Abstract
Relatively consistent findings from recent studies using population-level data identify heightened physical and psychiatric morbidity in autistic people compared to the general population. Health problems that commonly present with autism spectrum disorder (ASD) are generally discussed in the literature as ‘co-occurring’ or ‘comorbid’ regardless of their known or hypothesized causal mechanisms. In this commentary, we introduce a new temporally-focused terminology to describe health conditions that present with ASD. Emphasizing the temporal development of health conditions in research will help the field to understand whether conditions are: (1) ‘truly co-occurring’ (share an etiologic origin with ASD in utero, are a defining characteristic of a subphenotype), (2) ‘resulting’ (caused by ASD related disparity or the health effect of behaviors developed to cope with ASD symptoms); or (3) ‘associated’ (conditions more common in individuals with ASD with etiology not yet known or hypothesized; or an artifact of diagnostic process or trends). Whether a health condition is ‘truly co-occurring,’ ‘resulting,’ or ‘associated’ has implications for how we design interventions to prevent and treat health conditions in people on the autism spectrum. Ultimately, we think that using clear and temporally-focused language can set us on a path to better deduce etiology and develop effective prevention and intervention efforts for health conditions that impact the lives of autistic individuals. We hope that this approach to temporal language to describe health conditions that present with ASD promotes thought and discussion in the research, advocate, and autistic community.
Keywords: health, mental health, epidemiology, aging
Lay Abstract
Research finds autistic people have more health problems than the general population but we do not understand why. In this commentary, we argue researchers need to use language describing the timing of health problems in autistic people, specifying whether problems truly co-occur (share a cause), result from autism-related disparities, or are more common in autistic people for an unknown reason. Clarifying language can provide more specificity in research and improve efforts to prevent and treat health problems in autistic people.
Health conditions1 that present with autism spectrum disorder (ASD), as well as health management, are nearly universal parts of the lived experience for people on the autism spectrum. With prompting from the advocate community (Pellicano, Dinsmore, & Charman, 2014; Warner, Parr, & Cusack, 2018), researchers have increased urgency and focus on health problems in autism. For example, a number of groups recently published significant papers on health conditions that present with ASD using population-level data (Bishop-Fitzpatrick et al., 2018; Croen et al., 2015; Davignon, Qian, Massolo, & Croen, 2018; Levy et al., 2010; Maddox, Kang-Yi, Brodkin, & Mandell, 2018; Shea et al., 2018), confirming the high prevalence of conditions in children and adults with ASD compared to the general population, and what appears to be a growing disparity in health over the life course. Echoing this intensifying focus, the US Interagency Autism Coordinating Committee (IACC) created an objective in their 2016–2017 strategic plan to “Support research and implement approaches to reduce disabling co-occurring health conditions in adults with ASD, with the goal of improving safety, reducing premature mortality, and enhancing quality of life” (IACC, 2017).
We believe the field needs to move towards a cohesive research agenda geared at understanding, preventing, and intervening on mechanisms underlying the development of health conditions at the patient, provider, systems, and population level. A more cohesive and temporally focused research agenda will also help the field to identify and reduce the disparities that individuals on the spectrum face. The first step in this process is to clarify the language we use to characterize health conditions that present with ASD. Just as the medical terminology used around ASD influences the research agenda focused on cause and cure (Lai, Lombardo, & Baron-Cohen, 2014). Similarly, we assert that using specific, temporal language around health conditions that present with ASD will move the field in a more meaningful direction. The objective of this commentary is to introduce a temporally focused terminology to describe health conditions that present with ASD. We hope that this more specific language will refocus work towards deducing etiology and motivating prevention and intervention, with the ultimate goal of helping people on the autism spectrum live long, healthy, and self-determined lives in their communities.
