Abstract
Objective:
Fluid loss during Ebola virus disease (EVD) infections from gastrointestinal dysfunction leads to volume depletion. It is possible that high environmental temperatures may exacerbate volume depletion or interfere with the provision of medical care by providers in full personal protective equipment. We investigated the effect of environmental temperature on case fatality.
Methods:
The International Medical Corps (IMC) operated 5 Ebola Treatment Units (ETUs) in Liberia and Sierra Leone during the 2014–16 epidemic. Demographic and outcomes variables for 465 patients with EVD were sourced from a de-identified, quality-checked clinical database collected by IMC. Daily environmental temperature data for Liberia and Sierra Leone were collected from a publicly available database (Weather Underground). Mean daily environmental temperatures were averaged across each patient’s ETU stay and environmental temperature thresholds were determined. Multiple logistic regression was utilized, with forward variable selection and threshold for entry of p<0.1. Statistical significance was defined as p<0.05. The following variables were analyzed as potential confounders: age, sex, ETU, length of ETU operation, and date of treatment.
Results:
Case fatality was 57.6% among patients diagnosed with EVD. Analysis of case fatality across environmental temperature quintiles indicated a threshold effect; the optimal threshold for average environmental temperature during a patient’s ETU stay was determined empirically to be 27.4°C (81.3°F). Case fatality was significantly greater for patients with average environmental temperatures above the threshold (70.4%) versus below (52.0%) (p<0.001). In multiple regression, patients with average environmental temperature above the threshold during their ETU stay were significantly more likely to die than patients below the threshold (aOR=2.5, 95% CI 1.6–3.8, p<0.001). This trend was observed only among patients treated in white tent ETUs, and not in ETUs with aluminum roofs.
Discussion:
These findings suggest that an average environmental temperature above 27.4°C (81.3°F) during patients’ ETU stay is associated with greater risk of death among patients with EVD. Further studies should investigate this effect. These results have potential implications for reducing case fatality through improved ETU construction or other temperature control methods within ETUs during future outbreaks.
Keywords: Ebola virus disease, environmental temperature, mortality, viral hemorrhagic fever
Introduction
The 2014–16 Ebola Virus Disease (EVD) epidemic in West Africa was the largest ever, infecting over 28,000 patients and claiming over 11,000 lives.[1] Persistence of Ebola virus (EBOV) in immune-privileged body fluids of survivors, as well as continued movement of communities into forested regions toward likely animal reservoirs of EBOV, make future epidemics likely.[2,3] Though the literature is growing, there remains a critical need for research on clinical management to improve treatment and survival for patients with EVD. In particular, multisite research derived from large patient populations is crucial to better inform future response programs. As previously reported, throughout the course of the 2014–16 epidemic, the International Medical Corps (IMC) developed a clinical database to fulfill these criteria, thereby providing a robust data cache to analyze factors that affect case fatality. [4–10]
There are no data on the effect of environmental factors on case fatality in patients with EVD, though investigation of the impact of environmental temperature on EVD prognosis is warranted. IMC Ebola Treatment Units (ETUs) were located in regions of Liberia and Sierra Leone classified as “monsoon” climate areas, where environmental temperatures are high. [11] With full Personal Protective Equipment (PPE) to prevent EBOV transmission, clinicians caring for patients with EVD were limited to patient contact times of approximately one hour due to the danger of overheating. Maynard et al. found that EVD providers in full PPE lose 0.014 kg/min body weight in midday hours from fluid loss. [12] Patients are also exposed to intense temperatures inside of ETUs, often structures built of plastic sheeting and exposed to long hours of direct sunlight due to the West African climate. Though the exact pathophysiological process that causes death in humans with EVD has not been confirmed, >75% of individuals with EVD experience vomiting and diarrhea, which can reach volumes of 5–10 l per day.[9,13] Fluid and electrolyte replacement are considered some of the most important aspects of EVD care.[14,15] Severely depleted intravascular volume may lead to hypotension and inadequate perfusion of vital organs, and is associated with poorer prognosis.[15] As high environmental temperature directly affects fluid loss, its impact on EVD outcomes may be significant.
