Abstract
Hepatic fibrosis is marked by excessive synthesis and deposition of connective tissue proteins, especially interstitial collagens in the extracellular matrix of the liver. It is a result of an abnormal wound healing in response to chronic liver injury from various causes such as ethanol, viruses, toxins, drugs, or cholestasis. The chronic stimuli involved in the initiation of fibrosis leads to oxidative stress and generation of reactive oxygen species that serve as mediators of molecular events involved in the pathogenesis of hepatic fibrosis. These processes lead to cellular injury and initiate inflammatory responses releasing a variety of cytokines and growth factors that trigger activation and transformation of resting hepatic stellate cells into myofibroblast like cells, which in turn start excessive synthesis of connective tissue proteins, especially collagens. Uncontrolled and extensive fibrosis results in distortion of lobular architecture of the liver leading to nodular formation and cirrhosis. The perpetual injury and regeneration process could also results in genomic aberrations and mutations that lead to the development of hepatocellular carcinoma. This review covers most aspects of the molecular mechanisms involved in the pathogenesis of hepatic fibrosis with special emphasize on N-Nitrosodimethylamine (NDMA; Dimethylnitorsmaine, DMN) as the inducing agent.
Facts
Hepatic fibrosis is due to the excessive synthesis and deposition of connective tissue proteins, especially interstitial collagens in the extracellular matrix of the liver.
Abnormal wound healing in response to chronic liver injury is responsible for the pathogenesis of hepatic fibrosis.
The key event involved in the pathogenesis of hepatic fibrosis is the activation and transformation of resting hepatic stellate cells into myofibroblast like cells and subsequent upregulation of hundreds of genes.
Oxidative stress and generation of reactive oxygen species (ROS) serve as mediators of the molecular events implicated in hepatic fibrosis.
The precise molecular mechanism involved in the pathogenesis and progression of hepatic fibrosis is not clear.
Open Questions
Exploration of methods to arrest activation and transformation of hepatic stellate cells into myofibroblast like cells.
Development of potent antioxidant therapy that could destroy reactive oxygen species, which serve as mediators for the pathogenesis of hepatic fibrosis.
Identification of appropriate gene targets that block the pathogenesis of hepatic fibrosis.
Development of methods to reverse the process of hepatic fibrosis.
Identification of strategies to prevent transformation of hepatic fibrosis to liver cirrhosis.
Introduction
Hepatic fibrosis and liver cirrhosis are chronic diseases and serious health problems worldwide. Excessive synthesis and deposition of connective tissue proteins, especially interstitial collagens in the extracellular matrix of the liver is the hallmark of hepatic fibrosis1–6. It is a dynamic process resulting from a continuous wound healing response to a variety of chronic stimuli, such as ethanol, viruses, toxins, drugs, or cholestasis. The process of hepatic fibrosis is initiated with cellular oxidative stress and production of reactive oxygen species (ROS) that serve as mediators of molecular events involved in the pathogenesis of hepatic fibrosis7–10. These processes results in cellular injury and release a variety of cytokines and growth factors that induce activation of resting hepatic stellate cells (HSCs) into myofibroblast-like cells with the expression of α-smooth muscle actin filaments as a characteristic marker11–14. The activated stellate cells lose their lipid droplets (vitamin A), rapidly proliferate and dramatically upregulate a number of genes, especially for collagens, fibronectins, laminin, hyaluronic acid, and start increased synthesis of connective tissue proteins, markedly collagens15–17. This results in excessive deposition of several connective tissue proteins, mainly collagens in the hepatic parenchyma that leads to fibrosis. The uncontrolled and extensive fibrosis could produce distortion of normal architecture of the liver leading to nodular formation and cirrhosis. The repeated chronic injury and cellular regenerative events could result in genomic aberrations and mutations of oncogenes or tumor-suppressor genes leading to the development of hepatocellular carcinoma (HCC)18–23.
N-Nitrosodimethylamine
N-Nitrosodimethylamine, (NDMA, (CH3)2N2O, Mol. wt. 74.08) also known as dimethylnitrosamine (DMN), is a byproduct of several industrial processes and is present in trace amounts in tobacco smoke condensates24–26. It is formed by the interaction of nitrate with dimethylamine and by the action of nitrite reducing bacteria27,28. Some of the physical, chemical, and biological properties of NDMA are presented in Table 1. Barnes and Magee first reported its hepatotoxicity following an industrial accident of liver cirrhosis29. NDMA is characterized as a potent hepatotoxin, carcinogen, and mutagen4,30–32. The toxicities produced by NDMA and related nitrosamines are mediated by reactive metabolic intermediates and not by the parent compound32,33. NDMA targets primarily the liver, which contains the necessary enzymes for its metabolic activation. Metabolism in the liver is by the microsomal membrane-bound enzyme, cytochrome P-450 2E134–36. Its metabolic half-life is <10 min in rodents and about 20 min in non-human primates37,38. Activation and degradation of NDMA produces formaldehyde and methanol and an alkylating intermediate that reacts with nucleic acids and proteins to form methylated macromolecules (Fig. 1). It has been demonstrated that NDMA and other nitrosamines are metabolized in vitro by liver homogenates to yield the corresponding aldehyde and a chemically reactive alkylating species39. NDMA methylates proteins40,41 and DNA42 and forms specific DNA adducts43,44. In vitro preparations of human liver slices can also metabolize NDMA and methylates its DNA in the same order as rat liver slices45.
Table 1.
Physical, chemical, and biological properties of N-Nitrosodimethylamine
| Property | Value/description |
|---|---|
| Chemical Abstract Systems (CAS) Numbera | 62–75–9 |
| Chemical formula | C2H6N2O |
| Physical description (physical state at room temperature) | Yellow liquid with no distinct odor |
| Molecular weight | 74.083 g/mol |
| Solubility in water | 290 g/L at 20 oC |
| Specific gravity/density at 20 oC/4 oC | 1.0048 g/mL |
| Melting point | <25 °C (estimated) |
| Boiling point | 153.1 oC (307.5 °F) |
| Vapor pressure at 20 oC | 2.7 mm Hg |
| Flash point | 61.0 oC (141.8 °F) |
| LD50 (rat) | 37.0 mg/kg (oral) |
| Biohazards | Highly hepatotoxic, carcinogenic |
g/mol grams per mole, g/mL grams per milliliter, °C degrees Celsius,
°F degrees Fahrenheit, mm Hg millimeters of mercury, LD50 Median lethal dose (lethal dose 50%), mg/kg milligram per kilogram
aSource
Fig. 1. Metabolic activation and degradation of N-nitrosodimethylamine (NDMA) in liver.