A New Framework for Health Conditions that Present with ASD
In the medical literature, there is a general ambiguity in terminology around health conditions that present with an index condition (i.e., the condition of interest; Valderas, Starfield, Sibbald, Salisbury, & Roland, 2009). In the existing ASD literature, ‘co-occurring’2 is often used to cover all health conditions that occur more often in people on the spectrum than in the general population. While the seminal paper by Caron and Rutter (1991) outlined some of these issues, we believe that the field is at a juncture where increased emphasis on when conditions develop is crucial. A temporally-focused approach may allow us to determine whether conditions are (1) ‘truly co-occurring’ (share an etiologic origin with ASD in utero, and are a defining characteristic of a subphenotype), (2) ‘resulting’ (caused by ASD related disparity or the health effect of behaviors developed to cope with ASD symptoms); or (3) ‘associated’ (etiology not yet known or hypothesized; or an artifact of diagnostic process or trends). Whether a health condition falls in each of these temporal categories has implications for how we design interventions to prevent or treat a said condition.
Given the heterogeneity of both autism and general human health, conditions may develop at different times for different individuals through different ‘resulting’ mechanisms. For instance, a person on the autism spectrum could have cardiovascular disease that develops either congenitally or during middle age, and prevention and treatment strategies would differ based on temporal origin. The examples presented illustrate a pattern of temporal thinking rather than an attributional causal mechanism for all instances of the health condition. Further, given increased awareness of and access to diagnosis of ASD we recognize that there are cohort effects that may impact the phenotypic profile and potential dual diagnoses individuals on the spectrum with formal ASD diagnoses can have (i.e., attention deficit hyperactivity disorder could not be co-diagnosed with ASD in DSM-IV); these factors mainly impact how and when health conditions are identified in older cohorts of people with identified ASD for whom we have less longitudinal and lifespan data. However, the importance of temporal thinking still applies to earlier generations who may not have received formal diagnoses in childhood but still experience increased physical and psychiatric morbidity throughout their lives. Figure 1 presents our framework with examples.
Figure 1.
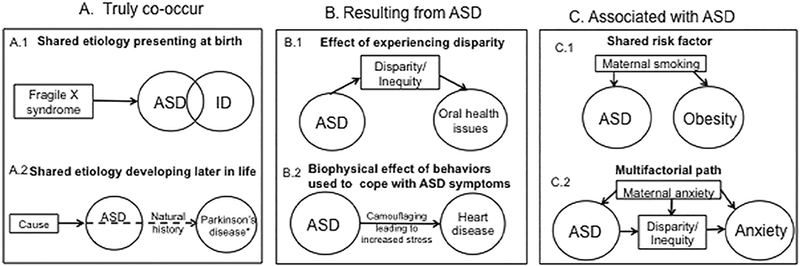
Models for health conditions that present with autism spectrum disorder
*Since we know very little about health conditions in older adults with ASD, we highlight a potential condition (Parkinson’s disease) that has been hypothesized to share an etiologic link with ASD but would not present until later in life (Starkstein, Gellar, Parlier, Payne, & Piven, 2015). We convey this uncertainty with a dashed line.
In all models, the time scale begins with development of ASD (in utero) with right facing arrows indicating the forward movement of time.
Health conditions that truly co-occur.
Conditions that truly co-occur may be pivotal in parsing heterogeneity in ASD etiology and phenotype (Wiggins et al., 2017) and should guide efforts to reduce exposure to risk factors with the goal of reducing the incidence of health conditions (primary prevention) and alleviate the burden of health conditions and their interaction with ASD symptomatology (tertiary prevention). Causally, a given health condition may be part of an ASD subphenotype and be intrinsic to the presentation of an identified, or yet to be identified, subgroup (Figure 1.A.1). For example, fragile X syndrome and tuberous sclerosis have known genetic origins that are likely causal for both ASD and the genetic condition. Although specific origins have yet to be identified, epilepsy and intellectual disability are conditions that develop in utero and are found to be markers of distinct subgroups in data-driven approaches (Wiggins et al., 2017). Due to the near paucity of studies characterizing the health conditions of older-adults with ASD, there may be ‘truly co-occurring’ conditions that do not manifest until older adulthood (e.g., Parkinsonism; Starkstein, Gellar, Parlier, Payne, & Piven, 2015) that we do not have enough evidence of to make inference on (Figure 1.A.2).
