Abstract
Experts in the field of interprofessional education (IPE) have called for the use of theory in curriculum design to produce better results with measurable outcomes. While evidence of this practice is growing in the IPE literature, publications about using theoretical approaches to inform curricular design in pharmacy education is nonexistent. This paper describes the process used at the University of Washington for developing a theoretically grounded framework to anchor and guide curriculum design. Faculty charged with implementing IPE at other institutions may learn from our team’s approach to co-creating an inclusive framework, developing a common philosophy, and applying appropriate theory in building a framework to guide curriculum development and IPE implementation.
Keywords: interprofessional education, curriculum, social identity, social learning, pharmacy education
BACKGROUND
In 2005, Freeth and colleagues reported that educators in the field of interprofessional education (IPE) had failed to use explicit theoretical underpinnings in curricular design.1 Reeves and colleagues also reported that most educators implicitly use general adult learning principles and only a few interprofessional interventions have employed an explicit theoretical/conceptual approach.2,3 Yet, use of theoretical approaches to support design and evaluation of IPE activities has been identified as essential to produce pedagogically sound and effective curricula that achieve desired outcomes.4,5 In fact, multiple scholars in the IPE field have published guidelines that emphasize use of theoretical frameworks in designing and evaluating IPE curricula.6-11 In 2015, the Institute of Medicine (IOM) underscored the importance of systematic development of interprofessional activities along the learning continuum in the Interprofessional Learning Continuum (IPLC) Model.12 This comprehensive concept model provides an example of a framework that can greatly enhance the purpose of IPE interventions and their potential impact.12 Adoption of a conceptual model to guide IPE is important for bringing vision and clarity to an IPE implementation plan across an organization.13,14 Yet, pharmacy education literature is lacking in published theories to support curriculum and instructional design.
While the University of Washington (UW) has had a long history with IPE, the need for a theory-based approach and common framework arose in early 2014 after IPE events began to be required of students on a broader scale.15,16 A collection of IPE activities involving pharmacy, social work, dentistry, physician assistant and health administration students were embedded within coursework in the Doctor of Nursing Practice program and a yearlong series of small discussion groups was coordinated across the six UW Health Sciences schools (Dental, Nursing, Medicine, Pharmacy, Public Health, and Social Work) and the Health Administration (MHA), Physician Assistant (PA), and Dietetics programs. Evaluations of these individual activities were positive, yet faculty reported needing a developmental and pedagogical anchor to ground IPE efforts. Therefore, the IPE faculty team began the process of dialogue and reflection to develop a theory-driven curricular framework that could guide IPE efforts at the UW.
Multiple theories have been proposed to support interprofessional learning and development. Contact and social identity theory are commonly cited as theoretical grounding upon which to design IPE curricula.17-21 Contact theory – originally developed by Alloport as contact hypothesis22 – focuses on intergroup relations as the foundation to understand social interactions and prejudicial biases. Its four main conditions – equal status, cooperation, common goals, and social and institutional support – align with the principles of IPE.22 As such, it can be used as a theoretical premise in IPE, which strives to foster collaboration and teamwork. Groups of learners must have more than mere contact with each other to develop skills for interprofessional collaborative practice. Learners must have the opportunity to develop interpersonal communication skills that will begin to break down hierarchical silos, contribute to mutual respect, work on common goals, and engage in shared decision making. Those opportunities take the form of shared learning opportunities early in the training of health professions students. Thus, this theory supports structuring IPE curricula to bring learners at similar levels in their educational development together in active problem-solving situations. If designed well, such cooperation allows learners to address and modify their perceptions of each other, thus building relationship.
Social identity theory is a theory of inter-group relations but is based on the premise that learners derive their identity from membership in social groups, especially if the group identity is viewed as positive.23 Group membership influences a person’s perceptions of their own position in different social contexts as well as their perceptions of others. Consequently, health profession students developing their professional identity as they participate in IPE come to value collaboration if they build positive relationships with fellow learners, develop a sense of team membership(s), and perceive that their roles on the team(s) is desirable. A curriculum with repeated experiences over time where learners successfully cooperate in teams would presumably provide the structure for building group membership and professional identities; thus, facilitating development of skill-based competencies in team-based care.
