the rollout and subsequent implementation of the program has been patchy and fractured. Identifying the need to demonstrate an implementation model, the project undertook a baseline assessment of the WIFS program in the state of Punjab and subsequently developed an operational framework to facilitate implementation. The framework adopted a system-based approach and included developing standard operating procedures for the intervention, capacity enhancement of service providers, streamlining of the supply chain processes, developing and initiating usage of standard recording and reporting formats, strengthening review mechanisms through SS, appropriate screening and referral of anemic adolescents, developing Nutrition and Health Education Day (NHED) calendars to generate demand, and ensuring compliance and interdepartmental coordination. The operational framework was discussed and approved by the state NHM authorities and was piloted in the district of Barnala before statewide scale up.
It was, thus, envisaged that through a combination of approaches the technical assistance resourced through the project would help improve the processes and outcomes of the interventions, thereby adding to the existing knowledge base on implementing RKSK interventions through an integrated approach.
RESULTS
Model 1
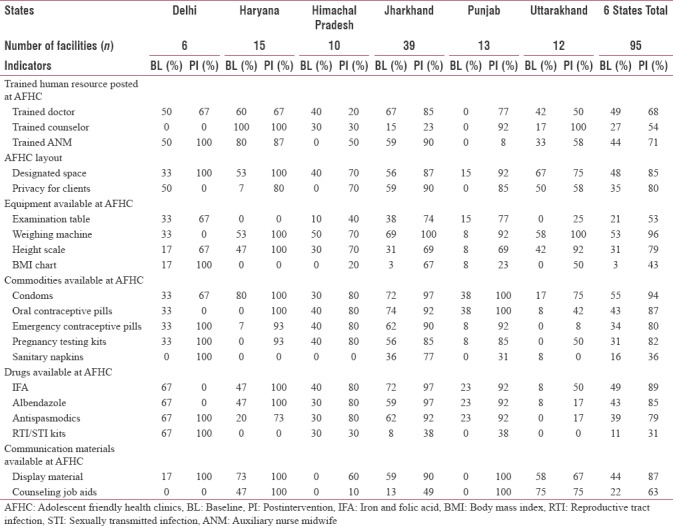
The baseline assessment showed that AFHCs were functioning at 79 out of 95 selected facilities (83%). Reasons for suboptimal performance included issues such as inadequate staffing, untrained service providers, inadequate equipment, frequent stock out of drugs, low priority accorded by program managers, and service delivery restricted to ARSH without availability of curative services.
Postintervention, all 95 centers were fully functional with variability in certain service delivery indicators owing to infrastructure and other health system-related issues in the 6 states [Table 1]. End-line assessment showed improved availability of both counseling (from 63% to 97%) and clinical services (54%–95%). About 43% of centers were found to have reference material for the service providers (manuals, standard-operating-procedures, and frequently asked questions); and 56% centers had taken-away material for clients (leaflets and handouts). Overall satisfaction rates among adolescent clients were found to be 96% (n = 191) during the exit interviews. Almost all clients interviewed mentioned about availability of free services and friendly and nonjudgmental behavior of doctors and counselors at these centers. About 90% of clients stated that privacy was provided during consultation and 1.63 lakh adolescent clients availed services at intervention AFHCs over the 2-year intervention period.
Table 1.
State wise and total availability of workforce, equipment, and communication material at adolescent-friendly health clinics s (baseline and postintervention)
Model 2
Postintervention interviews with senior officials from NHM revealed that revival and strengthening of DCAH in the intervention districts resulted in better coordination with other line departments. This has further resulted into timely procurement and distribution of supplies (Iron and Folic Acid [IFA] tablets and sanitary napkins), increased registration of adolescent clients to avail health services, and effective implementation of information education and communication (IEC) activities to address issues such as teenage marriage and adolescent fertility.
Model 3
The cross-sectional study conducted among adolescent school-going boys and girls revealed critical behavior-related findings. While 16% of boys and 6% of girls from 10th to 12th class reported having sexual intercourse, 54% of boys and 4% girls reported to have used condom during the last sexual intercourse. Higher percentage of early adolescent girls (Classes 7–9) reported smoking and having drugs ever while close to 12% boys in late adolescence (Classes 10–12) reported smoking and 3% reported taking drugs, ever. About 12% early adolescent and 16% late adolescent boys reported consuming liquor at least once. The formative research facilitated the development of a SBCC plan spread over from 2016–17 to 2018–19 to address critical AH issues in Haryana. Based on the SBCC plan, key behaviors were identified, focused IEC material was developed, and roll out of the same was undertaken through the AFHCs.