Though previous research has investigated the effect of temperature as a predictor for EVD transmission [16,17], there have been no studies to date investigating the effects of environmental temperature on case fatality among EVD patients. We sought to assess the impact of environmental temperature on case fatality of EVD patients treated at IMC ETUs during the 2014–16 EVD epidemic.
Methods
Study Design, Patient Population & Ethics
The humanitarian organization IMC operated five ETUs in Liberia and Sierra Leone during the EVD epidemic. This retrospective cohort study analyzed data collected during care provision for patients with EVD admitted to IMC ETUs between September 2014 and September 2015. All patients with available outcome data were included in the study. The five ETUs were located in Bong and Margibi Counties in Liberia and in Port Loko District, Bombali District, and Kambia District in Sierra Leone. The University of Liberia - Pacific Institute for Research & Evaluation Institutional Review Board (UL-IRB), the Sierra Leone Ethics and Scientific Review Committee, and the Lifespan (Rhode Island Hospital) Institutional Review Board all granted ethical approval and exemption from informed consent for this study.
Data Collection & Management
Demographic and outcome (i.e. survived versus deceased) data were collected upon patient triage and discharge. Clinical data were recorded on standardized forms by trained providers during the course of patient care. Data from all 5 IMC ETUs were combined into a unified, de-identified database as previously reported. [4] Data were quality-checked using a lot quality assurance sampling (LQAS) method. Using iterative data entry, the LQAS process achieved 99% accuracy vs. source clinical data, as previously described. [4]
Historical daily environmental temperature data for Liberia and Sierra Leone were collected from Weather Underground, a publicly available, crowd-sourced database. Historical environmental temperature data for the study period were only available from international airport locations – Lungi International Airport in Sierra Leone and Roberts International Airport in Liberia. Therefore, these data do not have ideal geographic precision. However, previous studies used temperature measurements from Freetown, Sierra Leone to assess the effect of environmental temperature on EVD transmission across Sierra Leone.[17] Sierra Leone has an area of 71,740 km2 and is divided into two regions by the Köppen-Geiger Climate Classification system, which is one of the most commonly-used worldwide climate classification systems.[11,18] Lungi International Airport (Lungi, Sierra Leone) and all three IMC ETUs were located in the same “Monsoon” classification area (Figure 1). Liberia has an area of 111,369 km2 and is divided into three Köppen-Geiger Climate Classification areas - Roberts International Airport and both IMC ETUs in Liberia were situated within the same “Monsoon” classification area (Figure 1). [11,19]
Figure1:
Distribution of geographic origin of patients with confirmed EVD treated at IMC ETUs (reproduced with permission from Roshania et al. 2016).
Data Analysis
Mean daily environmental temperatures were averaged during each patient’s ETU stay. Only 1.8% of the 163 days of ETU operation in Liberia had missing temperature data, and 7.0% of the 300 days of ETU operation in Sierra Leone had missing temperature data. With one exception, missing temperature data did not exceed two consecutive days. Missing temperature data were filled in with the average of the previous and subsequent day of available data. This method was based on the assumption that environmental temperature on a particular day is likely to be similar to the previous and subsequent days, and that other variables in the dataset could not be used to impute missing temperature data. Age categories were selected based on the results of previous analyses of the impact of age on case fatality using the IMC EVD database. [4]
Analysis of average environmental temperature quintiles revealed a nonlinear association of environmental temperature and case fatality, with a threshold effect occurring at the fifth quintile. The optimal environmental temperature threshold was then determined using the cutpt package and the Liu method, which empirically determines the threshold that maximizes the product of specificity and sensitivity. The following variables were analyzed as potential confounders: age, sex, ETU, length of ETU operation, and weeks since the opening of the first IMC ETU. Univariate analyses for categorical and continuous variables were conducted using logistic regression. Multiple logistic regression with forward variable selection and threshold for entry of p<0.1 was subsequently used to assess independent variable association with case fatality. ETU was removed from multiple logistic regression analysis due to collinearity with the variable specifying the number of weeks since the opening of the first IMC ETU. This relationship was observed by regressing the number of weeks since the opening of the first IMC ETU against the other potential confounding variables.
