Abstract
Background
China has ambitious to achieve significant reductions in HIV transmission and HIV-related mortality by adopting the World Health Organization's “Treat All” approach. Such a prevention strategy is needed future study on regional scale.
Methods
An observational cohort study of HIV epidemiology and treatment databases was used to study the effectiveness of antiretroviral therapy on the transmission of HIV in serodiscordant couples in Guangxi of China.
Results
A total of 7713 couples were entered into the cohort study analysis which included 1885 couples in the treatment-naive cohort and 5828 couples in the treated cohort. During the follow-up of 18985.29 person-years from 2003 to 2014, the average incidence of HIV was 2.4 per 100 person-years (95% CI 2.1–2.6). HIV seroincidence rate was significantly higher among the treatment naive group (4.2 per 100 person-years, 3.7–4.8) compared with the on treatment group (1.6 per 100 person-years, 1.3–1.8). An overall 45% reduction in risk of HIV transmission among serodiscordant couple was associated with ART treatment (adjusted Hazard Ratio [HR] 0.55, 95% Confidence Interval [CI] 0.44–0.69). Treatment prevention had significantly effectiveness for most baseline characteristics of index partners, such as for male, female, age above 25 years, education below high school, farmer, infected by heterosexual intercourse.
Conclusion
Treatment-as-prevention can be implemented in the real-world on a national or regional scale, but ART adherence and comprehensive harm reduction while implementing this strategy require further study.
Keywords: HIV, ART, Sero-discordant couples, Transmission, Cohort study
Abbreviations: HIV, human immunodeficiency virus; AIDS, acquired immune deficiency syndrome; ART, antiretroviral therapy; CI, confidence interval; HR, hazard ratio; IDUs, injection drug users; MSM, men who have sex with men; CDC, center for disease control and prevention
1. Introduction
Since the first case was discovered in the mainland China in 1985, the HIV epidemic in the country has experienced a small and low expanding phase in the 1980s to several regional epidemics in the 1990s of injection drug users (IDUs) in the south western border regions (Qian, Vermund, & Wang, 2005). In addition, unregulated commercial blood/plasma collection among farmers occurred between 1992 and 1995 in several provinces in central China, including Henan, Anhui and Shanxi provinces, and caused a second important endemic in China (Shan et al., 2002; Yan et al., 2000). Although this was banned by Chinese government at the end of 1995, the practice of using contaminated blood collection equipment or re-infusing pooled buffy coats back to donors caused thousands of HIV infection among paid commercial blood donors in rural areas of those provinces (Shan et al., 2002; L.; Wang, Zheng, Qian, Lu, & Xing, 2005; Yan et al., 2000). Since 2006, HIV infection caused by heterosexual contact has become the main mode of HIV transmission taking over drug injection in China (Chinese Center for Disease Control and Prevention, China, 2006). Meanwhile, HIV transmission in men who have sex with men (MSM) is increasing at an alarming speed. The proportion of reported HIV/AIDS cases among MSM increased from 3.5% in 2007 to 28.3% in 2015 in China (Chinese Center for Disease Control and Prevention, China, 2007; Chinese Center for Disease Control and Prevention, China, 2015). China is no exception to the evolution of the HIV epidemic happening in other Asian countries, starting from a drug-driven epidemic and shifting to mainly sexual transmission (Qian et al., 2005).
