Abstract
Introduction:
Little is known about the effectiveness of cigarette health warning labels (HWLs) among U.S. pregnant and non-pregnant women of reproductive age. Our intent was to examine HWL responses by pregnancy status and their associations with knowledge and perceived harm.
Methods:
We conducted cross-sectional analyses of first (2013–2014) and second (2014–2015) Population Assessment of Tobacco and Health waves. The sample (N = 19,095) was representative of U.S. women of reproductive age (18–45 years). We examined three HWL responses (seeing HWLs, forgoing cigarettes because of HWLs, likely-to-quit because of HWLs), perceived harm from smoking, and knowledge of health effects to fetuses and others. Weighted logistic regression compared HWL responses by pregnancy status and their associations with perceived harm and knowledge, adjusting for demographics and tobacco use. Results were presented as marginal predicted probabilities.
Results:
Pregnant smokers were less likely than never-pregnant smokers to report likelihood of quitting (57% vs 67%, p = 0.020). Forgoing cigarettes and likely-to- quit due to HWLs—but not seeing HWLs—were positively associated with perceived harm and knowledge. Pregnant smokers were less likely to have knowledge of fetal harm (83%) than ever-pregnant (91%, p = 0.006) and never-pregnant (92%, p = 0.003) smokers. However, pregnant smokers who reported likelihood of quitting were much more likely to have knowledge of fetal harm than those who did not (93% vs. 67%, p = 0.028).
Conclusions:
Implementation of HWLs that elicit stronger reactions—such as pictorial HWLs—and increase knowledge of fetal risks is one action to help reduce tobacco use in pregnant and non-pregnant U.S. women of reproductive age.
1. Introduction
Women who are or may become pregnant are key populations to target for smoking prevention and cessation. Tobacco use is a major cause of negative reproductive outcomes, including reduced fertility, low birth weight, and infant mortality.1–3 Cessation during pregnancy can significantly improve babies’ outcomes.4 In the U.S., 13.8% of pregnant women and 20.1% of non-pregnant reproductive age women smoke.5,6
One policy-level approach for cessation is health warning labels (HWLs) on cigarette packaging. HWLs are ubiquitous information sources to warn about the health risks of smoking and secondhand smoke (SHS). In the U.S., the four HWLs are text-only and have been on packaging since 1984; one label describes harm to fetuses, and another states that smoking “may complicate pregnancy.” Studies have shown that HWLs—especially pictorial HWLs—are effective for increasing knowledge about health risks and quitting.7–9 Responses to HWLs—such as seeing (“salience”) or forgoing cigarettes because of HWLs (“behavioral response”)—are important intermediary steps between HWL exposure and attitudinal and behavioral changes.10–12
Pregnancy-related HWLs may elicit stronger responses than non-pregnancy-related HWLs in reproductive age women compared to men and older women.14 However, to our knowledge, no information is available about responses among U.S. pregnant women, and if responses are associated with harm perceptions and knowledge. Among U.S. reproductive age women, our aims are to: (1) determine whether pregnant women are more responsive to HWLs than non-pregnant women, and (2) examine whether HWL responses are associated with knowledge of health effects and harm perceptions. Our results with a nationally representative sample will help determine whether current labels effectively target pregnant and non-pregnant women of reproductive age, or provide evidence to support the FDA in implementing new HWLs.
2. Methods
We collapsed Public Use File (PUF) data from Waves 1 (2013–2014) and 2 (2014–2015) of the Population Assessment of Tobacco and Health (PATH), a household-based, nationally- representative, cohort study of adults and youths from the civilian, non-institutionalized U.S. population.15 Weighting procedures adjusted for oversampling, nonresponse, and the complex survey design. Further information about PATH and weighting procedures is available elsewhere.16 We restricted our analyses to women of reproductive age (18–45 years) with complete information about current and previous pregnancies, current cigarette smoking, and frequency of seeing HWLs. Youth (<18) pregnancy status was unavailable.