The interaction between ETU structure type, environmental temperature, and death was analysed via a separate multivariable logistic regression model. ETUs at Makeni, Lunsar, and Margibi were standard, white tents, with an outer tent composed of 450–550 gsm PVC-coated fabric 5000 mm, and an inner tent composed of 120 gsm Poly-Cotton. ETUs at Kambia and Bong were constructed with aluminum roofs and either brick (Kambia) or blue-tarp walls (Bong). An interaction term between ETU structure type and environmental temperature threshold was included in this model, and odds ratios of death were generated for each structure classification. Analyses were completed in Stata 14.2. Statistical significance was defined as p<0.05, with p-values derived from Z-scores in regression analysis.
Results
Population Characteristics
470 patients diagnosed with EVD were admitted during the study period, of whom five were transferred to other facilities and excluded from analysis. Among all EVD patients with available survival data (n=465), case fatality was 57.6%. Females accounted for 60.0% of the study population (Table 1). 9.9% of the patients (n=46) were under-fives, 48.0% (n=223) were 5–34 years, and 42.0% (n=195) were 35 or older.
Table 1:
Descriptive Statistics and Univariate Analyses
| Variable | Patients | Percentage | Mortality (%) | P |
|---|---|---|---|---|
| ETU | 0.234 | |||
| Bong | 173 | 37.4 | 54.3 | |
| Kambia | 32 | 6.9 | 68.8 | |
| Lunsar | 146 | 31.5 | 59.6 | |
| Makeni | 109 | 23.1 | 58.7 | |
| Margibi | 5 | 1.1 | 20.0 | |
| Patient Age | <0.001 | |||
| 0–4 | 46 | 9.9 | 89.1 | |
| 5–34 | 223 | 48.0 | 44.0 | |
| 35+ | 195 | 42.0 | 66.2 | |
| Patient Sex | 0.497 | |||
| Female | 277 | 60.0 | 57.4 | |
| Male | 187 | 40.0 | 58.3 | |
| Average Environmental Temp | <0.001 | |||
| <27.4°C | 323 | 69.8 | 52.0 | |
| >27.4°C | 140 | 30.2 | 70.4 |
Univariate Analyses for Average Environmental Temperature
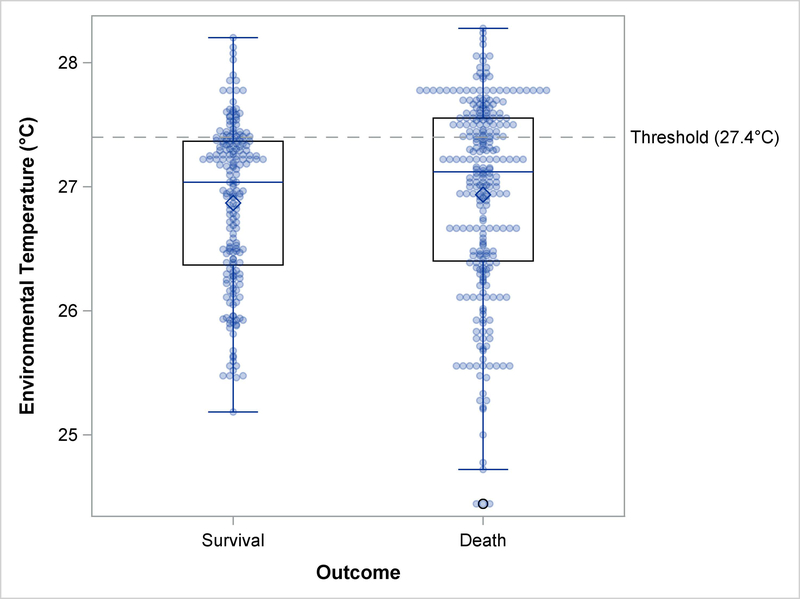
Univariate analysis of case fatality across environmental temperature quintiles indicated that the relationship between environmental temperature and case fatality was nonlinear; graphical analysis revealed an increase in case fatality at the fifth quintile only (Figure 2). The optimal threshold for average environmental temperature across a patient’s ETU stay was determined empirically to be 27.4°C (81.3°F); the distribution of environmental temperatures by clinical outcome is depicted in Figure 3. Univariate analysis of average environmental temperature across a patient’s ETU stay vs. case fatality revealed a significant difference of 52.0% case fatality below the threshold vs. 70.4% above the threshold (p<0.001) (Table 1).
