Abstract
Kumamoto was hit by a series of strong earthquakes beginning on April 14, 2016. We treated many deep vein thrombosis (DVT) patients and pulmonary thrombosis (PTE) patients. We came up with a strategy for diagnosis and therapy of venous thromboembolism (VTE). For VTE patients, we prescribed anticoagulant drugs, mainly direct oral anticoagulant (DOAC). To evaluate the validity and safety of the medical strategy for VTE in disasters, we investigated the prognosis of VTE patients at 4 months after the initial quake. In the two months following the initial quake we attended to 43 VTE patients, 11 PTE patients (including 9 patients with both DVT and PTE) and 32 DVT patients. We prescribed DOAC to 34 patients and Warfarin to 4 patients. Based on the survey at 4 months after the first tremblor, the period of anticoagulation therapy was 95.0±17.2 days for PTE and 57.1±36.5 days for DVT and 12 patients were continuing to take anticoagulant drugs. There were no recurrent VTE or bleeding events. DOAC therapy of VTE is therefore considered effective and safe in the event of a natural disaster. (This is a translation of J Jpn Coll Angiol 2017; 57: 33–40.)
Keywords: venous thromboembolism, deep vein thrombosis, pulmonary thromboembolism, direct oral anticoagulant
Introduction
On April 14, 2016, a series of earthquakes struck Kumamoto and its surrounding regions, including a foreshock, followed by the mainshock with a magnitude of 7, and aftershocks. Even at the time of writing this paper at 6 months following the earthquake, aftershocks could be occasionally felt.
Since the 2004 Chuetsu Earthquake in Niigata prefecture, it has been noted that the incidence of venous thromboembolism (VTE), including pulmonary thromboembolism (PTE) and deep vein thrombosis (DVT), increases after a disaster. In Japan, it has come to be known that the prevention, early detection, and early treatment of VTE related to earthquakes are all crucial.1)
Early after the Kumamoto Earthquake, many medical teams from inside and outside of Kumamoto prefecture, including our hospital, were gathered on-site. Services provided at the time of crisis included educational activities for the prevention of VTE, distribution of compression stockings, physical examination (PE), and lower limb ultrasonography (US). Our hospital, being the designated disaster base hospital closest to the epicenter, treated many patients with PTE and DVT. During normal non-disaster times, patients with VTE are generally treated in the Department of Cardiovascular Medicine or the Department of Cardiovascular Surgery, where care is provided based on the Japanese Circulation Society guidelines for the diagnosis, treatment, and prevention of PTE and DVT2) as well as the antithrombotic therapy and prevention of thrombosis evidence-based clinical practice guidelines of the American College of Chest Physicians (ACCP).3) After an earthquake, however, the time allocated for general outpatient medical care in normal periods became entirely occupied by the emergency care system. During this time, we expect that throughout the hospital there would be limited time for examination and drug administration, and thus, the number of patients with VTE would increase. Therefore, for the diagnosis and treatment of VTE, special measures that are different from those used in normal periods are deemed necessary. This study aimed to clarify the safety and usefulness of direct oral anticoagulant (DOAC) treatment by examining the state of VTE treatment and treatment progress after an earthquake at our hospital and examining the prognosis at 4 months after the earthquake.