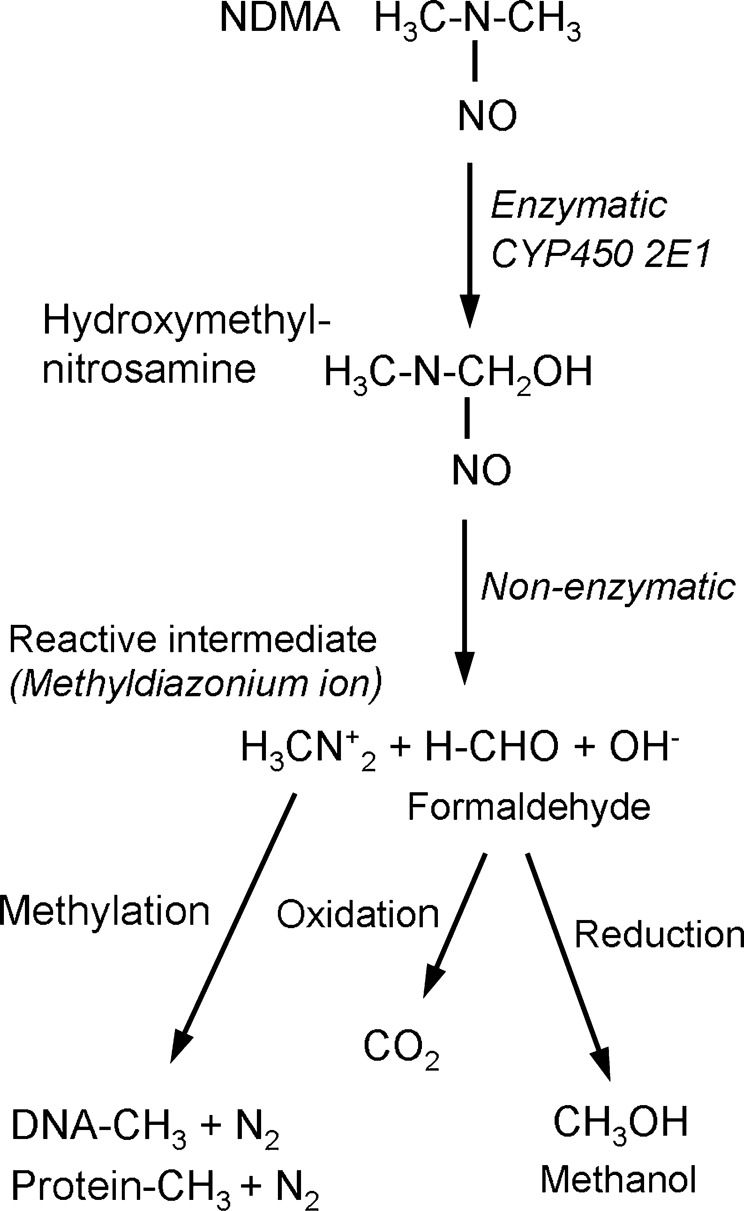
The metabolic degradation of NDMA produces formaldehyde and methanol, and the alkylating intermediate reacts with nucleic acids and proteins to form methylated macromolecules
N-Nitrosodimethylamine-induced hepatic fibrosis and liver cirrhosis
The NDMA-induced canine model of hepatic fibrosis was first developed by Madden et al46. Later it was demonstrated that serial administrations of NDMA in rats could produce a reproducible model of hepatic fibrosis, cirrhosis, and portal hypertension, as seen in human beings47. Afterwards Jezequel and coworkers conducted a pioneering study on various aspects of NDMA-induced hepatic fibrosis with special emphasis to pathophysiology and immunohistochemistry and demonstrated that it is a good and reproducible animal model, and appropriate for the study of the early events associated with the development of hepatic fibrosis48–52. Furthermore, the model has been employed recently to investigate various aspects of the molecular pathogenesis of hepatic fibrosis and to study therapeutic approaches including the arrest of activation of stellate cells53–60. Over the last 20 years, we have extensively studied various biochemical and pathophysiological aspects of the pathogenesis of NDMA-induced hepatic fibrosis in rats and mice involving glycoprotein metabolism17, collagen biosynthesis and metabolism4–6, LDH isoenzymes61, biochemical abnormalities62, oxidative stress and osteopontin10,63–65, hyaluronic acid and hyaluronidase66,67, mineral and trace element metabolism68–70, antioxidants10,71,72 and gene therapy13,73,74, lysosomal fragility75,76, and the role of metalloproteinases14,77,78. These studies demonstrated that NDMA-induced model of hepatic fibrosis and early cirrhosis in rats is an easy and quick model to study the molecular mechanisms involved in the pathogenesis of liver fibrosis and cirrhosis of human beings.
Events involved in the pathogenesis of NDMA induced hepatic fibrosis and cirrhosis
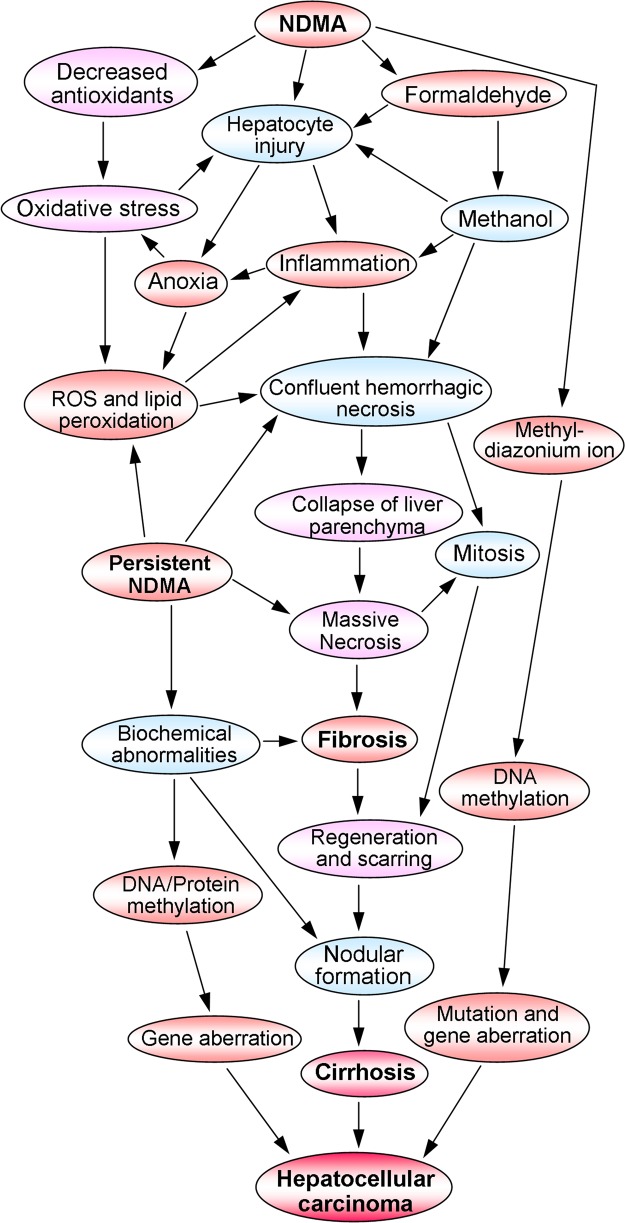
A schematic representation of the sequence of events involved in the pathogenesis of NDMA-induced hepatic fibrosis, liver cirrhosis, and the ultimate hepatocellular carcinoma is presented in Fig. 2. The metabolic activation and detoxification process of NDMA induces liver injury in multiple ways. The enzymatic degradation of NDMA produces hydroxymethylnitrosamine, which in turn non-enzymatically converted into formaldehyde and methanol (Fig. 1). Both compounds are highly toxic to the liver and initiates severe inflammation and confluent hemorrhagic necrosis. These processes results in extreme oxidative stress and production of reactive oxygen species (ROS) that further contributes to hepatocyte damage and necrosis. Furthermore, NDMA decreases catalase and glutathione peroxidase, the major antioxidant enzymes present in the liver79–81. We have observed that NDMA treatment dramatically decreases serum and liver concentrations of ascorbic acid, another major antioxidant10. In addition, the metabolic generation of reactive intermediate, the methyl carbonium ion by NDMA damages hepatic tissue in multiple ways and triggers fibrogenesis.
