Abstract
Objective
Fluoride varnish (FV) applications among non-dentist primary care providers has increased due to state Medicaid policies. In this study we examine the impact of FV policies on the oral health of publicly insured children aged 2 to 6 years old.
Methods
Using three waves of the National Survey of Children’s Health (2003, 2007, 2011/12), we used a logistic regression model with state and year fixed effects, adjusting for relevant child characteristics, to examine the association between years since a state implemented a FV policy and the odds of a publicly insured child having very good or excellent teeth. We compared children with public insurance in states with FV policies to children with public insurance in states without FV policies, controlling for the same difference among children with private insurance who were unlikely to be affected by Medicaid FV policies.
Results
Among 68,890 children aged 2–6 years, 38% had public insurance. Compared to privately insured children, publicly insured children had significantly lower odds of having very good or excellent teeth (odds ratio (OR)=0.70, 95% CI=0.62–0.81). Publicly insured children in states with FV policies implemented for four or more years had significantly greater odds of having very good or excellent teeth (OR=1.28, 95% CI=1.03–1.60) compared to publicly insured children in states without FV policies.
Conclusions for Practice
State policies supporting non-dental primary care providers application of FV were associated with improvements in oral health for young children with public insurance.
Keywords: Medicaid, oral health, early childhood, access to care
Introduction
Early childhood dental caries, commonly referred to as tooth decay, is a common and preventable disease in young children that is concentrated among children in low-income families and racial and ethnic minorities (Dye, Li & Thornton-Evans, 2012). Preventing dental caries is important because of the associated individual, social, and economic consequences, including pain and decreased quality of life due to untreated caries (Filstrup et al., 2003), missed days of school (Jackson, Vann Jr, Kotch, Pahel & Lee, 2011), and preventable medical services such as emergency department visits and hospitalization (Stearns, Rozier, Kranz, Pahel & Quinonez, 2012). Fluoride varnish prevents dental caries (Marinho, Worthington, Walsh, & Clarkson, 2013), but remains underused among Medicaid-enrolled infants and toddlers, who are disproportionally affected by dental caries. Factors contributing to underuse include shortages and uneven distribution of the dental workforce (Cao et al., 2017), caregivers’ attitudes and beliefs about dental visits and oral health (Hilton, Stephen, Barker & Weintraub, 2007), and dentists’ reluctance to treat young children or accept Medicaid (Seale & Casamassimo, 2003).
Since 2014, to increase fluoride varnish use, the U.S. Preventive Services Task Force (USPSTF) has recommended that primary care clinicians apply fluoride varnish to the teeth of all children aged 5 years and younger (Moyer, 2014). Delivering fluoride varnish in primary care offices can help increase access because infants and toddlers make frequent medical visits (Bright Futures & American Academy of Pediatrics, 2017), but have low rates of dental visits (Bouchery, 2013). One national study found that four years after enacting fluoride varnish policies states have higher rates of oral health services provided by non-dentists than states with policies implemented for shorter periods of time (Arthur & Rozier, 2016). However, this study relied on state-level aggregate data reported to CMS rather than individual data, raising concerns about utilization underreporting (Schneider, Rossetti & Crall, 2007), and did not examine oral health status outcomes. As of 2017, all state Medicaid programs support primary care providers’ application of fluoride varnish to children, and while empirical findings suggest that after a time lag these policies increase access, we are unaware of national studies examining the effects of these policies on children’s oral health. The few empirical studies on this topic focused on one or two-states, and report that Medicaid policies supporting pediatricians and other non-dental professionals to apply fluoride varnish were associated with increased varnish use (Herndon, Tomar, Catalanotto, Vogel & Shenkman, 2015; Okunseri, Szabo, Garcia, Jackson & Pajewski, 2010; Okunseri, Szabo, Jackson, Pajewski & Garcia, 2009; Rozier, Stearns, Pahel, Quinonez & Park, 2010) and reduced caries (Kranz, Preisser & Rozier, 2015). State-level studies also suggest a dose effect, with children receiving four or more fluoride varnish applications having reduced dental caries, restorative treatment, and related expenditures (Hendrix, Downs, Brophy, Carney Doebbeling & Swigonski, 2013; Pahel, Rozier, Stearns & Quiñonez, 2011; Stearns et al., 2012), positive outcomes not observed when children receive fewer applications (Blackburn, Morrisey & Sen, 2017).