Subjects and Methods
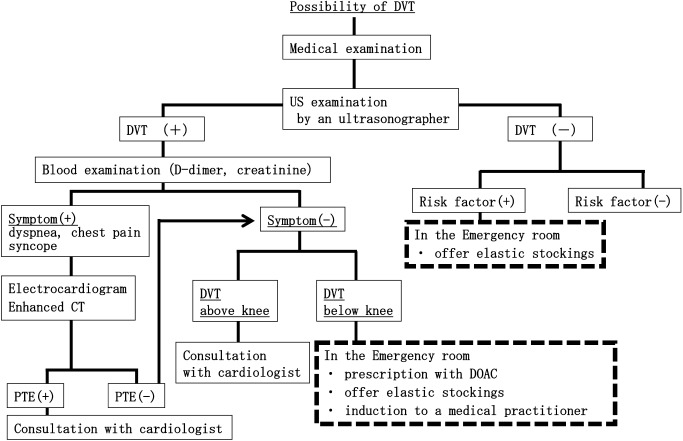
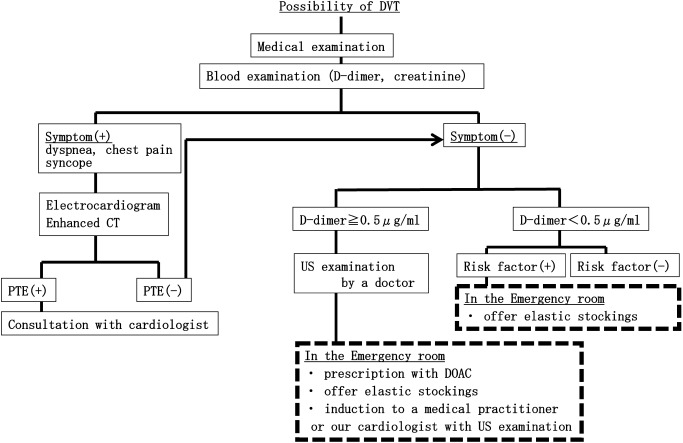
The subject sample included patients with VTE diagnosed at our hospital during the 2-month period after the earthquake from April 14, 2016 to June 14, 2016. To minimize treatment variability even if treated by a physician who rarely encounter VTE in routine medical practice, medical care was provided based on a DVT treatment flow chart created by the Department of Cardiovascular Medicine (Fig. 1A: weekly day shift schedule, Fig. 1B: evening and night shift schedule). Deep vein thrombi confirmed by lower limb US were diagnosed as DVT, whereas thrombi in the pulmonary artery confirmed by computed tomography (CT) were diagnosed as PTE. Even in the absence of lower limb US to evaluate concurrent DVT in patients with PTE, it was diagnosed as concurrent DVT if thrombi in the lower limbs were confirmed by contrast CT. D-dimer levels were measured using the latex immune-nephelometry method (Nanopia D dimer, Sekisui Medical Inc.), and the reference value was ≤1.0 µg/mL. For treatment at night, if the D-dimer level was <0.5 µg/mL, the possibility of DVT was considered low. In patients with D-dimer level ≥0.5 µg/mL, the presence or absence of DVT was confirmed using lower limb US performed by a physician. For patients diagnosed with VTE, treatment was generally initiated with anticoagulant therapy, and the first choice of treatment was DOAC. In such patients, the patient background, examination methods, treatment in hospital, and diagnosis and treatment methods were examined. For risk factors of VTE present at onset, the presence or absence of congenital factors, such as protein C deficiency, was determined, as well as acquired factors, including surgery, obesity, bed rest, malignant tumor, trauma, and fracture, based on self-assessment during noting medical history as well as medical charts obtained from our hospital.2) Obesity was defined as body mass index (BMI) ≥25 kg/m2.4) Follow-up treatment and progress were surveyed and analyzed 4 months after the earthquake. Patients who were unable to come for follow-up at our hospital were surveyed by telephone.
Fig. 1A Strategy of diagnosis and therapy for DVT during the day.
Fig. 1B Strategy of diagnosis and therapy for DVT during the night.
We showed the strategy of a medical treatment of DVT and PTE partly modified from the actual version. DVT: deep vein thrombosis; PTE: pulmonary thromboembolism; DOAC: direct oral anticoagulant
This study was conducted with the approval of the Ethical Review Board of Japan Red Cross Kumamoto Hospital. The database used in the present study was stored after performing linkable anonymization.
Results
The state of VTE response at our hospital
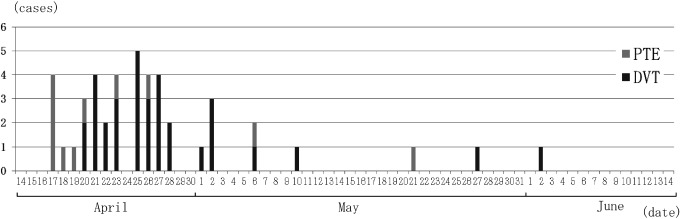
During the 2-month period after the earthquake, 43 patients were diagnosed with VTE at our hospital. This included 32 patients with DVT alone, 11 patients with PTE, and 9 patients with confirmed concurrent DVT and PTE. Patients with PTE were reported ≥4 days after the earthquake, and patients with DVT were reported ≥7 days after the earthquake (Fig. 2). The number of patients brought to our attention for VTE peaked 12 days after the earthquake (April 25), i.e., 5 patients.
