Abstract
Purpose:
To compare the visual outcomes and complications between the eyes receiving retropupillary iris claw intraocular lens (IOL) and scleral-fixated IOL (SFIOL) for post-cataract aphakia.
Methods:
Medical records of consecutive patients who had iris claw IOL and SFIOL surgery from January 2010 to March 2015, with > 1 year of follow up were retrospectively analyzed. The surgical technique was based on individual surgeon preference. The best-corrected distance visual acuity (BCDVA), previous surgery, surgical technique, and complications were analyzed.
Results:
Retropupillary iris claw IOL was fixated in 48 eyes (46%) and SFIOL was performed in 56 eyes. Iris claw was performed more frequently at the time of primary cataract surgery (56%) compared to SFIOL (14%) (P < 0.001). At 1 month postoperative, BCDVA was significantly better in the SFIOL group [0.7 ± 0.5 logarithm of minimum angle of resolution (logMAR) in iris claw vs. 0.3 ± 0.2 logMAR in SFIOL, P < 0.001] but this difference did not persist at 1 year (0.4 ± 0.4 logMAR in iris claw vs. 0.3 ± 0.2 logMAR in SFIOL, P = 0.56). Eyes with iris claw IOL experienced significantly more postoperative iritis (17%), intraocular pressure spikes (10%), and ovalization of the pupil (16%).
Conclusion:
Retropupillary iris claw IOL fixation is as safe as SFIOL for visual rehabilitation of post-cataract aphakia. Visual rehabilitation following iris claw IOL might take longer than SFIOL. Ovalization of the pupil is the commonest adverse effect reported with this type of IOL design.
Keywords: Aphakia, comparison, iris claw IOL, long-term, SFIOL, sutureless
Surgical correction of aphakia has evolved over the past few decades and has seen paradigm shifts in the past few years. Open-loop anterior chamber intraocular lenses (IOLs) that were angle fixated have largely fallen out of repute due to relatively higher incidence of secondary glaucoma, corneal endothelial decompensation, and cystoid macular edema (CME).[1,2] Scleral-fixated IOLs (SFIOLs) have been extensively utilized for surgical correction of aphakia with excellent results.[3,4] Suturing the SFIOL using non-absorbable sutures has been the traditionally accepted technique of IOL placements. Recently, Scharioth et al. popularized a technique of sutureless scleral fixation of a routinely used 3-Piece IOL which was modified by Kumar and Agarwal using fibrin glue to secure the exteriorized haptics under scleral flaps.[5,6] A comparative study between sutured and sutureless SFIOL in the Indian scenario showed that both were equally effective and yielded excellent visual results even after 2 years of follow up.[3]
Fixation of the IOL to the iris has been also described in the past.[2] Anterior chamber IOLs fixing the haptics to the anterior surface of the iris such as the Binkhorst lens have been described over 4 decades ago and are of historical importance now.[7] Suturing the IOL haptics to the iris using non-absorbable sutures have also been described in the past.[2] Recently, interest has been revived in retropupillary fixation of the iris claw lenses in view of their ease of surgery and relatively good results.[8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24] The retropupillary fixation of the iris claw lens theoretically reduces the risk of corneal endothelial damage but may be associated with higher incidence of pupillary distortions, glaucoma, and other complications. However, many studies have shown excellent outcomes and have established the effectiveness of this surgical approach in correcting aphakia.
Considering the increasing popularity of retropupillary fixation of iris claw lens, a comparison of their outcomes to those of the well-established techniques of SFIOL is required. Rashad et al. performed such a prospective study and concluded that the surgical procedure for iris claw IOL fixation was easier, shorter, and safer than sutured SFIOL.[23] However, we are unaware of similar studies comparing iris claw IOL fixation with sutureless SFIOL, which are commonly performed in the current era.
We performed a retrospective study to analyze the early and long-term differences in the outcomes of eyes undergoing retropupillary iris claw IOL and sutureless SFIOL in two tertiary eye care centers in South India.