To address this gap in the literature, we sought to examine the impact of state Medicaid policies on the oral health of publicly insured children, who are the intended and likely benefactors of polices supporting primary care providers’ application of fluoride varnish. We used three waves of the National Survey of Children’s Health (NSCH), which provides individual-level data for a national sample of children, and compared the oral health status of children with public insurance in states with fluoride varnish policies to publicly insured children in states without fluoride varnish policies, while simultaneously controlling for the same difference among privately insured children unlikely to be affected by these policies. This difference-in-differences approach allowed us to estimate the impact of state Medicaid policies supporting the application of fluoride varnish by non-dentists on the oral health of publicly insured children.
Methods
Data
We used the 2003, 2007, and 2011/2012 NSCH to examine the impact of Medicaid policy on children’s oral health. Information on children’s dental health, physical health, insurance coverage, demographic characteristics, and socioeconomic status was obtained via telephone survey (Data Resource Center for Child and Adolescent Health, 2016). Randomly sampled telephone numbers were called to find households with children aged 0 to 17 years. One child in a household was randomly selected to be the subject of the interview, and the adult in the household who knows the most about the child’s health was interviewed. We excluded from analyses children with no natural teeth and parents who didn’t know or refused to respond. We also excluded uninsured children and those whose insurance status was unknown in order to directly compare children likely to be affected by these policies (i.e., publicly insured children) and children unlikely to be affected by these policies (i.e., privately insured children). Our analytic sample included children aged 2 to 6 years because the U.S. Preventive Services Task Force (USPSTF) recommends that primary care clinicians apply fluoride varnish to the teeth of all children aged 5 years and younger (Moyer, 2014) and most state Medicaid programs limit benefits to children younger than 6 years (American Academy of Pediatrics, 2017).
The American Academy of Pediatrics (AAP) Caries Prevention Services Reimbursement Table provided information on the year that each state’s Medicaid program began reimbursing fluoride varnish applied in primary care settings (AAP, 2017). These data were compiled and updated over time through conversations with state Medicaid officials and published state Medicaid bulletins.
Variables
We used information about the parent-reported condition of the child’s teeth (response options: excellent, very good, good, fair, or poor) to construct a dichotomous dependent variable indicating the child’s teeth were in excellent or very good condition. Although there are limitations to using parent-reported survey data, research suggests parents’ assessment of child oral health is associated with actual need (Talekar, Rozier, Slade & Ennett, 2005). We dichotomized this variable due to the distribution of the data and based on how others have operationalized this NSCH variable (Shariff & Edelstein, 2016).
Our key explanatory variable provided a measure of the number of years a state policy supporting Medicaid reimbursement for fluoride varnish by non-dental professionals had been implemented. For each NSCH survey year and each state, we determined if a fluoride varnish policy had been implemented and the number of years since implementation. We constructed a 4-category ordinal variable for years since the fluoride varnish policy’s implementation (no policy, fewer than 2 years, 2 or 3 years, and 4 or more years). For the 2011/12 NSCH survey, we counted years of implementation from 2011.
Child’s insurance type was categorized as private or public (i.e., Medicaid or the state Children’s Health Insurance Program (CHIP)). We constructed a categorical variable of poverty ratio (<100%, 100–200%, 200–400%, >400%) using information about household income and family size and included an additional category to indicate poverty data was missing for approximately 10% of observations. Additional demographic variables included: age (categorized as 2–3 years and 4–6 years); race/ethnicity (Hispanic, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Other race); and gender. Child’s physical health status was reported on a five-point scale (excellent, very good, good, fair, or poor). We combined the fair and poor responses due to low frequency of responses of poor health to construct a four-category measure of physical health status. An indicator of special health care needs was constructed using the five-item children with special health care needs (SHCN) screener (Child and Adolescent Health Measurement Initiative, 2017).
Analysis
We present unweighted frequencies and unadjusted, weighted percentages to describe the study sample’s demographic and health-related characteristics. Responses were weighted using the standard weights for the sample of persons in the NSCH. Descriptive statistics are reported by private and public insurance status and we used chi-squared tests to examine differences between privately and publicly insured children.
We used a logistic regression model to estimate the odds of having excellent or very good teeth, adjusting for the aforementioned variables and the interaction between insurance-type and years since policy implementation, allowing us to interpret the interaction term as the incremental effect of a fluoride varnish policy on a publicly-insured child’s odds of having excellent or very good teeth. The model also included an interaction between SHCN and physical health, providing an interpretation of the additive effect of SHCN by each physical health category. The inclusion of fixed effects for state of residence and survey year made this a difference-in-differences model, and the inclusion of privately insured children as an additional control made this a triple difference model. Analyses were conducted using STATA 14 (College Station, TX: StataCorp LP) and the survey (svy) commands to account for the complex survey design when determining variance estimates. This study was conducted in accord with prevailing ethical principles and was determined to be exempt by our institution’s Institutional Review Board.