Illicit drugs reemerged in China in the 1980s due to China adopted an open-door economic policy which was associated with global drug trafficking activities (Zhang & Ma, 2002). As the Southwest China is close proximity to the world's major heroin producing area known as the Golden Triangle, the major drug of heroin in the Chinese market is brought from Myanmar into Yunnan and then to Guangxi or from Viet Nam into Guangxi, and the drug trafficking routes were to Sichuan, Guizhou and Xinjiang and another to other provinces (National Narcotics Control Commission, China, 2002). Recently, the proportion of heroin which is trafficked from the “Golden Crescent” to Xinjiang was rapid increased, and them into other neighbor areas. The first HIV case in Chinese IDU was reported in the Southwestern province of Yunnan along the border with Myanmar in 1989 (Ma, Li, & Zhao, 1990). After that, HIV transmission among drug users has increased rapidly. HIV prevalence among IDU has exceeded 20% in the Southwestern and Western provinces, such as Yunnan, Guangxi, Sichuan and Xinjiang (Ruan et al., 2005, 2013; Wei et al., 2006; Yin et al., 2007; Zhang et al., 2007; Zheng et al., 1994, 1995). Due to a free market economy, rapid social development, large income disparities and changing notions of sexuality, commercial sex activities have flourished across the country. Skyrocketing STD epidemic has been becoming an important public health problem in China. Heterosexual transmission of HIV through female sex workers (FSWs) is of particular concern (Qian et al., 2005). Since the 2000s, HIV prevalence among FSWs has remained relatively low and stable, ranging from 0.0% to 10.3% (median, 0.6%), however higher prevalence in several areas of Yunnan and Guangxi (Poon, Li, Wang, & Hong, 2011). Because sexual intercourse is the mode of transmission bridging the HIV infection from high risk groups to the general population, the HIV epidemic in China has entered a new ear. These new changes pose greater challenges than ever before to China's AIDS control efforts. In response to the growing burden of HIV, China's government has implemented National AIDS Control Policy has been the “Four Frees and One Care” program since 2003 (Han et al., 2010). As part of this policy initiative, comprehensive harm reduction programs such as knowledge education, HIV testing and counselling, condom promotion, methadone maintenance therapy and needle exchange were rapidly scaled-up and implemented in 2004 (Han et al., 2010; Liu, Sullivan, & Wu, 2007; Qian et al., 2008; Rou, Sullivan, Liu, & Wu, 2010; Ruan et al., 2013; Yin et al., 2010; L.; Zhang et al., 2014). Today, China has ambitious to achieve significant reductions in HIV transmission and HIV-related mortality by adopting the World Health Organization's 90–90–90 policy.
Guangxi Zhuang Autonomous Region is located on the southwestern of China. Due to its location along the major drug trafficking route linking Guangxi to Yunnan and Vietnam, the HIV transmission has been fueled mainly by IDU. The first HIV infection among local IDUs was reported in 1996 in Guangxi. Since then, the epidemic had rapidly spread among drug users. However, starting from 2006, the transmission mode has been shifted to heterosexual contacts (Chinese Center for Disease Control and Prevention, China, 2006). In 2015, 93% of reported HIV cases in Guangxi were infected through heterosexual intercourse. Among the 31 provinces and municipalities in China, Guangxi reported the largest number of HIV cases. Of the total number of reported HIV cases in China, about 10% was reported from Guangxi (Chinese Center for Disease Control and Prevention, China, 2017). The aim of our study was to use observational cohort study of HIV epidemiology and treatment databases to study the effectiveness of antiretroviral therapy on the transmission of HIV in serodiscordant couples in Guangxi of China.
2. Methods
2.1. Study design and study population
This observational cohort study of serodiscordant couples was conducted in Guangxi from 2003 to 2014. Serodiscordant couples were defined as one participant was HIV positive (index patient), and their heterosexual regular partner was HIV negative at baseline who had at least one additional HIV test results at follow-up. Index patients were followed up every 6 months for care and clinical evaluation. The local CDC tested their spouse or regular sex partners for HIV every 6 months for partners who tested negative. Participants in the epidemiology database were linked to their own records in the treatment database by linkage of their unique treatment identification numbers or national identification numbers. Additional details about the cohort follow-up study have been previously published elsewhere (Jia et al., 2013; Ma et al., 2010; Zhang et al., 2008, 2011).
2.2. Data collection
According to their treatment status of the cohort study, the index patients could be classified into three groups: those never treated (group 1), those who entered untreated but subsequently began treatment during follow-up (group 2), and those treated immediately upon entry into the database (group 3). Baseline characteristics of all index patients included sex, age, education status, marital status, occupation, and transmission route. CD4 count at the baseline visit was extracted for those never treated in group 1 and before treatment in group 2, respectively. CD4 count at the visit before initializing treatment was extracted for those after treatment in group 2 and in group 3.
