Abstract
Problem Considered:
Accessibility by telephone to cystic fibrosis (CF) centers for a sweat test appointment from a parental perspective, which can be stressful, compared to experience in contacting a general pediatrics practice in the same area.
Methods:
We called each CF center and affiliate twice and a sample of multi-physician general pediatrics practices selected from yellowpages.com after being matched by area and zip codes to 50 randomly selected CF centers, including Wisconsin’s two nationally accredited centers. After national alerts to CF centers, we made follow-up calls to randomly selected centers. A call was considered successful if time and date of the next available sweat test or well-baby check-up appointment was provided.
Results:
In contrast to calls made to general pediatricians’ offices, in which 98% were successful and an appointment available in an average of 8.6 days, only 31% of CF centers and affiliates could be successfully contacted. Although a sweat test appointment was available in 4.9 days on average, delays as long as 26 days were possible. In the subsequent follow-up calls, only 40% were successful.
Conclusions:
Substantial difficulties and inconsistencies were encountered in accessing CF centers, suggesting that parents may often be challenged in their efforts, while they generally have no difficulty contacting and scheduling an appointment with a general pediatrician. This contrasting experience could be stressful to parents when their baby has a positive screening test. The role of primary care physicians in newborn screening communications is increasingly important while the role of regional centers needs reconsideration.
Keywords: Cystic fibrosis, accessibility, primary care, newborn screening
INTRODUCTION
Cystic Fibrosis (CF), the most common, life-threatening genetic disease in the Caucasian population (1), is difficult to diagnose and treat effectively without newborn screening (NBS) (2). After evidence of screening benefits was published (3), including an influential article in the Wisconsin Medical Journal (4), and the Centers for Disease Control and Prevention (CDC) recommended this diagnostic strategy (5), a proliferation of CF NBS programs occurred rapidly and by 2010 the entire U.S. was screening. It was anticipated by the CDC (5) and CF Foundation (6) that the network of accredited CF centers would facilitate the nationwide implementation of CF NBS programs in partnership with primary care physicians, particularly the follow-up communications and care (6). Recently published guidelines (7) emphasize the importance of this partnership and excellent, timely communications. On the other hand, previous studies (8) revealed that regional newborn screening programs vary widely in their approaches to communications with parents. In addition, parents have expressed concerns regarding access to a diagnostic sweat test appointment for their newborn infant (9). Data indicate that a delay in access can result in psychosocial stress and also has potential adverse consequences for the health of the infant (10,11). Indeed, it has been observed that “most parents of infants with abnormal NBS results for CF experience a significant amount of distress during their wait for the final diagnostic results” (9,12).
Although access to care by parents for potentially ill infants is obviously crucial, studies are very limited, especially attempts to determine accessibility through telephone calls. No such study could be found in PubMed search or from the American Academy of Pediatrics. Thus, an innovative objective of this project was to design a telephone accessibility study and determine from a parental perspective the accessibility of CF centers compared with nearby general pediatrics practices. The research question, therefore, was how responsive are regional CF centers in the U.S. to parental inquiry about resources for their infant compared to pediatrician practices. Apparently, this is the first time either clinical setting has been so evaluated nationally, although the topic is considered important (13).