Even when grounded in appropriate theory, curricular development of IPE without effective evaluation and assessment strategies does not allow for quality improvement and affects sustainability.24 The modified Kirkpatrick outcome model has become widely accepted as the framework for evaluation of IPE with a growing imperative to move beyond measuring reactions, attitudes, and perceptions of individual IPE activities and focus on behavioral and organizational change.7 Curricular effectiveness is ultimately demonstrated through changes in behavior, organizational change, and improvement in patient outcomes. This has been underscored in the IOM report examining the outcomes of IPE.25 Therefore, a pedagogically grounded curriculum design that aligns with the Kirkpatrick evaluation framework presents the potential for producing measurable change in team behavior over time. This paper will describe the process in developing a theory-based framework to guide curriculum development across multiple health professions programs. Understanding this framework development process can be useful to other pharmacy schools and colleges that seek to develop a curriculum that builds interprofessional team competency over time rather than simply offer an assortment of exposures to other professions.
FRAMEWORK DEVELOPMENT
Development of this framework involved a series of iterative steps, the first of which was to build a common philosophy for how and why interprofessional learning occurs in students. A group of core faculty with expertise in curricular development met to compare curricula and examine accreditation standards for IPE across multiple health science schools and programs. Through this work, faculty identified areas of common content across the programs and where students would be at similar knowledge and skill levels. For example, the medical, pharmacy, undergraduate nursing, and physician assistant programs were found to cover cardiovascular disease states and treatments during the same month, so a case activity dealing with heart failure was built and offered then. Discovering common content areas across the health sciences curricula and creating learning activities that addressed these content areas led to the emergence of a shared philosophy – that learning specific content together would promote mutually beneficial and respectful relationships and support sportsmanship – consistent with contact and social identity theories. The faculty committed to leveraging these points in time to allow students to work repeatedly in consistent teams.
After articulating our shared philosophy, we then worked to build a concrete framework consistent with this philosophy by mapping the Core Competencies for Interprofessional Collaborative Practice (IPEC sub-competencies)26 on to the Kirkpatrick evaluation domains (adapted from the Kirkpatrick program evaluation model).27 As an interprofessional team of IPE-expert faculty, we conducted provisional coding28 to categorize the 38 IPEC sub-competencies into the Kirkpatrick model domains (reaction, attitudes, knowledge, behavior change, change in practice).27 We used an iterative process with bi-weekly meetings to resolve discrepancies that allowed us to reflect upon the “how” and “why” competencies were mapped into certain Kirkpatrick levels. Although these iterations lengthened the mapping process, it prompted thoughtful dialogue that provided us with the reassurance that final decisions were deliberate and meaningful. This mapping process allowed us to clearly identify which sub-competencies were better suited to impacting reactions/attitudes, knowledge or behavior.
We then independently performed axial coding28 of the categorized sub-competencies according to three domains adapted from learning trajectory models developed by the Universities of Alberta and British Columbia.29,30 These models posit that learning occurs developmentally and curricula should be structured such that learners move through exposure, immersion and mastery learning activities.29 The Interprofessional Learning Pathway developed by the University of Alberta identified these stages as exposure, immersion and integration.30 Both of these approaches have underpinnings similar to contact and identity theory in that learners are progressively and repeatedly immersed in experiences that provide interactions with others which in turn, shapes their individual and joint professional development. Similar to what was done with the IPEC competencies and the Kirkpatrick model, we iteratively compared and resolved discrepancies until we reached consensus on which sub-competencies were better targeted in each of the learning stages (exposure, immersion, integration). By overlaying the two mapping products, the blending of categorized sub-competencies according to the Kirkpatrick and Canadian models created an overall curricular framework. This framework could then guide the development of specific curricula targeting IPEC domains (values and ethics; roles and responsibilities; communication; and teamwork) so that it was sequenced in accordance to the learning trajectory.
