Abstract
Duane retraction (or co-contraction) syndrome is a congenital restrictive strabismus which can occur either as an isolated entity or in conjunction with other congenital anomalies and is now listed as a congenital cranial dysinnervation disorder. It is characterized by co-contraction of horizontal recti on attempted adduction causing globe retraction along with variable amounts of upshoots or downshoots. It may have limited abduction or adduction or both and present as esotropic, exotropic, or orthotropic Duane. The diagnosis of this disease is usually clinical. However, recent research has provided a greater insight into the genetic basis of this disease paving a way for a greater role of genetics in the diagnosis and management. This disease can have a varied presentation and hence the treatment plan should be tailor-made for every patient. The indications for surgery are abnormal head posture, deviations in the primary position, retraction and narrowing of palpebral aperture and up- or downshoots during adduction, and sometimes also to improve abduction. The arrival of newer surgical techniques of periosteal fixation (PF) of lateral rectus (LR), partial vertical rectus transposition, or superior or inferior rectus transposition in addition to LR recession with Y-split has vastly improved the management outcomes, providing not only primary position orthophoria but also increased binocular visual fields as well.
Keywords: Duane retraction syndrome, restrictive strabismus, strabismus surgery
Duane retraction syndrome (DRS) is a congenital complex strabismus. This condition was first described by Stilling in 1887. However, it was later made popular by Alexander Duane who published a series of 54 patients having this condition. The frequency of this syndrome in the general population of strabismus patients is 1–4%.[1] This disease has a female preponderance with about 60% of affected individuals being females.[2] About 80% of cases are unilateral with a predominance of the left eye being affected.[3] DRS is included in a group of disorders called congenital cranial dysinnervation disorders.[4] These disorders can have a varied presentation which is caused by either primary or secondary dysinnervation.
Etiopathogenesis
A maldevelopment due to any insult to the development of the sixth nerve nucleus/nerve at 4–8 weeks of gestation has been shown to be the causative factor in the development of this disease process.[5] The branches of the third nerve, in turn, are redirected to the lateral rectus (LR). This abnormal or paradoxical innervational impulse to the horizontal recti is the basic pathology of this disease. The LR may exhibit a spectrum of abnormal innervational pattern ranging from paradoxical to the subnormal innervation. In some cases, even the medial rectus (MR) may have subnormal innervations owing to the redirection of developing nerve fibers to the sixth nerve. Secondary muscle changes may occur in the form of contracture and subsequent fibrosis of MR and superior rectus as a result of constant esotropia and upshoots, respectively.
Clinical Features and Diagnosis
The diagnosis of DRS is usually clinical. Molecular genetic testing is being investigated for this disease; however, it remains in infancy. It involves single gene testing using sequential and deletion/duplication analysis of the CHN1 gene[6] which is known to cause isolated familial DRS, and more genes which are also being identified. This disease has been differentiated into three subtypes on the basis of myography by Huber.[7] Apart from these, it can also be classified on the basis of the primary position deviation into eso-DRS, exo-DRS, and ortho-DRS.[8] This classification is easier to use for surgical planning.[9] High-definition magnetic resonance imaging has shown the absence of abducens nerve/nucleus in many studies as well as secondary changes in the extraocular muscles.[10,11]
DRS is characterized by the limitation of abduction and/or adduction along with a narrowing of palpebral aperture and retraction of the globe and variable upshoot and downshoot of the globe on attempted adduction. The patients may also have a face turn to achieve binocularity.
Other ocular findings may include nystagmus, anisocoria, ptosis, epibulbar dermoid, congenital cataract, heterochromia, and optic nerve hypoplasia. DRS has also been shown to be associated with gustatory lacrimal reflex or crocodile tears. The clinical features may vary from case to case and one may see a myriad of presentations. About 30% of cases of DRS are associated with congenital syndromes. Among the isolated cases of DRS, 90% are sporadic, whereas the remaining 10% are inherited. Several syndromic associations of DRS have been noted out of which the most common ones include Goldenhar syndrome, Wildervanck syndrome, spalt like transcription factor 4 (SALL4)-related syndromes, spalt like transcription factor 1 (SALL1)-related syndromes, and homeobox A1 (HOXA1)-related disorders.[6] Genetic basis of DRS is being explored in detail and in future it may play a bigger role in its management.