Fig. 2. Schematic representation of the sequence of events involved in the pathogenesis of N-nitrosodimethylamine (NDMA) induced hepatic fibrosis, cirrhosis, and hepatocellular carcinoma.
The metabolic activation and detoxification of NDMA cause hepatocyte injury, inflammation, neutrophilic infiltration, and massive hepatic necrosis, which results in oxidative stress and production of reactive oxygen species. These processes induce activation of hepatic stellate cells and increased synthesis of connective tissue components, especially collagens that end up in hepatic fibrosis. The chronic liver injury and perpetual fibrosis lead to liver cirrhosis, which could develop into hepatocellular carcinoma
The persistent treatment of NDMA further increases oxidative stress and lipid peroxidation that enhances hemorrhagic necrosis and collapse of liver parenchyma. The extensive panlobular and multilobular necrosis lead to massive hepatic necrosis, which in turn initiates mitosis and hepatic regeneration. On the other hand, the resting HSCs transform into myofibroblast like cells and start extensive synthesis of connective tissue proteins. This causes deposition of mature collagen fibrils in the extracellular matrix of the liver and results in hepatic fibrosis. All these processes lead to condensation of hepatic reticulin framework, production of granulation tissue, and ultimately scar formation82–84. The ischemic consequences of the hepatic tissue and confluent necrosis amplify the process of nodular regeneration and drive towards to liver cirrhosis. The repeated tissue repair and regeneration process can lead to aberrations and mutations in genes and end up in development of HCC85–88. Alternatively, the methyl carbonium ions produced during metabolic degradation of NDMA methylate the hepatocyte DNA that results in gene mutation and trigger HCC89–91.
Cellular interactions and molecular mechanisms in the pathogenesis of NDMA-induced hepatic fibrosis
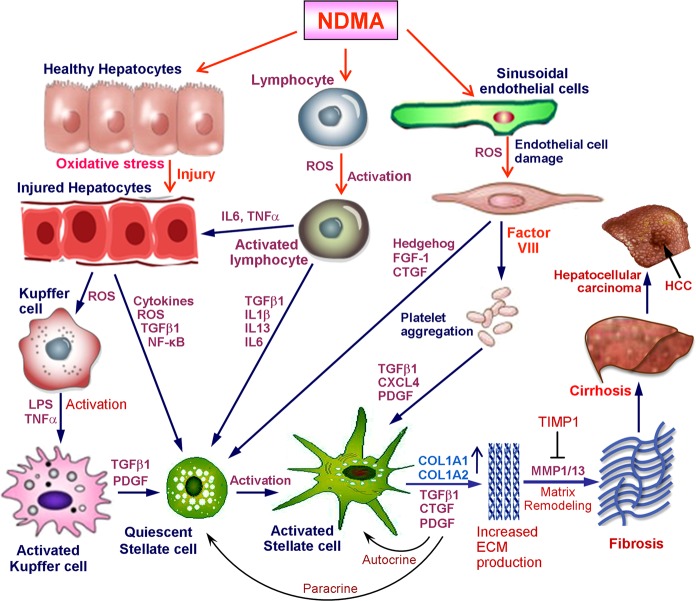
A schematic representation of the cellular interactions and molecular mechanisms involved in the pathogenesis of NDMA-induced hepatic fibrosis is presented in Fig. 3. An injury to the liver produces a response from various types of cells and alters cell–cell and cell–matrix interactions. Such a response leads to inflammation accompanied by the infiltration of lymphocytes, monocytes, granulocytes, and macrophages into the space of Disse92–94. Treatment with NDMA injures both parenchymal and non-parenchymal cells in multiple ways, produces inflammation, and generates oxidative stress and reactive oxygen species (ROS). In addition, NDMA could produce increased gut permeability, which in turn accelerates the entry of bacterial endotoxin (lipopolysaccharide) into the blood stream, which interacts with Kupffer cells in the liver and activates them95,96. Lipopolysaccharide (LPS), a component of the cell walls of some gram-negative bacteria that normally inhabit the intestine, is one substance that can effectively activate Kupffer cells97,98. The activated Kupffer cells produce several cytokines and growth factors such as tumor necrosis factor-α (TNF-α), transforming growth factor-β1 (TGF-β1), platelet derived growth factor (PDGF), and interleukin (IL)−1β which in turn activate and transform the quiescent HSCs into myofibroblast like cells99–101.
Fig. 3. Schematic representation of the cellular interactions and molecular mechanisms involved in the pathogenesis of N-nitrosodimethylamine induced hepatic fibrosis.
Hepatocyte injury leads to inflammation and generation of reactive oxygen species that in turn activate Kupffer cells. The activated Kupffer cells produce the most potent fibrogenic factor TGF-β1, which activate the quiescent hepatic stellate cells into myofibroblast like cells with the expression of α-smooth muscle actin filaments. Alternatively, metabolism of NDMA cause activation of lymphocytes and injury to sinusoidal endothelial cells which produce potent fibrogenic factors like TGF-β1, CTGF, and FGF-1 and cytokines and growth factors such as NF-κB, IL-1β, IL-6, IL-13, IL-22, and CXCL4 which altogether contribute the activation of resting hepatic stellate cells. The activated and transformed stellate cells express and upregulate hundreds of genes, especially for collagens and other connective tissue proteins. The excessive synthesis and deposition of these proteins, specifically fibril forming collagens in the extracellular matrix of the liver leads to fibrosis and cirrhosis and ultimately to HCC
Ingestion or administration of NDMA triggers the immune system and activate the lymphocytes which in turn produce various pro-inflammatory cytokines such as IL-1β, IL-6, IL-22, interferon-γ (IFN-γ), and TNF-α102–104. The pro-inflammatory cytokines trigger hepatocytes to activate downstream signaling pathways such as nuclear factor-kB (NF-kB) and TGF-β, which in turn induce activation of resting hepatic stellate cells. On the other hand, the activated lymphocytes produce a variety of cytokines and growth factors including TGF-β1, IL-1β, IL-6, and IL-13, which directly activate and transform the quiescent stellate cells105–107. Alternatively, the sinusoidal endothelial cell damage caused by ROS and other methods during NDMA treatment produce potent fibrogenic factors such as connective tissues growth factor (CTGF) and fibroblast growth factor-1 (FGF-1) and may also induce hedgehog signaling108–110. Both CTGF and FGF-1 induce activation of stellate cells into myofibroblast like cells. In addition, it was shown that hedgehog signaling in liver sinusoidal endothelial cells regulate capillarisation during fibrogenesis110,111. Damage to the endothelial cells could release several factors including Factor VIII that cause platelet aggregation and further produce TGF-β1 and platelet derived growth factor (PDGF) and CXC chemokine ligand 4 (CXCL4)112,113. Furthermore, cytosolic fragments released by injured hepatocytes could directly stimulate perisinusoidal cells and induce production several fibrogenic and growth factors that in turn transform the resting stellate cells into myofibroblast like cells112,114.