2.3. Laboratory testing
Blood samples were tested for HIV infection. HIV antibody was screened for each blood sample by enzyme-linked immunosorbent assay (Diagnostic Kit for Antibody to Human Immunodeficiency Virus, Beijing WANTAI Biological Pharmacy Enterprise Co.Ltd, China; and GenscreenTM ULTRA HIV Ag-Ab, Bio-Rad Laboratories, USA), and was confirmed by HIV Western Blot confirmation (MP Diagnostics HIV BLOT2.2, MP Biomedicals Asia Pacific Pte.Ltd).
2.4. Statistical analysis
The outcome of cohort study was time to HIV seroconversion. Univariate and multivariate extended Cox regression models with the time-varying covariate of treatment status were used to estimate the treatment hazard ratio (HRs; reported with 95% CIs). The following variables were included in the adjusted models for controlling bias: duration of follow-up, age, sex, education, marital status, occupation, transmission route, baseline CD4 cell count of the index patient and time of initial ART. A two-sided p-value of 0.05 or less was regarded as statistically significant. The data were analyzed using Statistical Analysis System (SAS 9.1 for Windows; SAS Institute Inc., NC, USA).
2.5. Ethics statement
This study was approved by the institutional review board of the Guangxi Center for Disease Control and Prevention.
3. Results
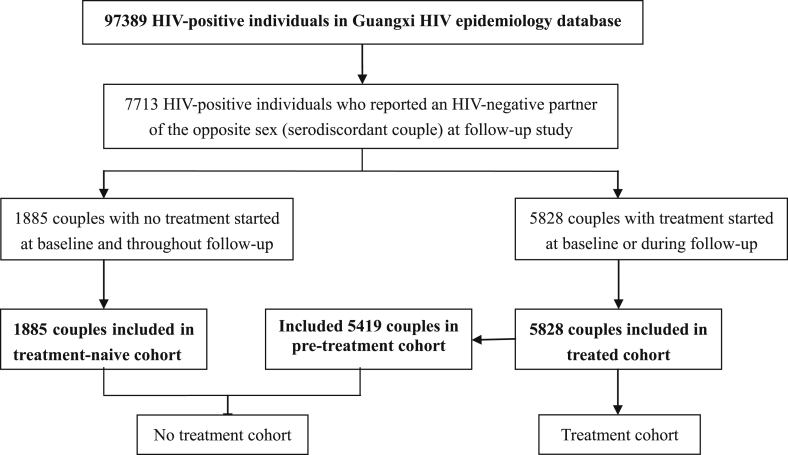
By the end of 2014, 97389 HIV cases were reported to the Guangxi HIV epidemiology database. After exclusion of couples who did not meet the study criteria, a total of 7713 couples were entered into the cohort study analysis which included 1885 couples in the treatment-naive cohort and 5828 couples in the treated cohort. Fig. 1.
Fig. 1.
Study profile.
The numbers of participants were 7266 for non seroconversion couples and 447 for seroconversion couples, respectively. During the follow-up of 18985.29 person-years from 2003 to 2014, the average incidence of HIV was 2.4 per 100 person-years (95% CI 2.1–2.6). HIV seroincidence rate was significantly higher among the treatment naive group (4.2 per 100 person-years, 3.7–4.8) compared with the on treatment group (1.6 per 100 person-years, 1.3–1.8). Table 1.
Table 1.