Model 4
Overall, baseline assessment of the WIFS program showed irrational procurement and distribution of logistics as a major gap adversely affecting program performance and coverage. During visits, IFA tablets were found to be available at majority of the schools, but out-of-stock at all 666 Anganwadi Centers in Barnala district. The availability of other related logistics and lack of uniform recording-reporting formats were also revealed as issues. The model adopted a “One Stop Shop” approach wherein bundling of drugs and other logistics (recording and reporting formats) was done and distributed to all the involved departments on the same day at the same platform. In addition, the process of maintaining buffer stock at the block education office and cluster schools, on-site mentoring, and periodic reviews ensured smooth and effective implementation of the program. This model resulted in significant improvements in the program performance in Barnala. Postintervention results showed an increase in consumption of IFA tablets from 42% to 78%. IFA tablets and reporting formats were available at all schools from the baseline statistic of 69% and 0%, respectively. Almost 87% of schools were found to have started organizing health education sessions from a baseline of 0%. Encouraged from the success of this model, an amount of 44 lakhs was approved in the State Program Implementation Plan for year 2017–2018 toward for strengthening WIFS program in all 22 districts of the state.
DISCUSSION
Addressing issues underlying AH is complex because of nonhomogeneity of the target group. Moreover, in India, programs for promoting health and welfare of adolescents are implemented by different ministries/departments which often translates to suboptimal results due to operational challenges. Although RKSK has shown the way forward and looks at developing a comprehensive service delivery package for adolescents, mainstreaming of AH interventions with other RMNCH + A thematic areas is the need of the hour.
The models and their implementation frameworks outlined in this article have focused on a holistic approach. These models emphasize on the importance of integration of service delivery for adolescents along with other RMNCH services in a facility-based setting; using schools as a platform to reach and deliver AH services; strengthen coordination and collaboration with concerned departments; and targeting behavior change through a specially designed communication package based on the needs of target group.
According to a GOI report, 7250 AFHC was established in India, by 2016. Various evaluations conducted from time to time have documented their uneven distribution, suboptimal quality of services provided at these clinics, and limited utilization by adolescents.[8,9,10,11] An evaluation of AFHCs in Bangladesh also showed very limited public awareness about AFHCs, more so among the target group.[12] The model tested for strengthening selected high caseload AFHCs emerged as a successful approach and results have shown that a model with a comprehensive strategy, ensuring facility readiness, capacity building of service providers, mentoring support, and periodic review of progress can contribute toward improvements in the AH service delivery.
Programs targeting AH are constrained by the absence of interventional research to inform and guide interventions.[13] Although effect of SBCC on increasing awareness among adolescents is known, there is gap in the documentation on effect of SBCC at the community level to increase awareness among adolescents.[14,15] The formative research conducted as an approach for strengthening AH service delivery successfully generated evidence for guiding the development of a communication plan for AH. Similarly, the success of the model based on strengthening DCAH showed that ensuring an administrative will and adopting a governance and policy framework are essential for strengthening AH service delivery mechanisms.
Earlier studies have shown that WIFS combined with monthly education sessions and deworming every 6 months has been cost-effective in reducing anemia prevalence among adolescent girls.[16] In addition, studies have shown that in 70.1% of cases teachers played a motivating role for consuming IFA tablets.[17] However, literature also points toward poor implementation of the WIFS program.[18] The approach adopted to strengthen the WIFS program successfully addressed the issues identified during the baseline assessment and from earlier studies. Involvement of teaching staff to mobilize beneficiaries and deliver services was a critical input and significantly contributed to improved service delivery.
CONCLUSION
Optimizing AH service delivery will require a multidimensional approach with equal emphasis on reproductive and sexual health, SBCC, healthy lifestyle, and social environment. It is imperative that implementation of the various programs is integrated and coordinated to realize their full potential. The models tested out have demonstrated improvement in outcomes, but sustainability and scale can only be achieved if the health system demonstrates readiness and motivation to prioritize AH interventions. Recent efforts have demonstrated a willingness from MoHFW and the respective state governments to move forward on this important agenda and harmonizing and mainstreaming operational and implementation frameworks are the way forward.[19]
Financial support and sponsorship
This work was made possible by the support of the American people through the United States Agency for International Development and its VRIDDHI (scaling up RMNCH + A Interventions) Project, implemented by IPE Global Ltd. under the terms of Cooperative Agreement Number AID-386-A-14-00001. The contents of this paper represent the views of the authors and do not necessarily reflect the views of USAID.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The Vriddhi team would like to acknowledge the support of MoHFW, GOI, the State Governments of Delhi, Haryana, Himachal Pradesh, Jharkhand, Punjab, and Uttarakhand, for supporting the intervention.