METHODS
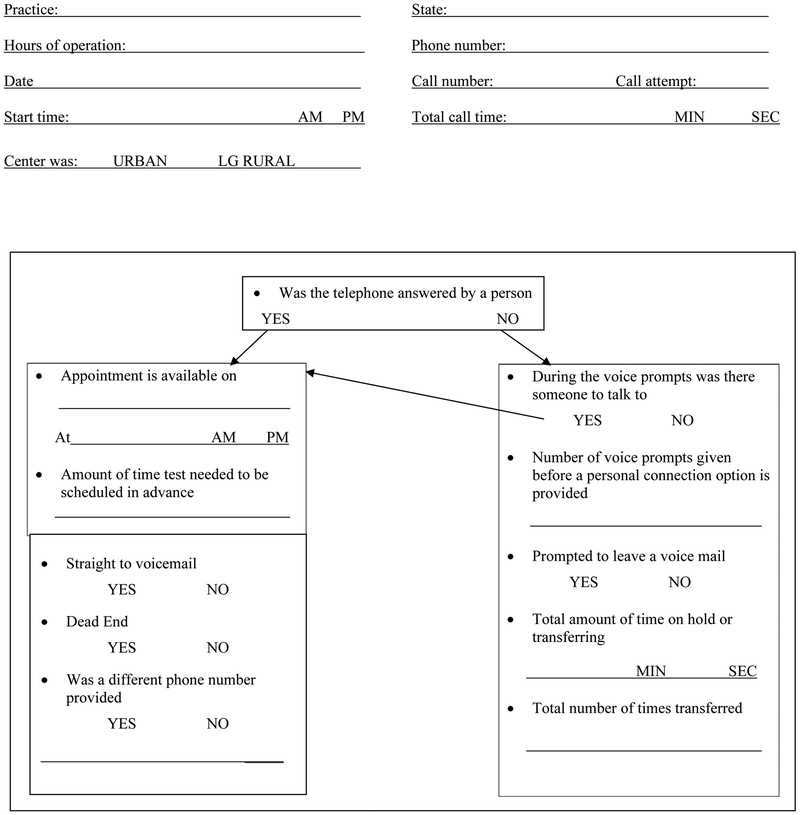
As shown in Figure 1, an original telephone survey from a parents’ perspective on access was designed and conducted with a script as we attempted to communicate with CF centers/affiliates and then obtain similar data from “matched” general pediatrics practices. The contact information on the 160 certified centers and affiliates was obtained from the CF Foundation for all states and D.C.
Figure 1. Data Collection Tool for Telephone Survey on Accessibility.
Basic data collected and recorded for each call included the provider’s name, U.S. state of operation, hours of operation, telephone number, telephone call start and end time, total telephone call time, date of telephone call, urban or large rural status, and the call round. During the telephone call the following additional information was recorded: if the telephone was answered by a person, language options, if we were prompted to leave a voice mail, if the telephone call went straight to voicemail, the telephone number if an alternative telephone number was provided, if there was someone to talk to during the voice prompts, if new patients were being accepted, if and when (date and time) an appointment was available for a ST or well baby visit, the amount of time needed to schedule the ST and if the telephone call ended in a “dead end” (defined as a call that: went straight to voicemail, was on hold for more than 10 minutes at one time, was the wrong telephone number, rang for more than 90 seconds without an answer, went to the wrong department within a CF center and could not provide a telephone number or transfer to the correct department, had no proper option in the voice prompts listed at a CF center or affiliate or ended in a technical or personnel problem). Additional data included the number of voice prompts before a personal connection option is given, total number of voice prompts, total number of times transferred and total amount of time on hold or transferring.
Recognizing that parents would be accustomed to calling primary care physician offices, we carefully selected for comparison during 2012 a total of 50 multi-physician general pediatrics practices using yellowpages.com to identify area and zip code groups matched to a 33% random sample of the CF centers. By chance, both of Wisconsin’s CF Foundation accredited centers in Madison and Milwaukee were included in the random sample. University and children’s hospital practices were excluded in the selection of general pediatricians to ensure that the provider was a distinct, private practice. For Madison and Milwaukee, the immediate, contiguous suburban pediatric practices were eligible for the matching process. When more than one general pediatrics practice was found nearby, the first on the list was selected. Multi-physician general pediatric practices were called once and asked if they were accepting new patients and when the first well baby check-up appointment was available. The call started with “I’m calling for my daughter who recently had a baby and may be moving into your area.”