We vetted the framework systematically with internal stakeholders. First, the framework was introduced to the UW Health Sciences IPE Implementation Committee which sponsors IPE activities. This committee is comprised of representatives from each of the six Health Science Schools. Overall, the response was positive; feedback that exposure-type activities should be repeated throughout the curriculum was incorporated. Second, the framework was circulated to six interprofessional focus groups between January and April 2015, as part of an ongoing UW Health Sciences IPE planning process. Focus groups were comprised of faculty and students from the six health science schools and clinical practice partners from several health systems in the Puget Sound area. Again, feedback was positive with suggestions for minor changes which were adopted.
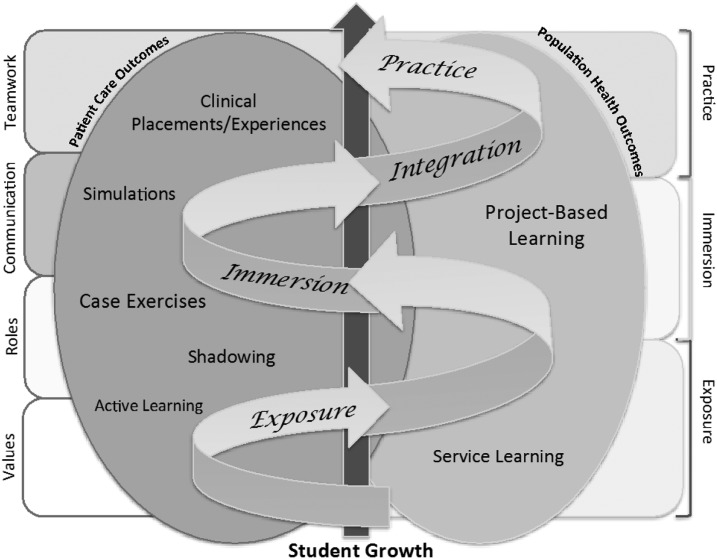
The final version of the UW IPE curricular framework (Figure 1) displays potential activities that systematically progress over time from exposure in the classroom to immersion in simulations and ending with integration of skills into practice. Assessing competency in interprofessional practice begins with measuring shift in values and increased knowledge about roles and responsibilities. Changes in attitudes and knowledge occur with additional exposure and introduction to immersion activities. As students participate in simulations, they begin to learn new behaviors. But actual behavior change does not occur until learners enter practice settings where they experience interdependency and collaboration in taking care of patients with their peers. The left side of the figure represents IP learning in the context of patient care outcomes while the right side represents IP learning in the context of community or population health. The right side of the figure shows how service learning and project-based learning are included as examples of activities aimed at population health outcomes. While the foundations and concepts of effective teamwork are assessed throughout the interprofessional curriculum, actual teamwork behaviors are evaluated toward the end of the curriculum as learners integrate their individual professional knowledge and competency with interprofessional interaction and display team behavior. Importantly, the IPEC learning domains are not mutually exclusive or unidirectional. As learners move back and forth across the learning continuum between classroom and clinical practice, they build and rebuild competencies of interprofessional collaborative practice, from understanding roles and responsibilities, to gaining skills in teamwork and team communication, to displaying changes in team behaviors; and eventually becoming competent.
Figure 1.
University of Washington Health Sciences Curricular Framework for IPE.
The curricular framework was presented across multiple external interprofessional audiences over a 2-year period (2015-2017).31-37 These audiences included faculty and staff from multiple professions with differing levels of experience in IPE design. Responses to the framework were overwhelmingly positive with few suggested modifications throughout this vetting process. In 2017, the framework was reviewed and approved by the steering committee for the UW Center for Health Sciences Interprofessional Education, Research and Practice (CHSIE) and subsequently presented to the IPE committees in each of the UW Health Science schools for their adoption and use.
