Supplemental digital content is available in the text.
Abstract
Background
Deceased-donor kidney discard rates vary by region, but it is unknown whether discard rates and transplant outcomes vary during the American Transplant Congress (ATC) each year.
Methods
Using national registry data, we determined rates of kidney discard, delayed graft function, graft failure, and mortality from December 31, 1999, through December 30, 2015, during ATC dates and compared these rates with those on the same days of the week during the 2 weeks before and after the ATC (non-ATC). We used multivariable regression to determine associations between ATC and these outcomes.
Results
From 7902 donors (1575 ATC; 6327 non-ATC), 12 588 recipients received kidney transplants (2455 ATC; 10 133 non-ATC), and 2666 kidneys were discarded (582 ATC; 2084 non-ATC). Kidneys were more often discarded during ATC (19% vs 17%, P = 0.006; adjusted odds ratio, 1.21; 95% confidence interval, 1.05-1.40). There were no significant differences in donor, transplant, or recipient characteristics by ATC/non-ATC dates or by ATC/non-ATC transplant dates for delayed graft function, graft failure, or mortality.
Conclusions
On the basis of a 21% increased odds of discard, the ATC itself may result in 5 additional kidney discards during this important conference every year, which suggests the need for innovative staffing or other logistic solutions during these planned meetings.
The American Transplant Congress (ATC) is the primary annual transplant conference in the United States. Thousands of physicians, surgeons, coordinators, nurses, and additional professional staff who work in transplant medicine attend this conference every year. In transplant, important decisions are made and high-risk procedures are performed daily. With primary physicians and other staff away during the meeting, transplant centers and patients could be negatively impacted. Kidney discard rates could also be indirectly affected during these conferences. Currently, more than 5000 persons die yearly waiting for kidney transplants, and nearly 2700 kidneys are discarded every year.1
Outcomes of transplant procedures, including discard rates, are unknown during the dates of the ATC conference. Some studies have shown that patients have worse outcomes during weekends, especially for urgent operations or interventions,2-4 although recent data from the United Kingdom revealed no differences in short-term or one-year outcomes for weekend compared with weekday transplants.5 However, Mohan et al6 found 13% increased adjusted odds for discard for deceased-donor kidneys procured during weekends.
We studied the rates of discard, delayed graft function (DGF), allograft failure, and recipient mortality for transplants performed during ATC conferences. We hypothesized that there would be increased discard and DGF rates during the conferences.
MATERIALS AND METHODS
Patient Data
To obtain data for this retrospective, observational study, we queried the Scientific Registry of Transplant Recipients (SRTR) database, which includes data for all donors, wait-listed candidates, and transplant recipients in the United States. The data primarily come from members of the Organ Procurement and Transplantation Network (OPTN), which has been described elsewhere.7 The study protocol was reviewed by the University of Utah Institutional Review Board and was declared exempt because of the use of preexisting, deidentified data from the OPTN.
Study Design
Scientific Registry of Transplant Recipients data from 2000 through 2015 for the exact dates of the ATC conferences were used for this study. Donors were defined as having at least one kidney procured for the purpose of transplant. We constructed the cohort using transplant/discard dates shifted by 1 day earlier to account for the fact that deceased-donor kidneys are typically procured one calendar day before they are transplanted or discarded (ie, December 31, 1999, through December 30, 2015). We then reviewed the rates of kidney discards, DGF (defined as any dialysis during the first week of transplant), allograft failure (defined as recipient death, return to chronic dialysis or retransplantation), recipient mortality, and death-censored allograft failure. To control for annual ATC meetings that occurred on different days of the week and for varying numbers of days, these rates were compared with those on the same days of the week during the 2 weeks before and after each ATC (non-ATC). We controlled for donor sex and the 10 characteristics that comprise the Kidney Donor Risk Index (KDRI) to determine associations between ATC and the outcomes listed above.
Statistical Analysis
Descriptive statistics for baseline donor or recipient characteristics were reported as means (standard deviations) or medians (25th and 75th percentiles) for numeric variables and as numbers and proportions for categorical variables. We compared donor and recipient characteristics between ATC and non-ATC groups by t tests for numeric variables and a χ2 test or Fisher exact test if appropriate for categorical variables. Skewed variables (eg, serum creatinine) were compared by nonparametric equality-of-medians tests.8 We also compared the rates for kidney discard and DGF between ATC and non-ATC groups by χ2 tests.