The activation and transformation of quiescent HSCs into large myofibroblast like cells with the loss of fat globules and expression of alpha smooth muscle actin (α-SMA) is a very crucial and important step in hepatic fibrogenesis115,116. Increased level of intracellular cAMP is required for the conversion of HSCs into myofibroblasts and their proliferation117,118. The transformed HSCs further produce several cytokines and growth factors, especially TGF-β1, CTGF, and PDGF which in turn further stimulate more production of cytokines and growth factors through the autocrine mechanism and also transforms the remaining quiescent stellate cells by the paracrine mechanism (Fig. 3). The process of activation of quiescent HSCs is accompanied with the expression and upregulation of 100 s of genes, especially for collagens and other extracellular matrix proteins11,119,120. The net result is excessive and non-regulated synthesis and deposition of connective tissue components especially fibril forming collagens in the extracellular space of the liver4,121,122. This coincides with the development of basement membrane formed with type IV collagen and laminin in the space of Disse and decreases the number of fenestrations of sinusoidal endothelial cells123. The defenestration of endothelial cells leads to increased diffusional barrier and interferes with the transport of nutrients to hepatocytes contributing to the development of portal hypertension and impairment of liver functions.
Matrix metalloproteinases (MMPs) are capable of degrading extracellular matrix proteins including all forms of native collagens and play a prominent role in remodeling of connective tissue matrix during pathogenesis of hepatic fibrosis14,124,125. The major interstitial collagenases that degrade native fibrillar collagens in human are MMP-1 and MMP-13. However, mice and rats do not possess a homologous to human MMP-1 gene126. We have demonstrated that NDMA-induced fibrotic fiver collagen is more cross-linked than normal liver collagen and the deposition of type III collagen is more prominent than type I collagen6. The extreme necrosis of hepatic parenchyma during persistent NDMA administration leads to decreased enzyme synthesis and thus reduced interstitial collagenases levels. On the other hand, tissue inhibitor of metalloproteinases (TIMPS), especially TIMP-1 is markedly upregulated during pathogenesis of hepatic fibrosis, which inhibits the activity of MMPs78,127–129. Thus there is impairment in the balance between synthesis and degradation of collagens in multiple ways and the net result is deposition of excessive amount of fibril forming collagens in the extracellular matrix of the liver. Once mature collagen fibrils are deposited in the extracellular compartment of the liver, it will form stable inter and intra cross-linking and lead to hepatic fibrosis130. The persistent stimulus results in repeated confluent necrosis, wound healing, scarring, and nodular formation, which could lead to liver cirrhosis and ultimate death.
Summary and conclusion
Hepatic fibrosis is the result of excessive synthesis and deposition of connective tissue proteins, especially fibril forming collagens (collagens type I and type III) in the extracellular matrix of the liver. An abnormal wound healing process in response to a chronic liver injury is responsible for the pathogenesis of hepatic fibrosis and subsequent liver cirrhosis leading to hepatocellular carcinoma and ultimate death. The repeated stimuli involved in the initiation of fibrosis lead to oxidative stress and generation of reactive oxygen species along with marked decrease of antioxidant status. These processes results in cellular injury and initiate inflammatory responses releasing a variety of cytokines and growth factors that serve as mediators of molecular events involved in the initiation of fibrosis. The key event involved in the pathogenesis of hepatic fibrosis is the activation and transformation of resting hepatic stellate cells into myofibroblast like cells and subsequent upregulation of numerous genes, especially genes for connective tissue proteins. The transformed stellate cells abandon its vitamin-A storage function and start excessive synthesis and deposition of connective tissue components especially collagens, glyocoproteins, and glycosaminoglycans in the extracellular matrix of the liver. Extensive and uncontrolled fibrosis results in distortion of lobular architecture of the liver leading to nodular formation and cirrhosis. The chronic injury and regeneration process could results in genomic aberrations and mutations that lead to the development of hepatocellular carcinoma. Unraveling the precise molecular mechanism involved in the pathogenesis and progression of hepatic fibrosis would help to design successful therapeutic approaches that could prevent liver cirrhosis and subsequent hepatocellular carcinoma.
Acknowledgements
This work was partly supported from Japan Society for the Promotion of Science (JSPS) by Grant # 10670515 to M. Tsutsumi.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Edited by Stephanou
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Parola, M. & Pinzani, M. Liver fibrosis: pathophysiology, pathogenetic targets and clinical issues. Mol. Aspects Med.S0098-2997, 30070-0 (2018) 10.1016/j.mam.2018.09.002. [DOI] [PubMed]
- 2.Bellan M, Castello LM, Pirisi M. Candidate Biomarkers of liver fibrosis: a concise, pathophysiology-oriented review. J. Clin. Transl. Hepatol. 2018;6:317–325. doi: 10.14218/JCTH.2018.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aydın MM, Akçalı KC. Liver fibrosis. Turk. J. Gastroenterol. 2018;29:14–21. doi: 10.5152/tjg.2018.17330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.George J, Rao KR, Stern R, Chandrakasan G. Dimethylnitrosamine-induced liver injury in rats: the early deposition of collagen. Toxicology. 2001;156:129–138. doi: 10.1016/s0300-483x(00)00352-8. [DOI] [PubMed] [Google Scholar]
- 5.George J, Chandrakasan G. Collagen metabolism in dimethylnitrosamine induced hepatic fibrosis in rats. FASEB J. 1997;11:A1094. doi: 10.1016/1357-2725(95)00140-9. [DOI] [PubMed] [Google Scholar]
- 6.George J, Chandrakasan G. Molecular characteristics of dimethylnitrosamine induced fibrotic liver collagen. Biochim. Biophys. Acta. 1996;1292:215–222. doi: 10.1016/0167-4838(95)00202-2. [DOI] [PubMed] [Google Scholar]
- 7.Luangmonkong T, et al. Targeting oxidative stress for the treatment of liver fibrosis. Rev. Physiol. Biochem. Pharmacol. 2018;175:71–102. doi: 10.1007/112_2018_10. [DOI] [PubMed] [Google Scholar]
- 8.Torok NJ. Dysregulation of redox pathways in liver fibrosis. Am. J. Physiol. Gastrointest. Liver Physiol. 2016;311:G667–G674. doi: 10.1152/ajpgi.00050.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mormone E, George J, Nieto N. Molecular pathogenesis of hepatic fibrosis and current therapeutic approaches. Chem. Biol. Interact. 2011;193:225–231. doi: 10.1016/j.cbi.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George J. Ascorbic acid concentrations in dimethylnitrosamine-induced hepatic fibrosis in rats. Clin. Chim. Acta. 2003;335:39–47. doi: 10.1016/s0009-8981(03)00285-7. [DOI] [PubMed] [Google Scholar]