FRAMEWORK IMPLEMENTATION
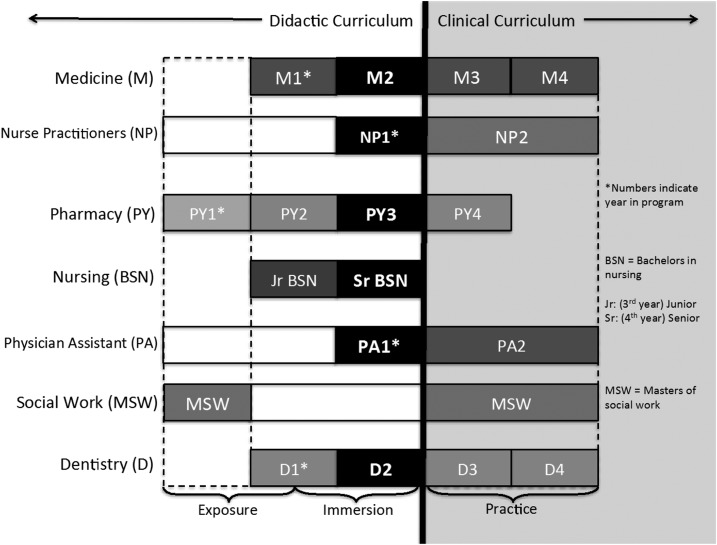
The UW CHSIE uses the framework in conjunction with the IPLC Model from the IOM to guide curriculum development. Whenever possible, students are matched across health professions based on their knowledge and skill levels in their respective programs (Figure 2). Because of the widely disparate content in the first year of the Health Professions curricula, we began implementation in the second year. A blend of exposure and immersion activities were inserted including a series of small group discussions (three per year, six hours total) and interprofessional shadowing experiences in practice settings (two to four hours total). In the third year of the program, immersion experiences in the form of high fidelity clinical reasoning and team communication simulations (three per year, 12 hours total) with medicine and nursing were initiated. In both the second and third years of the pharmacy program, students are matched with students in the other health professions and assigned to teams that stay together through multiple experiences over an academic year. This design – consistent with the social contact and identity theoretical underpinnings – promotes social connection and fosters trust among students, which facilitates development of a professional identity together.
Figure 2.
Matching Schema for IPE at the University of Washington Health Sciences.
IPE curriculum implementation in the fourth professional year began with measuring baseline students’ interprofessional interactions, collaboration opportunities and teamwork behaviors in practice settings (emphasis on third level of Kirkpatrick model). Responses from both students and preceptors indicated that opportunities for interprofessional interactions to foster team competency exist, yet intentional progression in clinical settings is not consistent.38-40 Consequently, faculty development and preceptor training to coach students in team performance is being developed as an intervention to support explicit teamwork and collaborative practice, followed by creating behaviorally grounded items for assessing student performance on teams that are common across multiple professions.
IMPLICATIONS
Blending concepts from the University of Alberta and UBC IPE models with the Kirkpatrick assessment model into a curricular framework has allowed our academic institution to conceptually visualize how ongoing IPE activities may be integrated in a pedagogically logical manner. Further, it has provided organization and prioritization to guide new IPE offerings. With acceptance of the curricular framework, the UW Health Sciences schools have a coordinated, systematic and progressive strategy to design IPE. The framework has in effect created a road map of IPE curricular development across multiple schools and programs.
Using contact and social identity theory as the foundation for curriculum has facilitated progressive implementation of IPE in the pharmacy school. As described previously, a series of high fidelity clinical reasoning simulations were implemented for third-year pharmacy students where teams were to remain constant over time to foster a sense of team identity – consistent with contact theory.20,41 However, scheduling difficulties with other coursework precluded pharmacy students from participating in the same teams throughout all simulations the first year. Because of the lack of sustained teams, it was not surprising that student evaluations indicated learning occurred at the lowest level of the framework (primarily shift in values rather than change in behavior). Student comments demonstrated their insight into the importance of teams but did not show that they attained team cohesion and trust. They spoke of the necessity for effective communication for team-based care but did not speak to their experience as being part of a team.
The following year, pharmacy students were scheduled into consistent teams across multiple clinical reasoning simulations. Student evaluations demonstrated a greater sense of teamwork, as contact theory would suggest. They expressed equal status with their colleagues and an enhanced professional identity. They spoke of working side-by-side with other professionals as part of a team. They stated they felt validated as a member of the pharmacy profession.