Figure2:
Case fatality across average environmental temperature quintiles.
Figure3:
Distribution of average environmental temperature by survival status.
Univariate Analyses for Confounding Variables
There was no difference in case fatality between males and females (58.3% and 57.4% case fatality, respectively; p=0.497), and no significant difference in case fatality across the five ETUs (case fatality of 54.3% at Bong, 68.8% at Kambia, 59.6% at Lunsar, 58.7% at Makeni, and 20.0% at Margibi; p=0.234) (Table 1). Univariate analysis demonstrated that case fatality was higher among patients under 5 years of age (89.1% case fatality) and among patients 35 years and older (66.2% case fatality) than among other age groups (44.0% case fatality) (p<0.001) (Table 1).
The number of weeks since the opening of the first IMC ETU was not significantly different between surviving and deceased patients (p=0.895) (Table 2). The number of weeks from the opening of each ETU until the date of patient triage into that particular ETU approached significance, with longer time open associated with lower case fatality (p=0.076) (Table 2).
Table 2:
Descriptive Statistics and Univariate Analyses
| Variable | OR | 95% CI | P |
|---|---|---|---|
| Number of Weeks from ETU Opening to Patient Triage | 0.974 | 0.947–1.003 | 0.076 |
| Number of Weeks Since the Opening of the First IMC ETU | 1.001 | 0.985–1.018 | 0.895 |
Multivariable Analyses
In multiple logistic regression, patients with average environmental temperature greater than the threshold during their ETU stay had significantly higher odds of death than patients below the threshold (aOR=2.5, 95% CI 1.6–3.8, p<0.001). Patient ages less than 5 years (aOR 14.3, 95% CI 5.1–39.7, p<0.001) or 35 and older (aOR 2.6, 95% CI 1.7–4.0, p<0.001) were associated with increased case fatality, and number of weeks from ETU opening to patient triage (aOR 0.95, 95% CI 0.92–0.98, P=0.003) was associated with decreased case fatality (Table 3).
Table 3:
Multivariable Analysis of EVD Case Fatality. Note: Odds ratio for ETU operation duration reflects incremental change per week open. ‘Ref.’ denotes the reference level for each variable.
| Variable | OR | 95% CI | P |
|---|---|---|---|
| Average Environmental Temperature (ref. = Under 27.4° Celsius) | |||
| Over 27.4° Celsius | 2.5 | 1.6–3.8 | <0.001 |
| Patient Age (ref. = 5 to 34) | |||
| 0 to 4 | 14.3 | 5.1–39.7 | <0.001 |
| 35+ | 2.6 | 1.7–4.0 | <0.001 |
| Length of ETU Operation | |||
| Weekly Change | 0.95 | 0.92–0.98 | 0.003 |
ETU Structure Sub-analysis
Of the 465 EVD-positive patients treated during the study period, 260 were treated in ETUs located in standard white tents, and 205 were in aluminum-roofed structures. The odds of fatality did not differ significantly between these two groups (aOR 0.93 in aluminum-roofed structures vs. tents, 95% CI 0.6–1.1, p=0.684). Acknowledging that ETU material likely affects the indoor temperature inside of an ETU, and that the association between environmental temperature and case fatality may then vary between different types of ETUs, we conducted a sub-analysis to assess the interaction among environmental temperature, ETU material, and case fatality. In multivariable analysis, among patients treated in tents, environmental temperature above vs. below threshold was associated with higher odds of death (aOR 3.89, 95% CI 2.12–7.15, p<0.001). Among patients treated in aluminum-roofed structures, environmental temperature was not significantly associated with death (aOR 1.27, 95% CI 0.64–2.52, p=0.485). The difference between odds ratios for the two structure types was statistically significant (p=0.016). The temperature threshold remained at 27.4°C (81.3°F) when including only patients treated in tent ETUs.