Major differentials of this condition include sixth nerve palsy, Moebius syndrome, infantile esotropia, and congenital oculomotor apraxia. At the outset, the most characteristic feature of a DRS (or any restrictive strabismus) is the minimal ocular deviation vis-a-vis the marked limitation of abduction; paralytic strabismus would have both in a commensurate degree. A simple patch test can rule out the presence of infantile esotropia as it may have minimal limitation of abduction which would also reduce after patching. Moreover, these conditions can be ruled out on the basis of the absence of characteristics like globe retraction, narrowing of the palpebral aperture on attempted adduction, and upshoots or downshoots.
The role of evaluating for associated refractive errors especially anisometropic amblyopia and treating it cannot be overemphasized to restore full binocularity, which is mostly preserved with anomalous head posture.
Surgical Management
The primary indication for surgery in DRS is the correction of primary position deviation and anomalous face turn. Apart from this, surgery can also be done to ward off cosmetically unacceptable globe retraction and upshoots or downshoots, which are present as a result of severe co-contraction of LR and MR on attempted adduction. While planning surgery, it is important to look for any contracture/fibrosis in medial rectus and LR by doing forced duction tests (FDTs). The presence of anomalous LR activity can be detected with the help of force degeneration test of Romero-Apis. This test is extremely useful in confirming LR innervation during adduction and the missing LR innervation on abduction and thus helps in deciding the plan of surgery. If binocular vision is present with cosmetically acceptable ocular appearance and not much of co-contraction, surgery must not be undertaken just for improving the abduction limitation.
Eso-DRS
Classically, eso-DRS cases do not have normal LR function, but anomalous LR action occurs during adduction. These patients have an esodeviation in the primary position and as a result, they assume a corrective face turn. Before planning any surgery in DRS, it is imperative to check FDT to rule out MR contracture in the affected eye. A tight MR should always be recessed, but only minimally as per the tightness of MR because a little more MR recession may induce synergistic divergence, limited adduction, and exotropia in adduction. In cases with minimal anomalous LR activity and normal LR abducting force, a small MR recession in the affected eye may suffice.[12,13] A single MR recession has been done in the affected eye in case of deviations less the 20 prism diopters (PD) [Fig. 1]. Those with anomalous LR activity should be tackled by LR weakening procedures with Y-splitting in addition.
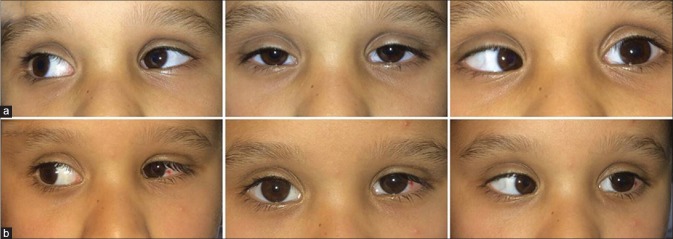
Figure 1.
(a) Preoperative photograph of a patient with left eye eso-DRS. The patient underwent MR recession in the affected eye leading to orthophoria in the postoperative period, corrected downshoot, but has some adduction deficit (b)
If the MR is not tight and the co-contraction is minimal or mild, one may do just superior rectus transposition (SRT) or inferior rectus transposition (IRT) or partial vertical rectus transpositions (pVRTs). Other treatment options include asymmetric bilateral MR recessions.[14] This is especially suited if the esodeviation is large and the MR tightness on FDT is minimal. Asymmetric, larger MR recession done in the good (fellow eye) to produce a fixation duress not only corrects the primary position esotropia but also decreases the likelihood of contracture of the MR in the affected eye. The fixation duress in the good eye leads to a continuous inhibition of the affected eye's MR. One must never resect LR in the involved eye, although it has been described in an odd case.[15]
In cases with significant upshoot or downshoot, the co-contraction needs to be countered by the recession of ipsilateral LR with a Y-split[16] in addition to the tight MR of the affected eye. In this procedure, the LR is split from its insertion to 18–20 mm posteriorly and the two halves are placed at a distance of 20–22 mm apart. A recession LR of 6–7 mm is usually required partly to reduce the increased tension due to stretch by Y-split and also to reduce the retraction due to co-contraction. This procedure has been shown to be effective in tackling severe upshoot and downshoot.