Many theories can be used to inform IPE, yet effective application of a specific theory to curriculum development can be imprecise.42,43 Consequently, contact and social identity theory may not fully characterize our framework. In fact, interprofessional socialization could occur in the context of social capital theory, which is based on tenets that include: network characteristics (frequency of participation and cohesion among team members), external resources (matching of professional knowledge and skills of team members), internal resources (self-efficacy of team members), trust between team members, and ground rules and norms set by team members.44,45 As we continue to use and refine our framework, we may find aspects of additional theories useful in informing our curricular development and choosing appropriate assessment strategies. Our framework, nonetheless, has provided clarity of vision for faculty from multiple schools and has moved UW toward a shared mental model for IPE. The framework has been useful in guiding both central and individual school decisions with respect to priorities and resource allocation. As a result, implementing IPE across multiple schools and programs has progressed beyond merely meeting accreditation standards to a pedagogically grounded approach to IPE that trains students for interprofessional collaborative practice. Other schools and institutions may find it useful to identify a common philosophy for how students learn and practice to engage in collaborative practice. Having a shared mental model across health professions schools and programs is essential to guide planning, instruction and appropriate assessment of IPE.
CONCLUSION
The curricular framework conceptualized and developed through joint faculty effort with supporting theory is effectively guiding curricular development, facilitating implementation of IPE, and informing evaluation efforts across multiple health professional programs at UW. Using theory and pedagogy as a foundation to inform IPE is essential to creating sound, meaningful, and effective curricula to ensure students are “collaborative-practice ready” in health care delivery.
ACKNOWLEDGMENTS
We would like to thank Drs. Brenda Zierler, Karen McDonough and Susan Kemp for their contributions and thoughtful dialogue throughout this process.
REFERENCES
- 1.Freeth D, Hammick M, Reeves S, Koppel I, Barr H. Effective Interprofessional Education: Development, Delivery & Evaluation. Oxford, UK: Blackwell Publishing; 2005. [Google Scholar]
- 2.Reeves S. Ideas for the development of the interprofessional field. J Interprof Care. 2010;24(3):217–219. doi: 10.3109/13561821003788930. [DOI] [PubMed] [Google Scholar]
- 3.Reeves S, Goldman J, Gilbert J, et al. A scoping review to improve conceptual clarity of interprofessional interventions. J Interprof Care. 2011;25(3):167–174. doi: 10.3109/13561820.2010.529960. [DOI] [PubMed] [Google Scholar]
- 4.Clark P. What would a theory of interprofessional education look like? Some suggestions for developing a theoretical framework for teamwork training. J Interprof Care. 2006;20(6):577–589. doi: 10.1080/13561820600916717. [DOI] [PubMed] [Google Scholar]
- 5.Reeves S, Hean S. Why we need theory to help us better understand the nature of interprofessional education, practice and care. J Interprof Care. 2013;27(1):1–3. doi: 10.3109/13561820.2013.751293. [DOI] [PubMed] [Google Scholar]
- 6.Barr H. Toward a theoretical framework for interprofessional education. J Interprof Care. 2013;27(1):4–9. doi: 10.3109/13561820.2012.698328. [DOI] [PubMed] [Google Scholar]
- 7.Thistlewaite JE, Forman D, Matthews LR, Rogers GD, Steketee C, Yassine T. Competencies and frameworks in interprofessional education: a comparative analysis. Acad Med. 2014;89(6):869–875. doi: 10.1097/ACM.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 8.Moran MC, Steketee C, Forman D, Dunston R. Using a research-informed interprofessional curriculum framework to guide reflection and future planning of interprofessional education in a multi-state context. J Res Interprof Prac Educ. 2015;5(1):1–13. [Google Scholar]
- 9.Reeves S, Boet S, Zierler B, Kitto S. Interprofessional education and practice guide No. 3: evaluating interprofessional education. J Interprof Care. 2015;29(4):305–312. doi: 10.3109/13561820.2014.1003637. [DOI] [PubMed] [Google Scholar]
- 10.Thistlewaite J, Kumar K, Moran M, Saunders R, Carr S. An exploratory review of pre-qualification interprofessional education evaluations. J Interprof Care. 2015;29(4):292–297. doi: 10.3109/13561820.2014.985292. [DOI] [PubMed] [Google Scholar]
- 11.Anderson E, Smith R, Hammick M. Evaluating an interprofessional education curriculum: a theory-informed approach. Med Teach. 2016;38(4):385–394. doi: 10.3109/0142159X.2015.1047756. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine of the National Academies. Measuring the impact of inteprofessional education on collaborative practice and patient outcomes. http://www.nationalacademies.org/hmd/∼/media/Files/Report%20Files/2015/IPE_RAAG.pdf. Accessed March 5, 2018.