Comparison of seroconversion rates by treatment history, duration of follow-up, sociodemographics, and CD4 count.
| Treatment naive |
On treatment |
|||||||
|---|---|---|---|---|---|---|---|---|
| No. of index patients | Person-years | Seroconversions | Ratea (95%) | No. of index patients | Person-years | Seroconversions | Ratea (95%) | |
| Overall | 7304 | 5650.66 | 239 | 4.2 (3.7, 4.8) | 5828 | 13334.63 | 208 | 1.6 (1.3, 1.8) |
| Duration of follow-up | ||||||||
| ≤3 years | 7304 | 5129.42 | 229 | 4.5 (3.9, 5.0) | 5828 | 10400.99 | 190 | 1.8 (1.6, 2.1) |
| >3 years | 475 | 521.24 | 10 | 1.9 (0.7, 3.1) | 1628 | 2933.64 | 18 | 0.6 (0.3, 0.9) |
| Sex | ||||||||
| Male | 5432 | 3843.35 | 145 | 3.8 (3.2, 4.4) | 4403 | 9862.67 | 140 | 1.4 (1.2, 1.7) |
| Female | 1872 | 1807.31 | 94 | 5.2 (4.1, 6.3) | 1425 | 3471.96 | 68 | 2.0 (1.5, 2.4) |
| Age (years) | ||||||||
| 18-24 | 578 | 783.16 | 32 | 4.1 (2.7, 5.5) | 317 | 812.94 | 11 | 1.4 (0.6, 2.1) |
| ≥25 | 6726 | 4867.50 | 207 | 4.3 (3.7, 4.8) | 5511 | 12521.69 | 197 | 1.6 (1.4, 1.8) |
| Education | ||||||||
| Below high school | 6314 | 4887.68 | 211 | 4.3 (3.7, 4.9) | 4967 | 11194.38 | 182 | 1.6 (1.4, 1.9) |
| Above high school | 990 | 762.99 | 28 | 3.7 (2.3, 5.0) | 861 | 2140.26 | 26 | 1.2 (0.7, 1.7) |
| Marital status | ||||||||
| Living with partner | 476 | 509.90 | 19 | 3.7 (2.1, 5.4) | 333 | 890.03 | 12 | 1.3 (0.6, 2.1) |
| Married | 6828 | 5140.77 | 220 | 4.3 (3.7, 4.8) | 5495 | 12444.60 | 196 | 1.6 (1.4, 1.8) |
| Occupation | ||||||||
| Farmer | 5755 | 4464.61 | 200 | 4.5 (3.9, 5.1) | 4486 | 9645.12 | 160 | 1.7 (1.4, 1.9) |
| Other | 1549 | 1186.06 | 39 | 3.3 (2.3, 4.3) | 1342 | 3689.51 | 48 | 1.3 (0.9, 1.7) |
| Route of HIV transmission | ||||||||
| Heterosexual intercourse | 6660 | 4897.10 | 217 | 4.4 (3.8, 5.0) | 5266 | 11335.51 | 175 | 1.5 (1.5, 2.1) |
| Injecting drug use | 445 | 524.64 | 18 | 3.4 (1.8, 5.0) | 342 | 1164.52 | 20 | 1.7 (0.7, 2.2) |
| Other or unknown | 199 | 228.93 | 4 | 1.7 (0.0, 3.5) | 220 | 834.60 | 13 | 1.6 (0.8, 2.9) |
| CD4 cell count (per ul) | ||||||||
| <500 | 5648 | 2855.23 | 118 | 4.1 (3.4, 4.9) | 5509 | 12900.97 | 201 | 1.6 (1.3, 1.8) |
| ≥500 | 824 | 1328.08 | 39 | 2.9 (2.0, 3.9) | 214 | 294.66 | 5 | 1.7 (0.2, 3.2) |
| Missing data | 832 | 1467.35 | 82 | 5.6 (4.4, 6.8) | 105 | 139.00 | 2 | 1.4 (-0.6, 3.4) |
Note.
Rate is number of seroconversions per 100 person-years.
