Abstract
Purpose:
To evaluate the surgical outcomes of repeat trabeculectomy augmented with risk factor adjusted mitomycin C (MMC) exposure in eyes with previous failed trabeculectomy.
Methods:
Case records of 38 eyes of 37 patients with previous failed filter who underwent repeat trabeculectomy with MMC were reviewed retrospectively. Main outcome measures were best-corrected visual acuity (BCVA), intraocular pressure (IOP) reduction, requirement of anti-glaucoma medications, postoperative complications, and surgical success (defined as IOP of ≤21 mmHg and >5 mmHg along with 20% reduction from preoperative IOP with or without adjuvant medications) at 1-year postoperatively. Statistical analysis was done using the STATA 14.1 (Texas, USA).
Results:
Patient's mean age was 46.41 (±20.43) years and the mean preoperative IOP was 32.73 (±9.26) mmHg which reduced to 16.22 (±7.08) mmHg postoperatively at 12 months (P < 0.001). Mean number of anti-glaucoma medications reduced from 2.76 (±0.83) preoperatively to 1.89 (±0.95) postoperatively (P < 0.001). Surgical success was observed in 81.1% at 1 year (n = 30). Eyes that received MMC >3 min had a postoperative mean IOP of 12.50 (±3.23) mmHg compared to 23.08 (±7.19) mmHg with MMC <3 min (P < 0.001). Seven eyes (18.4%) developed postoperative complications, and all were seen in eyes that received MMC >3 min (P = 0.033).
Conclusion:
Repeat trabeculectomy with MMC, used in higher concentration and exposure time altered according to individual risk factor plays a crucial role in the success and hence it could be considered as a viable option before planning a tube surgery.
Keywords: Failed trabeculectomy, mitomycin C, repeat trabeculectomy
Trabeculectomy has been considered as the gold standard procedure in the surgical management of all types of glaucoma since its inception, with high operative effect and low incidence of complications, and until recently has been the mainstay of treatment for glaucoma.[1] However, the success of trabeculectomy is often affected by subconjunctival fibrosis which may occur within days, months, or even years after surgery.[2,3] This fibrosis response can be seen even after Seton implant.[4] The anti-neoplastic-antibiotic agent mitomycin C (MMC) first introduced by Chen decreases fibroblast replication both in vitro and in animal models.[5] Subsequent studies have shown a higher intraocular pressure (IOP) lowering effect with intraoperative application of MMC at the surgical site of the future filtering bleb in eyes with poor surgical prognosis.[6,7]
Once surgical failure sets in, all measures are taken to re-establish IOP control beginning with medical management, digital maneuvers to improve the aqueous outflow, bleb needling, or further surgical intervention like repeat trabeculectomy or tube implant surgery.[8,9,10,11] Once the primary surgery fails, the success rate of subsequent surgery becomes low. Under such circumstances, one may have to choose to perform a repeat trabeculectomy with antimetabolites or a tube implant surgery. The outcomes of primary trabeculectomy have been reported in many studies, however, there are a very few reports describing the outcome of repeat trabeculectomy augmented with MMC. The success of repeat trabeculectomy is documented to be around 30–60%, however, none in the Indian subcontinent.[10,12,13,14] The results of tube versus trabeculectomy (TVT)[11] study did not show a clear superiority in IOP reduction between the two groups, however consistent IOP control with lesser re-surgeries were seen with drainage implants. This makes it imperative to understand if this is truly the best option especially in countries where patients may not be economically sound and only a few surgeons may be trained in drainage implants. Hence our study was conducted on south Indian population to understand the outcomes of repeat trabeculectomy augmented with MMC in terms of success and complications.
Methods
The study was approved by the institutional review board at our hospital (RET201500161). Retrospective case records of 38 eyes of 37 patients with previous failed filtering surgery who underwent repeat trabeculectomy with MMC at our institute between December 2015 to January 2017 were enrolled in the study.