Results
The analytic sample included 68,890 children between the ages of 2 and 6 years. Approximately 18.24% of children lived in poverty, (Table 1) and most had excellent or very good teeth (75.40%), excellent (62.96%) or very good (22.84%) physical health and were privately insured (62%). Compared to privately insured children, publicly insured children were significantly more likely to live in poverty (42.18% vs. 3.59%, P<0.001), have a SHCN (17.91% vs. 13.66%, P<0.001), and report fair or poor physical health (5.14% vs. 1.36%, P<0.001). Publicly-insured children were more likely to have parent-reported excellent or very good teeth in states with a fluoride varnish policy (67.1% vs. 60.1%, P=0.002) than their peers in states without a policy (Table 2). Privately-insured children were more likely to have parent-report excellent or very good teeth than their publicly-insured counterparts in states with a policy (83.92% vs. 67.08%, P<0.001) and without a policy (82.74% vs. 60.91%, P<0.001).
Table 1.
Characteristics of U.S. children aged 2–6 years (NSCH 2003, 2007, 2011/12)
| Variables | Full sample (Unweighted N=68,890) | Public insurance (Unweighted N=20,780) | Private insurance (Unweighted N=48,110) |
|---|---|---|---|
| Parent-reported condition of child’s teeth* | |||
| Excellent | 52.15% | 40.37% | 59.37% |
| Very good | 23.25% | 22.50% | 23.71% |
| Good | 17.36% | 25.45% | 12.41% |
| Fair | 5.41% | 8.73% | 3.38% |
| Poor | 1.62% | 2.70% | 0.97% |
| No teeth, didn’t know, or refused | 0.21% | 0.26% | 0.17% |
| Parent-reported condition of child’s teeth dichotomized as excellent or very good teeth* | 75.40% | 62.87% | 83.07% |
| Public health insurance | 37.97% | 100.00% | |
| Private health insurance | 62.03% | 100.00% | |
| Years since state implemented Medicaid fluoride varnish policy* | |||
| No policy | 67.24% | 65.98% | 68.02% |
| <2 years | 3.26% | 2.27% | 3.87% |
| 2 or 3 years | 18.66% | 19.95% | 17.87% |
| 4 or more years | 10.84% | 11.80% | 10.25% |
| Sex | |||
| Female | 48.56% | 48.86% | 48.38% |
| Male | 51.44% | 51.14% | 51.62% |
| Age group* | |||
| 2–3 years | 38.09% | 39.89% | 36.99% |
| 4–6 years | 61.91% | 60.11% | 63.01% |
| Race/ethnicity* | |||
| White, non-Hispanic | 54.76% | 33.39% | 67.85% |
| Black, non-Hispanic | 12.74% | 20.49% | 8.00% |
| Multi-racial/Other, non-Hispanic | 11.84% | 10.59% | 12.60% |
| Hispanic | 20.66% | 35.52% | 11.56% |
| Federal poverty level (FPL)* | |||
| Missing | 9.45% | 11.73% | 8.05% |
| < 100% FPL | 18.24% | 42.18% | 3.59% |
| 100–199% FPL | 19.77% | 31.30% | 12.72% |
| 200–399% FPL | 27.31% | 12.43% | 36.41% |
| 400% or more FPL | 25.23% | 2.37% | 39.23% |
| Child has a special health care need* | 15.27% | 17.91% | 13.66% |
| Physical health status* | |||
| Excellent | 62.96% | 50.82% | 70.39% |
| Very Good | 22.84% | 25.50% | 21.22% |
| Good | 11.41% | 18.55% | 7.04% |
| Fair or Poor | 2.79% | 5.14% | 1.36% |
Unweighted frequencies and weighted percentages are provided. Chi-square tests were used to compare each variable for children with public and private insurance coverage.
P-value <0.001
Table 2.