The abduction deficit can be tackled by transposition procedures like SRT[17,18] [Fig. 2] or a VRT to LR,[19] if there is no significant anomalous LR recruitment causing co-contraction. It has been found that the combination of SRT and MR recession is more effective than MR recession or bilateral MR recession at improving abduction while allowing for a smaller recession to obtain alignment.[17] However, in cases with uncorrected, severe, anomalous LR recruitment, transposition procedures are not indicated as they may worsen adduction, retraction, and vertical offshoots. Moreover, in case the MR and LR are both to be operated, adding the SRT or even partial VRT is fraught with the danger of anterior segment ischemia.[20] In cases where the affected eye is the fixing eye, surgery should be performed in the affected fixing eye to ward off the large secondary deviations that occur in non-fixing eye. We generally prefer a “balanced” partial VRT to SRT as the latter has a risk of vertical incomitance and inducing torsion.[21] Velez et al.[22] have suggested doing SRT in cases with preoperative hypotropia, inferior recti transposition in preoperative hypertropia, and pVRT in case of no preoperative vertical deviations. In patients with residual esotropia after undergoing VRT and having a negative FDT, one must explore the transposed muscles to look for their migration or slippage.[23] Fig. 3 summarizes the management protocol for eso-DRS.
Figure 2.
(a) Abduction deficit in a patient with left eso-DRS successfully managed by SRT alone (b)
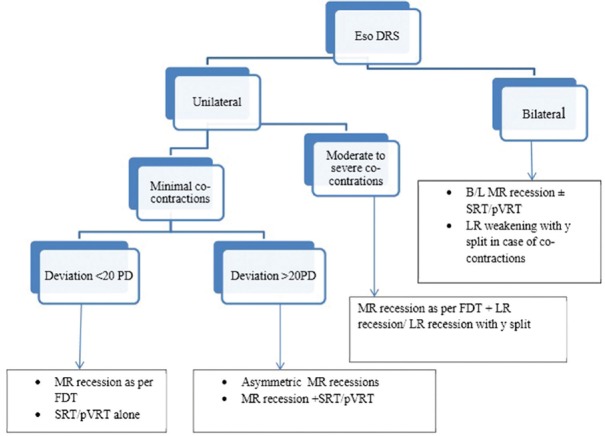
Figure 3.
Flow diagram summarizing management of eso-DRS
Exo-DRS
Exo-DRS patients present with a primary position exotropia and may have significant upshoots and/or downshoots along with retraction on adduction. Such patients can be tackled by LR recession with Y-split or a supramaximal LR recession or a PF of LR. An LR recession with Y-split is the preferred option in cases with normal LR activity during abduction, and the exotropia and upshoots and downshoots are the problems [Fig. 4]. It may be noted that the LR recession should be substantial to correct the retraction in adduction, as the Y-split per se does not affect the retraction (in fact induces a stretch in LR due to Y-split). When the exotropia is large with no normal LR activity during abduction LR, PF is preferred. In cases where supramaximal recession or LR PF fails to redress the exodeviation fully, LR of the normal eye can also be recessed to achieve successful outcome [Fig. 5]. The PF wards off the anomalous LR activity most substantially. Some authors have even suggested extirpation of the LR.[24,25] The resultant lack of abduction can be taken care of by VRT procedures to LR. In a study done at our centre, it was seen that a standalone PF may lead to consecutive esodeviation in a few cases.[26] Such cases can be corrected with the help of transposition procedure like partial VRT [Fig. 6]. The study also showed LR PF to be an effective surgery to correct exodeviation, anomalous head posture, and improving adduction in exo-DRS and partial VRT in addition to be effective in improving abduction and binocular single visual field. Fig. 7 summarizes the management protocol for exo-DRS.
