This brief communication highlights an online patient portal allowing patients direct access to outpatient visit notes written by their providers. Physicians' perceptions of sharing visit notes were collected and assessed via questionnaire.
Abstract
In a large survey (n = 809) conducted to understand how oncologists differ from nononcologists regarding routinely sharing visit notes with patients, oncologists were less likely to agree patient safety would improve (p = .03) or that patients would be offended after reading notes (p = .01); however, they agreed with nononcologists that sharing notes would lead to less candid documentation (69% vs. 73%; p = .39). Oncologists share a high level of worry about the impact of sharing notes on documentation practices, a concern that will need to be addressed as the practice of sharing visit notes expands to cancer care.
The Health Insurance Portability and Accountability Act of 1996 mandated that patients have the right to access their medical records. Patient portals, secure online websites connected to the electronic health record (EHR), provide patients with electronic access to their health record, including appointment schedules, medication lists, lab results, and, as of 2010, visit notes.
The OpenNotes project was launched in 2010 at three health systems in the U.S., leveraging the patient portal function to grant access to primary care outpatient visit notes [1]. Many of the 105 primary care physicians surveyed anticipated disruption in workflow and need to modify notes, whereas others expected improved patient satisfaction and safer patient care as a result of OpenNotes [2]. We aimed to characterize the perceptions of oncologists versus nononcologists in a different U.S. health system outside of the OpenNotes project and identify barriers to implementation, conducting a new survey of provider perceptions prior to launch of a shared notes system.
On January 10, 2017, the Brigham and Women's Hospital and the Dana‐Farber Cancer Institute, located in Boston, which share an EHR, launched a new feature of their secure online patient portal allowing direct access to outpatient visit notes. All providers were trained on the process of sharing outpatient visit notes with patients at least 1 month prior to launch and were able to disable sharing for any specific visit. Between January 5, 2017, and January 27, 2017, 1,616 eligible providers (309 oncologists, 1,307 nononcologists) were sent an email linked to the online survey to assess perceptions of routinely sharing visit notes. The questionnaire was adapted from the OpenNotes physician survey [2], modified to reflect concerns of specialty providers (e.g., replacing “illness” with “cancer” for oncologists). The final provider survey resulted from iterative review following cognitive debriefing, reaching saturation following six provider interviews. The anonymous provider survey was determined to be exempt from institutional review board review (45 CFR 46; category 2).
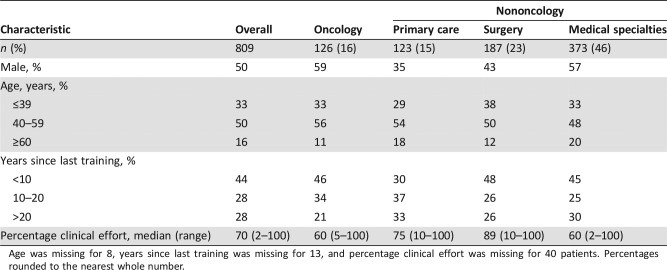
Specialties were categorized as either oncology (medical oncology and radiation oncology) or nononcology (primary care [family practice and internal medicine], surgical specialties [general surgery and surgical specialties], and medical specialties [infectious disease, cardiology, pulmonology, gastroenterology, endocrinology, nephrology, neurology, and all others]) (Table 1). Eligible providers included all physicians and physician assistants with an active email address during the survey period. Of those, 809 responded (126 oncologists [16%] and 683 nononcologists [84%]), yielding an overall response rate of 50% (56% for oncologists and 49% for nononcologists).
Table 1. Characteristics of participating providers.
Age was missing for 8, years since last training was missing for 13, and percentage clinical effort was missing for 40 patients. Percentages rounded to the nearest whole number.
Prior to open notes, oncologists reported sharing visit notes with 12% of their patients, similar to 17% for nononcologists. Oncologists planned not to share visit notes with a median of 10% of their patient panel, less than nononcologists (20%; p = .06). Both oncologists and nononcologists anticipated that a median 50% of their patient panel would review visit notes via the patient portal.