Oral health status of U.S. children aged 2–6 years in states with and without a Medicaid fluoride varnish policy (NSCH 2003, 2007, 2011/12)
| Variables | Medicaid policy | No Medicaid policy | ||
|---|---|---|---|---|
| Public health insurance (n=7,653) | Private health insurance (n=15,538) | Public health insurance (n=13,127) | Private health insurance (n=32,572) | |
| Parent-reported condition of child’s teeth | ||||
| Excellent | 44.14% | 60.66% | 38.61% | 58.86% |
| Very good | 22.94% | 23.26% | 22.30% | 23.88% |
| Good | 23.93% | 12.15% | 26.15% | 12.52% |
| Fair | 6.96% | 3.16% | 9.55% | 3.46% |
| Poor | 1.87% | 0.75% | 3.08% | 1.05% |
| No teeth, didn't know, or refused | 0.16% | 0.02% | 0.31% | 0.23% |
| Parent-reported condition of child’s teeth dichotomized as excellent or very good | 67.08% | 83.92% | 60.91% | 82.74% |
Unweighted frequencies and weighted percentages are provided.
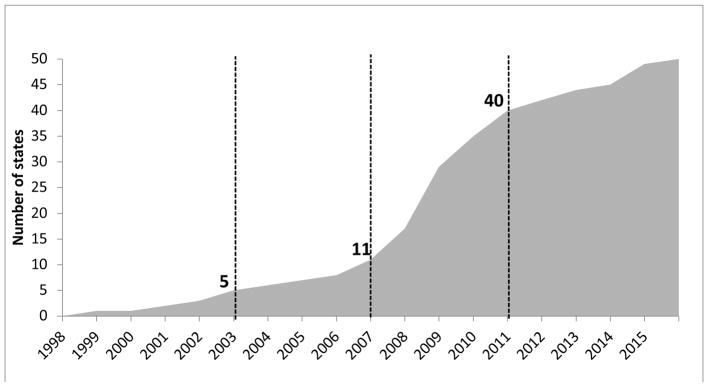
As Figure 1 illustrates, the number of states with fluoride varnish policies has increased over time. Five states had a policy in 2003, 12 states in 2007, and 40 states in 2011.
Figure 1.
States adopting a Medicaid policy for reimbursement of fluoride varnish by non-dental providers
Source: American Academy of Pediatrics. (2017). Caries prevention services reimbursement table (state specific Medicaid payment information). Retrieved from https://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Oral-Health/Map/Documents/OralHealthReimbursementChart.xlsx?Web=1
In a multivariable regression model, Table 3, children aged 2–3 years (odds ratio (OR)=1.87, 95% confidence interval (CI) =1.70, 2.07) and females (OR=1.11, 95% CI=1.02, 1.21) had significantly greater odds of having parent-reported very good or excellent teeth than males and children aged 4–6 years, respectively. Children who were White non-Hispanic, lived in families with incomes greater than 400% FPL, and had excellent physical health had significantly greater odds of having parent-reported very good or excellent teeth compared to all other racial/ethnic groups, children in families with lower household incomes, and children with worse physical health, respectively. Compared to children with private insurance, children with public insurance had significantly lower odds of having very good or excellent parent-reported teeth (OR=0.70, 95% CI=0.62, 0.81).
Table 3.
Results for logit model examining effect of Medicaid fluoride varnish policy on the odds of a child having very good or excellent teeth
| Variables | Odds Ratio (95% CI) |
|---|---|
| Key explanatory variables | |
| Years since state implemented Medicaid fluoride varnish policy (ref: no policy) | |
| <2 years | 0.93 (0.72 – 1.21) |
| 2 or 3 years | 0.92 (0.76 – 1.11) |
| 4 or more years | 0.78 (0.60 – 1.01) |
| Public health insurance (ref: private health insurance) | 0.70*** (0.62 – 0.81) |
| Public health insurance * Years since state implemented Medicaid fluoride varnish policy | |
| Public health insurance * Medicaid policy implemented <2 years ago | 1.21 (0.84 – 1.76) |
| Public health insurance * Medicaid policy implemented 2 or 3 years ago | 1.02 (0.82 – 1.28) |
| Public health insurance * Medicaid policy implemented 4 or more years ago | 1.28* (1.03 – 1.60) |
| Additional covariates | |
| Ages 2–3 years (ref: ages 4–6) | 1.87*** (1.70 – 2.07) |
| Female (ref: male) | 1.11* (1.02 – 1.21) |
| Race/ethnicity (ref: white, non-Hispanic) | |
| Black, non-Hispanic | 0.71*** (0.62 – 0.81) |
| Multi-racial/Other, non-Hispanic | 0.69*** (0.59 – 0.80) |
| Hispanic | 0.44*** (0.39 – 0.49) |
| FPL (ref: 400% FPL or more) | |
| Missing information on poverty | 0.60*** (0.50 – 0.71) |
| < 100% FPL | 0.47*** (0.40 – 0.55) |
| 100–199% FPL | 0.53*** (0.46 – 0.62) |
| 200–399% FPL | 0.77*** (0.67 – 0.88) |
| Child has a special health care need (CSHCN) | 0.94 (0.76 – 1.16) |
| Physical health status (ref: Excellent) | |
| Very Good | 0.56*** (0.50 – 0.63) |
| Good | 0.153*** (0.13 – 0.18) |
| Fair or Poor | 0.17*** (0.11 – 0.26) |
| CSHCN * Physical health status (ref: Excellent) | |
| CSHCN * Very good physical health | 1.32 (1.00 – 1.75) |
| CSHCN * Good physical health | 2.23*** (1.64 – 3.02) |
| CSHCN * Fair or poor physical health | 1.34 (0.78 – 2.28) |
| Survey year (ref: 2011) | |
| 2003 | 0.78** (0.66 – 0.91) |
| 2007 | 0.82** (0.70 – 0.95) |
|
| |
| Weighted N | 289,572 |
| Unweighted N | 68790 |
Model includes state fixed effects.