Demographic data like age, sex, eye operated, diagnosis of glaucoma, previous surgery details like type of surgery, use of antimetabolite, dose, and duration of antimetabolite used were all collected. Preoperative visual acuity, IOP, slit-lamp biomicroscopy, gonioscopy, fundus, number of anti-glaucoma medications, and visual field parameters were included. All patients underwent repeat trabeculectomy augmented with MMC 0.4 mg/ml for 3–5 min. The duration of MMC application time was decided by the operating surgeon (Sharmila Rajendrababu) taking into account preoperative risk factors for failure like younger age, multiple previous ocular surgeries, previous unaugmented trabeculectomy, extensive fibrosis of surgical site which is denoted by the thickness and mobility of conjunctiva, and tenon's layer at the time of surgery. Patients with the above risk factors were chosen to have a prolonged MMC exposure. All surgeries were performed by a single senior glaucoma specialist (Sharmila Rajendrababu). The site of surgery was decided based on previous surgical site and the mobility of conjunctiva.
All surgeries were performed under retrobulbar anesthesia with bupivacaine 0.5% and hyaluronidase 3 IE/ml. A corneal traction suture using 7-0 silk was placed. The site of surgery was chosen based on mobility of conjunctiva by checking gently with a cotton tip bud/forceps. A 10–13 mm width fornix-based conjunctival flap was taken with additional undermining of surrounding conjunctiva along with the tenon's capsule was dissected. Light wet-field cautery was applied to areas of bleeding and care was taken to avoid excessive cautery. A weck-cell sponge cut into three small pieces were soaked in MMC 0.04 mg/ml and applied posteriorly over a wider area and covered with conjunctiva, carefully avoiding the edges of conjunctiva. The duration of MMC application was individualized according to surgeon's discretion. MMC for >3 min were used in eyes with secondary glaucoma/multiple previous surgeries/younger age groups. It was then thoroughly washed out with 20 ml of balanced salt solution. A 4 × 4 mm partial thickness triangular scleral flap was raised. After which a paracentesis incision was made and intracameral pilocarpine was injected and then anterior chamber was entered with 2.8 mm keratome. The trabeculectomy fistula of size 1.5 mm was created using a Kelly's punch. Peripheral iridectomy was performed at the ostium. The flap was then closed by one fixed apical and two lateral releasable sutures with 10-0 nylon. Saline was injected through the side port to check for the flow of aqueous, wound integrity, and anterior chamber formation. Lastly, conjunctiva was closed water tight using 8-0 vicryl sutures. Intracameral injection of 0.1 ml of 500 mcg moxifloxacin was given and the eye patched with atropine eye ointment.
Postoperative management
All patients were reviewed on Day 1, 2 weeks, 4 weeks, 6 weeks, 8 weeks, 3 months, and then every 6 months with additional review as and when required. Best-corrected visual acuity (BCVA), IOP, number of anti-glaucoma medications, complications, and postoperative interventions were all entered at every visit.
Medications used were antibiotic–steroid combination gatifloxacin 0.3% and dexamethasone 1% six times/day which was tapered gradually, one drop every 15 days, and atropine 1% two times a day for 4 weeks. The duration and frequency of use of each eyedrop was altered according to the clinical circumstances, but in all cases topical steroids were continued for at least 3 months after surgery.
If there were concerns, with regard to the evolving bleb morphology or uncontrolled IOP in the early postoperative period, one or more of the following intervention was undertaken: Bleb massage, releasable suture removal, laser suturolysis, or bleb needling with 5 Fluorouracil (5-FU) injection.
Statistical methods and outcome measures
Descriptive variables were given with frequency (percentage) or mean (standard deviation). Chi-square test/Fisher's exact test was used to find out the association between categorical variables. Pre- and Postoperative comparison of logMAR BCVA and mean number of medications was analyzed by the Wilcoxon signed-rank test and mean IOP was compared using paired t-test. Factors associated with the surgical outcome were elucidated using logistic regression analysis. Cumulative probability of success was evaluated by the Kaplan–Meier survival analysis. P value <0.05 considered as statistically significant. All the statistical analysis was done using the STATA 14.1 (Texas, USA).
Outcome measures
The primary outcome measure was the control of IOP. Secondary outcome measures were BCVA, reduction in mean number of anti-glaucoma medications, and the complications with repeat trabeculectomy. The reported outcome after trabeculectomy is strongly influenced by the definition of success.