Discussion
This is the first study to investigate the effect of environmental temperature on case fatality in EVD. In multivariable analyses, the odds of death were over two and a half times higher among EVD patients for whom the average environmental temperature was above 27.4 °C (81.3°F) during their ETU stay as compared to those with averages below 27.4 °C. Sub-analysis by ETU structure type revealed that this effect was only significant among patients treated in ETUs set up in white tent structures. These results suggest that environmental temperature should be considered in future EVD response efforts and that the adjustment of indoor temperature, especially through the construction of cooler ETUs, could potentially reduce case fatality in future outbreaks.
These findings have potential implications for the way ETUs are built or modified and should inform biomedical engineering. They suggest that standard white tents should be replaced with structures that retain less heat, such as structures with aluminum or other reflective roofs. Another option is to find innovative approaches to ETU construction that reduce heat. In 2015, four ETUs were built with the goal of controlling temperature. Citing Liberia’s climate and hot environmental temperatures, the Welthungerhilfe, a German non-governmental organization funded by USAID, constructed four bamboo-walled ETUs to minimize captured heat. [20] Installation of air conditioning systems in ETUs is another option for achieving climate control, but may not be possible in all ETUs due to high costs for installation and utilization in low- and middle-income countries (LMIC). If significant increases in EVD case fatality at higher average environmental temperatures are confirmed in future studies, more intense efforts should be made to improve temperature control in ETUs.
Additional follow-up studies should explore why environmental temperatures affect EVD case fatality to better disentangle the impacts on patient physiology versus inhibition of care delivery. The threat of overheating and fluid loss for EVD providers in full PPE limits the amount of time that can be spent caring for patients. [12] It is possible that on days with relatively higher ambient temperatures, the amount of time providers can spend with patients is further limited, and that this could negatively impact patient outcomes. Alternatively, higher environmental temperatures could increase fluid losses, exacerbating the effects of gastrointestinal losses from EVD and insensible losses via hyperpyrexia compensatory physiological responses leading to increased volume depletion and higher case fatality. [9,13,15] In such a case, the prevention, identification, and treatment of dehydration may be of particular importance when environmental temperature is high. It is also possible that the association between heat and case fatality is influenced by other confounding variables yet to be adequately identified. An unlikely explanation for our findings is that the average environmental temperature across ETU stays was higher among deceased patients because the duration of ETU stay among deceased patients was shorter on average than that among patients who survived, as previously reported in the analyses using this dataset. [4] Shorter ETU stays could lead to more aberrant average environmental temperatures; as fewer days are included in the average. However, this interpretation is highly unlikely, as we would expect to also see higher case fatality among patients with the lowest environmental temperature averages, which we did not find in our analysis.
This study’s main limitation was the location from which the temperature data were sourced, and that indoor daily temperatures for each ETU were not available. Therefore, our environmental temperature data serve as an indirect proxy variable for the indoor daily temperatures at each ETU. Historical environmental temperature data for the study period could only be found at international airport locations in Sierra Leone and Liberia. Environmental temperatures at these locations likely differ slightly from the exact temperatures inside of the IMC ETUs. However, as described in the methods section, the IMC ETUs were in reasonable proximity to the airports, and their locations were within the same Köppen-Geiger Climate Classification areas. Further, previous research has shown that temperature measured inside of tent structures can be higher than environmental temperature and varies between tents constructed with different materials, but that indoor temperature was correlated with outdoor environmental temperature throughout the day regardless of tent material. [21] Overall, this suggests that temperature data used in this analysis is an adequate proxy with which to analyze these effects. [11] Follow-up studies should further explore the effect of temperature on EVD case fatality outcomes using temperature data sourced from inside each individual ETU. It is also important to emphasize that the observed threshold of 27.4°C (81.3°F) reflects only environmental temperature and not temperature inside of the ETUs. It is almost certain that any threshold calculated using temperatures inside ETUs would differ from that observed in the present study.