Figure 4.
(a) Severe upshoots in a patient with left exo-DRS managed effectively by left LR recession with Y-split (b)
Figure 5.
(a) Preoperative photograph of a patient with left eye exo-DRS. The patient underwent supramaximal LR recession (15 mm) in the affected eye leading to the improvement in exodeviation but sill a residual exotropia was present (b) which was corrected by LR recession in the other eye leading to orthophoria (c)
Figure 6.
(a) Consecutive esotropia in a patient with exo-DRS managed with PF earlier, which was managed successfully by pVRT leading to improved abduction, but has residual upshoot in adduction (b)
Figure 7.
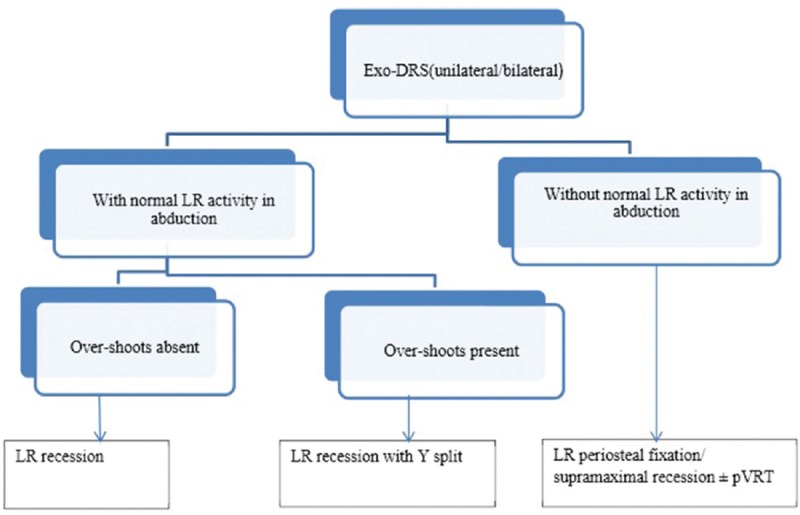
Flow diagram summarizing management of exo-DRS
Ortho-DRS
These patients are orthophoric in the primary position. These patients however present with retraction, palpebral aperture narrowing, and upshoots and/or downshoots on adduction, which may be cosmetically very disfiguring. The treatment in such cases may lead to a consecutive heterotropia as such should be tackled only by the experienced surgeons. We suggest managing such patients by equitable recession of both lateral rectus and MR in the affected eye in the presence of co-contractions with the use of adjustable surgery on MR and Y-split on LR to control the risk of undesirable under or over corrections [Fig. 8].
Figure 8.
(a) Preoperative clinical photograph of a patient having ortho-DRS with upshoot managed successfully with medial rectus recession and lateral rectus recession with Y-split (b)
Bilateral DRS
Bilateral DRS is seen in 15% of cases and most of them are either eso- or ortho-DRS.[27] This disease may present as an asymmetric entity as well. In patients with bilateral DRS with fusion, the eyes may be aligned in primary position with straight head or there may be the presence of deviation along with head posture. In these cases, all four horizontal recti need to be recessed depending on the deviation in primary position.[28] These can be managed on the basis of similar principles as the unilateral cases. These cases are treated as unilateral DRS and balancing of MR and LR forces is done depending on the deviation governed by the dominant eye. Bilateral eso-DRS can be managed by bilateral MR recessions[29] but being handled as per FDT and preferably one MR on adjustable procedure [Fig. 9]. Bilateral exo-DRS is quite rare and bilateral LR recessions have been recommended for its management. LR Y-split can be added in cases with marked upshoots.
Figure 9.