Surgical success in our study was defined as IOP of ≤21 mmHg and >5 mmHg along with 20% reduction from preoperative IOP. Complete success was IOP reduction as mentioned above with no medication, and qualified success was IOP reduction with additional medications. Failure was defined as IOP level >21 mmHg or below the lower limit of 5 mmHg, complete loss of light perception or requirement of repeat glaucoma surgical intervention like a tube surgery or diode cyclophotocoagulation.
Results
Data analysis was performed on 38 eyes of 37 patients and with a follow up of 12 months. Baseline patient information and preoperative characteristics is given in Table 1. Mean age was 46.41 (±20.43) years. Mean period for onset of failure of primary trabeculectomy was 4.88 (±3.28) years, range 1–12 years, and median was 4 years [interquartile range (IQR), 2–8 years]. Bleb fibrosis was the most common reason for failure (91.6%), and tenon's cyst/ encysted bleb (8.4%) were other reasons for failure. Table 1 shows the preoperative diagnosis which was a mix of different glaucoma conditions requiring a repeat procedure, and majority of them had undergone a trabeculectomy once earlier (86.5%). Type of previous surgery included unaugmented trabeculectomy, trabeculectomy with MMC, combined phacotrabeculectomy with IOL, and trabeculectomy with 5-FU. Fourteen eyes (36.8%) received MMC ≤3 min and 24 eyes (63.2%) received MMC >3 min [Table 2].
Table 1.
Demographics and preoperative characteristics of patients who underwent repeat trabeculectomy
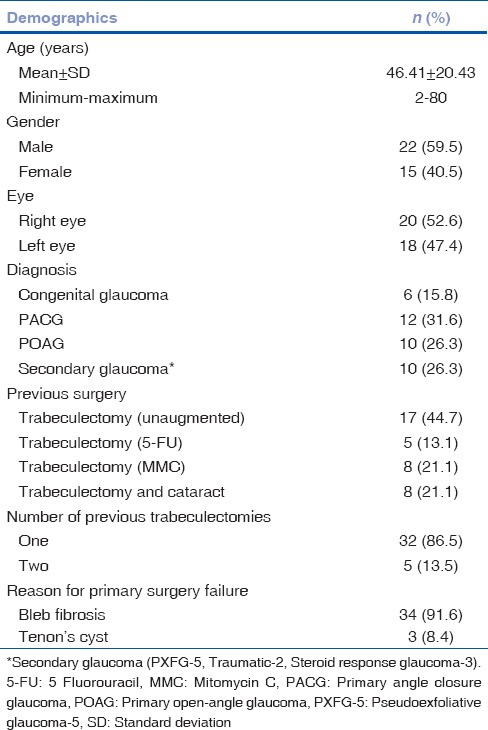
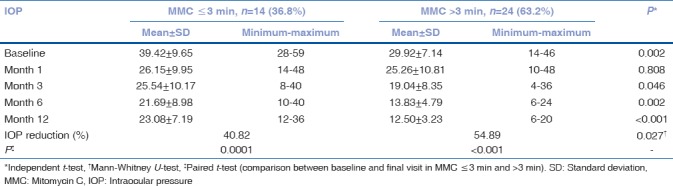
Table 2.
Comparison of intraocular pressure reduction based on the duration of mitomycin C application
Intraocular pressure outcome
Mean IOP and mean number of medications were plotted as a bar and line graph comparing the baseline values with each postoperative visit [Fig. 1]. At the final follow-up visit (12 months) the mean IOP dropped from preoperative value of 32.73 (±9.26) mmHg to 16.22 (±7.08) mmHg (P < 0.001) and the need for anti-glaucoma medication fell from a mean of 2.76 (±0.83) to 1.89 (±0.95) (P < 0.001). Table 2 compares the IOP reduction between two different duration of antimetabolite exposure. Eyes which received MMC for >3 min had a statistically significant IOP reduction of 54.89% compared to 40.82% in eyes that received MMC ≤3 min at final visit (P = 0.027).
Figure 1.