Methods
This retrospective study was approved by the institutional review board of the parent institution and followed the tenets of the declaration of Helsinki. Informed consent was obtained from all patients prior to surgery. Case records of all patients who underwent retropupillary fixation of iris claw IOL and those who received SFIOL, between January 2010 and March 2015, were retrieved from the medical records department. All eyes that underwent iris claw or SFIOL for post-cataract aphakia, either as a primary (i.e. at time of cataract surgery) or secondary sitting and had a minimum follow up of 1 year were included in the analysis. Those who had previous pars plana vitrectomy for post-cataract nucleus, cortex, or IOL drop were also included. Those with preexistent glaucoma, pseudoexfoliation, corneal opacity in visual axis, aphakia following trauma, penetrating keratoplasty, and such other procedures were excluded. Iris claw IOL fixation was carried out by a fellowship trained vitreoretina surgeon (NM) and the SFIOL surgeries were also performed by a different fellowship trained vitreoretina surgeon (MDS). Both surgeons were experienced at the procedures and had performed > 500 surgeries over the past 3 years. The timing of IOL placement (at time of primary cataract surgery vs. secondary procedure) was based on the surgeon preference alone.
Baseline demographic data like age, gender, and involved eye were noted. Preoperative characteristics including previous surgical procedure (cataract surgery, pars plana vitrectomy, lensectomy, etc.) and duration between previous cataract surgery and IOL implantation were recorded. Any preexisting corneal, retinal, or macular pathology, the technique used for IOL placement, and any intraoperative and postoperative complications were also recorded from the charts. Spike in intraocular pressure (IOP) in the early postoperative period was recorded when IOP was > 21 mmHg and required topical antiglaucoma medications to be controlled. Iritis was graded as per established norms and was classified as severe if cells and/or flare of > 3+ were noted in the case files. CME was recorded from the case files if it was noted either clinically or on optical coherence tomography. Uncorrected distance visual acuity (UCDVA) and best-corrected distance visual acuity (BCDVA) were recorded for the baseline visit and at 1 month, 1 year, or last follow-up whichever was later.
Surgical technique
Iris claw IOL implantation: The optima iris claw IOL (Rainbow MeditechLLC, Chennai, India) with optic size of 5.50 mm, length of 8 mm, and a constant of 117.2 were used during the study period. We preferred the SRK/T formula for all IOL power calculations. Under peribulbar anesthesia conjunctiva was separated and superior sclerocorneal tunnel incision was made. A 23-gauge pars plana vitrectomy was performed in all cases using triamcinolone acetonide assistance following which the pupil was constricted using intracameral pilocarpine. Two limbal paracentesis were made 180° apart, the iris claw IOL was placed over the iris, one haptic was guided below the iris and enclaved in the mid-peripheral iris using a blunt sinskey hook or ball dialer. The same procedure was repeated for the other haptic. Peripheral iridectomy was not performed in any case. Finally, wound integrity was checked and wound sutured if required. Subconjunctival steroids were injected in all cases.
SFIOL implantation: Our surgical technique for sutureless SFIOL is similar to that described previously[3] where the haptics of a regular rigid 3-Piece IOL (B3602, Aurolab) were exteriorized and tucked into scleral pockets.
Statistical analysis
All continuous variables were expressed as mean with standard deviation or median with interquartile range (IQR) and all categorical variables were expressed as proportions. Group differences in the continuous variables were analyzed using the Student's t-test or the Wilcoxon rank sum test, whereas group differences in categorical variables were analyzed using the Chi-squared or the Fisher's exact test. All data were entered in Microsoft Excel and analyzed using the STATA 12.0 (STATA Corp, Fort Worth, Texas). All P values < 0.05 were considered statistically significant.
Results
Data from 104 eyes of 104 patients satisfying the inclusion criteria were statistically analyzed. The mean age of patients was 63.6 ± 10.8 years and 53 (51%) were men. Retropupillary iris claw IOL was fixated in 48 eyes (46%) and sutureless SFIOL was performed in the remaining 56 eyes.