Each CF center or affiliate in the CFF directory was categorized as urban or rural (by zip code), and by size based on the number of patients under the age of 18; they were then categorized as defined by the CF Foundation into large (>65 patients), medium (41–65), small (20–40), or very small (<20). All telephone calls followed the script and were monitored for time using two Sportline 240 stopwatches (one used for hold time and other for total call time.) Telephone numbers for the first round of calls were from the CF Foundation Directory. After identifying many errors, we utilized telephone numbers for the second round of calls from the online directory of the CF Foundation website (www.cff.org/aboutCFFoundation/Locations/FindAChapter/). Avoiding holiday weeks such as Thanksgiving, we made two calls to each CF center during their normal business hours, which were obtained by calling in the evening and obtaining the information from recordings. Additional follow-up calls were conducted about one year after this study’s initial results were shared with the CF Foundation Centers Committee and pediatric CF centers at large --- leading to recommendations/efforts to improve telephone accessibility. Some methods employed were: 1) change in voice prompts; 2) referral of callers to the affiliated children’s hospital; 3) more frequent sweat test appointments; and 4) directly answering the phone, i.e., reverting to their original telephone communication method. Our repeat assessment method included alphabetizing the list of centers accredited by the CF Foundation and selecting a randomized subset of half of the CF centers that were not successful in the initial calls (N = 42). Then, during 2015–16, a third set of calls were made for additional assessment using an updated resource from the CFF website (www.cff.org/aboutCFFoundation/Locations/FindACareCenter/).
The main outcome variable was to ascertain the earliest time and date that an appointment could be scheduled. Basic data collected and recorded for each call included the responses, response times, transfers and appointment availability. Additional data included the number of voice prompts before a personal connection option is given, total number of voice prompts, total number of times transferred and total amount of time on hold or transferring. Call outcomes resulted in three categories: successful, partially successful and unsuccessful. A call was deemed successful when both a time and date for the next available appointment were readily available, partially successful if a ST date and time were provided during only one of the two telephone calls, and unsuccessful if a time/date was not obtained.
Our Institutional Review Board determined this study qualified for exemption under category 45 CFR 46.101(b) (2) and did not require informed consent. Members of the IRB contributed to the design and script.
RESULTS
Our primary objective of this survey was accomplished, namely to determine the accessibility by telephone of an appointment for a newborn infant. As shown in Table 1, we found that only 31% (49/160) of the CF centers and affiliates were successful on both rounds of calls, while 34% (55/160) of the CF centers and affiliates were categorized as completely unsuccessful. Although there were a variety of reasons for a lack of success, the most common explanation was an unanswered call. We found that 54% of calls with a “dead end” outcome resulted from the telephone call going straight to voicemail or ending in voicemail. We also found that on the average when the telephone was answered by a CF center/affiliate, there were an average of 3.8 voice prompts or messages. In contrast, 98% of the calls to general pediatricians’ offices were successful and transfer to voicemail occurred only once (Table 2). On average, calls were answered by a person in 22 seconds and appointments made in 8.6 days within 2 minutes and 4 seconds. Eleven of the 50 multi-physician general pediatric providers had one voice prompt and the remaining had zero. Because of the successful matching and very high success rate, we did not repeat these calls or expand the sample.
Table 1:
Provider Characteristicsa by Mean Outcome [Number (PERCENT)]
| Provider Access to Care Outcomes | ||||
|---|---|---|---|---|
| Successfulb | Partially Successful | Unsuccessful | ||
| Designation | Centers (110) | 33 (30) | 42 (38) | 35 (32) |
| Affiliates (50) | 16 (32) | 14 (28) | 20(40) | |
| Centers + Affiliates (160) | 49 (31) | 56 (35) | 55 (34) | |
| Location | Urban (156) | 45 (29) | 56 (36) | 55 (35) |
| Large Rural (4) | 4 (100) | 0 (0) | 0 (0) | |
| Size | Large, >65 patients (87) | 29 (33) | 28 (32) | 30 (35) |
| Medium, 41–65 patients (32) | 11 (34) | 13 (41) | 8 (25) | |
| Small, 20–40 patients (28) | 4 (14) | 11 (39) | 13 (47) | |
| Very small, <20 patients (13) | 5 (38) | 4 (31) | 4 (31) | |
Per CF Foundation definitions
All percentages were calculated across rows and within each characteristic.