- 11.Tsuchida T, Friedman SL. Mechanisms of hepatic stellate cell activation. Nat. Rev. Gastroenterol. Hepatol. 2017;14:397–411. doi: 10.1038/nrgastro.2017.38. [DOI] [PubMed] [Google Scholar]
- 12.Ying HZ, et al. PDGF signaling pathway in hepatic fibrosis pathogenesis and therapeutics (Review) Mol. Med. Rep. 2017;16:7879–7889. doi: 10.3892/mmr.2017.7641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.George J, Tsutsumi M. siRNA-mediated knockdown of connective tissue growth factor prevents N-nitrosodimethylamine-induced hepatic fibrosis in rats. Gene Ther. 2007;14:790–803. doi: 10.1038/sj.gt.3302929. [DOI] [PubMed] [Google Scholar]
- 14.George J, Tsutsumi M, Tsuchishima M. MMP-13 deletion decreases profibrogenic molecules and attenuates N-nitrosodimethylamine induced liver injury and fibrosis in mice. J. Cell. Mol. Med. 2017;21:3821–3835. doi: 10.1111/jcmm.13304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuppan D, Ashfaq-Khan M, Yang AT, Kim YO. Liver fibrosis: direct antifibrotic agents and targeted therapies. Matrix Biol. 2018;68–69:435–451. doi: 10.1016/j.matbio.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Elpek GOuml. Cellular and molecular mechanisms in the pathogenesis of liver fibrosis: an update. World J. Gastroenterol. 2014;20:7260–7276. doi: 10.3748/wjg.v20.i23.7260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.George J, Chandrakasan G. Glycoprotein metabolism in dimethylnitrosamine induced hepatic fibrosis in rats. Int. J. Biochem. Cell Biol. 1996;28:353–361. doi: 10.1016/1357-2725(95)00140-9. [DOI] [PubMed] [Google Scholar]
- 18.O’Rourke JM, Sagar VM, Shah T, Shetty S. Carcinogenesis on the background of liver fibrosis: Implications for the management of hepatocellular cancer. World J. Gastroenterol. 2018;24:4436–4447. doi: 10.3748/wjg.v24.i39.4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fujiwara N, Friedman SL, Goossens N, Hoshida Y. Risk factors and prevention of hepatocellular carcinoma in the era of precision medicine. J. Hepatol. 2018;68:526–549. doi: 10.1016/j.jhep.2017.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woo HG, et al. Integrative analysis of genomic and epigenomic regulation of the transcriptome in liver cancer. Nat. Commun. 2017;8:839. doi: 10.1038/s41467-017-00991-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khemlina G, Ikeda S, Kurzrock R. The biology of Hepatocellular carcinoma: implications for genomic and immune therapies. Mol. Cancer. 2017;16:149. doi: 10.1186/s12943-017-0712-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsue Y, et al. Serum osteopontin predicts degree of hepatic fibrosis and serves as a biomarker in patients with hepatitis C virus infection. PLoS One. 2015;10:e0118744. doi: 10.1371/journal.pone.0118744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsuchishima M, et al. Chronic ingestion of ethanol induces hepatocellular carcinoma in mice without additional hepatic insult. Dig. Dis. Sci. 2013;58:1923–1933. doi: 10.1007/s10620-013-2574-4. [DOI] [PubMed] [Google Scholar]
- 24.Lv J, Wang L, Li Y. Characterization of N-nitrosodimethylamine formation from the ozonation of ranitidine. J. Environ. Sci. 2017;58:116–126. doi: 10.1016/j.jes.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 25.Hatzinger PB, Lewis C, Webster TS. Biological treatment of N-nitrosodimethylamine (NDMA) and N-nitrodimethylamine (NTDMA) in a field-scale fluidized bed bioreactor. Water Res. 2017;126:361–371. doi: 10.1016/j.watres.2017.09.040. [DOI] [PubMed] [Google Scholar]
- 26.Rhoades JW, Johnson DE. N-Dimethylnitrosamine in tobacco smoke condensate. Nature. 1972;236:307–308. doi: 10.1038/236307b0. [DOI] [PubMed] [Google Scholar]
- 27.Liao E, Xu Y, Jiang Q, Xia W. Effects of inoculating autochthonous starter cultures on N-nitrosodimethylamine and its precursors formation during fermentation of Chinese traditional fermented fish. Food Chem. 2019;271:174–181. doi: 10.1016/j.foodchem.2018.07.186. [DOI] [PubMed] [Google Scholar]
- 28.Mitch WA, Sedlak DL. Formation of N-nitrosodimethylamine (NDMA) from dimethylamine during chlorination. Environ. Sci. Technol. 2002;36:588–595. doi: 10.1021/es010684q. [DOI] [PubMed] [Google Scholar]
- 29.Barnes JM, Magee PN. Some toxic properties of dimethylnitrosamine. Br. J. Ind. Med. 1954;11:167–174. doi: 10.1136/oem.11.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sheweita SA, El Banna YY, Balbaa M, Abdullah IA, Hassan HE. N-nitrosamines induced infertility and hepatotoxicity in male rabbits. Environ. Toxicol. 2017;32:2212–2220. doi: 10.1002/tox.22436. [DOI] [PubMed] [Google Scholar]
- 31.Choi MJ, et al. Protective effects of Centella asiatica leaf extract on dimethylnitrosamine-induced liver injury in rats. Mol. Med. Rep. 2016;14:4521–4528. doi: 10.3892/mmr.2016.5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haggerty HG, Holsapple MP. Role of metabolism in dimethylnitrosamine induced immunosuppression: a review. Toxicology. 1990;63:1–23. doi: 10.1016/0300-483x(90)90064-n. [DOI] [PubMed] [Google Scholar]
- 33.Wang X, Yang H, Zhou B, Wang X, Xie Y. Effect of oxidation on amine-based pharmaceutical degradation and N-Nitrosodimethylamine formation. Water Res. 2015;87:403–411. doi: 10.1016/j.watres.2015.07.045. [DOI] [PubMed] [Google Scholar]
- 34.Gao J, et al. Higher CYP2E1 activity correlates with hepatocarcinogenesis induced by diethylnitrosamine. J. Pharmacol. Exp. Ther. 2018;365:398–407. doi: 10.1124/jpet.117.245555. [DOI] [PubMed] [Google Scholar]
- 35.Chowdhury G, Calcutt MW, Nagy LD, Guengerich FP. Oxidation of methyl and ethyl nitrosamines by cytochrome P450 2E1 and 2B1. Biochemistry. 2012;51:9995–10007. doi: 10.1021/bi301092c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoo JS, Ishizaki H, Yang CS. Roles of cytochrome P450IIE1 in the dealkylation and denitrosation of N-nitrosodimethylamine and N-nitrosodiethylamine in rat liver microsomes. Carcinogenesis. 1990;11:2239–2243. doi: 10.1093/carcin/11.12.2239. [DOI] [PubMed] [Google Scholar]
- 37.Anderson LM, et al. Reduced blood clearance and increased urinary excretion of N-nitrosodimethylamine in patas monkeys exposed to ethanol or isopropyl alcohol. Cancer Res. 1992;52:1463–1468. [PubMed] [Google Scholar]
- 38.Gombar CT, et al. Pharmacokinetics of N-nitrosodimethylamine in swine. Carcinogenesis. 1988;9:1351–1354. doi: 10.1093/carcin/9.8.1351. [DOI] [PubMed] [Google Scholar]
- 39.Preussmann, R. & Stewart, B. W. in Chemical Carcinogens. 2nd edn, (ACS Monograph Series No.182) (ed. Searle CE) pp. 643–828 (American Chemical Society, Washington DC, 1984).
- 40.Croby, N. T. in Handbook of Naturally Occurring Food Toxicants, (ed. Rechcigl M.) pp. 131–160 (CRC Press, Boca Raton, 2018).