This analysis is limited by its retrospective design and our inability to control for all relevant factors that may have influenced case fatality. In particular, increased viral load and decreased polymerase chain reaction (PCR) cycle threshold (CT) values, which inversely approximate viral load, have been shown to be significantly associated with case fatality in EVD. [22–25] Neither viral load nor PCR CT value were controlled for in this study. Similarly, specific symptoms have been associated with case fatality in EVD, and symptoms were not included in this study. [9,23–24]
In conclusion, patients treated in white tents with an average environmental temperature >27.4 °C (81.3°F) during their ETU stay had significantly higher odds of death than patients below the threshold. Follow-up studies are needed to confirm these results using temperature data from inside ETUs, and to find out why environmental factors seem to impact EVD clinical outcomes. Given the high case fatality associated with EVD, all approaches with the goal of reducing case fatality – including clinical, environmental, and others –should be explored. This study suggests that avoiding white tent structures or installing temperature control in ETUs could reduce case fatality in future EVD outbreaks.
Acknowledgements
We would like to thank International Medical Corps and the governments of Liberia, Sierra Leone, and Guinea for contributing to the humanitarian response and providing data for this study. We would also like to thank all of the generous institutional, corporate, foundation, and individual donors who placed their confidence and trust in International Medical Corps and made its work during the Ebola epidemic possible. Finally, we would also like to thank International Medical Corps’ clinical, water, sanitation, and hygiene (WASH), and psychosocial teams as well as all of the monitoring and evaluation staff, including the data collection officers at each of the ETUs.
Funding for this study was provided by the National Institutes of Health (NIH), National Institute of Allergy and Infectious Diseases (R03AI132801), and by the Summer Assistantship Program at the Warren Alpert Medical School of Brown University. The funding sources had no involvement in the design or conduct of the study or the decision to submit for publication. Preliminary results from this work were presented at the 2017 American Society for Tropical Medicine and Hygiene Conference in Baltimore, MD.
References
- 1.Centers for Disease Control and Prevention (CDC). Outbreaks Chronology: Ebola Virus Disease. https://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html. Accessed January 7, 2018.
- 2.Diallo B, Sissoko D, Loman NJ, et al. Resurgence of Ebola Virus Disease in Guinea Linked to a Survivor with Virus Persistence in Seminal Fluid for More Than 500 Days. Clin Infect Dis. 2016;63(10):1353–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rulli MC, Santini M, Hayman DT, D’Odoroci P. The nexus between forest fragmentation in Africa and Ebola virus disease outbreaks. Sci Rep. 2017; 7:41613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roshania R, Mallow M, Dunbar N, et al. Successful implementation of a multicountry clinical surveillance and data collection system for Ebola virus disease in West Africa: findings and lessons learned. Glob Health Sci Pract. 2016;4(3):394–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smit MA, Michelow IC, Glavis-Bloom J, Wolfman V, Levine AC. Characteristics and Outcomes of Pediatric Patients with Ebola Virus Disease Admitted to Treatment Units in Liberia and Sierra Leone: A Retrospective Cohort Study. Clin Infect Dis. 2017;64(3):243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steinhubl SR, Feye D, Levine AC, Conkright C, Wegerich SW, Conkright G. Validation of a portable, deployable system for continuous vital sign monitoring using a multiparametric wearable sensor and personalised analytics in an Ebola treatment centre. BMJ Glob Health. 2016;1(1):e000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine AC, Shetty PP, Burbach R, et al. Derivation and Internal Validation of the Ebola Prediction Score for Risk Stratification of Patients with Suspected Ebola Virus Disease. Ann Emerg Med. 2015;66(3):285–293. [DOI] [PubMed] [Google Scholar]
- 8.Waxman M, Aluisio AR, Rege S, Levine AC. Characteristics and survival of patients with Ebola virus infection, malaria, or both in Sierra Leone: a retrospective cohort study. Lancet Infect Dis. 2017;17(6):654–660. [DOI] [PubMed] [Google Scholar]
- 9.Skrable K, Roshania R, Mallow M, Wolfman V, Siakor M, Levine AC. The natural history of acute Ebola virus disease among patients managed in five Ebola treatment units in West Africa: A retrospective cohort study. PLoS NTD. 2017;11(7): e0005700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henwood PC, Bebell LM, Roshania R, et al. Ebola Virus Disease and Pregnancy: A Retrospective Cohort Study of Patients Managed at 5 Ebola Treatment Units in West Africa. Clin Infect Dis. 2017;65(2):292–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Maps of Köppen-Geiger Climate Classification. World Map of the Köppen-Geiger Climate Classification Updated. http://koeppen-geiger.vu-wien.ac.at/present.htm. Accessed January 7, 2018.