Fig. 2 Time course changes in the number of VTE patients attending our hospital.
The number of VTE patients from April 14th 2016 to June 14th 2016 are shown. We treated 43 patients (11 PTE patients and 32 DVT patients). PTE: pulmonary thromboembolism; DVT: deep vein thrombosis
Regarding the reception of patients at our hospital in usual time, patients transported by ambulance are treated as an emergency, whereas all other patients are treated as outpatients if received during weekday outpatient business hours. After weekday outpatient business hours, patients are generally treated by emergency outpatient services. As disaster response immediately after the earthquake, that is, from 21:35 on April 14, an emergency outpatient service was opened to receive all patients at all periods of time, and this same system continued until the general outpatient services were reopened on April 20, that is, 7 days after the earthquake. For patients with VTE, all patients with PTE received emergency treatment. Half of patients with PTE were transported via ambulance, and the remaining patients consulted the emergency outpatient services during the disaster response period or after hours. Among the 32 patients with DVT, 2 patients were transported via ambulance and 22 consulted the emergency outpatient services (via walk-in services); therefore, 24 patients received emergency treatment. The reason for consultation in patients with DVT included a recommendation by mobile medical care units in 17 patients, referral from the family doctor or municipal hospital in 6 patients, and direct consultation without referral in 9 patients.
Patient background
PTE was observed in 2 men and 9 women, with mean age of 62.2±15.2 (33–91) years [mean±standard deviation (range)], body weight (BW) of 67.5±15.7 kg, and creatinine clearance (CCr) of 97.3±41.5 mL/min (Table 1). DVT was observed in 7 men and 25 women, with the mean age of 68.4±16.1 (33–94) years, BW of 58.0±15.4 kg, and CCr of 83.3±53.2 mL/min. For risk factors of VTE, there were no cases of trauma, surgery, pregnancy, or lower limb paralysis; however, there were patients with carcinoma (CA) receiving chemotherapy and patients taking oral corticosteroids. Obesity was observed in 6 patients with PTE and 13 with DVT. Regarding PTE, all patients presented symptoms including complaints of respiratory discomfort and chest pain or disturbance of consciousness. Regarding DVT, 26 patients presented with lower limb edema and pain; however, six patients were asymptomatic but consulted upon having thrombi identified by lower limb US performed in mobile medical care. The main sleeping place at the time of consultation among patients with PTE was a car in 9 patients and shelter in 2 patients, whereas, among patients with DVT, the corresponding data were 9 and 12 patients, respectively. Furthermore, the number of nights spent sleeping in their car until the time of consultation was 3.9±3.6 (0–12) nights among patients with PTE and 4.2±4.1 (0–12) nights among patients with DVT. Finally, 1 patient with PTE and 12 patients with DVT did not sleep in their car.
Table 1 Characteristics of subjects.