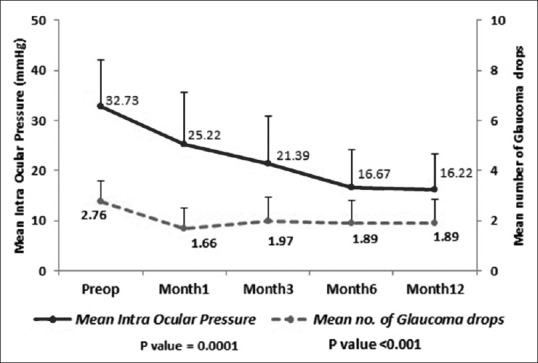
Intraocular pressure and number of medications at baseline and during follow up
Surgical success outcomes
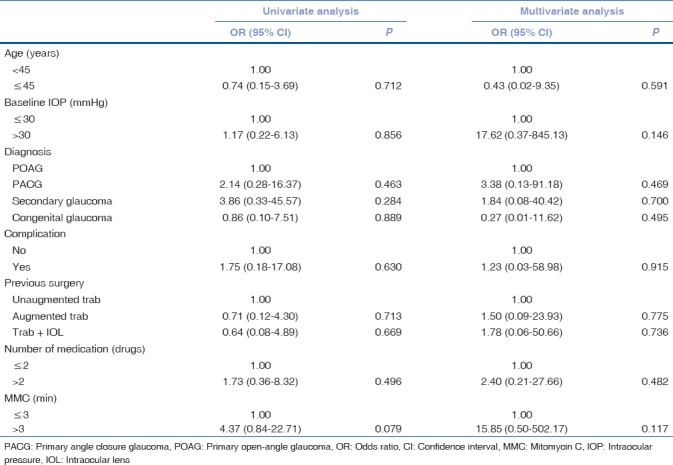
Overall success defined with IOP of ≤21 mmHg and >5 mmHg along with 20% reduction from preoperative IOP was achieved in 81.1% of patients at 1 year. Complete success (without medication) was achieved in 5.4% while 75.7% had qualified success (with medications) at 12 months. About 37.0% achieved qualified success with a single anti-glaucoma medication and 51.8% achieved success with two anti-glaucoma medications. The cumulative probability of success at 1, 3, 6, and 12 months were 92.1%, 88.7%, 83.8%, and 41.9%, respectively. Table 3 compares the surgical success outcomes between eyes that received MMC ≤3 min with MMC >3 min at every follow-up visit. At final visit, eyes that received MMC >3 min had total, complete, and qualified success of 91.7%, 8.3%, and 83.3%, respectively compared to a qualified success of 61.5% with none achieving complete success in eyes which received MMC ≤3 min (P = 0.059). To identify the factors associated with success a multiple regression analysis was done [Table 4]. There was no significant association with age, baseline IOP, diagnosis, number of preoperative medications, type of previous surgery, and complications, however, only longer duration exposure of MMC showed a marginally significant association to success (P = 0.079).
Table 3.
Success rate at each follow-up visit based on the duration of mitomycin C application
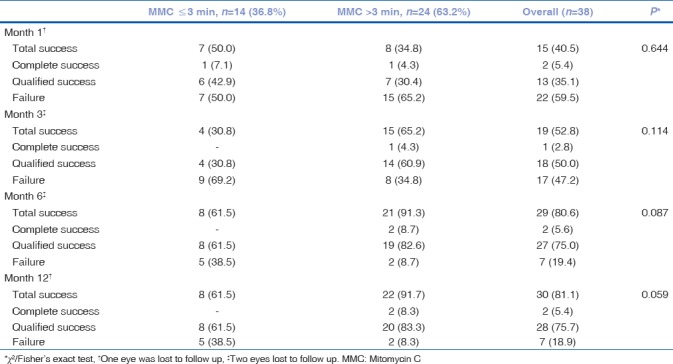
Table 4.
Multiple logistic regression analysis to find factors associated with surgical success of repeat trabeculectomy
Visual acuity outcomes
The mean logMAR BCVA was 0.83 (±0.89), median 0.60 (6/24, IQR 6/9–6/60) preoperatively and the mean logMAR BCVA was 0.91 (±1.02), median 0.30 (6/12, IQR 6/9–2/60) at final visit (P = 0.309). Eight patients lost >2 lines of vision at final follow up. Six out of those eight patients had cataract and two had macular degeneration.