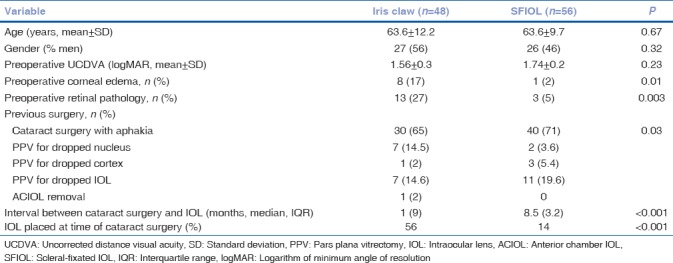
A comparison of the preoperative characteristics between eyes with iris claw IOL and SFIOL is shown in Table 1. Iris claw IOL fixation was performed at the same sitting as cataract surgery (i.e. primary placement) much more frequently compared to SFIOL. Even when performing as a secondary procedure, the iris claw IOL was fixated much sooner after the previous cataract surgery (median = 1 month) compared to the SFIOL. Eyes with iris claw had significantly more corneal edema at the time of secondary IOL placement and had significantly more retinal pathology [diabetic retinopathy (n = 6), high myopia (n = 4), macular hole (n = 1), epiretinal membrane (n = 2)] compared to the SFIOL group [epiretinal membrane (n = 1), previous retinal detachment (RD) (n = 2)]. For eyes that underwents a secondary surgery for IOL placement, the preoperative BCVA was significantly lower in the iris claw group compared to the SFIOL group.
Table 1.
Preoperative characteristics iris claw vs. scleral-fixated intraocular lens in management of post-cataract aphakia
There were no intraoperative complications noted in either of the surgical groups. At 1-month postoperative period, eyes with SFIOL had better BCVA compared to those that received iris claw IOLs [Table 2]. However, there was no difference in BCVA at 1-year follow up. Fig. 1 shows a comparison of BCVA between iris claw and SFIOL groups at 1-month and 1-year time points. Overall, the uncorrected visual acuity (UCVA) improved from 2/60 to 6/24 in the iris claw group (P < 0.001) and from 1/60 to 6/36 in the SFIOL group (P < 0.001, paired t test). A BCVA of 6/12 or better was achieved by 71% eyes (n = 34) that received the iris claw IOL and in 77% eyes (n = 43) that received SFIOL (P = 0.41).
Table 2.
Postoperative complications and visual outcomes of iris claw vs. scleral-fixated intraocular lens
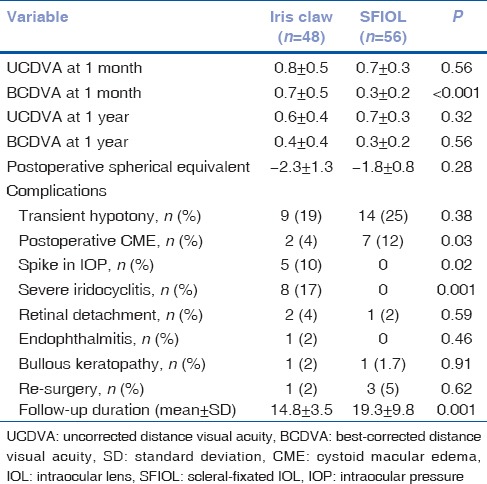
Figure 1.
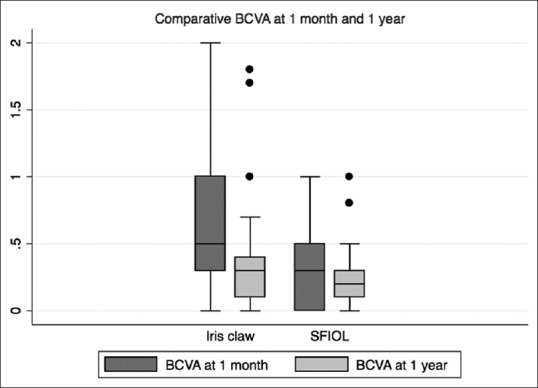
Box-and-whisker plot showing best-corrected visual acuity comparisons at 1 month and 1 year between iris claw and scleral-fixated intraocular lens
Over the postoperative period, eyes that received the iris claw IOL experienced greater transient IOP spikes and had significantly greater instances of severe iritis compared to SFIOL eyes [Table 2]. However, eyes with SFIOL had greater incidence of postoperative CME. Ovalization of the pupil was seen in eight eyes (16%) with iris claw IOL. There was no difference in groups in terms of other postoperative complications [Table 2]. One eye in the iris claw group underwent re-surgery for wound suturing, while three eyes in the SFIOL group underwent re-surgery, two for globe reformation due to hypotony, and one for haptic re-fixation. None of the eyes with iris claw IOL experienced de-enclavation or drop into the vitreous cavity. There was no difference in outcomes between iris claw IOL fixated as primary vs. secondary setting.