(a) Preoperative clinical photograph of a patient having bilateral eso-DRS managed successfully with bilateral MR recessions (b)
Conclusion
As a result of its varied clinical presentation, the treatment of DRS should be individualized for the patients. With the advent of newer transposition techniques, the surgical outcomes have improved. These newer techniques help in achieving deviation-free primary position, ensure the improvement in the binocular field of vision, and also improve abductions. One must remember to follow the simple prescription for strabismus management, that is, observation, confirmation, inference, planning, and finally execution to achieve or restore stereopsis.[30]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane's retraction syndrome. Surv Ophthalmol. 1993;38:257–88. doi: 10.1016/0039-6257(93)90077-k. [DOI] [PubMed] [Google Scholar]
- 2.O’Malley ER, Helveston EM, Ellis FD. Duane's retraction syndrome-plus. J Pediatr Ophthalmol Strabismus. 1982;19:161–5. doi: 10.3928/0191-3913-19820501-11. [DOI] [PubMed] [Google Scholar]
- 3.Pfaffenbach DD, Cross HE, Kearns TP. Congenital anomalies in Duane's retraction syndrome. Arch Ophthalmol. 1972;88:635–9. doi: 10.1001/archopht.1972.01000030637013. [DOI] [PubMed] [Google Scholar]
- 4.Bosley TM, Abu-Amero KK, Oystreck DT. Congenital cranial dysinnervation disorders: A concept in evolution. Curr Opin Ophthalmol. 2013;24:398–406. doi: 10.1097/ICU.0b013e3283645ad6. [DOI] [PubMed] [Google Scholar]
- 5.Hoyt WF, Nachtigäller H. Anomalies of ocular motor nerves. Neuroanatomic correlates of paradoxical innervation in Duane's syndrome and related congenital ocular motor disorders. Am J Ophthalmol. 1965;60:443–8. [PubMed] [Google Scholar]
- 6.Andrews CV, Hunter DG, Engle EC. Duane syndrome. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, editors. GeneReviews®. Seattle (WA): University of Washington; 1993. [Last accessed on 2018 Jun 05]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1190/ [Google Scholar]
- 7.Huber A. Electrophysiology of the retraction syndromes. Br J Ophthalmol. 1974;58:293–300. doi: 10.1136/bjo.58.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahluwalia BK, Gupta NC, Goel SR, Khurana AK. Study of Duane's retraction syndrome. Acta Ophthalmol (Copenh) 1988;66:728–30. doi: 10.1111/j.1755-3768.1988.tb04071.x. [DOI] [PubMed] [Google Scholar]
- 9.Akbari MR, Manouchehri V, Mirmohammadsadeghi A. Surgical treatment of Duane retraction syndrome. J Curr Ophthalmol. 2017;29:248–57. doi: 10.1016/j.joco.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta C, Sharma P, Saxena R, Garg A, Sharma S. Clinical correlation of imaging findings in congenital cranial dysinnervation disorders involving abducens nerve. Indian J Ophthalmol. 2017;65:155–9. doi: 10.4103/ijo.IJO_1013_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yonghong J, Kanxing Z, Zhenchang W, Xiao W, Xuehan Q, Fengyuan M, et al. Detailed magnetic resonance imaging findings of the ocular motor nerves in Duane's retraction syndrome. J Pediatr Ophthalmol Strabismus. 2009;46:278–85. doi: 10.3928/01913913-20090903-05. [DOI] [PubMed] [Google Scholar]
- 12.Natan K, Traboulsi EI. Unilateral rectus muscle recession in the treatment of Duane syndrome. J AAPOS. 2012;16:145–9. doi: 10.1016/j.jaapos.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 13.Sharma P. Unilateral rectus muscle recession in the treatment of Duane syndrome. J AAPOS. 2012;16:492–3. doi: 10.1016/j.jaapos.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Dotan G, Klein A, Ela-Dalman N, Shulman S, Stolovitch C. The efficacy of asymmetric bilateral medial rectus muscle recession surgery in unilateral, esotropic, type 1 Duane syndrome. J AAPOS. 2012;16:543–7. doi: 10.1016/j.jaapos.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Kraft SP. Lateral rectus resection strabismus surgery in unilateral Duane syndrome with esotropia and limited abduction. Binocul Vis Strabismus Q. 2010;25:149–57. [PubMed] [Google Scholar]