Because differential variables of baseline characteristics between the treatment naïve and on treatment group, we adjusted the HRs to control for potential confounding. HIV incidence rate was calculated for sub-groups stratified by the baseline variables of index patients. The analysis results of the final Cox regression model showed that HIV incidence stratified by baseline characteristics was mostly significantly negative associated with the one treatment group. An overall 45% reduction in risk of HIV transmission among serodiscordant couple was associated with ART treatment (adjusted Hazard Ratio [HR] 0.55, 95% Confidence Interval [CI] 0.44–0.69). Treatment for prevention was found to be significantly associated with several baseline characteristics of index partners: male sex 0.57 (0.43, 0.75), female sex 0.54 (0.37, 0.79), age above 25 years 0.56 (0.44, 0.71), less than high school education 0.54 (0.43, 0.69), living with partner 0.40 (0.17, 0.96), being married 0.60 (0.45, 0.72), being a farmer 0.52 (0.40, 0.66), heterosexual intercourse 0.50 (0.40, 0.64), baseline CD4 counts of 500 cells per μl or less 0.57 (0.45, 0.72), duration of follow up ≤ 3 years 0.57 (0.45, 0.71) and duration of follow up > 3 years 0.31 (0.11, 0.84). No significant differences between the treatment naïve and on treatment groups were found for the following baseline characteristics: age between 18 and 24 years, education above high school, not being a farmer, infected by injection drug use or other means, and CD4 counts of 500 cells per μl and above. Table 2.
Table 2.
Comparison of Cox regression model analyses stratified by duration of follow-up and baseline characteristics of the index patient (HIV-positive partner).
| HR (95%CI) | AHR* (95%CI) | |
|---|---|---|
| Overall | 0.48 (0.40, 0.59) | 0.55 (0.44, 0.69) |
| Duration of follow-up | ||
| ≤3 years | 0.49 (0.41, 0.60) | 0.57 (0.45, 0.71) |
| >3 years | 0.33 (0.15, 0.73) | 0.31 (0.11, 0.84) |
| Sex | ||
| Male | 0.49 (0.39, 0.63) | 0.57 (0.43, 0.75) |
| Female | 0.51 (0.37, 0.70) | 0.54 (0.37, 0.79) |
| Age (years) | ||
| 18-24 | 0.38 (0.19, 0.78) | 0.52 (0.24, 1.15) |
| ≥25 | 0.50 (0.41, 0.61) | 0.56 (0.44, 0.71) |
| Education | ||
| Below high school | 0.49 (0.40, 0.60) | 0.54 (0.43, 0.69) |
| Above high school | 0.48 (0.28, 0.84) | 0.62 (0.33, 1.19) |
| Marital status | ||
| Living with partner | 0.47 (0.22, 0.99) | 0.40 (0.17, 0.96) |
| Married | 0.49 (0.40, 0.59) | 0.60 (0.45, 0.72) |
| Occupation | ||
| Farmer | 0.47 (0.38, 0.59) | 0.52 (0.40, 0.66) |
| Other | 0.56 (0.36, 0.87) | 0.75 (0.44, 1.28) |
| Route of HIV transmission | ||
| Heterosexual intercourse | 0.45 (0.37, 0.55) | 0.50 (0.40, 0.64) |
| Injecting drug use | 0.63 (0.32, 1.23) | 1.07 (0.42, 2.75) |
| Other or unknown | 1.82 (0.58, 5.77) | 2.18 (0.52, 9.11) |
| CD4 cell count (per ul) | ||
| <500 | 0.56 (0.44, 0.71) | 0.57 (0.45, 0.72) |
| ≥500 | 0.69 (0.27, 1.75) | 0.66 (0.26, 1.71) |
| Missing data | 0.25 (0.06, 1.01) | 0.24 (0.06, 0.97) |
Note: HR = hazard ratio.