| Characteristics | PTE (n=11) | DVT (n=32) | Total (n=43) |
|---|---|---|---|
| Age (years), mean±SD | 62.2±15.2 | 68.4±16.1 | 66.8±15.9 |
| (33–91) | (33–94) | (33–94) | |
| Gender, male : female | 2 : 9 | 7 : 25 | 9 : 34 |
| Weight (kg) | 67.5±15.7 | 58.0±15.4 | 60.47±15.9 |
| Body mass index (kg/m2), mean±SD | 26.8±6.3 | 24.5±4.7 | 25.1±5.1 |
| Body mass index ≧25 kg/m2 | 6 | 13 | |
| Creatinine clearance (mL/min), mean±SD | 97.3±41.5 | 83.3±53.2 | 87.1±50.2 |
| Currently smoking | 1 | 3 | 4 |
| Hypertension | 8 | 19 | 27 |
| Hyperlipidemia | 2 | 3 | 5 |
| Diabetes mellitus | 2 | 1 | 3 |
| On medication | 0 | Sleep inducing agent 5 | |
| Steroid 2 | |||
| Estrogen preparation 1 | |||
| Cancer chemotherapy 1 | |||
| Sleeping space | |||
| In car | 9 | 9 | 18 |
| Evacuation center | 2 | 12 | 14 |
| Own home or relatives’ home | 0 | 11 | 11 |
| Symptom | |||
| Chest symptom (dyspnea, chest pain etc.) | 8 | 0 | 8 |
| Limb symptom (swelling, pain etc.) | 10 | 26 | 36 |
| Complications | Head trauma 1 | Thrombophlebitis 1 | |
| Cerebellar infarction 1 |
PTE: pulmonary thromboembolism; DVT: deep vein thrombosis; SD: standard deviation
Test results
Among the 43 patients in the present study, 2 were excluded because lower limb symptoms in PTE were absent, lower limb US was not performed, and lower limb thrombi were not clearly confirmed on contrast CT. Therefore, 51 limbs in 41 patients with confirmed thrombi in the deep veins of the lower limbs were included. The location of the confirmed lower limb deep vein thrombi was the left lower limb only in 18 patients, the right lower limb only in 13 patients, and both lower limbs in 10 patients. The location of the thrombi was the crus in 46 limbs, including the soleal vein in 37 limbs, the anterior tibial vein in 3 limbs, the posterior tibial vein in 2 limbs, the fibular vein in 4 limbs, the popliteal vein in 2 limbs, and the femoral vein in 3 limbs. No patient had confirmed thrombi in the deep veins of the pelvis (Table 2). Among the 39 limbs with thrombi properties confirmed by US, 17 limbs were diagnosed with acute thrombi because of venous dilatation at the location of thrombi with low brightness or due to free-floating thrombi, 20 with subacute thrombi because of uneven echogenicity at a site of revascularization, and 2 with chronic thrombi because of predominantly high brightness and organic changes. All patients with PTE underwent image evaluation by contrast CT. Clinical severity was classified2) as non-massive in 5 patents and sub-massive in 6 patients. D-dimer levels were measured at the time of PE at our hospital in 9 patients with PTE and 25 patients with DVT. High D-dimer levels were found in both groups: 8.3±6.4 (1.6–20.8) µg/mL in the patients with PTE and 2.5±2.6 (0.5–9.1) µg/mL in the patients with DVT.
Table 2 Location of thrombi in PTE and DVT patients.
| PTE (11 legs) | DVT (40 legs) | Total (51 legs) | |
|---|---|---|---|
| Pelvic vein | 0 | 0 | 0 |
| Femoral vein | 1 | 2 | 3 |
| Popliteal vein | 1 | 1 | 2 |
| Calf vein | |||
| soleal vein | 7 | 30 | 37 |
| anterior tibial vein | 1 | 2 | 3 |
| posterior tibial vein | 1 | 1 | 2 |
| peroneal vein | 0 | 4 | 4 |
PTE: pulmonary thromboembolism; DVT: deep vein thrombosis
Treatment
PTE was treated on an inpatient basis for 9 patients, excluding 2 patients who did not wish to be hospitalized and had no chest symptoms with good oxygenation. The length of hospital stay was 7.8±6.2 (3–23) days. In 1 patient, an inferior vena cava (IVC) filter was placed, and all patients received anticoagulant therapy without thrombolytic therapy. DVT was treated on an outpatient basis only for all 32 patients, and 27 patients received anticoagulant therapy (Table 3). In all 5 patients who did not receive anticoagulant therapy, the DVT was limited to the crus. The main reason for not selecting anticoagulant therapy was that the lower limb symptoms were mild and the patient had already changed or planned to change their place of sleeping from their car to a home or shelter. Furthermore, some patients had a history of subarachnoid hemorrhage, which made them poor candidates for anticoagulant therapy.