- 13.Kahaleh A, Danielson D, Franson KL, Nuffer WA, Umland EM. An interprofessional education panel on development, implementation, and assessment strategies. Am J Pharm Educ. 2015;79(6):Article 78. doi: 10.5688/ajpe79678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brewer M. Exploring the potential of a capability framework as a vision and “sensemaking” tool for leaders of interprofessional education. J Interprof Care. 2016;30(5):574–581. doi: 10.1080/13561820.2016.1182969. [DOI] [PubMed] [Google Scholar]
- 15.Odegard PS, Robins L, Murphy N, et al. Interprofessional initiatives at the University of Washington. Am J Pharm Educ. 2009;73(4):Article 63. doi: 10.5688/aj730463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willgerodt MA, Abu-Rish Blakeney E, Brock DM, Liner D, Murphy N, Zierler B. Interprofessional education and practice guide No. 4: developing and sustaining interprofessional education at an academic health center. J Interprof Care. 2015;29(5):421–425. doi: 10.3109/13561820.2015.1039117. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter J, Dickinson C. Understanding interprofessional education as an intergroup encounter: the use of contact theory in programme planning. J Interprof Care. 2016;30(1):103–108. doi: 10.3109/13561820.2015.1070134. [DOI] [PubMed] [Google Scholar]
- 18.Thistlethwaite J. Interprofessional education: a review of context, learning and the research agenda. Med Educ. 2012;46(1):58–70. doi: 10.1111/j.1365-2923.2011.04143.x. [DOI] [PubMed] [Google Scholar]
- 19.Mohaupt J, van Soeren M, Andrusyszyn MA, MacMillan K, Devlin-Cop S, Reeves S. Understanding interprofessional relationships by the use of contact theory. J Interprof Care. 2012;26(5):370–375. doi: 10.3109/13561820.2012.673512. [DOI] [PubMed] [Google Scholar]
- 20.Barr H. Toward a theoretical framework for interprofessional education. J Interprof Care. 2013;27(1):4–9. doi: 10.3109/13561820.2012.698328. [DOI] [PubMed] [Google Scholar]
- 21.Carpenter J, Dickinson C. Understanding interprofessional education as an intergroup encounter: the use of contact theory in programme planning. J Interprof Care. 2016;30(1):103–108. doi: 10.3109/13561820.2015.1070134. [DOI] [PubMed] [Google Scholar]
- 22.Allport GW. The Nature of Prejudice. Reading, MA: Addison-Wesley; 1954. [Google Scholar]
- 23.Hogg M, Abrams D. Social Identifications: A Social Psychology of Intergroup Relations and Group Processes. New York, NY: Routledge, Taylor & Francis Group; 1998. [Google Scholar]
- 24.Reeves S, Boet S, Zierler B, Kitto S. Interprofessional education and practice guide No. 3: evaluating interprofessional education. J Interprof Care. 2015;29(4):305–312. doi: 10.3109/13561820.2014.1003637. [DOI] [PubMed] [Google Scholar]
- 25.Reeves S, Palaganas J, Zierler B. Institute of Medicine, Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. Washington, DC: The National Academies Press; 2015. Synthesis of interprofessional education reviews; pp. 135–145. [PubMed] [Google Scholar]
- 26.Interprofessional Education Collaborative. Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative; 2016. https://hsc.unm.edu/ipe/resources/ipec-2016-core-competencies.pdf.