4. Discussion
Our study found an overall 45% reduction of treatment for preventing HIV among serodiscordant couples in Guangxi. Several previous study results showed a relative reduction in HIV in the treated cohort of Chinese national or regional serodiscordant couples (He et al., 2013; Jia et al., 2013; Wang et al., 2013). However, results from those studies may have been biased because the follow-up time of index patients prior to their initiation of ART was not included. Treatment effectiveness was evaluated by only comparing the follow-up time of index partners who never received any ART with the follow-up time of index partners after they had initiated ART. Such an analysis might result in a bias towards couples who are inherently less likely to transmit. Our study was to conduct a cohort analysis of serodiscordant couples whether the index partner receives ART or not will be treated as a time-dependent covariate in the extended Cox model. According to the results of the HIV Prevention Trials Network (HPTN) 052 trial (Cohen et al., 2011, 2016), treatment-as-prevention among serodiscordant couples under real-world conditions can be feasible on a national or regional scale.
The finding of our study was that treatment for prevention may be less to those couples whose index partners had CD4 cell counts above 500 before initializing ART. One cohort study in China showed that patients with higher CD4 counts before treatment were at increased risk for poor virological outcome (Wang et al., 2014), and other study in China has also found that patients with higher CD4 cell counts at ART initiation were more likely to attrition (Pan, Shen, Xing, Ruan, & Shao, 2018; Tang et al., 2017). The impact of early ART initiation on adherence warrants further investigation. Treatment prevention had significantly effectiveness for most baseline characteristics of index partners, such as for male, female, age above 25 years, education below high school, farmer, infected by heterosexual intercourse. ART adherence and education are a main challenge for successful implementing such strategies in real-world settings. Meanwhile, the comprehensive harm reduction programs are urgently needed to serodiscordant couples.
Conflicts of interest
The authors declare that they have no competing interests.
Authors' contributions
HC, XY, SP, HX, YS, WY, YS were responsible for study design and planning. HC, XY, QZ, XW, LC, HL, LL, GL, XG, ZT, ZS, HX, YR, WY, YS contributed to data collection and analysis. HC, XY, QZ, XW, SP, YR, YS, WY, YS contributed to interpretation. HC, XY, SP, YR, YS, WY, YS contributed to writing the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgments
This study was supported by the Guangxi Medical and Health Project (Z20170126), Guangxi Science and Technology Bureau (Grant AB16380213), National Natural Science Foundation of China (Grants 81502862, 81460510 and 81360442), Guangxi Bagui Honor Scholarship, Ministry of Science and Technology of China (2017ZX10201101, 2018ZX10721102-006), and Chinese State Key Laboratory of Infectious Disease Prevention and Control.
Handling Editor: Jianhong Wu
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.idm.2018.09.007.
Contributor Information
Yiming Shao, Email: yshao@bjmu.edu.cn.
Wenmin Yang, Email: ywm5839@168.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Chinese Center for Disease Control and Prevention, China . 2006. Analysis of HIV/STD epidemic in 2006. (Beijing,China) [Google Scholar]
- Chinese Center for Disease Control and Prevention, China . 2007. Analysis of HIV/STD epidemic in 2007. (Beijing,China) [Google Scholar]
- Chinese Center for Disease Control and Prevention, China . 2015. Analysis of HIV/STD epidemic in 2015. (Beijing,China) [Google Scholar]
- Chinese Center for Disease Control and Prevention, China . 2017. Analysis of HIV/STD epidemic in 2017. (Beijing,China) [Google Scholar]