Discussion
We compared the 1-year outcomes of eyes undergoing retropupillary iris claw IOL fixation and SFIOL implantation and found that more than half the iris claw IOLs were placed at the same time as primary cataract surgery as opposed to very few SFIOL done in primary setting, visual outcomes in the iris claw group was not as good as SFIOL in the initial postoperative period, though this difference in vision did not persist at 1 year and both the IOL types were safe with minimal vision threatening adverse effects over a minimum of 1-year follow up.
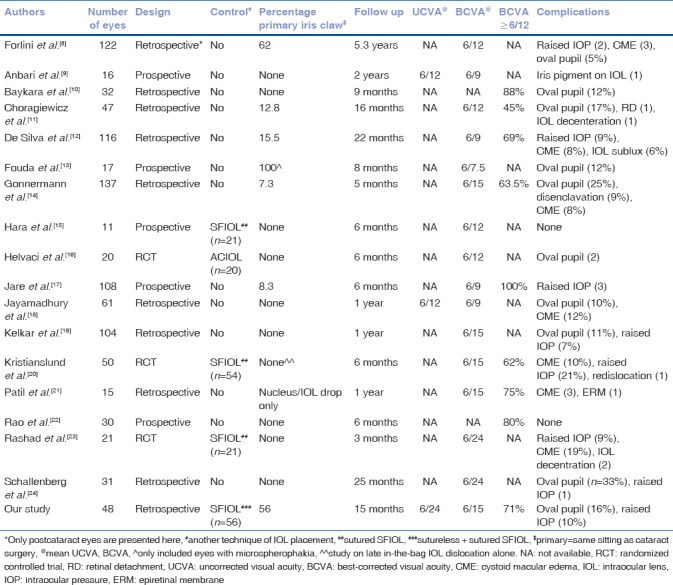
In terms of technical difficulty, it is much easier to enclave the iris claw IOL to the posterior surface of the iris compared to implanting the SFIOL using either the sutured or sutureless technique. Additionally, the iris claw IOL fixation also takes much shorter time to complete than the SFIOL.[23] Due to these advantages, it is more likely that the cataract surgeon will opt for fixation of the iris claw IOL at the time of primary cataract surgery, as seen from our results where > 50% cases were done as a primary procedure. Most authors have fixated the iris claw IOL as a secondary procedure [Table 3], except for Forlini et al.[8] who performed the surgery in the primary sitting in majority. Given that our results show no difference in complications or outcomes with primary vs. secondary iris claw IOL, echoed by Forlini et al., primary fixation may be desirable in most cases due to surgical ease and the advantage of avoiding an additional surgery.
Table 3.
Summary of recent studies available in English literature on the outcomes of retropupillary iris claw intraocular lens fixation
The visual outcomes in the iris claw group were inferior to SFIOL at 1 month after surgery, but at 1 year there were no differences. This could be because eyes with iris claw IOL had more retinal comorbidities such as high myopia and diabetic retinopathy compared with eyes that had SFIOL. Yet, most of these were not vision threatening but may predispose to delayed wound healing and visual recovery. Another reason could be that a lot of the iris claw lenses were fixated at the time of cataract surgery or very soon after (at 1 month), thus leading to delayed wound healing and visual stabilization. In contrast, most SFIOLs were performed as planned secondary procedures in quiet eyes and resulted in minimal inflammation, leading to quicker wound healing and visual recovery.