- 12.Maynard SL, Kao R, Craig DG. Impact of personal protective equipment on clinical output and perceived exertion. J R Army Med Corps. 2016;162(3):180–3. [DOI] [PubMed] [Google Scholar]
- 13.Bishop BM. Potential and emerging treatment options for Ebola virus disease. Ann Pharmacother. 2015;49(2):196–206. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC). Ebola Virus Disease Information for Clinicians in U.S. Healthcare Settings; https://www.cdc.gov/vhf/ebola/healthcare-us/preparing/clinicians.html. Accessed January 7, 2018. [Google Scholar]
- 15.Bray M, Chertow DS. Treatment and prevention of Ebola virus disease - UpToDate. https://www-uptodate-com.revproxy.brown.edu/contents/treatment-and-prevention-of-ebola-virus-disease?source=see_link§ionName=Prognosticfactors&anchor=H132411-H132411. Accessed January 7, 2018.
- 16.Zinszer K, Morrison K, Verma A, Brownstein JS. Spatial Determinants of Ebola Virus Disease Risk for the West African Epidemic. PLoS Curr. 2017;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang LQ, Yang Y, Jiang JF, et al. Transmission dynamics of Ebola virus disease and intervention effectiveness in Sierra Leone. Proc Natl Acad Sci U S A. 2016;113(16):4488–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Central Intelligence Agency (CIA). The World Fact book - Sierra Leone. https://www.cia.gov/library/publications/the-world-factbook/geos/sl.html. Accessed January 7, 2018.
- 19.Central Intelligence Agency (CIA). The World Fact book - Liberia. https://www.cia.gov/library/publications/the-world-factbook/geos/li.html. Accessed January 7, 2018.
- 20.Han C Breaking New Ground: A Different Approach to Building Ebola Clinics in Liberia. USAID Impact. https://blog.usaid.gov/2015/01/breaking-new-ground-a-different-approach-to-building-ebola-clinics-in-liberia/. Accessed January 7, 2018.
- 21.Zhang L, Meng X, Lui F, Xu L, Long E. Effect of retro-reflective materials on temperature environment in tents. Case Studies in Thermal Engineering. 2017; 9:122–127. [Google Scholar]
- 22.Crowe SJ, Maenner MJ, Kuah S, et al. Prognostic Indicators for Ebola Patient Survival. Emerg Infect Dis. 2016;22(2):217–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J, Duan HJ, Chen HY, et al. Age and Ebola viral load correlate with mortality and survival time in 288 Ebola virus disease patients. Int J Infect Dis. 2016; 42:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Rong Y, Sun L, et al. Prognostic Analysis of Patients with Ebola Virus Disease. PLoS Negl Trop Dis. 2015;9(9): e0004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crowe SJ, Maenner MJ, Kuah S, et al. Prognostic Indicators for Ebola Patient Survival. Emerg Infect Dis. 2016;22(2):217–23. [DOI] [PMC free article] [PubMed] [Google Scholar]