Table 2:
Comparisons of CF Provider and General Pediatrics Practice Telephone Call Outcomes [NUMBER (PERCENT)]
| CF Centers | CF Affiliates | Pediatric Practices | |
|---|---|---|---|
| Successfully provided time and date of next appointment [number (percent)] | 33 (30) | 16 (32) | 49 (98) |
| Answered by a persona [number (percent)] |
33.5 (30) | 19.5 (39) | 37 (74) |
| Mean total call time (sec) | 172 | 145 | 124 |
| Range of mean total call time (sec) | 38 – 527 | 18 – 699 | 48 – 551 |
| Mean hold time (sec) | 119 | 97 | 144 |
| Range of mean hold time (sec) | 0 – 449 | 4 – 640 | 27 – 520 |
| Mean time to first appointment (days) | 5 | 5 | 8.6 |
| Range of mean time to first appointment (days) | 1 – 18 | 1 – 26 | 1 – 49 |
The number of providers who are included in this analysis are the summed average of all calls that had call time.
When a call to a CF center/affiliate was successful, the average total time spent on the telephone was 158 seconds and the time on hold was 106 seconds. Similar results were found with the general pediatrics practices, i.e., 124 and 144 seconds. Table 1 also lists some characteristics for the CF centers and affiliates. These results revealed that there were no significant difference between the centers/affiliates in terms of success rate. CF centers and affiliates were also analyzed by the number of patients under the age of 18 at their facility. In this analysis, the data suggest that the small CF centers/affiliates caring for 20 to 40 patients might be less accessible than the others. The data by geographical for location were also analyzed and revealed no regional trends (data not shown). From the subset list of 42 CF centers called in the follow-up calls, we found that only 40% were successful in being able to reach the CF scheduler/coordinator and being provided both the date and time of next available ST. Thus, there was no significant improvement compared with our initial experiences. Similar results were found on the third set of calls to CF centers.
The Wisconsin results were typical of our national findings. Specifically, the first call to one center was partially successful while the other was unsuccessful. However, on the second call, neither was successful but led to dead end outcomes as described in the figure legend. On the other hand, the calls to the matched general pediatricians’ offices were all successful.
DISCUSSION
Limited research has been done on timely communications and accessibility for newborns in pediatric practices. We designed/performed an innovative, telephone-based study and found that CF centers have poor access while nearby general pediatric practices were almost invariably accessible. Two widely accepted definitions of access to care include: the Institute of Medicine’s, namely “the timely use of personal health services to achieve the best health outcomes” (14), and the Agency for Healthcare Research and Quality’s statement: “assessments by patients of how easily they are able to gain access to health care” (15). Because parents of newborn infants obviously need to contact physicians on an urgent basis for primary care and sometimes for subspecialist care, we designed this original study from a parental perspective to determine accessibility for either a well-baby visit or for follow-up of a positive NBS test. As emphasized in the pivotal CDC report recommending universal NBS, “The net balance of benefits and risks is contingent on how newborn screening for CF is implemented” (9). Because some of the risks are associated with delays occurring after a positive screening test, we assumed that an important element in the follow-up component would be access. If a delay in access occurs, parental psychological stress becomes an important concern whenever parents face a possible diagnosis of CF (9, 10, 16). Studies have revealed that “Most parents experienced strong emotional responses to the news of a positive IRT test, including anxiety, shock, denial and anger. Parents also reported heightened vigilance during the typical delay between being informed of a positive IRT results and diagnostic sweat test” (16). These negative experiences are part of the risks of NBS.
Because of such risks, it is important that parents have adequate access and are satisfied with their communications. However, in this study, we found that 34% of all CF centers and affiliates in the U.S. were completely inaccessible by telephone and that only 31% were accessible on both of our attempts. These results show that the majority of such centers cannot be readily contacted and suggest that parental accessibility is a barrier to care. The question can be raised if other kinds of specialty centers would be similarly difficult to contact, but this has not been studied. We considered this as an adjunct study but found that it was difficult to identify a high-performing pediatric specialty with regard to communication and moreover this ancillary study would be challenging to design without a published network of centers engaged in NBS. On the other hand, contacting general pediatricians’ offices nationwide for an appointment was found to be quick and generally successful with regard to an appointment soon after the call.