p<0.001,
p<0.01,
p<0.05
When examining the effect of state policies, controlling for individual and family characteristics, we found that fluoride varnish policies were associated with better oral health, but only after a time lag following enactment. Specifically, publicly insured children in states that had a fluoride varnish policy for four or more years had significantly greater odds of parent-reported very good or excellent teeth (OR=1.28, 95% CI=1.03–1.60) compared to publicly insured children in states without a policy. Among publicly insured children in states that had a fluoride varnish policy for fewer than 4 years, there was not a significant difference in oral health status compared to children in states without a policy.
Discussion
This study is the first national examination of the impact of state Medicaid policies supporting non-dental primary care providers to apply fluoride varnish on the oral health of publicly insured children, which revealed that publicly insured children in states that had fluoride varnish Medicaid policies for four or more years had significantly greater odds of reporting very good or excellent oral health compared to publicly insured children in states without policies. Our findings are consistent with studies reporting a time-lagged association between fluoride varnish policies and increased utilization among Medicaid-enrolled children (Herndon et al., 2015; Okunseri et al., 2010; Okunseri et al., 2009; Rozier et al., 2010) and two North Carolina studies that reported associations with reduced dental caries (Achembong, Kranz, & Rozier, 2014; Kranz et al., 2015). Our results examining individual level outcomes provide empirical support of the oral health benefits of the USPSTF endorsement of fluoride varnish application in primary care settings (Moyer, 2014).
Policy changes often take time to have an effect. The lagged effect observed here is likely due to both (1) the lag between policy implementation and adoption by non-dental primary care providers and (2) the lag between services provided and the effect on children’s oral health. Neither lag is unexpected. Providers often need time for training and changing workplace practices before beginning to provide a new service, and children need to obtain multiple applications of fluoride varnish to reduce dental caries (Kranz et al., 2015). Both factors may help to explain our finding and those of others (Arthur & Rozier, 2016) that there are no immediate changes in outcomes in the years immediately following fluoride varnish policy implementation. Importantly, however, we found that the benefits of fluoride varnish are realized relatively quickly after policy implementation. Improved oral health was observed within four years in our study and others have reported the potential for cost-savings due to fluoride varnish by 6 years of age (Stearns et al., 2012), substantially faster than other interventions such as smoking cessation that have effects 15 years later (Anthonisen et al., 2005).
Reducing the lag between policy implementation and delivery of services is important so that children start accruing benefits as soon as possible, and can potentially be addressed through improved policymaking. For example, policies vary in their training requirements, reimbursement rates, and patient eligibility criteria, which may affect increase or decrease the lag between policy implementation and delivery of services. Once a policy supporting reimbursement for fluoride varnish is enacted, physicians and other non-dental providers often need to obtain training to enable them to begin delivering fluoride varnish, and some states require in-person or online training before providers can obtain reimbursement (Arthur & Rozier, 2016; AAP, 2017). In addition to training requirements, states also vary in reimbursement rates and whether or not comprehensive services are reimbursed. Pediatricians have reported insufficient reimbursement and lack of oral health training as barriers to delivering fluoride varnish (Quinonez et al., 2014), suggesting policies addressing these concerns may bolster delivery of care. Future studies should explore how these varying policy characteristics may affect the lag between policy implementation and oral health.