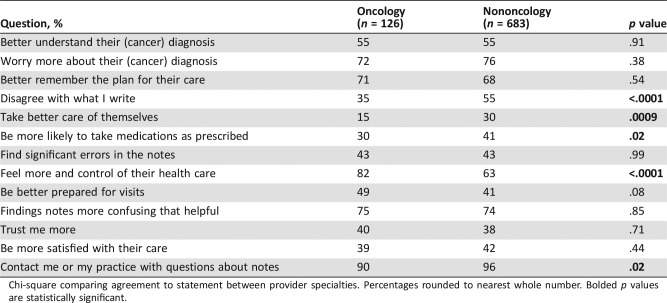
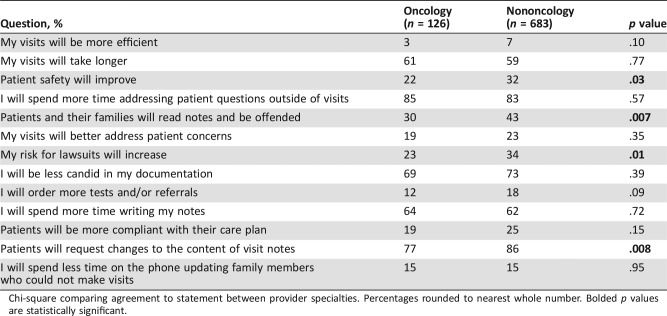
Both groups reported documentation for their own reference (95%) or another provider's reference (97%) as a more important purpose of visit notes, whereas documentation for the patients’ reference was viewed as a less important purpose (69% oncologists vs. 60% nononcologists; p = .04). Most oncologists and nononcologists felt that patients would better understand their diagnosis (both 55%) and better remember their plan of care (68% and 71%) (Table 2). About 4 out of 10 providers felt that patients would trust them more, be more satisfied with their care, and be more likely to take medications as prescribed. Oncologists were less likely to feel that patient safety would improve (22% vs. 31%; p = .03), that patients who read notes would be offended (30% vs. 43%; p = .007), or that risks for lawsuits would increase (23% vs. 34%; p < .01) (Table 3).
Table 2. Expected impact of open notes on clinical care, by specialty.
Chi‐square comparing agreement to statement between provider specialties. Percentages rounded to nearest whole number. Bolded p values are statistically significant.
Table 3. Expected impact of open notes on clinical practice, by specialty.
Chi‐square comparing agreement to statement between provider specialties. Percentages rounded to nearest whole number. Bolded p values are statistically significant.
Fewer oncologists than nononcologists reported concern that patients would disagree with what they wrote (35% vs. 55%; p < .0001). Most respondents were concerned that patients would contact them or their practice or request changes (90% oncologists vs. 96% nononcologists; p = .02). Most felt that they would spend more time writing notes, and more than two thirds reported they would be less candid in their documentation.
In this preimplementation assessment of provider receptiveness to sharing visit notes with patients, we found that oncologists were overall positive about sharing visit notes, but differed in their impressions from other specialists in several ways. Oncologists were more likely to feel that open notes would result in patients having a better understanding of their diagnoses, but less likely to feel that patient safety would improve. Oncologists were less likely than other specialists to agree that patients would be offended after reading notes, or that they would request changes, although a majority expected that this would occur. Finally, along with nononcologists, a large majority of oncologists felt that, knowing patients could easily read their notes, they would be less candid in their documentation.
Similar to the initial perceptions of open notes among primary care physicians [3], only a minority of oncologists in our study felt that the purpose of visit notes is to communicate with patients. This finding, along with the fact that a large majority felt they would need to change the content of notes to be shared with patients, is a concern that will need to be addressed as open notes expand to cancer care. A striking contrast to other providers was oncologists’ perceptions regarding the impact of sharing notes on patient safety, with only 22% agreeing this would improve versus 32% for nononcologists (p = .03).
We acknowledge that providers are only half of the open notes equation [4], [5], and future work will need to focus on the perceptions of patients themselves in the context of the different specialists they see. Our survey was conducted in two hospitals from one large academic health system in the U.S., limiting generalizability to community providers and/or those who practice in countries with single‐payer systems. Our analysis suggests that oncologists are open to providing direct electronic access to visit notes; implementers should engage oncologists to ensure that cancer‐specific benefits and concerns are addressed. Our data also suggest that we should carefully examine opportunities as well as unintended consequences, particularly the risk of less candid documentation, arising from implementation of open notes in cancer care.
Disclosures
The authors indicated no financial relationships.
References
- 1.Leveille SG, Walker J, Ralston JD et al. Evaluating the impact of patients' online access to doctors' visit notes: Designing and executing the OpenNotes project. BMC Med Inform Decis Mak 2012;12:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delbanco T, Walker J, Bell SK et al. Inviting patients to read their doctors' notes: A quasi‐experimental study and a look ahead. Ann Intern Med 2012;157:461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delbanco T, Walker J, Darer JD et al: Open notes: Doctors and patients signing on. Ann Intern Med 2010;153:121–125. [DOI] [PubMed] [Google Scholar]
- 4.Vodicka E, Mejilla R, Leveille SG et al. Online access to doctors' notes: Patient concerns about privacy. J Med Internet Res 2013;15:e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright E, Darer J, Tang X et al. Sharing physician notes through an electronic portal is associated with improved medication adherence: Quasi‐experimental study. J Med Internet Res 2015;17:e226. [DOI] [PMC free article] [PubMed] [Google Scholar]