There have been many reports of visual outcomes of retropupillary iris claw IOL placement in the recent past [Table 3]. Our results in the iris claw group are very similar to that reported in literature. In contrast, there are very few studies comparing iris claw with SFIOL in the sitting of post-cataract aphakia. Rashad et al. performed a randomized controlled study (without masking) of 21 eyes with iris claw vs. 21 eyes with sutured SFIOL and found no differences in best-corrected vision and complications.[23] However, this study reported outcomes limited to 3 months postoperative period compared to our outcomes beyond 1 year in all eyes. We found a higher incidence of CME in the SFIOL group, which was surprising. It is possible that using triamcinolone-assisted vitrectomy in the iris claw group reduced the incidence of CME, as shown by Kelkar et al. recently.[19] We also found a higher incidence of transient-raised IOP (spikes) in the iris claw group probably due to lack of prophylactic iridectomy not being performed in these eyes as well as greater pigment dispersion which is expected due to enclavation of iris tissue.
Ovalization of the pupil is a consistent finding reported by all studies on retropupillary iris claw IOL fixation [Table 3] and can be as high as 33%. Distortion of the pupil may compromise quality of vision regained by patients, however, this phenomenon has never been adequately addressed in the literature. Additionally, enclavation of iris tissue may cause localized or generalized atrophic changes in the iris and thereby affect the physiological functioning of the pupil. Very few studies have followed up patients for > 1 year and, those which have, do not employ anterior segment OCT (ASOCT) to document changes in the iris architecture and pupil dynamics in bright and dim illumination. Prospective studies in the future should address these issues with longer follow-up data.
The advantages of our study are the comparative design, relatively good sample, and follow-up periods. The drawbacks are the retrospective design and lack of data regarding endothelial cell counts and dynamic changes occurring in the iris and pupil over the follow-up period.
Conclusion
Retropupillary iris claw IOL fixation is as safe as SFIOL for visual rehabilitation of post-cataract aphakia. Both primary (i.e. at the time of cataract surgery) and secondary approaches yield comparable visual results. Visual rehabilitation following iris claw IOL might take longer than SFIOL and ovalization of the pupil is the commonest adverse effect reported with this type of IOL design. Lastly, as SFIOL implantation is much more technically challenging with a longer learning curve compared to iris claw IOL, the choice of IOL depends on the surgeons’ expertise and previous exposure. Also, iris claw IOLs may be preferred in eyes with poorly dilating pupils without other iris deformities as in such cases, performing SFIOL becomes extremely difficult. Future randomized control trials are required with larger sample, better methodologies including serial ASOCT images and longer follow up to determine superiority of one IOL type over the other.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Evereklioglu C, Er H, Bekir NA, Borazan M, Zorlu F. Comparison of secondary implantation of flexible open-loop anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29:301–8. doi: 10.1016/s0886-3350(02)01526-2. [DOI] [PubMed] [Google Scholar]
- 2.Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL American Academy of phthalmology. Intraocular lens implantation in the absence of capsular support: A report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:840–59. doi: 10.1016/s0161-6420(02)02000-6. [DOI] [PubMed] [Google Scholar]
- 3.Sindal MD, Nakhwa CP, Sengupta S. Comparison of sutured versus sutureless scleral-fixated intraocular lenses. J Cataract Refract Surg. 2016;42:27–34. doi: 10.1016/j.jcrs.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 4.Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144:371–7. doi: 10.1016/j.ajo.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Scharioth GB, Prasad S, Georgalas I, Tataru C, Pavlidis M. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2010;36:254–9. doi: 10.1016/j.jcrs.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Kumar DA, Agarwal A. Glued intraocular lens: A major review on surgical technique and results. Curr Opin Ophthalmol. 2013;24:21–9. doi: 10.1097/ICU.0b013e32835a939f. [DOI] [PubMed] [Google Scholar]