Children insured by Medicaid and CHIP historically have fewer dental visits and worse oral health than privately insured children (Shariff & Edelstein, 2016; Vujicic & Nasseh, 2015), consistent with our finding that publicly insured children were less likely to have very good or excellent oral health than privately insured children. While delivering fluoride varnish in primary care settings can promote both access to preventive oral health services and oral health (Herndon et al., 2015; Okunseri et al., 2010; Okunseri et al., 2009; Rozier et al., 2010), state Medicaid fluoride varnish policies did not eliminate the disparity in oral health status between publicly and privately insured children. The combination of many factors affects oral health including diet, behavior, receipt of preventive dental care, timely treatment of dental problems, and parental knowledge and opinions about children’s oral health. Thus, strategies beyond fluoride varnish will be needed to reduce oral health disparities. Having pediatricians and dentists provide anticipatory guidance on oral health to parents of young children is one such strategy recommended by the American Association of Pediatric Dentistry and the American Association of Pediatrics (Bright Futures & AAP, 2017; American Academy of Pediatric Dentistry, 2016). Additionally, helping families with young children obtain a usual source of dental care can encourage receipt of timely preventive services and treatment. Moreover, because maternal oral health can effect the oral health of their children (Boggess & Edelstein, 2006), integrating oral healthcare into pregnancy is another recommended strategy for promoting young children’s oral health (Oral Health Care During Pregnancy Expert Workgroup, 2012). However, the link between medicine and dentistry remains tenuous, with physicians potentially under referring for oral health problems (Long et al., 2012) and children visiting medical offices for a first oral health visit having low rates of subsequent dental visits (Kranz et al., 2015). Thus, more work is needed to address the varied factors affecting oral health and to improve the linkage between medical and dental homes.
All state Medicaid programs support fluoride varnish application by primary care providers (Arthur & Rozier, 2016), yet commercial health insurers only recently began to reimburse for such applications, primarily in response to the Affordable Care Act’s (ACA) requirement effective May 2015 to cover all preventive services without cost sharing recommended by the USPSTF (Moyer, 2014). Better understanding the effects of such responses to the ACA among primary care providers and privately insured children are needed, particularly given recent findings that privately insured children younger than five years of age had equivalent or lower rates of dental care than publicly insured peers (Shariff & Edelstein, 2016). Furthermore, now that primary care providers can deliver fluoride varnish applications at no cost to all children, this may help to enhance delivery and help to reduce the lag between policy implementation and utilization because previously pediatricians have reported patients’ inability to pay for care as a barrier to the delivery of fluoride varnish (Quinonez et al., 2014).
We do not have clinical measures of oral health status, but instead use parents’ assessment of child oral health as our outcome, a variable associated with actual need (Talekar et al., 2005). Future studies should examine the impact of these policies on clinical measures of oral health. We are also unable to examine heterogeneity in outcomes within a state, as the publicly available version of the NSCH does not provide geographic identifiers smaller than the state-level. Additionally, we lack information on individual receipt of fluoride varnish, allowing us to comment only on the population health impact of these policies. We designed our empirical approach to mitigate threats to the validity of causal inference, identifying effects within each state based on policy change, and using privately insured children as additional controls for secular changes within a state. Although our design is strong, threats remain. For example, policy implementation could be an endogenous response to oral health needs in states. However, policies were adopted throughout the study period across numerous states, helping to mitigate this concern.
Our finding makes an important contribution by identifying and quantifying the oral health benefits of Medicaid policies that support application of fluoride varnish by primary care providers. This finding is particularly important given the disparities in access to care and oral health for publicly insured children compared to privately insured children (Shariff & Edelstein, 2016; Vujicic & Nasseh, 2015) and the extent to which poor oral health has been found to profoundly affect children’s quality of life (Filstrup et al., 2003; Jackson et al., 2011). Although we found benefits to oral health from such policies, the improvements in oral health were not realized until four or more years after policy implementation. To our knowledge, ours is the first study to provide national evidence of the oral health benefits that can be realized by the expansion of Medicaid benefits to cover fluoride varnish in primary care settings. Our focus was limited to the identification and quantification of oral health benefits, yet improved oral health outcomes may lead to many other important benefits that we have not attempted to quantify here, including those that may manifest more quickly following policy implementation. For example, others have documented the following outcomes associated with improved oral health among young children: reduced Medicaid expenditures for dental treatment (Stearns et al., 2012), fewer days absent from school (Jackson et al., 2011), and improved quality of life (Filstrup et al., 2003). As a result, the value of improvements in oral health that we have identified may substantially underestimate the total welfare improvements from such policies. Thus, such policies may be an efficient way of improving the quality of care provided by Medicaid and overall child health and well-being.