We then compared donor characteristics between ATC and non-ATC groups, specifically for the subset of kidneys that were discarded. To determine whether these and other factors were associated with kidney discard within the entire cohort, the data were fit via a generalized estimating equation (GEE) model using a robust standard error estimation with a log-link function and binary distribution for the dependent variable. Separate models were applied for ATC, donor sex, and the 10 donor characteristics that comprise the KDRI (age, race, weight, height, history of hypertension, history of diabetes, terminal serum creatinine, cerebrovascular accident as cause of death, donation after cardiovascular determination of death, and hepatitis C virus serostatus). The multivariable GEE model was then used to estimate the independent effect of ATC by controlling for these characteristics.
The number of additional kidney discards due to ATC was estimated using a counterfactual framework, which determines the average difference in discarded kidneys recovered during ATC had they instead been recovered during the non-ATC timeframe. We performed the counterfactual analysis based on the following steps. First, we fit a multivariable GEE model for all donors, combining both ATC and non-ATC groups. Second, we generated a counterfactual non-ATC group by switching all ATC donors to non-ATC while maintaining all other covariates unchanged. Third, we noted the expected probability of kidney discard for each donor in the ATC group and the counterfactual non-ATC group based on the fitted regression model from the first step. Fourth, we calculated the number of kidney discards by summing the expected probability for the ATC and counterfactual non-ATC groups separately. Finally, we subtracted the non-ATC discard counts from the ATC counts for each year.
We then used separate multivariable proportional hazards regression models to determine potential independent ATC effects on time to allograft failure, recipient mortality, and death-censored allograft failure. We also performed a post hoc analysis of the total number of kidneys transplanted by each center throughout the study period (ATC plus non-ATC timeframes) in relation to the percentage of those transplants performed during ATC. For all statistical tests, we controlled for possible correlation of outcomes between kidneys from the same donor and used 2-tailed significance values less than 0.05. All analyses were performed using STATA, version MP 14.0, software (StataCorp LLC, College Station, TX) or SAS, version 9.4, software (SAS Institute Inc, Cary, NC).
RESULTS
During the timeframes studied (ATC and non-ATC), 7902 deceased donors became available: 1575 during ATC meetings and 6327 during the non-ATC timeframe. Tables 1A and 1B show that there were no significant between-group differences in donor, recipient, or transplant characteristics; however, donors during ATC meetings were more likely to have had 1 or both kidneys discarded (P = 0.002). Of the 15 285 kidneys that were procured, 2666 were discarded: 582 (19%) during ATC meetings and 2084 (17%) during the non-ATC timeframe (P = 0.006). There were 12 588 kidney recipients: 2455 during ATC meetings and 10 133 during the non-ATC timeframe. There was also no significant difference between ATC groups for the development of DGF (Table 1).
TABLE 1A.
Donor characteristics (N = 7902)
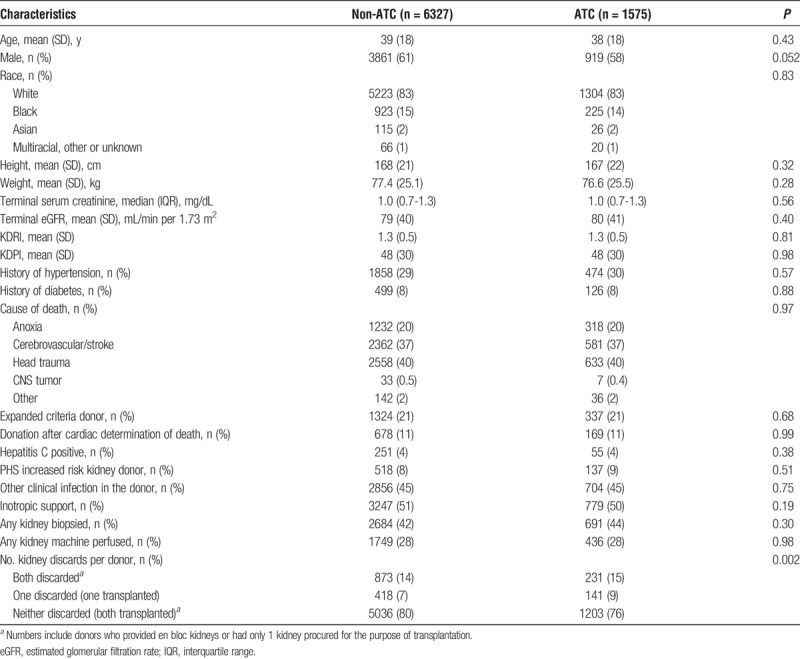
TABLE 1B.