In assessing etiologic mechanisms for conditions with this temporal order, close consideration should be given to in utero development, perinatal risk factors, shared genetic origins, and their effects across the life course.
Health conditions resulting from ASD.
Recent, population-level studies present relatively consistent findings that people on the autism spectrum experience increased morbidity in areas unrelated to the core features of ASD compared to the general population (Bishop-Fitzpatrick et al., 2018; Croen et al., 2015; Davignon et al., 2018; Levy et al., 2010; Shea et al., 2018). Although this area of research has yet to be fully developed, the presence of morbidity unrelated to core features of ASD suggests that many health conditions that commonly present with ASD do not mechanistically co-occur, but are instead related to health and healthcare access disparities that are part of the lived experience for people on the autism spectrum (Figure 1.B.1). People on the autism spectrum are frequently excluded from full and meaningful participation in their communities, resulting in social isolation, economic injustice, and a lack of opportunities. In addition, they may receive substandard healthcare compared to people in the general population. For example, sensory stimuli in dental visits may lead to an avoidance of dental care, leading to an increase in periodontal disease compared to the general population (Gandhi & Klein, 2014). ASD-specific access and health disparities, possibly compounded by other racial, ethnic, or economic disparity (e.g., ‘double hit’; Krahn, Hammond, & Turner, 2006), lead to poorer health outcomes.
Research from the general population suggests that health conditions result from the experience of social and economic injustice throughout life (Sanbonmatsu et al., 2012). We have reason to believe that experienced injustice would also affect people on the autism spectrum (Bishop-Fitzpatrick & Kind, 2017). Similarly, a lifetime of being on the autism spectrum may lead to the development of a chronic health condition through the biophysical impacts of autistic traits. There may also be a natural course of ASD leading to development of health conditions (Figure 1.B.2). For example, amplified cortisol (Spratt et al., 2012) and cardiovascular reactivity (Bishop-Fitzpatrick, Minshew, Mazefsky, & Eack, 2017) to social stressors may be associated with identified heightened rates of cardiovascular disease in later life (Bishop-Fitzpatrick et al., 2018; Croen et al., 2015).
Health conditions associated with ASD.
Because of the innovative use of large data we are now aware of many conditions that present more often in people on the spectrum, without necessarily having pre-specified causal hypotheses (either biological or sociological). Given the lack of mechanistic understanding, we believe that a conservative use of language is warranted. We propose the term ‘associated’ conditions for health conditions that are more prevalent in individuals on the spectrum where the scientific literature does not yet have testable and consistent hypotheses based on mechanistic development. In our proposed framework, the key to differentiating ‘resulting’ conditions from ‘associated’ conditions is the availability of data or hypotheses that suggest mechanisms underlying timing of onset. A ‘resulting’ condition has a temporal origin after ASD onset whereas an ‘associated’ condition has a temporal origin that is not yet known. Given that we do not know the temporal origins of ‘associated’ conditions, identifying their temporal origin should be at the forefront of our research on these ‘associated’ conditions.
Diagnosing ASD and other health conditions among individuals on the spectrum is difficult, which may account for the abundance of ‘associated’ conditions. Individuals may be erroneously diagnosed with a condition that presents similarly to ASD (general developmental delay, speech language impairment) and carry these diagnoses for years, altering treatment programs (Rubenstein et al., 2018). Individuals may later acquire an ASD diagnosis and retain the original diagnosis (diagnostic accretion) or lose the original diagnosis (diagnostic substitution). In population level data, these individuals may carry previous diagnoses as an artifact but not truly have these conditions that alter our treatment approaches.
Additionally, ‘associated’ health conditions may share risk factors with ASD, but develop through differing etiologies. These ‘associated’ conditions are most visible in large population-based studies where we have increased power to see effects in smaller subsets of the population. Health conditions with shared risk factors are more common in individuals with ASD compared to the general population, based on exposure to the risk factor but etiological mechanisms caused by that exposure likely differ (Figure 1.C.1). For example, maternal smoking during pregnancy is both a risk factor for ASD (Kalkbrenner, Schmidt, & Penlesky, 2014) and childhood obesity (Toschke, Montgomery, Pfeiffer, & von Kries, 2003) but it is unlikely that these conditions share an etiologic mechanism, given the vast effect of maternal smoking during pregnancy on genetic and epigenetic alterations (Barua & Junaid, 2015).