- 16.Farid MF. Y-split recession vs. isolated recession of the lateral rectus muscle in the treatment of vertical shooting in exotropic Duane retraction syndrome. Eur J Ophthalmol. 2016;26:523–8. doi: 10.5301/ejo.5000746. [DOI] [PubMed] [Google Scholar]
- 17.Yang S, MacKinnon S, Dagi LR, Hunter DG. Superior rectus transposition vs. medial rectus recession for treatment of esotropic Duane syndrome. JAMA Ophthalmol. 2014;132:669–75. doi: 10.1001/jamaophthalmol.2014.358. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal R, Sharma M, Saxena R, Sharma P. Surgical outcome of superior rectus transposition in esotropic Duane syndrome and abducens nerve palsy. J AAPOS. 2018;22:12–60. doi: 10.1016/j.jaapos.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Molarte AB, Rosenbaum AL. Vertical rectus muscle transposition surgery for Duane's syndrome. J Pediatr Ophthalmol Strabismus. 1990;27:171–7. doi: 10.3928/0191-3913-19900701-03. [DOI] [PubMed] [Google Scholar]
- 20.Göçmen ES, Atalay Y, Evren Kemer Ö, Sarıkatipoğlu HY. Anterior segment ischemia after strabismus surgery. Turk J Ophthalmol. 2017;47:47–51. doi: 10.4274/tjo.93824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Özkan SB. Pearls and pitfalls in the management of Duane syndrome. Taiwan J Ophthalmol. 2017;7:3–11. doi: 10.4103/tjo.tjo_20_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velez FG, Chang MY, Pineles SL. Inferior rectus transposition: A novel procedure for abducens palsy. Am J Ophthalmol. 2017;177:126–30. doi: 10.1016/j.ajo.2017.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kekunnaya R, Negalur M. Duane retraction syndrome: Causes, effects and management strategies. Clin Ophthalmol. 2017;11:1917–30. doi: 10.2147/OPTH.S127481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velez FG, Thacker N, Britt MT, Alcorn D, Foster RS, Rosenbaum AL, et al. Rectus muscle orbital wall fixation: A reversible profound weakening procedure. J AAPOS. 2004;8:473–80. doi: 10.1016/j.jaapos.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Carlson MR, Jampolsky A. An adjustable transposition procedure for abduction deficiencies. Am J Ophthalmol. 1979;87:382–7. doi: 10.1016/0002-9394(79)90081-3. [DOI] [PubMed] [Google Scholar]
- 26.Sharma P, Tomer R, Menon V, Saxena R, Sharma A. Evaluation of periosteal fixation of lateral rectus and partial VRT for cases of exotropic Duane retraction syndrome. Indian J Ophthalmol. 2014;62:204–8. doi: 10.4103/0301-4738.121145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kekunnaya R, Kraft S, Rao VB, Velez FG, Sachdeva V, Hunter DG, et al. Surgical management of strabismus in Duane retraction syndrome. J AAPOS. 2015;19:63–9. doi: 10.1016/j.jaapos.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 28.Goldstein JH, Sacks DB. Bilateral Duane's syndrome. J Pediatr Ophthalmol. 1977;14:12–7. [PubMed] [Google Scholar]
- 29.Sachdeva V, Kekunnaya R, Gupta A, Bhoompally VR. Surgical management of bilateral esotropic Duane syndrome. J AAPOS. 2012;16:445–8. doi: 10.1016/j.jaapos.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Sharma P. The pursuit of stereopsis. J AAPOS. 2018;22:2.e1–2.e5. doi: 10.1016/j.jaapos.2017.10.009. [DOI] [PubMed] [Google Scholar]