2.1. Measures
We obtained age, race/ethnicity, household income, education, lifetime use of cigarettes, and past 30-day use of other tobacco products. Using PATH derived variables, current cigarette smokers were defined as those who reported currently smoking cigarettes every day or some days, including both experimental (<100 cigarettes in lifetime) and established (≥100 cigarettes in lifetime) smokers. We did not include number of years smoking, frequency and intensity of smoking, and time to first cigarette because of the large amount of missing data. Pregnancy status was categorized as never-pregnant, ever-pregnant (pregnant previously), and currently pregnant at the time of survey completion.
Three measures of HWL responses were asked at both waves:
-
(1)
Seeing HWLs: all respondents were asked: “In the past 30 days, how often have you noticed health warnings on cigarette packages?” We dichotomized the 5-point Likert scale: 0=never, 1=rarely, sometimes, often, or very often.
Smokers who reported seeing HWLs rarely, sometimes, often, or very often were subsequently asked:
-
(2)
Forgoing cigarettes: “In the past 30 days, how often have health warnings stopped you from having a cigarette when you were about to smoke one?” We dichotomized the 5-point Likert scale: 0=never, 1=rarely, sometimes, often, or very often.
-
(3)
Likely-to-quit: “To what extent, if at all, do the health warnings on cigarette packs make you more likely to quit smoking?” We dichotomized the 4-point Likert scale: 0=not at all, 1=a little, somewhat, or a lot.
Three measures of harm perceptions and knowledge were used:
-
(1)
Perceived harm: “How harmful do you think cigarettes are to health?” Based on the mean value of 4.13 in the sample, we dichotomized the 5-point Likert scale: 0=not at all, slightly, or somewhat harmful, 1=very or extremely harmful.
-
(2)
Knowledge of health effects: Respondents were asked, “Based on what you know or believe, does smoking cause...” (0=no, 1=yes). PATH included 11 conditions in the survey at both waves: stroke, lung cancer, heart disease, blindness, poor circulation, bladder cancer, mouth cancer, and lung disease in smokers, lung disease and heart attack in non-smokers from second-hand smoke (SHS), and harm to fetuses (or unborn children) during pregnancy from SHS. Harm to fetuses was kept separately (see below). We summarized the other 10 items into one composite score of knowledge (range=0–10, Cronbach’s α=0.76). Based on the mean score of 7.83 in the sample, we dichotomized the variable: low (0–8) and high (9–10) knowledge level.
-
(3)
Knowledge of fetal effects: Knowledge about SHS effect on the fetus was kept as a separate item (0=no, 1=yes).
2.2. Study Sample
A total of 19,095 reproductive age women were analyzed (weighted N=112,188,239); 747 (3.6%) were currently pregnant, 9,980 (60.2%) were ever-pregnant, and 8,368 (36.2%) were never-pregnant. About 20.9% (n=6,885) were current smokers, including 12.7% (n=176) of pregnant, 24.1% (n=4,646) of ever-pregnant, and 16.4% (n=2,063) of never-pregnant women. The mean gestational age was 20.7 weeks (BRR SE=0.52, n=745).
2.3. Analysis
We performed a cross-sectional analysis following the procedures described in the PATH User Guide. Variance and p-value computations used supplied survey weights and the recommended Balanced Repeated Replication (BRR) method (Fay=0.3). We conducted a descriptive analysis of the frequencies of HWL responses, knowledge, and harm perceptions by smoking status.
Next, we conducted weighted multivariate logistic regression of: 1) the association between pregnancy status and the three HWL responses; and 2) cigarette harm perceptions, knowledge of health effects, and knowledge about fetal effects as a function of HWL responses (each response tested separately). Models adjusted for pregnancy status, age, race/ethnicity, income, education, lifetime cigarette use, other tobacco product use, and wave. In the models of knowledge and perceived harm, we used Wald χ2 tests of interaction terms between pregnancy and HWL responses. Models stratified by pregnancy status were then run for statistically significant interactions. All models were conducted with current smokers. The model of seeing HWLs as a function of pregnancy was additionally conducted with the total sample because this HWL response was the only one asked of non-smokers. Results are reported in terms of adjusted marginal predicted probabilities, with p-values from the odds ratios. Analyses were conducted in Stata 15 (StataCorp, College Station, TX).