Individual kidney, transplant, and recipient characteristics
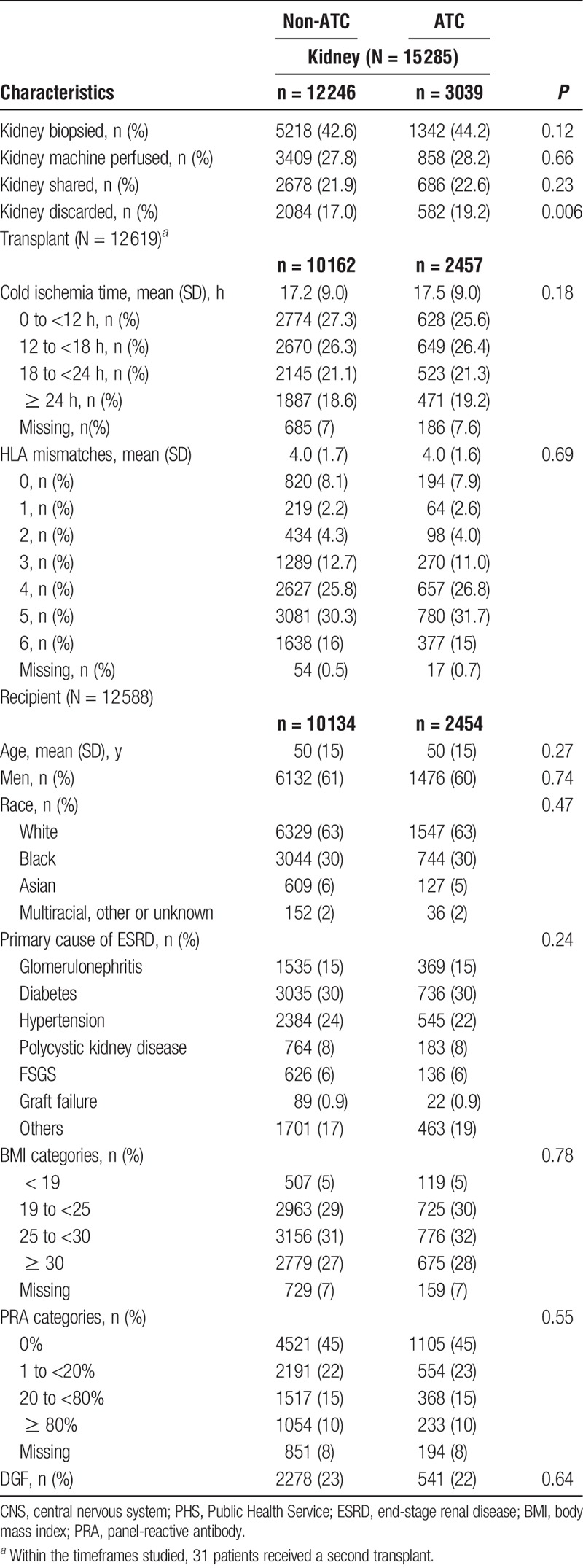
Table S1 (http://links.lww.com/TXD/A154) provides donor characteristics by ATC timeframes, specifically for discarded kidneys. Compared with the kidneys discarded during the non-ATC timeframe, the kidneys that were discarded during ATC meetings were more likely to be from female donors (47% vs 52%, P = 0.01) and to have undergone machine perfusion (24% vs 29%, P = 0.03). Based on KDRI values, however, overall quality of the discarded kidneys was similar for the two timeframes (1.8 ± 0.5 for non-ATC vs 1.8 ± 0.6 for ATC, P = 0.19).