Postoperative complications and interventions
Total of seven eyes (18.4%) developed postoperative complications, and they were all seen in eyes that received MMC >3 min (P = 0.033). Five amongst them were in the early postoperative period and two eyes presented late. Five cases of early complications were: one eye had hyphema on postoperative Day 1 that was managed conservatively; one had conjunctival buttonhole and one conjunctival retraction requiring resuturing and bleb revision. One case of choroidal was managed conservatively. One patient developed aqueous misdirection at 4weeks, which was treated with steroids and atropine. This was persistent even after 12 weeks despite medical management and subsequently underwent pars plana vitrectomy with anterior chamber reformation at 16 weeks.
Late postoperative complications was one case of kissing choroidals which required choroidal drainage due to persistent hypotony. One patient developed endophthalmitis, with sudden decrease is visual acuity and severe pain at 20 weeks and underwent vitreous tap with intravitreal vancomycin + cefazolin + dexamethasone and topical antibiotics, and had a significant improvement in visual acuity.
Failure was observed in seven eyes. One patient required bleb revision with corneal patch graft. Four eyes underwent glaucoma drainage implant to control IOP. Two patients underwent cyclophotocoagulation. Routine postoperative protocol to improve the success of filter in the form of digital massage, releasable suture removal, and or laser suturolysis to titrate the IOP was done for all patients at every visit. Six patients showed early signs of fibrosis and underwent bleb needling with 5-FU injection at third and fourth week.
Discussion
Multiple factors contribute to the failure of filtering surgery, the most common one is subconjunctival fibrosis, and with a previously failed trabeculectomy this risk is even higher. MMC augmented filtering surgeries have proven to improve the success of primary trabeculectomies,[15,16] however, its role in improving success of repeat trabeculectomy and its effectiveness over tube surgery is still unclear making surgeons decision often difficult.
The present study demonstrates that repeat trabeculectomy augmented with high dose of MMC (0.4 mg/ml) with exposure time titrated according to individual risk factor adjusted protocol helps in improved bleb survival until close to a year after surgery. Eyes which received MMC for >3 min had a statistically significant IOP reduction of 54.89% compared to 40.82% in eyes that received MMC ≤3 min at final visit (P = 0.027). But this could not be solely attributed to the duration of MMC exposure per se as there was a significant difference between the two groups at baseline.
Our study demonstrated a positive correlation between better surgical outcome and prolonged exposure of MMC on multiple regression analysis. Total success in our study group was 81.1%, of which eyes received MMC >3 min had marginally significant IOP reduction, with qualified success of 83.3% compared to 61.5% in MMC <3 min at 1 year (P = 0.059). Our results were comparable with studies by Rodriguez-Una et al.,[17] Meyer et al.,[10] and Yun and Cha[18] with similar MMC dosing schedule which had a longer follow up.
Several studies comparing the outcomes of repeat trabeculectomy and primary trabeculectomy, had concluded that the second surgery is less successful in terms of IOP control.[14,19] Law et al.[14] compared the results of repeat trabeculectomy with a series of matched primary trabeculectomy with MMC (used for 1 min in all patients) and found a qualified success of only 54.6% in the repeat trabeculectomy group. On the contrary Cha et al.[20] who also compared the outcome of primary and repeat trabeculectomy with MMC reported a better success of 89.9% in their 18 repeat trabeculectomy eyes which is comparable to our success of 81.1%. Differences in results may be related to the surgical technique, MMC dose and duration of exposure, less aggressive postoperative bleb manipulation, a different case mix of patients undergoing glaucoma surgery, and definition of success criteria.
In spite of meticulous tissue handling and use of releasable sutures failure was noted in 7 eyes; 1 underwent bleb revision, four underwent a tube surgery, and two had diode cyclophotocoagulation. Seven patients developed postoperative complications in the group with longer duration of MMC exposure. This signifies that despite increased likelihood of fibrosing response in eye with prior trabeculectomy, one needs to exercise extreme caution while using antifibrotics.