- Cohen M.S., Chen Y.Q., McCauley M., Gamble T., Hosseinipour M.C., Kumarasamy N.…Fleming T.R. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen M.S., Chen Y.Q., McCauley M., Gamble T., Hosseinipour M.C., Kumarasamy N.…Fleming T.R. Antiretroviral therapy for the prevention of HIV-1 transmission. New England Journal of Medicine. 2016;375(9):830–839. doi: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han M., Chen Q., Hao Y., Hu Y., Wang D., Gao Y. Design and implementation of a China comprehensive AIDS response programme (China CARES), 2003-08. International Journal of Epidemiology. 2010;39(Suppl 2):ii47–ii55. doi: 10.1093/ije/dyq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He N., Duan S., Ding Y., Rou K., McGoogan J.M., Jia M.…Wu Z. Antiretroviral therapy reduces HIV transmission in discordant couples in rural Yunnan, China. PloS One. 2013;8(11) doi: 10.1371/journal.pone.0077981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia Z., Mao Y., Zhang F., Ruan Y., Ma Y., Li J.…Shao Y. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003-11): A national observational cohort study. Lancet. 2013;382(9899):1195–1203. doi: 10.1016/S0140-6736(12)61898-4. [DOI] [PubMed] [Google Scholar]
- Liu B., Sullivan S.G., Wu Z. An evaluation of needle exchange programmes in China. AIDS. 2007;21(Suppl 8):S123–S128. doi: 10.1097/01.aids.0000304707.56670.cf. [DOI] [PubMed] [Google Scholar]
- Ma Y., Li Z., Zhao S.D. HIV was first discovered among IDUs in China. Zhonghua Liuxingbingxue Zazhi. 1990;11:184–185. [Google Scholar]
- Ma Y., Zhang F., Zhao Y., Zang C., Zhao D., Dou Z.…Chen R.Y. Cohort profile: The Chinese national free antiretroviral treatment cohort. International Journal of Epidemiology. 2010;39(4):973–979. doi: 10.1093/ije/dyp233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Narcotics Control Commission, China . 2002. Annual report on drug control in China. (Beijing,China) [Google Scholar]
- Pan S.W., Shen Z., Xing H., Ruan Y., Shao Y. High baseline CD4 counts and antiretroviral therapy cessation. Clinical Infectious Diseases. 2018 doi: 10.1093/cid/ciy131. [DOI] [PubMed] [Google Scholar]
- Poon A.N., Li Z., Wang N., Hong Y. Review of HIV and other sexually transmitted infections among female sex workers in China. AIDS Care. 2011 Jun;23(Suppl 1):5–25. doi: 10.1080/09540121.2011.554519. Review. PubMed PMID: 21660747. [DOI] [PubMed] [Google Scholar]
- Qian H.Z., Hao C., Ruan Y., Cassell H.M., Chen K., Qin G.…Shao Y. Impact of methadone on drug use and risky sex in China. Journal of Substance Abuse Treatment. 2008;34(4):391–397. doi: 10.1016/j.jsat.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Qian H.Z., Vermund S.H., Wang N. Risk of HIV/AIDS in China: Subpopulations of special importance. Sexually Transmitted Infections. 2005;81(6):442–447. doi: 10.1136/sti.2004.014258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rou K., Sullivan S.G., Liu P., Wu Z. Scaling up prevention programmes to reduce the sexual transmission of HIV in China. International Journal of Epidemiology. 2010;39(Suppl 2):ii38–ii46. doi: 10.1093/ije/dyq211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan Y., Liang S., Zhu J., Li X., Pan S.W., Liu Q. Evaluation of harm reduction programs on seroincidence of HIV, hepatitis B and C, and syphilis among intravenous drug users in southwest China. Sexually Transmitted Diseases. 2013;40(4):323–328. doi: 10.1097/OLQ.0b013e31827fd4d4. [DOI] [PubMed] [Google Scholar]
- Ruan Y., Qin G., Liu S., Qian H., Zhang L., Zhou F. HIV incidence and factors contributed to retention in a 12-month follow-up study of injection drug users in Sichuan Province, China. Journal of Acquired Immune Deficiency Syndromes. 2005;39(4):459–463. doi: 10.1097/01.qai.0000152398.47025.0f. [DOI] [PubMed] [Google Scholar]
- Shan H., Wang J.X., Ren F.R., Zhang Y.Z., Zhao H.Y., Gao G.J. Blood banking in China. Lancet. 2002;360(9347):1770–1775. doi: 10.1016/S0140-6736(02)11669-2. [DOI] [PubMed] [Google Scholar]