- 41.Magee PN, Hultin T. Toxic liver injury and carcinogenesis. Methylation of proteins of rat liver slices by dimethylnitrosamine in vitro. Biochem. J. 1962;83:106–114. doi: 10.1042/bj0830106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin H, Hollenberg PF. N-nitrosodimethylamine-mediated formation of oxidized and methylated DNA bases in a cytochrome P450 2E1 expressing cell line. Chem. Res. Toxicol. 2001;14:562–566. doi: 10.1021/tx0001979. [DOI] [PubMed] [Google Scholar]
- 43.Carlson ES, Upadhyaya P, Hecht SS. A general method for detecting nitrosamide formation in the in vitro metabolism of nitrosamines by cytochrome P450s. J. Vis. Exp. 2017;127:e56312. doi: 10.3791/56312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asamoto M, et al. Immunohistochemical detection of DNA alkylation adducts in rat and hamster liver after treatment with dimethylnitrosamine. Exp. Pathol. 1991;41:71–78. doi: 10.1016/s0232-1513(11)80004-6. [DOI] [PubMed] [Google Scholar]
- 45.Jensen DE, Lotlikar PD, Magee PN. The in vitro methylation of DNA by microsomally activated dimethylnitrosamine and its correlation with formaldehyde production. Carcinogenesis. 1981;2:349–354. doi: 10.1093/carcin/2.4.349. [DOI] [PubMed] [Google Scholar]
- 46.Madden JW, Gertman PM, Peacock EE. Dimethylnitrosamine induced hepatic cirrhosis: a new canine model of an ancient human disease. Surgery. 1970;68:260–268. [PubMed] [Google Scholar]
- 47.Jenkins SA, et al. A dimethylnitrosamine induced model of cirrhosis and portal hypertension in the rat. J. Hepatol. 1985;1:489–499. doi: 10.1016/s0168-8278(85)80747-9. [DOI] [PubMed] [Google Scholar]
- 48.Jézéquel AM, et al. A morphological study of the early stages of hepatic fibrosis induced by low doses of dimethylnitrosamine in the rat. J. Hepatol. 1987;5:174–181. doi: 10.1016/s0168-8278(87)80570-6. [DOI] [PubMed] [Google Scholar]
- 49.Jézéquel AM, et al. Dimethylnitrosamine induced cirrhosis. Evidence for an immunological mechanism. J. Hepatol. 1989;8:42–52. doi: 10.1016/0168-8278(89)90160-8. [DOI] [PubMed] [Google Scholar]
- 50.Jezequel AM, et al. Modulation of extracellular matrix components during dimethylnitrosamine induced cirrhosis. J. Hepatol. 1990;11:206–214. doi: 10.1016/0168-8278(90)90115-8. [DOI] [PubMed] [Google Scholar]
- 51.Mancini R, Paolucci F, Svegliati Baroni G, Jezequel AM, Orlandi F. Phenotypic analysis of inflammatory infiltrate in rats with dimethylnitrosamine induced cirrhosis. Int. J. Exp. Pathol. 1991;72:19–128. [PMC free article] [PubMed] [Google Scholar]
- 52.Mancini R, et al. Quantitative analysis of proliferating sinusoidal cells in dimethylnitrosamine induced cirrhosis. An immunohistochemical study. J. Hepatol. 1992;15:361–366. doi: 10.1016/0168-8278(92)90069-2. [DOI] [PubMed] [Google Scholar]
- 53.Salem NA, Hamza A, Alnahdi H, Ayaz N. Biochemical and molecular mechanisms of platelet-rich plasma in ameliorating liver fibrosis induced by dimethylnitrosamine. Cell. Physiol. Biochem. 2018;47:2331–2339. doi: 10.1159/000491544. [DOI] [PubMed] [Google Scholar]
- 54.Liu X, et al. Differential proteomic analysis of dimethylnitrosamine (DMN)-induced liver fibrosis. Proteomics. 2017;17:22. doi: 10.1002/pmic.201700267. [DOI] [PubMed] [Google Scholar]
- 55.Kiziltas H, et al. Antioxidant properties of Ferulago angulata and its hepatoprotective effect against N-nitrosodimethylamine-induced oxidative stress in rats. Pharm. Biol. 2017;55:888–897. doi: 10.1080/13880209.2016.1270974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sferra R, et al. Expression of pro-fibrotic and anti-fibrotic molecules in dimethylnitrosamine-induced hepatic fibrosis. Pathol. Res. Pract. 2017;213:58–65. doi: 10.1016/j.prp.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Kawano T, et al. Noninvasive mapping of the redox status of dimethylnitrosamine-induced hepatic fibrosis using in vivo dynamic nuclear polarization-magnetic resonance imaging. Sci. Rep. 2016;6:32604. doi: 10.1038/srep32604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chooi KF, Kuppan Rajendran DB, Phang SS, Toh HH. The dimethylnitrosamine induced liver fibrosis model in the rat. J. Vis. Exp. 2016;112:e54208. doi: 10.3791/54208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang X, Zhang J, Jia L, Xiao S. Dicliptera Chinensis polysaccharides target TGF-β/Smad pathway and inhibit stellate cells activation in rats with dimethylnitrosamine-induced hepatic fibrosis. Cell. Mol. Biol. 2016;62:99–103. [PubMed] [Google Scholar]
- 60.Zhang K, et al. Hepatoprotective effects of Dicliptera chinensis polysaccharides on dimethylnitrosamine-induced hepatic fibrosis rats and its underlying mechanism. J. Ethnopharmacol. 2016;179:38–44. doi: 10.1016/j.jep.2015.12.053. [DOI] [PubMed] [Google Scholar]
- 61.George J, Chandrakasan G. Lactate dehydrogenase isoenzymes in dimethylnitrosamine induced hepatic fibrosis. J. Clin. Biochem. Nutr. 1997;22:51–62. [Google Scholar]
- 62.George J, Chandrakasan G. Biochemical abnormalities during the progression of hepatic fibrosis induced by dimethylnitrosamine. Clin. Biochem. 2000;33:563–570. doi: 10.1016/s0009-9120(00)00170-3. [DOI] [PubMed] [Google Scholar]
- 63.Lopategi A, George J, Nieto N. Hepatic stellate cells secretes osteopontin under oxidative stress and contributes to fibrogenic response mediated through integrin αvβ3 and PI3K/pAkt pathway. Hepatology. 2010;52(Suppl S1):1260A–1261A. [Google Scholar]
- 64.Tsutsumi M, George J, Nomura T, Hayashi N, Arisawa T. Serum osteopontin levels as a diagnostic marker for hepatic fibrosis. Alcohol. Clin. Exp. Res. 2012;36(Suppl S2):59A. [Google Scholar]
- 65.George J, Isabel Fiel M, Nieto N. Carbon tetrachloride-induced liver injury and fibrosis correlates with osteopontin expression in mice. Hepatology. 2010;52(Suppl S1):453A. [Google Scholar]
- 66.George J, Tsutsumi M, Takase S. Expression of hyaluronic acid in N-nitrosodimethylamine induced hepatic fibrosis in rats. Int. J. Biochem. Cell Biol. 2004;36:307–319. doi: 10.1016/s1357-2725(03)00253-x. [DOI] [PubMed] [Google Scholar]
- 67.George J, Stern R. Serum hyaluronan and hyaluronidase: very early markers of toxic liver injury. Clin. Chim. Acta. 2004;348:189–197. doi: 10.1016/j.cccn.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 68.George, J., Tsutsumi, M. & Tsuchishima, M. Alteration of trace elements during pathogenesis of N-nitrosodimethylamine induced hepatic fibrosis. Sci. Rep. (2019) 10.1038/s41598-018-37516-4. [DOI] [PMC free article] [PubMed]
- 69.George J. Determination of selenium during pathogenesis of hepatic fibrosis employing hydride generation and inductively coupled plasma mass spectrometry. Biol. Chem. 2018;399:499–509. doi: 10.1515/hsz-2017-0260. [DOI] [PubMed] [Google Scholar]