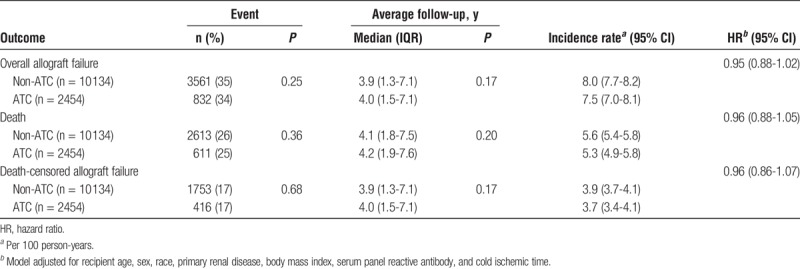
Univariate analyses for kidney discard in the full cohort showed that all 10 donor variables that comprise the KDRI, as well as procurement during ATC meetings, were significantly associated with kidney discard (Table 2). With multivariable adjustment, donation during ATC meetings remained independently associated with kidney discard with an adjusted odds ratio of 1.21 (95% confidence interval, 1.05-1.4). Using counterfactual analysis on the basis of this 21% increased odds of discard, an estimated 5 additional kidneys may be discarded each year during the ATC meeting. There were no significant between-group differences in allograft failure, recipient mortality, or death-censored allograft failure (Table 3).
TABLE 2.
Associations for donor characteristics with kidney discard
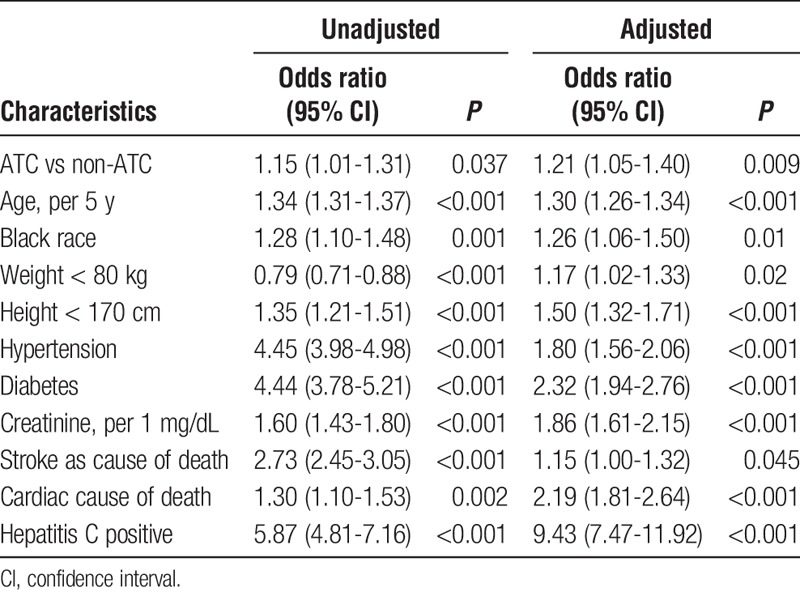
TABLE 3.
Recipient outcomes after the first week of transplant
By study design, the ATC timeframe was one-fifth of the study period (non-ATC represented four-fifths). Thus, 20% of the transplants would be expected to have occurred during ATC. Via post hoc analysis, 34 centers performed zero transplants during ATC meetings. All of these centers performed fewer than 50 total transplants during the study period, but as shown in Figure S1 (http://links.lww.com/TXD/A155), there were also many relatively small centers (in terms of total transplants) that performed much more than the expected 20% of transplants during the ATC timeframe. The statistical trend was flat and close to the expected 20% rate, however, suggesting no significant relationship between center size and ATC transplantation rate.
DISCUSSION
In this large, retrospective study of the SRTR database, we calculated the direct effects that ATC meetings may have had on kidney transplantation outcomes in the United States. Although no differences existed in the rates of DGF, allograft survival, or recipient mortality for transplanted kidneys, we found 21% increased odds of discard for the kidneys procured during the ATC compared with kidneys procured the same days of the week for the 2 weeks before and after the conferences.
Transplant centers have different procedures for accepting deceased-donor kidney allografts, but, in most cases, acceptance is determined by surgeon experience, especially if the donor is considered high risk. Additional highly trained personnel (ie, transplant nurse coordinators) are also frequently required to initially evaluate kidney offers. These clinical staff members must work efficiently to review all of the information necessary to complete the evaluation quickly. Time is also limited during kidney offers to evaluate the intended recipient for any acute symptoms that could cause procedural complications. Decisions about kidney offers could be impacted during ATC conferences because of limited staffing while center personnel attend the meetings.