Table 3 Selection of anticoagulant therapy.
| PTE (n=11) | DVT (n=32) | Total (n=43) | |
|---|---|---|---|
| Hospitalization | 9 | 0 | 9 |
| Duration of hospitalization in days, mean±SD | 7.8±6.2 (3–23) | — | — |
| IVC filter placement | 1 | 0 | 1 |
| Thrombolysis | 0 | 0 | 0 |
| Anticoagulation | |||
| Edoxaban | 7 | 19 | 26 |
| Rivaroxaban | 2 | 5 | 7 |
| Apixaban | 0 | 1 | 1 |
| Warfarin | 2 | 2 | 4 |
| None | 0 | 5 | 5 |
PTE: pulmonary thromboembolism; DVT: deep vein thrombosis; IVC: inferior vena cava
Among the 38 patients who received anticoagulant therapy for VTE, edoxaban was administered in 26 patients, rivaroxaban in 7 patients, apixaban in 1 patient, and warfarin in 4 patients. Reasons for selecting warfarin rather than DOAC included impaired renal function, individual wishes based on the financial burden, and the possibility that rapid reversal would be needed because of concurrent head injury. Treatment was started with heparin and subsequently changed to oral treatment in 3 patients with PTE, including warfarin in 1 patient and DOAC in 2 patients. Furthermore, among 7 patients given rivaroxaban and 1 patient given apixaban, the stipulated initial introduction dose was administered at the time of commencing oral treatment in 3 patients. Among the other patients, 4 were commenced from a maintenance dose and 1 was commenced at one-half the maintenance dose. The reason for not administering the initial introduction dose or administering a reduced dose was mild renal function impairment, mild clinical symptoms, and hypertension concurrent with cerebral aneurysm.
The patient in whom the IVC filter was placed included a 35-year-old man presenting acute-to-subacute thrombus below the superficial femoral vein and PTE in the left and right pulmonary arteries. He experienced pain in the left gastrocnemius area while sleeping in his car for 1 week, and, despite temporary remission of symptoms, approximately 2 weeks later, swelling and pain recurred in the left crus; thus, the patient presented at our hospital. There was no respiratory discomfort or clear right cardiac loading on echocardiography; however, considering relapse or progression of DVT, an IVC filter was indicated. With oral edoxaban, a retrievable Gunther Tulip filter was placed. Examination at 1 month after the onset revealed that the PTE had disappeared; however, DVT below the superficial femoral vein persisted, and the filter had not been retrieved at the time of examination to determine prognosis.
Post-diagnosis progress
Examinations to determine prognosis were performed at 4 months after the earthquake struck. Other than the 10 patients being treated on an outpatient basis at our hospital, 33 patients were surveyed via telephone for symptoms, treatment duration, and the presence or absence of hemorrhage events. During the follow-up period, there were no PTE complications or deaths, no DVT exacerbation, no cases of recurrence, and no exacerbation of lower limbs symptoms suggestive of recurrence. At post-treatment evaluation, 19 limbs in 14 patients underwent lower limb US at our hospital or a different hospital at 1 month or more after onset. The results revealed thrombus disappearance in 15 limbs and thrombus size reduction in 4 limbs. There were no patients in whom the thrombus was unchanged or exacerbated.
Among the 38 patients who underwent anticoagulant therapy (11 patients with PTE and 27 patients with DVT), at the interview 4 months after the earthquake, 12 patients (5 with PTE and 7 with DVT) were continuing treatment. The continued treatment duration was 95.0±17.2 days among the patients with PTE, 57.1±36.5 days among the patients with DVT, and 70.9±35.3 days among the patients with both. During treatment, 1 patient developed a rash on the thigh 2 months after commencing edoxaban, which disappeared after discontinuing the drug. In addition, there were no hemorrhagic events observed (Table 4).
Table 4 Outcomes of VTE patients on anticoagulant therapy at 4 months after first-earthquake.
| PTE (n=11) | DVT (n=27) | Total (n=38) | |
|---|---|---|---|
| Duration of treatment in days, mean±SD | 95.0±17.2 | 57.1±36.5 | 70.9±35.3 |
| Number of patients continuing therapy | 5 | 7 | 12 |
| Adverse event | |||
| Any event emerging during treatment | 0 | 1 (Skin eruption) | 1 |
| Bleeding during treatment | 0 | 0 | 0 |
PTE: pulmonary thromboembolism; DVT: deep vein thrombosis; SD: standard deviation
Discussion
The medical care system for VTE at the time of a disaster
Specific problems in providing medical care at the time of a disaster include unstable conditions, such as aftershocks or secondary disasters that may occur. This instability makes the degree of care that medical institutions can provide unclear. Because of the living space and the lifeline recovery situation, the possibility of accessing medical institutions differs for each patient, and a standard policy cannot be adopted.