- 70.George J. Mineral metabolism in dimethylnitrosamine-induced hepatic fibrosis. Clin. Biochem. 2006;39:984–991. doi: 10.1016/j.clinbiochem.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 71.George J, Tsutsumi M. Epigallocatechin gallate treatment decreases osteopontin expression and attenuates N-Nitrosodimethylamine induced hepatic fibrosis in rats. Hepatology. 2014;60(Suppl S1):583A. [Google Scholar]
- 72.George J, Suguna L, Jayalakshmi R, Chandrakasan G. Efficacy of silymarin and curcumin on dimethylnitrosamine induced liver fibrosis in rats. Biomedicine. 2006;26:18–26. [Google Scholar]
- 73.George J, Tsutsumi M, D’Armiento J. MMP-13 deletion attenuates N-nitrosodimethylamine induced hepatic fibrosis in mice. Hepatology. 2010;52(Suppl S1):1284A. [Google Scholar]
- 74.George J, Tsutusmi M. Interfering of connective tissue growth factor mRNA protects N-nitrosodimethylamine induced toxic liver injury in rats. Hepatology. 2008;48(Suppl S1):912A–913A. [Google Scholar]
- 75.George J. Elevated serum beta-glucuronidase reflects hepatic lysosomal fragility following toxic liver injury in rats. Biochem. Cell Biol. 2008;86:235–243. doi: 10.1139/o08-038. [DOI] [PubMed] [Google Scholar]
- 76.George J, Tsutsumi M. Elevated serum beta-glucuronidase reflects hepatic lysosomal fragility following toxic liver injury in rats. Hepatology. 2008;48(Suppl S1):929A–930A. doi: 10.1139/o08-038. [DOI] [PubMed] [Google Scholar]
- 77.George J, D’Armiento J, Tsutsumi M. Human MMP-1 transgene protects experimentally induced hepatic fibrosis in mice. Hepatology. 2011;54(Suppl S1):1223A. [Google Scholar]
- 78.George J, Tsutusmi M, Takase S. Expression of TIMP-1 and TIMP-2 in N-nitrosodimethylamine induced hepatic fibrosis in rats. Hepatology. 2000;32:505A. doi: 10.1016/s1357-2725(03)00253-x. [DOI] [PubMed] [Google Scholar]
- 79.Adeleke GE, Adaramoye OA. Betulinic acid protects against N-nitrosodimethylamine-induced redox imbalance in testes of rats. Redox Rep. 2017;22:556–562. doi: 10.1080/13510002.2017.1322750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ezhilarasan D, Karthikeyan S. Silibinin alleviates N-nitrosodimethylamine-induced glutathione dysregulation and hepatotoxicity in rats. Chin. J. Nat. Med. 2016;14:40–47. doi: 10.3724/SP.J.1009.2016.00040. [DOI] [PubMed] [Google Scholar]
- 81.Taniguchi M, Yasutake A, Takedomi K, Inoue K. Effects of N-nitrosodimethylamine (NDMA) on the oxidative status of rat liver. Arch. Toxicol. 1999;73:141–146. doi: 10.1007/s002040050598. [DOI] [PubMed] [Google Scholar]
- 82.Gilgenkrantz H, Collin de l’Hortet A. Understanding liver regeneration: from mechanisms to regenerative medicine. Am. J. Pathol. 2018;188:1316–1327. doi: 10.1016/j.ajpath.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 83.Gligorijević N, Minić S, Križáková M, Katrlík J, Nedić O. Structural changes of fibrinogen as a consequence of cirrhosis. Thromb. Res. 2018;166:43–49. doi: 10.1016/j.thromres.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 84.Callea F, et al. Cirrhosis of the liver. A regenerative process. Dig. Dis. Sci. 1991;36:1287–1293. doi: 10.1007/BF01307524. [DOI] [PubMed] [Google Scholar]
- 85.Affo S, Yu LX, Schwabe RF. The role of cancer-associated fibroblasts and fibrosis in liver cancer. Annu. Rev. Pathol. 2017;12:153–186. doi: 10.1146/annurev-pathol-052016-100322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bishayee A. The role of inflammation and liver cancer. Adv. Exp. Med. Biol. 2014;816:401–435. doi: 10.1007/978-3-0348-0837-8_16. [DOI] [PubMed] [Google Scholar]
- 87.Thorgeirsson SS, Grisham JW. Molecular pathogenesis of human hepatocellular carcinoma. Nat. Genet. 2002;31:339–346. doi: 10.1038/ng0802-339. [DOI] [PubMed] [Google Scholar]
- 88.Wong N, et al. Genomic aberrations in human hepatocellular carcinomas of differing etiologies. Clin. Cancer Res. 2000;6:4000–4009. [PubMed] [Google Scholar]
- 89.Fan G, et al. DNA methylation biomarkers for hepatocellular carcinoma. Cancer Cell Int. 2018;18:140. doi: 10.1186/s12935-018-0629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zheng YF, Lu X, Zhang XY, Guan BG. The landscape of DNA methylation in hepatocellular carcinoma. J. Cell Physiol. 2019;234:2631–2638. doi: 10.1002/jcp.27077. [DOI] [PubMed] [Google Scholar]
- 91.Villanueva A, et al. DNA methylation-based prognosis and epidrivers in hepatocellular carcinoma. Hepatology. 2015;61:1945–1956. doi: 10.1002/hep.27732. [DOI] [PubMed] [Google Scholar]
- 92.Koyama Y, Brenner DA. Liver inflammation and fibrosis. J. Clin. Invest. 2017;127:55–64. doi: 10.1172/JCI88881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brempelis KJ, Crispe IN. Infiltrating monocytes in liver injury and repair. Clin. Transl. Immunol. 2016;5:e113. doi: 10.1038/cti.2016.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ramadori G, Moriconi F, Malik I, Dudas J. Physiology and pathophysiology of liver inflammation, damage and repair. J. Physiol. Pharmacol. 2008;59(Suppl 1):107–117. [PubMed] [Google Scholar]
- 95.Li P, He K, Li J, Liu Z, Gong J. The role of Kupffer cells in hepatic diseases. Mol. Immunol. 2017;85:222–229. doi: 10.1016/j.molimm.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 96.Luedde T, Schwabe RF. NF-κB in the liver--linking injury, fibrosis and hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2011;8:108–118. doi: 10.1038/nrgastro.2010.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu H, et al. The SMAC mimetic birinapant attenuates lipopolysaccharide-induced liver injury by inhibiting the tumor necrosis factor receptor-associated factor 3 degradation in Kupffer cells. Immunol. Lett. 2017;185:79–83. doi: 10.1016/j.imlet.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 98.Wheeler MD. Endotoxin and Kupffer cell activation in alcoholic liver disease. Alcohol Res. Health. 2003;27:300–306. [PMC free article] [PubMed] [Google Scholar]
- 99.Mekala S, et al. Cellular crosstalk mediated by platelet-derived growth factor BB and transforming growth factor β during hepatic injury activates hepatic stellate cells. Can. J. Physiol. Pharmacol. 2018;96:728–741. doi: 10.1139/cjpp-2017-0768. [DOI] [PubMed] [Google Scholar]
- 100.Kiagiadaki F, et al. Activin-A causes Hepatic stellate cell activation via the induction of TNFα and TGFβ in Kupffer cells. Biochim. Biophys. Acta Mol. Basis Dis. 2018;1864:891–899. doi: 10.1016/j.bbadis.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 101.Gressner AM. The cell biology of liver fibrogenesis - an imbalance of proliferation, growth arrest and apoptosis of myofibroblasts. Cell Tissue Res. 1998;292:447–452. doi: 10.1007/s004410051073. [DOI] [PubMed] [Google Scholar]