Recently the TVT study supported a shift in practice pattern among surgeons toward greater use of tube shunts in eyes with previous ocular surgery. Their results suggested that IOP control was more consistent with tube surgery than that achieved with trabeculectomy with MMC (0.5 mg/ml) in patients with previous trabeculectomy or cataract extraction.[11] Qualified success rate at 3 years in patients who had a previous surgery was 71.4% in the trabeculectomy group compared to 75.7% in our cohort. However only a small strata of the TVT study were patients who had undergone previous failed trabeculectomy. Also, the TVT study did not establish clear superiority in IOP control between the trabeculectomy and tube groups.
In situations as in India where ophthalmologists trained in tube surgeries are not widely available, a repeat trabeculectomy with high dose mitomycin is an effective alternative to glaucoma drainage implants in eyes with subconjunctival fibrosis and progressive glaucoma. Close monitoring of IOP and judicious use of postoperative bleb modulation is indicated to optimize outcomes and minimize complications in eyes with repeat trabeculectomy.
Our study had a few limitations, like the retrospective study design, a modest sample size with a short follow-up period. Major shortcoming was that it is not a comparative or a randomized study to evaluate safety and efficacy of repeat trabeculectomy in eyes with subconjunctival fibrosis. Heterogeneous group of eyes with different types of glaucoma and age groups is also likely to have confounded the results, since eyes with congenital glaucoma or other secondary glaucoma's are likely to be refractory to multiple surgical treatments.[21,22]
Strength of the present study was that all surgeries were done by a single experienced surgeon, with a standard dose of MMC, and to the best of our knowledge this is the first study in Indian population analyzing the surgical outcomes in eyes undergoing repeat trabeculectomy. Future multicenter studies randomizing eyes with failed filters to tube vs. repeat trabeculectomy and also randomizing the MMC exposure time to less than or more than 3 min with a longer follow up are likely to help surgeons chose an ideal surgical procedure for eyes with progressive glaucoma after failed initial trabeculectomy.
Conclusion
Success of repeat trabeculectomy is unpredictable and depends on multiple factors. Considering the inherent likelihood of failure and poor success with repeat trabeculectomy, and with results of TVT study one may need to weigh the risks and benefits of each, before choosing an appropriate surgery in eyes with previous failed filters. Our study demonstrates that repeat trabeculectomy augmented with high dose of MMC (0.4 mg/ml) with exposure time altered according to individual risk factor adjusted protocol helps in improving bleb survival and it would therefore be unwise to abandon this viable option completely in the management of patients with previously failed trabeculectomy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ramulu PY, Corcoran KJ, Corcoran SL, Robin AL. Utilization of various glaucoma surgeries and procedures in medicare beneficiaries from 1995 to 2004. Ophthalmology. 2007;114:2265–70. doi: 10.1016/j.ophtha.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Skuta GL, Parrish RK 2nd. Wound healing in glaucoma filtering surgery. Surv Ophthalmol. 1987;32:149–70. doi: 10.1016/0039-6257(87)90091-9. [DOI] [PubMed] [Google Scholar]
- 3.Broadway DC, Grierson I, Hitchings RA. Local effects of previous conjunctival incisional surgery and the subsequent outcome of filtration surgery. Am J Ophthalmol. 1998;125:805–18. doi: 10.1016/s0002-9394(98)00045-2. [DOI] [PubMed] [Google Scholar]
- 4.Classen L, Kivelä T, Tarkkanen A. Histopathologic and immunohistochemical analysis of the filtration bleb after unsuccessful glaucoma Seton implantation. Am J Ophthalmol. 1996;122:205–12. doi: 10.1016/s0002-9394(14)72011-2. [DOI] [PubMed] [Google Scholar]