According to a Best Practices LLC (18), telephone call centers on average have a 4% call abandonment rate and rates that reach 10% or higher should be reviewed for quality improvement. Likewise, it was noted that the majority of benchmark companies improve their center processes based on customer needs (18). Consequently, the CF Foundation Centers Committee reviewed our results and the pediatric centers were notified about this issue and the need for better communication and quality improvement (19). Suggestions were made as described previously. The aim of our additional follow-up calls was to determine if these efforts had any impact. Because our data revealed that only 40% of re-assessed CF centers were accessible during their second round of calls, and indeed some were less accessible, it is clear further efforts are needed. Recognizing that this may be the case and its responsibility to provide parents with information on the screening and diagnosis of infants, as well as the nature of the disease, the CF Foundation has created the first parent website ever on NBS (http://www.cff.org/AboutCF/Testing/NewbornScreening/). Although its impact remains to be determined, the initial usage has been very impressive with an average of more than 1,955 and 2658 “hits” per month during 2011 and 2012, respectively. The website includes a section “For Health Care Providers” that has received 150–200 unique viewings per month (data provided by Leslie Hazle, RN, of the CF Foundation).
Studies show that “Convenient accessibility was the most important factor for the initial choice of primary care doctors by the general public” (20). Our innovative evaluation revealed that general pediatric practices do show “convenient accessibility” during random assessment nationwide. In view of the limited accessibility of the nation’s CF centers, however, it must be concluded that primary care providers, especially readily accessible general pediatricians, and informative websites can assume increasingly important roles in communication and facilitation of follow-up procedures after newborn screening and other genetic disorders.
CONCLUSIONS
Substantial difficulties and inconsistencies were encountered in parental access for scheduling a follow-up appointment with a CF center, indicating that parents may often be challenged in their efforts. On the other hand, we conclude that they generally have no difficulty contacting and scheduling an appointment with a general pediatric practice. This contrasting experience could be a source of stress to parents, especially when their baby has a positive NBS test (9). However, there are methods that CF centers could employ to improve their accessibility by telephone such as triaging calls to nurse specialists or responsive children’s hospitals. From a broader perspective, our results reinforce how responsive and helpful pediatricians and family physicians can be to their patients and families. In addition, this study complements our previous research and emphasizes the need for continued quality improvement in NBS. One aspect of this should be reconsideration of the role of regional centers in NBS follow-up activities if their accessibility is limited.
ACKNOWLEDGEMENTS
We thank Anita Laxova for her expert assistance in the organization of this study, especially with IRB communication, and Professor Patrick Remington for his guidance on aspects of evaluating heath care accessibility. We also appreciate the advice of the CFF, especially Dr. Bruce C. Marshall (Vice President of Clinical Affairs, US Cystic Fibrosis Foundation), and our communications with the American Academy of Pediatrics, especially Dr. V. Fan Tait (Associate Executive Director, Department of Community and Specialty Pediatrics) who recommended that we proceed with this unique study.
Disclosures: This research was supported in part through National Institutes of Health grant DK 34108 to Dr. Philip Farrell as Principal Investigator.