- 7.Bras JF. Review of binkhorst intraocular lenses. Br J Ophthalmol. 1977;61:631–3. doi: 10.1136/bjo.61.10.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forlini M, Soliman W, Bratu A, Rossini P, Cavallini GM, Forlini C, et al. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: A retrospective analysis. BMC Ophthalmol. 2015;15:143. doi: 10.1186/s12886-015-0146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anbari A, Lake DB. Posteriorly enclavated iris claw intraocular lens for aphakia: Long-term corneal endothelial safety study. Eur J Ophthalmol. 2015;25:208–13. doi: 10.5301/ejo.5000527. [DOI] [PubMed] [Google Scholar]
- 10.Baykara M, Ozcetin H, Yilmaz S, Timuçin OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol. 2007;144:586–91. doi: 10.1016/j.ajo.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 11.Choragiewicz T, Rejdak R, Grzybowski A, Nowomiejska K, Moneta-Wielgoś J, Ozimek M, et al. Outcomes of sutureless iris-claw lens implantation. J Ophthalmol 2016. 2016:7013709. doi: 10.1155/2016/7013709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Silva SR, Arun K, Anandan M, Glover N, Patel CK, Rosen P, et al. Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg. 2011;37:1667–72. doi: 10.1016/j.jcrs.2011.03.051. [DOI] [PubMed] [Google Scholar]
- 13.Fouda SM, Al Aswad MA, Ibrahim BM, Bori A, Mattout HK. Retropupillary iris-claw intraocular lens for the surgical correction of aphakia in cases with microspherophakia. Indian J Ophthalmol. 2016;64:884–7. doi: 10.4103/0301-4738.198844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139–43. doi: 10.1016/j.jcrs.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 15.Hara S, Borkenstein AF, Ehmer A, Auffarth GU. Retropupillary fixation of iris-claw intraocular lens versus transscleral suturing fixation for aphakic eyes without capsular support. J Refract Surg. 2011;27:729–35. doi: 10.3928/1081597X-20110623-01. [DOI] [PubMed] [Google Scholar]
- 16.Helvaci S, Demirduzen S, Oksuz H. Iris-claw intraocular lens implantation: Anterior chamber versus retropupillary implantation. Indian J Ophthalmol. 2016;64:45–9. doi: 10.4103/0301-4738.178139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jare NM, Kesari AG, Gadkari SS, Deshpande MD. The posterior iris-claw lens outcome study: 6-month follow-up. Indian J Ophthalmol. 2016;64:878–83. doi: 10.4103/0301-4738.198843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jayamadhury G, Potti S, Kumar KV, Kumar RM, Divyansh Mishra KC, Nambula SR, et al. Retropupillary fixation of iris-claw lens in visual rehabilitation of aphakic eyes. Indian J Ophthalmol. 2016;64:743–6. doi: 10.4103/0301-4738.195012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelkar A, Shah R, Vasavda V, Kelkar J, Kelkar S. Primary iris claw IOL retrofixation with intravitreal triamcinolone acetonide in cases of inadequate capsular support. Int Ophthalmol. 2018;38:111–7. doi: 10.1007/s10792-017-0467-9. [doi: 101007/s10792-017-0467-9] [DOI] [PubMed] [Google Scholar]
- 20.Kristianslund O, Råen M, Østern AE, Drolsum L. Late in-the-bag intraocular lens dislocation: A Randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology. 2017;124:151–9. doi: 10.1016/j.ophtha.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 21.Patil KB, Meleth P, Shanker MP. Pars plana vitrectomy with posterior iris claw implantation for posteriorly dislocated nucleus and intraocular lens. Indian J Ophthalmol. 2011;59:497–500. doi: 10.4103/0301-4738.86321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rao R, Sasidharan A. Iris claw intraocular lens: A viable option in monocular surgical aphakia. Indian J Ophthalmol. 2013;61:74–5. doi: 10.4103/0301-4738.107198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rashad DM, Afifi OM, Elmotie GA, Khattab HA. Retropupillary fixation of iris-claw intraocular lens versus trans-scleral suturing fixation for aphakic eyes without capsular support. J Egypt Ophthalmol Soc. 2015;108:157–66. [Google Scholar]
- 24.Schallenberg M, Dekowski D, Hahn A, Laube T, Steuhl KP, Meller D, et al. Aphakia correction with retropupillary fixated iris-claw lens (Artisan) – Long-term results. Clin Ophthalmol. 2014;8:137–41. doi: 10.2147/OPTH.S55205. [DOI] [PMC free article] [PubMed] [Google Scholar]