3. Results
3.1. Descriptive Analysis
About half of the sample (52.4%) and most smokers (80.4%) reported seeing HWLs. Among smokers who saw HWLs, 35.6% reported forgoing cigarettes, and 65.2% reported being likely to quit. Most smokers reported cigarettes as harmful (78.4%) and SHS as harmful to fetuses (90.8%). However, fewer than half (42.0%) reported a high knowledge level of other health effects.
3.2. Responses to HWLs By Pregnancy Status
In multivariate models, pregnancy was not associated with seeing HWLs in the total sample or in smokers only (Figure 1). Among smokers, pregnancy was not associated with forgoing cigarettes because of HWLs. Never-pregnant smokers were more likely than pregnant smokers to report increased likelihood of quitting because of HWLs (67.1% vs. 57.4%, p=0.020).
Fig. 1.
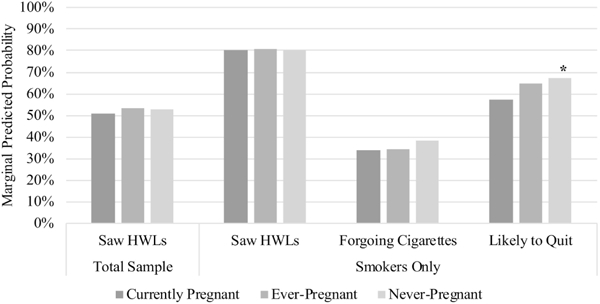
Adjusted marginal predicted probabilities of health warning label (HWL) responses by pregnancy status among women of reproductive age (18–45 years).Note. Currently pregnant women are the reference group; *p < 0.05, **p < 0.01, ***p < 0.001; Models adjusted for pregnancy status, age, race/ethnicity, household income, education, lifetime use of cigarettes, use of other tobacco products, and wave.
3.3. Knowledge and Harm Perceptions by HWL Responses and Pregnancy Status
In multivariate models, smokers who saw HWLs were more likely than those who did not to have knowledge of health effects (43.2% vs. 39.3%, p=0.022). However, seeing HWLs was not associated with perceived harm or knowledge of fetal effects (Figure 2). Smokers who reported forgoing cigarettes were more likely than those who did not to perceive harm from smoking (81.8% vs. 77.2%, p=0.001), know about health effects (49.8% vs. 39.5%, p<0.001), and know about fetal effects (92.7% vs. 90.4%, p=0.023). Similarly, smokers who reported being likely to quit were more likely than those who did not to perceive harm (83.0% vs. 70.9%, p<0.001), know about health effects (47.1% vs 35.7%, p<0.001), and know about fetal effects (93.2%, vs. 87.4%, p<0.001).
Fig. 2.
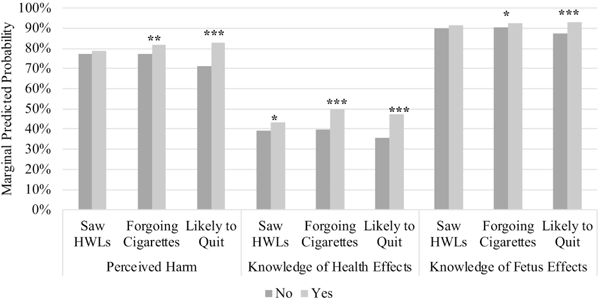
Adjusted marginal predicted probabilities of harm perceptions and knowledge by health warning label (HWL) responses among female smokers of reproductive age (18–45 years). Note. “No” is the reference group for each HWL response; *p < 0.05, **p < 0.01, ***p < 0.001; Models adjusted for pregnancy status, age, race/ethnicity, household income, education, lifetime use of cigarettes, use of other tobacco products, and wave.
Pregnancy was associated with reduced knowledge of fetal effects due to SHS, but not with perceived harm or knowledge of other health effects. In the model adjusting for the likely-to-quit HWL response, pregnant smokers were less likely to know about fetal effects (82.5%) than ever- pregnant (91.3%, p=0.006) and never-pregnant (91.7%, p=0.003) smokers. Results were similar in the models adjusting for other HWL responses.