In addition to potentially affecting kidney offer decisions, limited staffing during ATC conferences could affect immediate postoperative care for kidney transplant recipients, especially high-risk patients receiving kidneys from high-risk donors. Such concerns might even impact a transplant center's willingness to accept high-risk donor allografts in settings of limited staffing. However, we found no associations with important posttransplant outcomes, and we noted similar kidney quality (based on KDRI) for discarded kidneys between timeframes. Nonetheless, our finding of 21% increased odds for discard during ATC can be compared with the 13% increased odds for discard on weekends as reported by Mohan et al.6
Interestingly, Mohan et al6 also noted that kidneys procured and discarded during weekends tended to be of slightly better quality (lower Kidney Donor Profile Index [KDPI]) than those that were discarded during weekdays (KDPI, 76.5% vs 77.3%; P = 0.02). Our sample size may have limited our ability to detect small differences in donor kidney quality. Alternatively, it may be that the limits in staffing that can occur during ATC reduces the total number of transplants that certain centers can physically perform during those few days but does not alter acceptance thresholds regarding kidney quality per se. Of note, kidneys discarded during the ATC meetings were more often machine perfused, indicating that transplant centers may be more willing to forego transplantation of a machine-perfused kidney (despite its associated costs) during ATC conferences than at other times.
There have been no other published studies examining potential ATC effects on postoperative transplant care and outcomes, but prior research of the weekend effect revealed no significant associations between night and weekend liver transplant operations and graft survival.9 In addition, Baid-Agrawal et al,10 and more recently Anderson et al, found no significant associations for kidney transplant operations performed on weekends compared with weekdays with regard to posttransplant outcomes, such as DGF and kidney allograft and recipient survival. Our study of ATC versus non-ATC timeframes found no change in DGF rates, and overall allograft and recipient survival were not different at a median follow-up of 4.7 years. Taken as a whole, these reassuring findings suggest transplant centers are able to adequately maintain treatment protocols and patient safety measures during periods that could be challenging in terms of staffing (ie, during weekends and ATC conferences) compared with other, potentially more resource-replete timeframes.
We estimated there have been about 5 additional discarded kidneys per ATC conference each year, which may seem small relative to the total number of nearly 12 500 deceased-donor kidney transplants performed in 2015.11 However, considering that approximately 25 patients are removed everyday from the ever-growing kidney waiting list because of death or deteriorating health, discarding any available kidneys because of logistical or other nonmedical reasons can seem unacceptable to those continuing to wait on the list. For many of these patients, receiving a kidney that may otherwise be discarded, especially if it means coming off the waiting list earlier, could potentially save their lives.12-17
This study has a number of important limitations, including its retrospective, observational design and use of registry data. Hence, while we controlled for multiple factors to evaluate independent associations for ATC on transplant outcomes, residual confounding remains possible. In addition, several reasons may combine and lead to kidney discard, but such complex decision making is not captured by the SRTR database. Detailed biopsy findings for transplanted or discarded kidneys were not available. Lastly, our analysis was designed to evaluate direct ATC effects on transplant outcomes, but we could not assess potential indirect (though no less important) effects that the ATC conferences likely have on the field of transplantation in terms of knowledge dissemination.
In summary, this is the first study to report an increased odds of kidney discard during ATC meetings, leading to approximately 5 additional procured kidneys going unutilized each year. Although the annual ATC conference is tremendously important for disseminating new knowledge within the transplant community, the loss of potential life years saved from these additionally discarded kidneys may represent the true opportunity cost of the ATC. This is especially relevant given that transplantation during ATC meetings does not appear to negatively impact recipient outcomes.
In conclusion, our findings suggest the need for innovative staffing or other logistic solutions for transplant centers during ATC conferences, such as enhanced remote conferencing for essential clinical staff who stay behind. However, individual center-level interventions may not be feasible and may not adequately address the relatively small negative impact that activities like the ATC may have on kidney discard. Alternatively, generalized modifications to organ allocation designed to reduce the effect of such time-dependent community-based activities on organ utilization could be considered. For example, the OPTN could propose and request feedback on a policy change to allocate kidneys by centers instead of individual candidates after a certain point in the match run. These and other creative solutions may ultimately help to reduce the complexity of certain acceptance decisions and attenuate the impact of staffing on organ utilization.