- Tang Z., Pan S.W., Ruan Y., Liu X., Su J., Zhu Q.…Shao Y. Effects of high CD4 cell counts on death and attrition among HIV patients receiving antiretroviral treatment: An observational cohort study. Scientific Reports. 2017;7(1):3129. doi: 10.1038/s41598-017-03384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., He C., Hsi J.H., Xu X., Liu Y., He J.…Xing H. Virological outcomes and drug resistance in Chinese patients after 12 months of 3TC-based first-line antiretroviral treatment, 2011-2012. PloS One. 2014;9(2) doi: 10.1371/journal.pone.0088305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Wang L., Smith M.K., Li L.M., Ming S., Lu J.…Wang N. Heterosexual transmission of HIV and related risk factors among serodiscordant couples in Henan province, China. Chinese Medical Journal (Engl) 2013;126(19):3694–3700. [PubMed] [Google Scholar]
- Wang L., Zheng X.W., Qian H.Z., Lu F., Xing H. Epidemiologic study on human immunodeficiency virus infection among children in a former paid plasma donating community in China. Chinese Medical Journal (Engl) 2005;118(9):720–724. [PubMed] [Google Scholar]
- Wei L., Chen J., Rodolph M., Beauchamp G., Masse B., Li R.…Jackson J.B. HIV incidence, retention, and changes of high-risk behaviors among rural injection drug users in Guangxi, China. Substance Abuse. 2006;27(4):53–61. doi: 10.1300/j465v27n04_07. [DOI] [PubMed] [Google Scholar]
- Yan J., Zheng X., Zhang X., Liu S., Zhang Y., Wang C. The survey of prevalence of HIV infection among paid blood donors in one county in China. Zhonghua Liuxingbingxue Zazhi. 2000;21(1):10–13. [PubMed] [Google Scholar]
- Yin W., Hao Y., Sun X., Gong X., Li F., Li J.…Wu Z. Scaling up the national methadone maintenance treatment program in China: Achievements and challenges. International Journal of Epidemiology. 2010;39(Suppl 2):ii29–ii37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin L., Qin G., Qian H.Z., Zhu Y., Hu W., Zhang L.…Shao Y. Continued spread of HIV among injecting drug users in southern Sichuan Province, China. Harm Reduction Journal. 2007;4:6. doi: 10.1186/1477-7517-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K.K.L., Ma S.J. Epidemiology of HIV in China. BMJ. 2002;324(7341):803–804. doi: 10.1136/bmj.324.7341.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Dou Z., Ma Y., Zhang Y., Zhao Y., Zhao D. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on hiv-related mortality in China: A national observational cohort study. The Lancet Infectious Diseases. 2011;11(7):516. doi: 10.1016/S1473-3099(11)70097-4. [DOI] [PubMed] [Google Scholar]
- Zhang F., Dou Z., Yu L., Xu J., Jiao J.H., Wang N.…Chen R.Y. The effect of highly active antiretroviral therapy on mortality among HIV-infected former plasma donors in China. Clinical Infectious Diseases. 2008;47(6):825–833. doi: 10.1086/590945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Liang S., Lu W., Pan S.W., Song B., Liu Q.…Ruan Y. HIV, syphilis, and behavioral risk factors among female sex workers before and after implementation of harm reduction programs in a high drug-using area of China. PloS One. 2014;9(1) doi: 10.1371/journal.pone.0084950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Shan H., Trizzino J., Ruan Y., Beauchamp G., Masse B.…Shao Y. HIV incidence, retention rate, and baseline predictors of HIV incidence and retention in a prospective cohort study of injection drug users in Xinjiang, China. International Journal of Infectious Diseases. 2007;11(4):318–323. doi: 10.1016/j.ijid.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Zheng X., Tian C., Choi K.H., Zhang J., Cheng H., Yang X. Injecting drug use and HIV infection in southwest China. AIDS. 1994;8(8):1141–1147. doi: 10.1097/00002030-199408000-00017. [DOI] [PubMed] [Google Scholar]
- Zheng X., Tian C., Zhang G., Li D., Liu X., Hu D.J.…Dondero T.J. HIV risk behaviors but absence of infection among drug users in detoxification centers outside Yunnan province, China, 1993. AIDS. 1995;9(8):959–963. doi: 10.1097/00002030-199508000-00020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.