- 27.Barr H, Koppel I, Reeves S, Hammick M, Freeth D. Effective Interprofessional Education. Argument, Assumption & Evidence. Oxford, UK: Blackwell Publishing; 2005. [Google Scholar]
- 28.Saldana J. The Coding Manual for Qualitative Researchers. 2nd ed. London, UK: Sage; 2013. p. 303. [Google Scholar]
- 29.Charles G, Bainbridge L, Gilbert J. The University of British Columbia model of interprofessional education. J Interprof Care. 2010;24(1):9–18. doi: 10.3109/13561820903294549. [DOI] [PubMed] [Google Scholar]
- 30.Health Sciences Education and Research Commons. University of Alberta,Virtual Interprofessional Educator Resource (VIPER). Interprofessional Learning Pathway Competency Framework. https://sites.ualberta.ca/∼hsercweb/viper/Competency_Framework.pdf. Accessed March 5, 2018.
- 31. Danielson J, Shrader S, Willgerodt M, Haizlip J. Coaching skills toolkit: training faculty and preceptors for interprofessional practice. American Association of Colleges of Pharmacy Annual Meeting. Nashville, TN; 2017.
- 32. Willgerodt M, Danielson J. IPE/CP Curricular Development and Evaluation. Sinclair College Interprofessional Health Day, Faculty Workshop. Dayton, OH; 2017.
- 33. Danielson J, Willgerodt M. Level up: moving IPE forward in health professions education. Faculty development workshop and keynote. University of Alaska. Anchorage, AK; 2016.
- 34. Willgerodt M, Danielson J, Mendenhall P. Moving interprofessional education into practice. Collaborative Practice in Gerantology Practice (Conference): Translating Academics into Practice. Husson University. Bangor, ME; 2016.
- 35. Willgerodt M, Danielson J. Integrating interprofessional education, practice, and collaboration into master’s education. American Association of Colleges of Nursing Masters Education Conference. Tampa Bay, FL; 2014.
- 36. Willgerodt M, Danielson J. Bridging it all together: integrating and evaluating interprofessional education in the curricula. Faculty Development Workshop. University of Nebraska Medical Center. Omaha, NE; 2014.
- 37. Willgerodt M, Danielson J. The missing piece: facilitation skills within and across professions. Faculty development workshop. University of Nebraska Medical Center. Omaha, NE; 2014.
- 38. Clifton J, Danielson J, Weber S. A two-lens view: measuring interprofessional education (IPE) during APPEs. American Association of Colleges of Pharmacy Annual Meeting. National Harbor, MD; 2015.
- 39. Danielson J, Kim A, Bansal A, Weber S. An interprofessional education (IPE) fingerprint for APPEs: developing metrics for collaborative interactions. American Association of Colleges of Pharmacy Annual Meeting. Grapevine, TX; 2014.
- 40.Danielson J, Kim AP, Bansal A, Weber S. An interprofessional fingerprint for APPEs: developing metrics for collaborative interactions. AACP Experiential Education Section Newsletter. 2014;2(1-2) [Google Scholar]
- 41.Hean S, Dickinson C. The contact hypothesis: an exploration of its further potential in interprofessional education. J Interprof Care. 2005;19(5):480–491. doi: 10.1080/13561820500215202. [DOI] [PubMed] [Google Scholar]
- 42.Craddock D, O’Halloran C, McPherson K, Hean S, Hammick M. A top-down approach impedes the use of theory? Interprofessional education leaders’ approaches to curriculum development and the use of learning theory. J Interprof Care. 2013;27(1):65–72. doi: 10.3109/13561820.2012.736888. [DOI] [PubMed] [Google Scholar]
- 43.Hean S, Craddock D, Hammick M. Theoretical insights into interprofessional education: AMEE Guide No. 62. Med Teach. 2012;34(2):e78–e101. doi: 10.3109/0142159X.2012.650740. [DOI] [PubMed] [Google Scholar]
- 44.Hean S, O’Halloran C, Craddock D, Hammick M, Pitt R. Testing theory in interprofessional education: social capital as a case study. J Interprof Care. 2013;27(1):10–17. doi: 10.3109/13561820.2012.737381. [DOI] [PubMed] [Google Scholar]
- 45.Khalili H, Orchard C, Laschinger HK, Farah R. An interprofessional socialization framework for developing interprofessional identity among health professions students. J Interprof Care. 2013;27(6):448–453. doi: 10.3109/13561820.2013.804042. [DOI] [PubMed] [Google Scholar]