Significance.
What’s known on this subject
All state Medicaid programs support primary care providers’ application of fluoride varnish. State-level studies report that these policies increase fluoride varnish applications and reduce caries, yet no study has examined the national impact of these policies on children’s oral health.
What this study adds
This is the first national study examining the impact of Medicaid policies supporting primary care providers’ application of fluoride varnish on children’s oral health, finding that these policies help to improve the oral health of publicly insured children.
Acknowledgments
Funding: This study was supported by grant R01 DE026136-01 from the National Institute of Dental and Craniofacial Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Dental and Craniofacial Research or the National Institutes of Health.
References
- Achembong LN, Kranz AM, Rozier RG. Office-based preventive dental program and statewide trends in dental caries. Pediatrics. 2014;133(4):e827–e834. doi: 10.1542/peds.2013-2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Caries prevention services reimbursement table (state specific Medicaid payment information) 2017 Retrieved from https://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Oral-Health/Map/Documents/OralHealthReimbursementChart.xlsx?Web=1.
- American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. 2016 Retrieved from http://www.aapd.org/media/Policies_Guidelines/P_ECCClassifications.pdf. [PubMed]
- Anthonisen NR, Skeans MA, Wise RA, Manfreda J, Kanner RE, Connett JE. The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Annals of internal medicine. 2005;142(4):233–239. doi: 10.7326/0003-4819-142-4-200502150-00005. [DOI] [PubMed] [Google Scholar]
- Arthur T, Rozier RG. Provision of preventive dental services in children enrolled in Medicaid by nondental providers. Pediatrics. 2016;137(2):2015–3436. doi: 10.1542/peds.2015-3436. [DOI] [PubMed] [Google Scholar]
- Blackburn J, Morrisey MA, Sen B. Outcomes associated with early preventive dental care among Medicaid-enrolled children in Alabama. JAMA Pediatrics. 2017;171(4):335–341. doi: 10.1001/jamapediatrics.2016.4514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggess KA, Edelstein BL. Oral health in women during preconception and pregnancy: implications for birth outcomes and infant oral health. Maternal and Child Health Journal. 2006;10(1):169–174. doi: 10.1007/s10995-006-0095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchery E. Utilization of dental services among Medicaid-enrolled children. Medicare & Medicaid Research Review. 2013;3(3):e1–e14. doi: 10.5600/mmrr.003.03.b04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bright Futures & American Academy of Pediatrics. Recommendations for preventive pediatric health care. 2017 doi: 10.1542/peds.2017-0254. Retrieved from https://www.aap.org/en-us/documents/periodicity_schedule.pdf. [DOI] [PubMed]
- Cao S, Gentili M, Griffin PM, Griffin SO, Harati P, Johnson B, … Tomar S. Estimating demand for and supply of pediatric preventive dental care for children and identifying dental care shortage areas, Georgia, 2015. Public Health Reports. 2017;132(3):343–349. doi: 10.1177/0033354917699579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child and Adolescent Health Measurement Initiative. Children with special health care needs screener. 2017 Retrieved from http://www.cahmi.org/projects/children-with-special-health-care-needs-screener/
- Data Resource Center for Child and Adolescent Health. NSCH Survey Methodology. 2016 Retrieved from http://www.childhealthdata.org/learn/NSCH/resources/methods.