At the population level there are health conditions that could be categorized as either ‘truly co-occurring,’ ‘resulting,’ ‘associated’, or an interaction between these categories based on the specific etiologic mechanism (Figure 1.C.2). For example, generalized anxiety disorder could be a natural extension of the ASD phenotype for a subgroup (Wiggins et al., 2017) and truly co-occur, whether it first manifests in young childhood or later in life. Or, anxiety may develop only as a result of the social stressors of living in a world not designed for people on the spectrum (South, Rodgers, & Van Hecke, 2017) and in the counterfactual world with no disparity the anxiety would not develop. Anxiety may share a common risk factor such that if the individual were not to have ASD, the anxiety would still manifest. Of note, two or more of these categories may interact dynamically within the same individual or between individuals. For example, anxiety may present in some individuals only if they had a genetic predisposition and experienced disparity later in life (i.e., diathesis-stress model). When using population-level data, anxiety may be more prevalent in administrative datasets because of diagnostic accretion (White, Oswald, Ollendick, & Scahill, 2009) and the effect we see in certain populations may be driven by misdiagnosis / diagnostic trends rather than true presence of the condition. In the situation where the etiologic origin is unclear or the research is describing a health conditions in people on the autism spectrum without an etiologic hypothesis, we believe that the phrase ‘associated condition’ is most appropriate. It is vital to parse ‘truly co-occurring’ and ‘resulting’ conditions from this larger ‘associated’ group to most effectively prevent and intervene on health conditions.
Implications for Research and Practice
Language is powerful and influences the way that we study and clinically manage health conditions. We have laid out what we believe is a strong lexical framework to more effectively describe health conditions that present with ASD. Our framework will orient the field to better understand the origins and course of health conditions associated with ASD, and eventually, in partnership with the autism community, reduce health conditions that present with ASD to enhance quality of life. We argue that our model will enhance research through more specificity and temporally driven hypotheses. Improving clarity in language around these health conditions has clear implications for developing preventative strategies and clinical practice.
Describing health conditions that present with autism as ‘truly co-occurring,’ ‘resulting,’ or ‘associated’ will solidify our scientific approach to determining mechanisms. Understanding temporality can aid us in making causal inference. Causality is often erroneously considered outside the scope of observational studies (Hernán, 2018), but we argue that the causal framework for which health conditions develop in ASD is necessary in order to conduct meaningful research on improving and extending the lives of individuals on the autism spectrum. Causal models, whether the study is cross-sectional or longitudinal, allow for better conceptualization of how a condition develops and where in the pathway prevention or intervention would be most effective. We highlight the approach of Rai et al (2018) who looked at depression, a likely multi-factorial associated feature of ASD, in longitudinal data over two life-stages (childhood and adolescence) and parsed effects for genetic contributions (which would ‘truly co-occur’) and bullying (‘resulting’ condition). Future research should capitalize on the increasing availability of population-level data collected over the life course and development of advanced analytic techniques to identify causal mechanisms underlying the development of ‘truly co-occurring,’ ‘resulting,’ and ‘associated’ conditions.
Ultimately, this specific temporal language can be aligned with prevention strategies. The three-level public health model of prevention (primary prevention, secondary prevention, and tertiary prevention) supports this proposed terminology. Primary prevention aims to prevent the onset of a condition; here we would aim to eliminate shared risk factors for ASD and ‘associated’ conditions. Secondary prevention targets early screening and intervention to change the course of a condition, which would be meaningful for ‘truly co-occurring’ conditions, such as epilepsy. Lastly, tertiary prevention aims at reducing the burden of chronic conditions and would be an appropriate short-term approach for ‘resulting’ conditions, wherein altering complex social systems to reduce disparities should be long-term goals. Prevention strategies should intervene at the patient, provider, systems, and public health level and be developed collaboratively with autistic people and the autism community (Nicolaidis et al., 2015; Raymaker et al., 2016).