- 5.Chen CW. Enhanced intraocular pressure controlling effectiveness of trabeculectomy by local application of mitomycin C. Trans Asia Pac Acad Ophthalmol. 1983;9:172. [Google Scholar]
- 6.Singh K, Mehta K, Shaikh NM, Tsai JC, Moster MR, Budenz DL, et al. Trabeculectomy with intraoperative mitomycin C versus 5-fluorouracil. Prospective randomized clinical trial. Ophthalmology. 2000;107:2305–9. doi: 10.1016/s0161-6420(00)00391-2. [DOI] [PubMed] [Google Scholar]
- 7.Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma. 2001;10:237–49. doi: 10.1097/00061198-200106000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Iwach AG, Delgado MF, Novack GD, Nguyen N, Wong PC. Transconjunctival mitomycin-C in needle revisions of failing filtering blebs. Ophthalmology. 2003;110:734–42. doi: 10.1016/S0161-6420(02)01978-4. [DOI] [PubMed] [Google Scholar]
- 9.Fagerli M, Løfors KT, Elsås T. Needling revision of failed filtering blebs after trabeculectomy: A retrospective study. Acta Ophthalmol Scand. 2003;81:577–82. doi: 10.1046/j.1395-3907.2003.0126.x. [DOI] [PubMed] [Google Scholar]
- 10.Meyer LM, Graf NE, Philipp S, Fischer MT, Haller K, Distelmaier P, et al. Two-year outcome of repeat trabeculectomy with mitomycin C in primary open-angle and PEX glaucoma. Eur J Ophthalmol. 2015;25:185–91. doi: 10.5301/ejo.5000542. [DOI] [PubMed] [Google Scholar]
- 11.Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL, et al. Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol. 2009;148:670–84. doi: 10.1016/j.ajo.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Eslami Y, Samarai V, Mohammadi M, Fakhraie G, Zarei R, Eslami S, et al. Outcomes of same-site re-operation with minimal use of mitomycin in failed trabeculectomy. Int Ophthalmol. 2014;34:501–4. doi: 10.1007/s10792-013-9840-5. [DOI] [PubMed] [Google Scholar]
- 13.Olali C, Rotchford AP, King AJ. Outcome of repeat trabeculectomies. Clin Exp Ophthalmol. 2011;39:658–64. doi: 10.1111/j.1442-9071.2011.02519.x. [DOI] [PubMed] [Google Scholar]
- 14.Law SK, Shih K, Tran DH, Coleman AL, Caprioli J. Long-term outcomes of repeat vs. initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol. 2009;148:685–950. doi: 10.1016/j.ajo.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 15.Scott IU, Greenfield DS, Schiffman J, Nicolela MT, Rueda JC, Tsai JC, et al. Outcomes of primary trabeculectomy with the use of adjunctive mitomycin. Arch Ophthalmol. 1998;116:286–91. doi: 10.1001/archopht.116.3.286. [DOI] [PubMed] [Google Scholar]
- 16.Smith MF, Doyle JW, Nguyen QH, Sherwood MB. Results of intraoperative 5-fluorouracil or lower dose mitomycin-C administration on initial trabeculectomy surgery. J Glaucoma. 1997;6:104–10. [PubMed] [Google Scholar]
- 17.Rodriguez-Una I, Rotchford AP, King AJ. Outcome of repeat trabeculectomies: Long-term follow-up. Br J Ophthalmol. 2017;101:1269–74. doi: 10.1136/bjophthalmol-2016-309318. [DOI] [PubMed] [Google Scholar]
- 18.Yun YS, Cha SC. Outcomes of repeat trabeculectomy with mitomycin C for previous failed trabeculectomy. J Korean Ophthalmol Soc. 2005;46:297–305. [Google Scholar]
- 19.Cankaya AB, Elgin U. Comparison of the outcome of repeat trabeculectomy with adjunctive mitomycin C and initial trabeculectomy. Korean J Ophthalmol. 2011;25:401–8. doi: 10.3341/kjo.2011.25.6.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cha S, Son J, Chang J, Chung W. Comparism of surgical outcomes in primary trabeculectomy with mitomycin C versus repeat trabeculectomy with mitomycin C. Invest Ophthalmol Vis Sci. 2004;45:SS94–B878. [Google Scholar]
- 21.Mandal AK, Gothwal VK, Nutheti R. Surgical outcome of primary developmental glaucoma: A single surgeon's long-term experience from a tertiary eye care centre in India. Eye (Lond) 2007;21:764–74. doi: 10.1038/sj.eye.6702324. [DOI] [PubMed] [Google Scholar]
- 22.Mandal AK, Netland PA. Amsterdam: Elsevier; 2006. The pediatric glaucomas; p. 86. [Google Scholar]