In this study, a uniquely created flow chart was used, and we found that major factors having allowed us to provide the medical care for VTE included: the staff, electricity, and testing equipment required to maintain hospital functioning were available in normal working condition; cooperation was achieved by having day shift ultrasound technicians stationed at the emergency outpatient services dispatched from the neighboring healthcare center; and the hospital had a certain amount of medical supplies, such as anticoagulants and compression stockings, in stock, thereby enabling us to provide medical care even before restocking could be done with outside departments. Immediately after the disaster and at night when a large number of patients were being treated by a limited number of staff members, it was considered difficult to perform lower limb US for all patients with suspected DVT. Therefore, in the event of suspected DVT with edema and swelling of the lower limbs, D-dimer levels were measured. If the results were negative, DVT was ruled out, but if the results were positive, lower limb US was generally performed. To avoid false negative D-dimer results, D-dimer was considered negative if the levels were strictly <0.5 µg/mL, which was lower than the in-hospital reference value of 1.0 µg/mL.
In fact, upon performing lower limb US in patients with D-dimer levels of 0.5–1.0 µg/mL, 10 patients were positive for DVT. Overall progress of patients with VTE, including these patients, following the earthquake was good; no patients experienced exacerbation of VTE or bleeding events, irrespective of the presence or absence of anticoagulant therapy.
For VTE treatment at our hospital after the Kumamoto Earthquake, despite changing the medical care system to maintain staff from the disaster and in accordance with the state of testing that could be performed, we believe that there was no major hindrance to physical examination and testing; therefore, accurate diagnosis could be made and the treatment was provided safely and effectively.
Anticoagulant therapy for DVT
With regards to the dose level and administration method of anticoagulants, treatment for DVT was usually selected according to the severity in distal type below the knee and proximal type for more central veins, including the popliteal vein. In the event of proximal type DVT, anticoagulant therapy was administered as per PTE. In the event of distal type DVT, if symptoms were mild and there were no acute or free-floating thrombi on US, anticoagulant therapy is not necessarily selected. In some instances, however, it was unclear how long the patient would be living as a refugee and whether blood sampling and lower limb US for follow-up observation could proceed as planned. In general, DOAC was administered rather than warfarin to treat DVT following the earthquake irrespective of whether a distal or proximal vein was affected. Oral edoxaban therapy was immediately commenced without initially selecting to bridge with heparin. Furthermore, rivaroxaban and apixaban were commenced from a maintenance dose, and the initial introduction dose was not selected for most cases. This was attributed to the fact that there was no consultation immediately after the appearance of swelling and pain of the lower limbs suggestive of thrombus formation, and it was believed to reflect the prescribing physicians’ concern that it would be difficult to perform close follow-up after the disaster. This addressed the concern about a hemorrhagic event, which is an adverse reaction. In the present study, 4 patients were administered oral warfarin, among whom 3 were patients with DVT of the crus. In these patients, in-hospital follow-up observation was considered unnecessary and combination heparin was not administered as outpatient treatment. In patients administered warfarin alone, there were no cases of DVT exacerbation; however, warfarin reportedly takes time to express its anticoagulation effect and, soon after administration, the short half-life can cause a state of hypercoagulability to potentially occur due to protein C reduction.5) It is believed that careful follow-up observation is particularly needed soon after treatment commencement to verify DVT exacerbation.