Finally, the language that we use to describe health conditions in ASD may have implications for clinical practice. Parsing conditions that ‘truly co-occur’ will help us identify distinct sub-and endophenotypes that could be a major step forward in precision medicine and subtype specific intervention. Further, the clearer we are about what exactly is part of the ASD phenotype and what is ‘resulting’ will help clinicians who may not be as familiar with ASD from misattributing health conditions to a feature of ASD and help to improve differential diagnosis in ASD. For instance, clinicians may interpret behavioral changes as a part of ASD rather than as a signal or manifestation of a change in health status.
Addressing the health needs of individuals on the spectrum across the life course is crucial, particularly as people on the autism spectrum age. We have attempted to introduce temporally-focused terms to improve clarity when working to solve this problem, and we hope that this idea promotes thought and discussion from the research, advocate, and autistic community.
Acknowledgements:
This commentary was supported in part by grants from the National Institute of Child Health and Human Development (U54 HD090256; T32HD007489) and the National Center for Advancing Translational Sciences (UL1TR002373; KL2TR002374; KL2TR000428). The authors would also like to acknowledge the helpful input to this commentary provided by the anonymous reviewers.
Footnotes
Throughout this piece, the term “health conditions” is meant as inclusive of both physical and mental health conditions that present with ASD
In the autism literature, ‘comorbid’ is frequently used in place of ‘co-occurring,’ but we choose not to use this term because it implies that the index condition (ASD) is an illness
References
- Barua S, & Junaid MA (2015). Lifestyle, pregnancy and epigenetic effects. Epigenomics, 7(1), 85–102. [DOI] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, & Kind AJ (2017). A scoping review of health disparities in autism spectrum disorder. Journal of Autism & Developmental Disorders, 47(11), 3380–3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Minshew NJ, Mazefsky C, & Eack SM (2017). Perception of life as stressful, not biological response to stress, is associated with greater social disability in adults with autism spectrum disorder. Journal of Autism & Developmental Disorders, 47(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Movaghar A, Greenberg JS, DaWalt LS, Brilliant MH, & Mailick MR (2018). Using machine learning to identify patterns of lifetime health problems in decedents with autism spectrum disorder. Autism Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron Chantal, & Rutter Michael. (1991). Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry, 32(7), 1063–1080. [DOI] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, & Kripke C (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. [DOI] [PubMed] [Google Scholar]
- Davignon MN, Qian Y, Massolo M, & Croen LA (2018). Psychiatric and medical conditions in transition-aged individuals with ASD. Pediatrics, 141(Supplement 4), S335–S345. [DOI] [PubMed] [Google Scholar]
- Gandhi RP, & Klein U (2014). Autism spectrum disorders: an update on oral health management. J Evid Based Dent Pract, 14 Suppl, 115–126. [DOI] [PubMed] [Google Scholar]
- Hernán MA (2018). The C-word: Scientific euphemisms do not improve causal inference from observational data. American Journal of Public Health, 108(5), 616–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interagency Autism Coordinating Committee. (2017). Interagency Autism Coordinating Committee Stregatic Plan for Autism Spectrum Disorder. Retrieved from the U.S. Department of Health and Human Services Interagency Autism Coordinating Committee website: https://iacc.hhs.gov/publications/strategic-plan/2017/strategic_plan_2017.pdf.