The effect of likely-to-quit HWL response on fetal effect knowledge was much larger for pregnant than non-pregnant smokers (Wald χ2: F(2,98)=4.29,p=0.0163). Specifically, 93.0% of pregnant smokers who reported that HWLs increased their likelihood of quitting knew about the fetal effects of SHS compared to 66.6% of pregnant smokers who reported that HWLs did not increase their likelihood of quitting (p=0.028). In contrast, likelihood of quitting was associated with smaller gains in fetal effect knowledge among ever-pregnant (93.1% vs. 87.4%, p<0.001) and never-pregnant (93.6% vs. 89.3%, p=0.007) smokers. Pregnancy status did not modify any other association.
4. Discussion
This study is the first to report HWL responses by pregnant and non-pregnant reproductive age U.S. women, and associations with harm perceptions and knowledge. Using two waves of a nationally-representative dataset, we included a significant number of reproductive age women, including pregnant smokers. Due to the cross-sectional analysis, the results presented are correlations, and do not indicate causal relationships. However, this study is a first step in examining HWL responses among U.S. women of reproductive age.
We found that pregnant women were as likely as non-pregnant women to report seeing HWLs and forgoing cigarettes because of HWLs, but were less likely to endorse likely-to-quit because of HWLs. Only about a third of smokers reported forgoing cigarettes and about two-thirds reported likely-to-quit. Together, these findings illustrate the need for more persuasive HWLs that target reproductive age women, particularly pregnant women. Other studies have shown that forgoing cigarettes and likely-to-quit because of HWLs are highly predictive of quitting.7,17,18 The difference in HWL response by pregnancy status could be due to differences in risk perceptions. One study found that never-pregnant women largely believed that smoking during pregnancy was too risky, whereas many ever-pregnant women thought quitting during pregnancy could be harmful to the baby.19 Further research is needed to develop HWLs that can overcome misconceptions and encourage cessation during pregnancy.
We also found that HWL responses were associated with women’s knowledge and harm perceptions, particularly among pregnant women. Simply seeing the HWLs was not associated with a high level of knowledge and perceived harm, illustrating the importance of persuasive HWLs that elicit strong cognitive (e.g., likelihood of quitting) and behavioral (e.g., forgoing cigarettes) reactions. Compared to non-pregnant women, pregnant women were less likely to know that SHS harms fetuses, but pregnant women with a strong cognitive reaction to HWLs were much more likely to be knowledgeable of this fact. HWLs may need to be targeted to elicit stronger reactions in pregnant women, and subsequently may improve knowledge. Conversely, prior knowledge or perceived harm may have “primed” women to have greater HWL responses. However, research has shown that strong responses were associated with quit attempts among smokers with low levels of perceived risk at baseline.20
Our findings support the need for pictorial HWLs in the U.S. as part of a comprehensive, multi-pronged approach to address the persistent prevalence of smoking during pregnancy. Pictorial HWLs may be more effective than text-only HWLs for women overall and young women specifically.13,21–23 In Uruguay, pictorial HWLs alongside other tobacco control policies increased the cessation rate during pregnancy, which improved birth weight.24 The 2009 Family Smoking Prevention and Tobacco Control Act mandated the use of pictorial HWLs on 50% of the front and back of cigarette packaging in the U.S., but it has yet to be implemented. Pictorial HWLs could potentially reduce prenatal smoking and hospital costs up to $100.2 million per year in the U.S.25 Pregnancy-related pictorial HWLs may be particularly effective for reproductive age and pregnant women, especially if pictures of real babies and testimonials are included.14,19,26,27
This study has several limitations. One limitation was our cross-sectional approach, which limits causal inferences about HWL effects. However, this approach allowed us to include a large number of pregnant smokers. Future research can use PATH data to examine longitudinal effects of HWLs on knowledge, attitude, and behavior changes. Also, we were unable to include women age 15–17 years, or to control for knowledge of health effects of other tobacco products, frequency of other product use, and dependence. Only one measure of cognitive HWL responses (likelihood of quitting) and one measure of behavioral HWL responses (forgoing cigarettes) were available, and future research should use multiple measures to better capture these latent constructs. The PATH survey does not measure exposure to specific HWLs; therefore, we cannot examine responses to pregnancy-specific HWLs. Lastly, we did not differentiate women who quit during pregnancy. Therefore, our pregnant sample may be “hard-core” smokers, i.e., completely unwilling or unable to quit and likely to remain that way.29 Longitudinal PATH analyses can examine whether HWLs encourage quitting when women become pregnant.