The duration of anticoagulant therapy for VTE
Three months after onset is considered as the ideal duration of anticoagulant therapy for VTE, except in the event of thrombus-related factors, malignant tumor, and motor impairment such as paralysis.2) Of course, depending on the individual patient, anticoagulant therapy in some instances is prolonged or administered permanently according to the presence or absence of lower limb congestive symptoms, surgery, trauma, or elimination of the risk of reversible thrombus formation, such as in pregnancy; the presence or absence of an IVC filter; and the state of venous thrombosis on US. According to the Japan VTE Treatment Registry (JAVA) reported in 2013, the mean duration of anticoagulant therapy for VTE is 7 months.6)
In the present study, the observation period of 4 months after the earthquake was short; however, in many patients, including those who did not receive anticoagulant therapy or who had already completed treatment, subjective symptoms improved and there were no patients with clear VTE recurrence or exacerbation. Furthermore, the thrombus had disappeared or reduced in size in patients with DVT thrombi confirmed on lower limb US performed later after receiving anticoagulant therapy. In VTE following an earthquake, it is believed that individuals who would not normally develop VTE (considering daily activity and healthy lifestyle) also develop VTE as a result of the difficult conditions caused by the earthquake, such as living in a shelter, sleeping in one’s car, or unable to drink sufficient water. Therefore, if food, clothing, and shelter are provided, the risk of thrombus formation is reduced when the patient returns to daily life. We believe that without temporary anticoagulant therapy, thrombi will spontaneously disappear and symptoms will improve. Therefore, the duration of anticoagulant therapy for VTE following an earthquake is roughly aimed at 3 months in patients who return to normal daily life and the reversible risk is judged to have been eliminated. However, at the time of a disaster, although many people face the same situation, only some develop VTE. For individuals who develop VTE, lower limb exercise and fluid intake should be strictly enforced. Furthermore, considering that some individuals may have risk factors of congenital thrombosis and potentially a malignant tumor or heart failure that has not been identified, examination for the presence or absence of an underlying cause of VTE and informing the individual concerned or family doctor is important for long-term prognosis.
At the point in time of the prognostic survey at 4 months after the earthquake, 12 of the 38 patients who commenced anticoagulant therapy for VTE were continuing the treatment. As the reason for continuing anticoagulants, some patients indicated that treatment discontinuation was scheduled to be at 6 months after the start of treatment, that the duration was determined as the period until IVC filter removal, and that permanent treatment was confirmed due to the onset of DVT and stroke coexistent with interatrial septum defect. However, in three patients, there was no specified time of anticoagulant therapy completion on the medical chart at our hospital or the referral form to the referral destination, and the patients did not know the discontinuation time. At the time of conducting a telephone survey, we urged such patients to verify the intentions of their current attending physician and recommended consulting our hospital for follow-up observation including US. In the event of requesting a different hospital to continue treatment, the timing of future evaluations and the timing of treatment discontinuation should be clearly presented.
Conclusion
At 2 months after the Kumamoto Earthquake, treatment was administered in 11 patients for PTE and in 32 patients for DVT. Follow-up observation at 4 months after the earthquake revealed no recurrence or exacerbation of PTE or DVT. Anticoagulant therapy was administered to 38 patients, and DOAC was administered to 34 patients as the first choice of treatment. No hemorrhagic event was observed. For VTE occurring because of a difficult environment following a disaster, such as living in a shelter and sleeping in one’s car, DOAC-based treatment is safe and useful.
Disclosure Statement
There are no companies with conflicts of interest that should be disclosed with regards to the present paper.
Additional Remarks
There are no companies with conflicts of interest that should be disclosed with regards to the present paper.
References
- 1).JCS, JSH and JCC Joint Working Group. Guidelines for disaster medicine for patients with cardiovascular diseases (JCS2014/JSH2014/JCC2014). Circ J 2016; 80: 261-84. [DOI] [PubMed] [Google Scholar]
- 2).JCS Joint Working Group. Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J 2011; 75: 1258-81. [DOI] [PubMed] [Google Scholar]
- 3).Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149: 315-52. [DOI] [PubMed] [Google Scholar]
- 4).JASSO. The goals of Guidelines for the Management of Obesity Disease 2016. In: Guidelines for the Management of Obesity Disease. Tokyo: Life Science Publishing, 2016: 1-3. (in Japanese)
- 5).Freedman MD. Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects. J Clin Pharmacol 1992; 32: 196-209. [DOI] [PubMed] [Google Scholar]
- 6).Nakamura M, Miyata T, Ozeki Y, et al. Current venous thromboembolism management and outcomes in Japan: nationwide the Japan Venous Thromboembolism Treatment Registry Observational Study. Circ J 2014; 78: 708-17. [DOI] [PubMed] [Google Scholar]