REFERENCES
- 1.Kosorok MR, Wei WH and Farrell PM. The incidence of cystic fibrosis. Statistics in Medicine 15:449–462, 1996 [DOI] [PubMed] [Google Scholar]
- 2.Balfour-Lynn I Newborn Screening for Cystic Fibrosis: Evidence for Benefit. Arch Dis Child. 2008;93: 7–10. [DOI] [PubMed] [Google Scholar]
- 3.Farrell P, Kosorok M, Rock M, et al. Early Diagnosis of Cystic Fibrosis Through Neonatal Screening Prevents Severe Malnutrition and Improves Long-Term Growth. Pediatrics. 2001;107:1–12. [DOI] [PubMed] [Google Scholar]
- 4.Farrell PM, Aronson RA, Hoffman G, Laessig RH. Newborn screening for cystic fibrosis in Wisconsin: first application of population-based molecular genetics testing. Wis Med J. 1994;93:415–21. [PubMed] [Google Scholar]
- 5.Grosse SD, Boyle CA, Botkin JR, et al. Newborn screening for cystic fibrosis: evaluation of benefits and risks and recommendations for state newborn screening programs. MMWR Recomm Rep. 2004;53(RR-13):1–36. [PubMed] [Google Scholar]
- 6.Campbell PW, White TB. Newborn screening for cystic fibrosis: an opportunity to improve care and outcomes. J Pediatr. 2005; 147:S2–5. [DOI] [PubMed] [Google Scholar]
- 7.Borowitz D, Robinson KA, Rosenfeld M, Davis SD, Sabadosa KA, Spear SL, Michel SH, Parad RB, White TB, Farrell PM, Marshall BC, Accurso FJ. Cystic fibrosis foundation evidence-based guidelines for management of infants with cystic fibrosis. J Pediatr. 2009, 155:S73–S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farrell MH, Certain LK, and Farrell PM. Genetic counseling and other risk communication services by newborn screening programs. Arch Pediatr Adol Med 2001; 155:120–126. [DOI] [PubMed] [Google Scholar]
- 9.Tluczek A, Koscik R, Farrell P, Rock M. Psychosocial risk associated with newborn screening for cystic fibrosis: parents’ experience while awaiting the sweat-test appointment. Pediatrics 2005;115:1692–1703. [DOI] [PubMed] [Google Scholar]
- 10.Sims EJ, Clark A, McCormick J, Mehta G, Connett G, Mehta A; United Kingdom Cystic Fibrosis Database Steering Committee. Cystic fibrosis diagnosed after 2 months of age leads to worse outcomes and requires more therapy. Pediatrics. 2007;119:19–28. [DOI] [PubMed] [Google Scholar]
- 11.Farrell PM. The meaning of “early” diagnosis in a new era of cystic fibrosis care. Pediatrics. 2007; 119: 156–7. [DOI] [PubMed] [Google Scholar]
- 12.Tluczek A, Mischler EH, Farrell PM, Fost N, Peterson NM, Carey P, et al. Parents’ knowledge of neonatal screening and response to false-positive cystic fibrosis testing. Journal of Developmental and Behavioral Pediatrics,1992;12, 181–6. [PubMed] [Google Scholar]
- 13.Feinberg R, Kim I, Leigh H. Operational determinants of caller satisfaction in the call center. Internat J Service Industry Management. 2000; 2:131–141. [Google Scholar]
- 14.Institute of Medicine, Committee on Monitoring Access to Personal Health Care Services. Access to health care in America. Millman M (Ed.).Washington, DC: National Academy Press; 1993. [Google Scholar]
- 15.Agency for Healthcare Research and Quality. US Department of Health and Human Service. Accessed on November 14, 2009 from: < http://www.ahrq.gov/>
- 16.Tluczek A, Koscik RL, Modaff P, Pfeil D, Rock MJ, Farrell PM. Newborn screening for cystic fibrosis: Parents’ preferences regarding counseling at the time of infants’ sweat test. J Genet Couns. 2006;15:277–291. [DOI] [PubMed] [Google Scholar]
- 17.Baroni M, Anderson Y, Mischler E. Cystic fibrosis newborn screening: impact of early screening results on parenting stress. Pediatr Nursing.1997;23:143. [PubMed] [Google Scholar]
- 18.Best Practices LLC. Managing World-Class Call Centers: Site Visit Findings. Best Practices, LLC Benchmark Report. 2004. [Google Scholar]
- 19.McPhail GL, Weiland J, Acton JD, Ednick M, Chima A, VanDyke R, Fenchel MC, Amin RS, Seid M. Improving evidence-based care in cystic fibrosis through quality improvement. Arch Pediatr Adolesc Med. 2011;164(10):957–60. [DOI] [PubMed] [Google Scholar]
- 20.Wun YT, Lam TP, Lam KF, Goldberg D, Li DK, Yip KC. How do patients choose their doctors for primary care in a free market? J Eval Clin Pract. 2010;16:1215–20. [DOI] [PubMed] [Google Scholar]