Our study confirms the need for more effective HWLs to increase cognitive and behavioral reactions among U.S. women of reproductive age, especially pregnant women. Findings indicate that stronger reactions are associated with higher levels of knowledge and perceived harm, and that HWLs may be beneficial for pregnant women’s knowledge of SHS effects on fetuses. For women’s and babies’ health, the development and implementation of effective pictorial HWLs is especially urgent to help pregnant women quit smoking.
Highlights.
Pregnant smokers were less likely to report likely-to-quit due to HWLs.
Women who responded to HWLs had knowledge of health risks and perceived harm.
Pregnant smokers were less likely to know about fetal effects of SHS.
Pregnant smokers’ knowledge notably improved if HWLs made them likely-to-quit.
Acknowledgements
The authors wish to thank Dr. Stephen Higgins and the TCORS Vulnerable Populations Working Group for their feedback and support of the study.
Role of Funding Sources
This project was completed as part of the collaborative research being conducted by the National Institutes of Health (NIH) and Food and Drug Administration (FDA) Tobacco Centers of Regulatory Science (TCORS) Vulnerable Populations Working Group. The research reported in this work was supported by: Grant # 5P50CA180523 from the National Cancer Institute and the FDA Center for Tobacco Products (CTP) and Grant # P50HL120163 from the National Heart, Lung and Blood Institute (NHLBI) and FDA CTP. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Footnotes
Conflict of Interest
The authors have no conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. Department of Health and Human Services. The health consequences of smoking— 50 years of progress. A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 2.Pollack H, Lantz PM, Frohna JG. Maternal smoking and adverse birth outcomes among singletons and twins. American Journal of Public Health. 2000;90(3):395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Human Reproduction. 1998; 13(6): 1532–1539. [DOI] [PubMed] [Google Scholar]
- 4.Yan J, Groothuis PA. Timing of prenatal smoking cessation or reduction and infant birth weight: Evidence from the United Kingdom Millennium Cohort Study. Maternal and Child Health Journal. 2015;19(3):447–458. doi: 10.1007/s10995-014-1516-x [DOI] [PubMed] [Google Scholar]
- 5.Kurti AN, Redner R, Lopez AA, et al. Tobacco and nicotine delivery product use in a national sample of pregnant women. Preventive Medicine. 2017;104:50–56. doi: 10.1016/j.ypmed.2017.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez AA, Redner R, Kurti AN, et al. Tobacco and nicotine delivery product use in a U.S. national sample of women of reproductive age. Preventive Medicine. 2018;[epub ahead of print]:pii: S0091–7435(0018)30090–30092. doi: 10.1016/j.ypmed.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borland R, Yong HH, Wilson N, et al. How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey. Addiction. 2009; 104(4):669–675. doi: 10.1111/j.1360-0443.2009.02508.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammond D, Fong GT, McNeill A, Borland R, Cummings KM. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: Findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15(Suppl 3):iii19–iii25.doi: 10.1136/tc.2005.012294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. Social Science & Medicine. 2016;164:118–129. doi: 10.1016/j.socscimed.2016.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammond D Health warning messages on tobacco products: A review. Tobacco Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.037630 [DOI] [PubMed] [Google Scholar]
- 11.Yong H-H, Borland R, Thrasher JF, et al. Mediational pathways of the impact of cigarette warning labels on quit attempts. Health Psychology. 2014;33(11): 1410–1420. doi: 10.1037/hea0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tobacco Control. 2016;25(3):341–354. doi: 10.1136/tobaccocontrol-2014-051978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gil-Lacruz AI, Gil-Lacruz M, Leeder S. Women and smoking — Prices and health warning messages: Evidence from Spain. Addictive Behaviors. 2015;45:294–300. doi: 10.1016/j.addbeh.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 14.Kollath-Cattano C, Osman A, Thrasher JF. Evaluating the perceived effectiveness of pregnancy-related cigarette package health warning labels among different gender/age groups. Addictive Behaviors. 2017;66:33–40. doi: 10.1016/j.addbeh.2016.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.USDHHS, NIH, NIDA, FDA, CTP. Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. Inter-university Consortium for Political and Social Research [distributor]; 2018. [Google Scholar]