REFERENCES
- 1.Global Strategy for Women's, Children's, and Adolescents' Health 2016–2030. New York: Every Woman Every Child; 2015. [Last accessed on 2018 Feb 06]. Every Woman Every Child. Available from: http://www.who.int/life-course/partners/global-strategy/globalstrategyreport2016-2030-lowres.pdf?ua=1 . [Google Scholar]
- 2.Guidance to Country Support Implementation. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2017. [Last accessed on 2018 Feb 06]. Global Accelerated Action for the Health of Adolescents (AA-HA!) Available from: http://www.apps.who.int/iris/bitstream/10665/255415/1/9789241512343-eng.pdf . [Google Scholar]
- 3.Maliye C, Garg BS. Adolescent health and adolescent health programs in India. [Last accessed on 2018 Feb 05];Mahatma Gandhi Inst Med Sci. 2017 22:78–82. Available from: http://www.jmgims.co.in/text.asp?2017/22/2/78/214748 . [Google Scholar]
- 4. [Last accessed on 2018 Mar 03]. Available from: http://www.rmncha.in/wp-content/uploads/publications_img/1488774356.pdf .
- 5. [Last accessed on 2018 Mar 03]. Available from: http://www.rmncha.in/
- 6.CBSE. India (CBSE) Global School-Based Student Health Survey. New Delhi: CBSE; 2007. [Last accessed on 2018 May 23]. Available from: http://www.who.int/chp/gshs/2007_India_CBSE_fact_sheet.pdf?ua=1 . [Google Scholar]
- 7.CDC. Global School Based Student Health Survey. 2013. [Last accessed on 2018 May 23]. Available from: http://www.who.int/chp/gshs/GSHS_Core_Modules_2013_English.pdf .
- 8.Assessment of Adolescent Reproductive and Sexual Health (ARSH) Centres in Gujarat. Vadodara: CORT; 2009. Centre for Operations Research and Training (CORT) [Google Scholar]
- 9.Evaluation study on Adolescent Friendly Health Clinics in Maharashtra. Jaipur: IIHMR; 2010. International Institute of Health Management Research (IIHMR) [Google Scholar]
- 10.Santhya KG, Prakash R, Jejeebhoy SJ, Singh SK. Accessing Adolescent Friendly Health Clinics in India: The Perspectives of Adolescents and Youth. New Delhi: Population Council; 2014. [Google Scholar]
- 11.Yadav RJ, Mehta R, Pandey A, Adhikari T. Evaluation of adolescent-friendly health services. India. 2009;32:66–72. [Google Scholar]
- 12.Sigma A, Ehsan I, Tanjeen T, Reichenbach L. Adolescent Friendly Health Corners (AFHCs) in Selected Government Health Facilities in Bangladesh: An Early Qualitative Assessment, Research Report. Bangladesh: Population Council, the Evidence Project; 2017. [Last accessed on 2018 Mar 03]. Available from: http://www.evidenceproject.popcouncil.org/wp-content/uploads/2017/05/Bangladesh-AFHC-Report_2017.pdf . [Google Scholar]
- 13.Sunitha S, Gururaj G. Health behaviours & problems among young people in India: Cause for concern & call for action. Indian J Med Res. 2014;140:185–208. [PMC free article] [PubMed] [Google Scholar]
- 14.Srivastava NM. Adolescent Health in India: Need for more Interventional Research. Editorial. Clinical Epidemiology and Global Health. 2016;4(3):101–2. [Google Scholar]
- 15.Mahanta TG, Boruah M, Singh VK, Gogoi P, Rane T, Mahanta BN. Effect of social and behavior change communication by using infotainment in community perception of adolescent girls for reproductive and sexual health care in high priority districts of Assam. Clinical Epidemiology and Global Health. 2016;4(3):133–9. [Google Scholar]
- 16.Vir SC, Singh N, Nigam AK, Jain R. Weekly iron and folic acid supplementation with counseling reduces anemia in adolescent girls: A large-scale effectiveness study in Uttar Pradesh, India. Food Nutr Bull. 2008;29:186–94. doi: 10.1177/156482650802900304. [DOI] [PubMed] [Google Scholar]
- 17.Nath L, Arya RK, Gupta GK, Singh N. Challenges in implementation of adolescent health strategies of RMNCH+A in Ghaziabad. Santosh University Journal of Health Sciences. 2015;1(2):88–98. [Google Scholar]
- 18.Dhikale P, Suguna E, Thamizharasi A, Dongre A. Evaluation of weekly iron and folic acid supplementation program for adolescents in rural Pondicherry, India. International Journal of Medical Science and Public Health. 2015;4:360–5. [Google Scholar]
- 19.Ministry of Health and Family Welfare & Ministry of Human Resource Development. Operational Guidelines on School Health Programme Under Ayushman Bharat. Government of India. 2018 [Google Scholar]