- Dye BA, Li X, Thornton-Evans G. Oral health disparities as determined by selected Healthy People 2020 oral health objectives for the United States, 2009–2010 [Internet] Hyattsville (MD): National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- Filstrup SL, Briskie D, Da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatric Dentistry. 2003;25(5):431–440. [PubMed] [Google Scholar]
- Hendrix KS, Downs SM, Brophy G, Carney Doebbeling C, Swigonski NL. Threshold analysis of reimbursing physicians for the application of fluoride varnish in young children. Journal of Public Health Dentistry. 2013;73(4):297–303. doi: 10.1111/jphd.12026. [DOI] [PubMed] [Google Scholar]
- Herndon JB, Tomar SL, Catalanotto FA, Vogel WB, Shenkman EA. The effect of Medicaid primary care provider reimbursement on access to early childhood caries preventive services. Health Services Research. 2015;50(1):136–160. doi: 10.1111/1475-6773.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children's oral health care: a qualitative study of carers of young children. Community Dentistry and Oral Epidemiology. 2007;35(6):429–438. doi: 10.1111/j.1600-0528.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. American Journal of Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranz AM, Preisser JS, Rozier RG. Effects of physician-based preventive oral health services on dental caries. Pediatrics. 2015;136(1):107–114. doi: 10.1542/peds.2014-2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranz AM, Rozier RG, Preisser JS, Stearns SC, Weinberger M, Lee JY. Examining continuity of care for Medicaid-enrolled children receiving oral health services in medical offices. Maternal and Child Health Journal. 2015;19(1):196–203. doi: 10.1007/s10995-014-1510-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long CM, Quinonez RB, Beil HA, Close K, Myers LP, Vann WF, Rozier RG. Pediatricians’ assessments of caries risk and need for a dental evaluation in preschool aged children. BMC Pediatrics. 2012;12(1):49. doi: 10.1186/1471-2431-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7(11) doi: 10.1002/14651858.CD002279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer VA. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102–1111. doi: 10.1542/peds.2014-0483. [DOI] [PubMed] [Google Scholar]
- Okunseri C, Szabo A, Garcia RI, Jackson S, Pajewski NM. Provision of fluoride varnish treatment by medical and dental care providers: variation by race/ethnicity and levels of urban influence. Journal of Public Health Dentistry. 2010;70(3):211–219. doi: 10.1111/j.1752-7325.2010.00168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okunseri C, Szabo A, Jackson S, Pajewski NM, Garcia RI. Increased children's access to fluoride varnish treatment by involving medical care providers: effect of a Medicaid policy change. Health Services Research. 2009;44(4):1144–1156. doi: 10.1111/j.1475-6773.2009.00975.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oral Health Care During Pregnancy Expert Workgroup. Oral health care during pregnancy: a national consensus statement. 2012 Retrieved from https://www.mchoralhealth.org/PDFs/OralHealthPregnancyConsensus.pdf.
- Pahel BT, Rozier RG, Stearns SC, Quiñonez RB. Effectiveness of preventive dental treatments by physicians for young Medicaid enrollees. Pediatrics. 2011;127(3):e682–e689. doi: 10.1542/peds.2010-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinonez RB, Kranz AM, Lewis CW, Barone L, Boulter S, O'Connor KG, Keels MA. Oral health opinions and practices of pediatricians: updated results from a national survey. Academic Pediatrics. 2014;14(6):616–623. doi: 10.1016/j.acap.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozier RG, Stearns SC, Pahel BT, Quinonez RB, Park J. How a North Carolina program boosted preventive oral health services for low-income children. Health Affairs. 2010;29(12):2278–2285. doi: 10.1377/hlthaff.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider D, Rossetti J, Crall JC. Assuring comprehensive dental services in Medicaid and Head Start programs: planning and implementation considerations. 2007 Retrieved from http://nmcohpc.net/resources/DentalServicesinMedicaidHeadStart.pdf.
- Seale NS, Casamassimo PS. Access to dental care for children in the United States: a survey of general practitioners. The Journal of the American Dental Association. 2003;134(12):1630–1640. doi: 10.14219/jada.archive.2003.0110. [DOI] [PubMed] [Google Scholar]
- Shariff JA, Edelstein BL. Medicaid meets its equal access requirement for dental care, but oral health disparities remain. Health Affairs. 2016;35(12):2259–2267. doi: 10.1377/hlthaff.2016.0583. [DOI] [PubMed] [Google Scholar]
- Stearns SC, Rozier RG, Kranz AM, Pahel BT, Quinonez RB. Cost-effectiveness of preventive oral health care in medical offices for young Medicaid enrollees. Archives of Pediatrics & Adolescent Medicine. 2012;166(10):945–951. doi: 10.1001/archpediatrics.2012.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children's oral health. The Journal of the American Dental Association. 2005;136(3):364–372. doi: 10.14219/jada.archive.2005.0179. [DOI] [PubMed] [Google Scholar]
- Vujicic M, Nasseh K. Health Policy Institute Research Brief. Chicago (IL): Health Policy Institute Research Brief American Dental Association; 2015. Gap in dental care utilization between Medicaid and privately insured children narrows, remains large for adults [Internet] (Revised)[cited 2016 May 17] Available from: http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0915_1.pdf. [Google Scholar]