Supplementary Material
Footnotes
Published online 4 December, 2018.
Portions of this article have been presented as a poster at the 2017 American Transplant Congress meeting, Chicago, Illinois, April 29-May 3, 2017.
Portions of this article have been published in abstract form: Am J Transplant. 2017;17 (suppl 3).
©2017 Mayo Foundation for Medical Education and Research.
The authors declare no funding or conflicts of interest.
D.A. participated in research design, data analysis, writing of the article. T.C. participated in research design, data analysis, and writing of the article. G.W. participated in research design, data analysis, and writing of the article. I.H. participated in research design, data analysis, and writing of the article.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Kasiske BL, Stewart DE, Bista BR, et al. The role of procurement biopsies in acceptance decisions for kidneys retrieved for transplant. Clin J Am Soc Nephrol. 2014;9:562–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. [DOI] [PubMed] [Google Scholar]
- 3.Kumar G, Deshmukh A, Sakhuja A, et al. Acute myocardial infarction: a national analysis of the weekend effect over time. J Am Coll Cardiol. 2015;65:217–218. [DOI] [PubMed] [Google Scholar]
- 4.Pathak R, Karmacharya P, Aryal MR, et al. Weekend versus weekday mortality in myocardial infarction in the United States: data from healthcare cost and utilization project nationwide inpatient sample. Int J Cardiol. 2014;174:877–878. [DOI] [PubMed] [Google Scholar]
- 5.Anderson BM, Mytton JL, Evison F, et al. Outcomes after weekend admission for deceased donor kidney transplantation: a population cohort study. Transplantation. 2017;101:2244–2252. [DOI] [PubMed] [Google Scholar]
- 6.Mohan S, Foley K, Chiles MC, et al. The weekend effect alters the procurement and discard rates of deceased donor kidneys in the United States. Kidney Int. 2016;90:157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickinson DM, Bryant PC, Williams MC, et al. Transplant data: sources, collection, and caveats. Am J Transplant. 2004;4(Suppl 9):13–26. [DOI] [PubMed] [Google Scholar]
- 8.Conover WJ. Practical Nonparametric Statistics. 3rd ed New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 9.Orman ES, Hayashi PH, Dellon ES, et al. Impact of nighttime and weekend liver transplants on graft and patient outcomes. Liver Transpl. 2012;18:558–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baid-Agrawal S, Martus P, Feldman H, et al. Weekend versus weekday transplant surgery and outcomes after kidney transplantation in the USA: a retrospective national database analysis. BMJ Open. 2016;6:e010482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hart A, Smith JM, Skeans MA, et al. OPTN/SRTR 2015 annual data report: kidney. Am J Transplant. 2017;17:21–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez-Flores I, Sanchez-Fructuoso A, Calvo N, et al. Preemptive kidney transplant from deceased donors: an advantage in relation to reduced waiting list. Transplant Proc. 2007;39:2123–2124. [DOI] [PubMed] [Google Scholar]
- 13.Schaeffner ES, Mehta J, Winkelmayer WC. Educational level as a determinant of access to and outcomes after kidney transplantation in the United States. Am J Kidney Dis. 2008;51:811–818. [DOI] [PubMed] [Google Scholar]
- 14.Resende L, Guerra J, Santana A, et al. Impact of donor age on renal allograft function and survival. Transplant Proc. 2009;41:794–796. [DOI] [PubMed] [Google Scholar]
- 15.Hurst FP, Sajjad I, Elster EA, et al. Transplantation of A2 kidneys into B and O recipients leads to reduction in waiting time: USRDS experience. Transplantation. 2010;89:1396–1402. [DOI] [PubMed] [Google Scholar]
- 16.Bouaoun L, Villar E, Ecochard R, et al. Excess risk of death increases with time from first dialysis for patients on the waiting list: implications for renal allograft allocation policy. Nephron Clin Pract. 2013;124:99–105. [DOI] [PubMed] [Google Scholar]
- 17.Scalea JR, Barth RN, Munivenkatappa R, et al. Shorter waitlist times and improved graft survivals are observed in patients who accept hepatitis C virus+ renal allografts. Transplantation. 2015;99:1192–1196. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