- Kalkbrenner AE, Schmidt RJ, & Penlesky AC (2014). Environmental chemical exposures and autism spectrum disorders: a review of the epidemiological evidence. Curr Probl Pediatr Adolesc Health Care, 44(10), 277–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahn GL, Hammond L, & Turner A (2006). A cascade of disparities: Health and health care access for people with intellectual disabilities. Developmental Disabilities Research Reviews, 12(1), 70–82. [DOI] [PubMed] [Google Scholar]
- Lai M-C, Lombardo MV, & Baron-Cohen S (2014). Autism. The Lancet, 383(896–910). [DOI] [PubMed] [Google Scholar]
- Levy SE, Giarelli E, Lee LC, Schieve LA, Kirby RS, Cunniff C, Nicholas J, Reaven J, & Rice CE (2010). Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. J Dev Behav Pediatr, 31(4), 267–275. [DOI] [PubMed] [Google Scholar]
- Maddox BB, Kang-Yi CD, Brodkin ES, & Mandell DS (2018). Treatment utilization by adults with autism and co-occurring anxiety or depression. Research in Autism Spectrum Disorders, 51, 32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis Christina, Raymaker Dora M., Ashkenazy Elesia, McDonald Katherine E., Dern Sebastian, Baggs Amelia E. V., . . . Boisclair W. Cody. (2015). “Respect the way I need to communicate with you”: Healthcare experiences of adults on the autism spectrum. Autism, 19(7), 824–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicano E, Dinsmore A, & Charman T (2014). What should autism research focus upon? Community views and priorities from the United Kingdom. Autism, 18(7), 756–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai D, Culpin I, Heuvelman H, Magnusson CMK, Carpenter P, Jones HJ, . . . Pearson RM (2018). Association of autistic traits with depression from childhood to age 18 years. JAMA Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymaker Dora M., McDonald Katherine E., Ashkenazy Elesia, Gerrity Martha, Baggs Amelia M., Kripke Clarissa, . . . Nicolaidis Christina. (2016). Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism, 21(8), 972–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubenstein E, Daniels J, Schieve LA, Christensen DL, Van Naarden Braun K, Rice CE, Bakian AV, Durkin MS, Rosenberg SA, & Kirby RS (2018). Trends in special education eligibility among children with autism spectrum disorder, 2002–2010. Public Health Reports, 133(1), 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanbonmatsu L, Potter NA, Adam E, Duncan GJ, Katz LF, Kessler RC, Ludwig J, Marvakov J, Yang F, & Congdon WJ (2012). The long-term effects of moving to opportunity on adult health and economic self-sufficiency. Cityscape, 109–136. [Google Scholar]
- Shea LL, Xie M, Turcotte P, Marcus S, Field R, Newschaffer C, & Mandell D (2018). Brief report: Service use and associated expenditures among adolescents with autism spectrum disorder transitioning to adulthood. J Autism Dev Disord. [DOI] [PubMed] [Google Scholar]
- South M, Rodgers J, & Van Hecke A (2017). Anxiety and ASD: Current progress and ongoing challenges. Journal of Autism and Developmental Disorders, 47(12), 3679–3681. [DOI] [PubMed] [Google Scholar]
- Spratt E, Nicholas J, Brady K, Carpenter L, Hatcher C, Meekins K, Furlanetto R, & Charles J (2012). Enhanced cortisol response to stress in children in autism. Journal of Autism and Developmental Disorders, 42(1), 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starkstein S, Gellar S, Parlier M, Payne L, & Piven J (2015). High rates of parkinsonism in adults with autism. Journal of neurodevelopmental disorders, 7(29), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toschke AM, Montgomery SM, Pfeiffer U, & von Kries R (2003). Early intrauterine exposure to tobacco-inhaled products and obesity. Am J Epidemiol, 158(11), 1068–1074. [DOI] [PubMed] [Google Scholar]
- Valderas JM, Starfield B, Sibbald B, Salisbury C, & Roland M (2009). Defining comorbidity: implications for understanding health and health services. Ann Fam Med, 7(4), 357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner G, Parr JR, & Cusack J (2018). Workshop report: Establishing priority research areas to improve the physical health and well-being of autistic adults and older people. Autism in Adulthood: Knowledge, Practice, and Policy. [Google Scholar]
- White SW, Oswald D, Ollendick T, & Scahill L (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins LD, Tian LH, Levy SE, Rice C, Lee LC, Schieve L, Pandey J, Daniels J, Blaskey L, Hepburn S, Landa R, Edmondson-Pretzel R, & Thompson W (2017). Homogeneous subgroups of young children with autism improve phenotypic characterization in the study to explore early development. J Autism Dev Disord, 47(11), 3634–3645. [DOI] [PMC free article] [PubMed] [Google Scholar]