- 102.Rani V, Verma Y, Rana K, Rana SVS. Zinc oxide nanoparticles inhibit dimethylnitrosamine induced liver injury in rat. Chem. Biol. Interact. 2018;295:84–92. doi: 10.1016/j.cbi.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 103.Zhou Z, Xu MJ, Gao B. Hepatocytes: a key cell type for innate immunity. Cell. Mol. Immunol. 2016;13:301–315. doi: 10.1038/cmi.2015.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Horn TL, O’Brien TD, Schook LB, Rutherford MS. Acute hepatotoxicant exposure induces TNFR-mediated hepatic injury and cytokine/apoptotic gene expression. Toxicol. Sci. 2000;54:262–273. doi: 10.1093/toxsci/54.1.262. [DOI] [PubMed] [Google Scholar]
- 105.Wang L, Tu L, Zhang J, Xu K, Qian W. Stellate cell activation and imbalanced expression of TGF-β1/TGF-β3 in acute autoimmune liver lesions induced by Con-A in mice. Biomed Res. Int. 2017;2017:12. doi: 10.1155/2017/2540540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Meng F, et al. Interleukin-17 signaling in inflammatory, Kupffer cells, and hepatic stellate cells exacerbates liver fibrosis in mice. Gastroenterology. 2012;143:765–776. doi: 10.1053/j.gastro.2012.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Holt AP, Salmon M, Buckley CD, Adams DH. Immune interactions in hepatic fibrosis. Clin. Liver Dis. 2008;12:861–882. doi: 10.1016/j.cld.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ruart M, et al. Impaired endothelial autophagy promotes liver fibrosis by aggravating the oxidative stress response during acute liver injury. J. Hepatol. 2018;S0168-8278:32498-X. doi: 10.1016/j.jhep.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.DeLeve LD. Liver sinusoidal endothelial cells and liver regeneration. J. Clin. Invest. 2013;123:1861–1866. doi: 10.1172/JCI66025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Xie G, et al. Hedgehog signalling regulates liver sinusoidal endothelial cell capillarisation. Gut. 2013;62:299–309. doi: 10.1136/gutjnl-2011-301494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Machado MV, Diehl AM. Hedgehog signalling in liver pathophysiology. J. Hepatol. 2018;68:550–562. doi: 10.1016/j.jhep.2017.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Burt ADCL. Oakley Lecture (1993). Cellular and molecular aspects of hepatic fibrosis. J. Pathol. 1993;170:105–114. doi: 10.1002/path.1711700203. [DOI] [PubMed] [Google Scholar]
- 113.Zaldivar MM, et al. CXC chemokine ligand 4 (Cxcl4) is a platelet-derived mediator of experimental liver fibrosis. Hepatology. 2010;51:1345–1353. doi: 10.1002/hep.23435. [DOI] [PubMed] [Google Scholar]
- 114.Wang Y, Sun Y, Zuo L, Wang Y, Huang Y. ASIC1a promotes high glucose and PDGF-induced hepatic stellate cell activation by inducing autophagy through CaMKKβ/ERK signaling pathway. Toxicol. Lett. 2018;300:1–9. doi: 10.1016/j.toxlet.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 115.Bobowski-Gerard M, Zummo FP, Stael sB, Lefebvre P, Eeckhoute J. Retinoids issued from hepatic stellate cell lipid droplet loss as potential signaling molecules orchestrating a multicellular liver injury response. Cells. 2018;7:E137. doi: 10.3390/cells7090137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gressner OA, Weiskirchen R, Gressner AM. Evolving concepts of liver fibrogenesis provide new diagnostic and therapeutic options. Comp. Hepatol. 2007;6:7. doi: 10.1186/1476-5926-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wahlang B, McClain C, Barve S, Gobejishvili L. Role of cAMP and phosphodiesterase signaling in liver health and disease. Cell Signal. 2018;49:105–115. doi: 10.1016/j.cellsig.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.da Silva FM, et al. Hepatic stellate cell activation in vitro: cell cycle arrest at G2/M and modification of cell motility. J. Cell Biochem. 2003;90:387–396. doi: 10.1002/jcb.10642. [DOI] [PubMed] [Google Scholar]
- 119.Higashi. T, Friedman SL, Hoshida Y. Hepatic stellate cells as key target in liver fibrosis. Adv. Drug Deliv. Rev. 2017;121:27–42. doi: 10.1016/j.addr.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Weiskirchen R, Tacke F. Cellular and molecular functions of hepatic stellate cells in inflammatory responses and liver immunology. Hepatobiliary Surg. Nutr. 2014;3:344–363. doi: 10.3978/j.issn.2304-3881.2014.11.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Praktiknjo M, et al. Acute decompensation boosts hepatic collagen type III deposition and deteriorates experimental and human cirrhosis. Hepatol. Commun. 2018;2:211–222. doi: 10.1002/hep4.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Urtasun R, et al. Osteopontin, an oxidant stress sensitive cytokine, up-regulates collagen-I ia integrin α(V)β(3) engagement and PI3K/pAkt/NFκB signaling. Hepatology. 2012;55:594–608. doi: 10.1002/hep.24701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mak KM, Mei R. Basement membrane type IV collagen and laminin: an overview of their biology and value as fibrosis biomarkers of liver disease. Anat. Rec. (Hoboken) 2017;300:1371–1390. doi: 10.1002/ar.23567. [DOI] [PubMed] [Google Scholar]
- 124.Roderfeld M. Matrix metalloproteinase functions in hepatic injury and fibrosis. Matrix Biol. 2018;68-69:452–462. doi: 10.1016/j.matbio.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 125.Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat. Rev. Mol. Cell Biol. 2007;8:221–233. doi: 10.1038/nrm2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Puente XS, Sánchez LM, Overall CM, López-Otín C. Human and mouse proteases: a comparative genomic approach. Nat. Rev. Genet. 2003;4:544–558. doi: 10.1038/nrg1111. [DOI] [PubMed] [Google Scholar]
- 127.Afratis NA, Selman M, Pardo A, Sagi I. Emerging insights into the role of matrix metalloproteases as therapeutic targets in fibrosis. Matrix Biol. 2018;68-69:167–179. doi: 10.1016/j.matbio.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 128.El Hajj EC, et al. Alcohol modulation of cardiac matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs favors collagen accumulation. Alcohol Clin. Exp. Res. 2014;38:448–456. doi: 10.1111/acer.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cong M, et al. Antifibrotic effects of a recombinant adino-associated virus carrying small interfering RNA targeting TIMP-1 in rat liver fibrosis. Am. J. Pathol. 2013;182:1607–1616. doi: 10.1016/j.ajpath.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 130.Liu SB, et al. Lysyl oxidase activity contributes to collagen stabilization during liver fibrosis progression and limits spontaneous fibrosis reversal in mice. FASEB J. 2016;30:1599–1609. doi: 10.1096/fj.14-268425. [DOI] [PubMed] [Google Scholar]