- 16.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tobacco Control. 2017;26(4):371–378. doi: 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho YJ, Thrasher JF, Swayampakala K, et al. Does reactance against cigarette warning labels matter? Warning label responses and downstream smoking cessation amongst adult smokers in Australia, Canada, Mexico and the United States. PLoS One. 2016;11(7):e0159245. doi: 10.1371/journal.pone.0159245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fathelrahman AI, Omar M, Awang R, et al. Smokers’ responses toward cigarette pack warning labels in predicting quit intention, stage of change, and self-efficacy. Nicotine & Tobacco Research. 2009;11(3):248–253. doi: 10.1093/ntr/ntn029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levis DM, Stone-Wiggins B, O’Hegarty M, et al. Women’s perspectives on smoking and pregnancy and graphic warning labels. American Journal of Health Behavior. 2014;38(5):755–764. doi: 10.5993/AJHB.38.5.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bekalu MA, Ramanadhan S, Bigman CA, Nagler RH, Viswanath K. Graphic and arousing? Emotional and cognitive reactions to tobacco graphic health warnings and associated quit-related outcomes among low SEP population groups. Health Communication. 2018:1–9. doi: 10.1080/10410236.2018.1434733 [DOI] [PubMed] [Google Scholar]
- 21.O’Hegarty M, Pederson LL, Nelson DE, Mowery P, Gable JM, Wortley P. Reactions of young adult smokers to warning labels on cigarette packages. American Journal of Preventive Medicine. 2006;30(6):467–473. doi: 10.1016/j.amepre.2006.01.018 [DOI] [PubMed] [Google Scholar]
- 22.Thrasher JF, Rousu MC, Anaya-Ocampo R, Reynales-Shigematsu LM, Arillo-Santillan E, Hernandez-Avila M. Estimating the impact of different cigarette package warning label policies: The auction method. Addictive Behaviors. 2007;32(12):2916–2925. doi: 10.1016/j.addbeh.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 23.Koval JJ, Aubut JA, Pederson LL, O’Hegarty M, Chan SS. The potential effectiveness of warning labels on cigarette packages: the perceptions of young adult Canadians. Canadian Journal of Public Health. 2005;96(5):353–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris JE, Balsa AI, Triunfo P. Tobacco control campaign in Uruguay: Impact on smoking cessation during pregnancy and birth weight. Journal of Health Economics. 2015;42:186–196. doi: 10.1016/j.jhealeco.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 25.Tauras JA, Peck RM, Cheng KW, Chaloupka FJ. Graphic warning labels and the cost savings from reduced smoking among pregnant women. International Journal of Environmental Research and Public Health. 2017; 14(2):pii: E164. doi: 10.3390/ijerph14020164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berg CJ, Thrasher JF, Westmaas JL, Buchanan T, Pinsker EA, Ahluwalia JS. College student reactions to health warning labels: Sociodemographic and psychosocial factors related to perceived effectiveness of different approaches. Preventive Medicine. 2011;53(6):427–430. doi: 10.1016/j.ypmed.2011.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammond D, Reid JL, Driezen P, Boudreau C. Pictorial health warnings on cigarette packs in the United States: An experimental evaluation of the proposed FDA warnings. Nicotine & Tobacco Research. 2013;15(1):93–102. doi: 10.1093/ntr/nts094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schindler-Ruwisch JM, Leavitt LE, Macherelli LE, Turner MM, Abroms LC. Motivating smoking cessation text messages: Perspectives from pregnant smokers. Maternal and Child Health Journal. 2018;22(6):822–829. doi: 10.1007/s10995-018-2452-y [DOI] [PubMed] [Google Scholar]
- 29.Warner KE, Burns DM. Hardening and the hard-core smoker: concepts, evidence, and implications. Nicotine & Tobacco Research. 2003;5(1):37–48. doi : 10.1080/1462220021000060428 [DOI] [PubMed] [Google Scholar]


