Abstract
Objective
To evaluate thermography application as a complementary method in preventing muscle injury in professional soccer players.
Methods
A longitudinal prospective study with 28 professional soccer players that composed a first division of Brazilian’s soccer team between 2015 and 2016. In both seasons (2015 and 2016), muscle injuries were documented and classified in grade of severity, by ultrasound. During the following season (2016), infrared medical thermography was applied twice a week (48 hours after game) and if a difference of temperature was detected higher than 0.4°C, a prevention protocol was initiated. Muscle injuries in 2016 were documented.
Results
In 2015, the total number of muscle injuries was 11. In 2016, the total number of muscle injuries was 4 (p=0.04). It represents an incidence/player of 78% in 2015 and 28% in 2016, corresponding to a decrease of 64% in 2016. Seven players played in the first team in both seasons. Among these seven players, muscle injuries were reduced from 8 (in 2015) to 3 (in 2016)—a decrease of 63% in the season we used thermographic monitoring (p=0.06).
Conclusion
The pilot data provide a promising catalyst for a rigorous RCT that could examine whether thermography can contribute to a muscle injury prevention programme.
Keywords: soccer, muscle injury, thermography, prevention and temperature
What are new findings?
Infrared medical thermography is as a non-invasive and non-ionising radiation method that can provide information about the states of muscle tissue.
Introduction
Muscle injuries are the most common cause of physical disability in sports practice and represents 20%–37% of all time-loss injuries at men’s professional soccer level.1 2 Treatment is challenging for both sports physician and athlete.
The first step in injury prevention is to evaluate the epidemiology of injuries and establish injuries risks and circumstances. It is known that number of matches per season,3 previous injuries,2 inadequate rehabilitation,4 decreased recovery time between matches,5 discrepancy between the coach-intended intensity and the actual training intensity perceived by the player (internal effort),6 the influence of the season,4 age and playing position7 are some of risks factors for muscle injuries. Some factors cannot be modified because they are intrinsic such as age and previous injuries. However, some of them are related to exercise load (number of matches, decrease of recovery time, internal effort) and can be modified or, at least, monitored.
Infrared medical thermography (IMT), a non-invasive and non-ionising radiation analysis, can provide information about the states of muscle tissue and, then, can be used as an instrument to identify risks and prevent injuries.8
Athletes are exposed to physical stress of training and competition and overload reactions cause a change in blood flow that affects skin temperature.9 IMT does not show anatomical abnormalities, but reveals functional changes related to the control of skin temperature.9 10 Our purpose was to trial IMT in a clinical setting.
Methods/Design
A longitudinal prospective study conducted during two seasons of Brazilian soccer league. During the first year (2015 season) of research, muscle injuries were documented and classified in grade of severity (minimal, mild, moderate and severe) by an ultrasound examination by the same team physicians. During the following season (2016), IMT was applied twice a week (48 hours after game), some positive result was detected, and a prevention protocol was initiated. Muscle injuries in 2016 were documented and classified in grade of severity with an ultrasound examination performed by the same team physicians.
2015 season players were used as a control group of 2016 season player.
Population
Twenty-eight professional soccer players who composed a first division Brazilian’s soccer team between 2015 and 2016.
The group was homogeneous in terms of age, body weight and body height. They were all healthy and had no musculoskeletal complaints at the beginning of research. All participants provided written informed consent.
Inclusion criteria
Athletes from a professional first division Brazilian soccer team in both seasons 2015 and 2016, who played regularly.
Exclusion criteria
Goalkeepers due to different time in training.
Muscle injury diagnosis
Muscle injury was defined as: any physical complaint sustained by a player that results from a match or training, irrespective of the need for medical attention or time away from soccer activities.11
Clinical evaluation was carried out by team physician using ultrasound examination, always performed by the same operator.
Severity of muscle injuries was classified according to the criteria of Federation Internationale de Football Association Medical Assessment and Research Centre (F-MARC): The number of days that have elapsed from the date of injury to the date of the player’s return to full participation in team training and availability for match selection: slight (0 days); minimal (1–3 days); mild (4–7 days); moderate (8–28 days); severe (>28 days); career ending.11
Thermography and data analysis
According to the literature, the highest incidence of muscle injury in soccer players occurs during games. In addition, around 48 hours of recovery is necessary to decrease the delayed onset muscle soreness and creative kinase activity.11 Because of that, thermography was applied 48 hours after games. Images were collected and analysed by a qualified medical professional.
Athletes were instructed not to consume alcohol or caffeine within 4 hours prior to thermographic analysis. They were also counselled to remove any cosmetic or anti-inflammatory products that could influence the thermal image of skin temperature.
The environmental conditions in the physiology laboratory during the tests were constant at 23.0°C (±1.0%) and 40%–60% of relative humidity air. Before the measurements were obtained, the subjects stayed in the laboratory for at least 15 min to acclimatise, in concordance with standard recommendations followed in the literature.12 Thermographic measurements from the front and back surfaces of each participant were acquired in a standing upright resting position.
All thermographic images were recorded digitally by a thermography camera with an infrared resolution of 320×240 pixels and thermal sensitivity of 30 mK (FLIR T450sc). The camera was positioned 3 m from the subjects and kept perpendicular to regions of interest. Images were recorded in a controlled environment (with light and temperature controlled room) and were stored for offline analysis using a scientific software (Flir ResearchIR Max 4). All images were processed using an emissivity factor of 0.98 to obtain human skin temperatures. The Rainbow pallet was used with scale fix to 27°C–35°C.
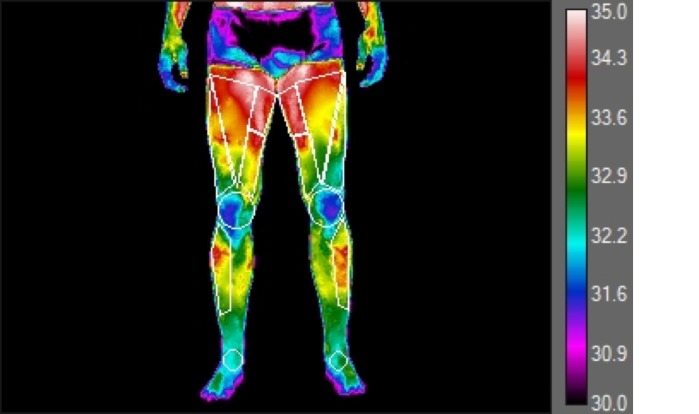
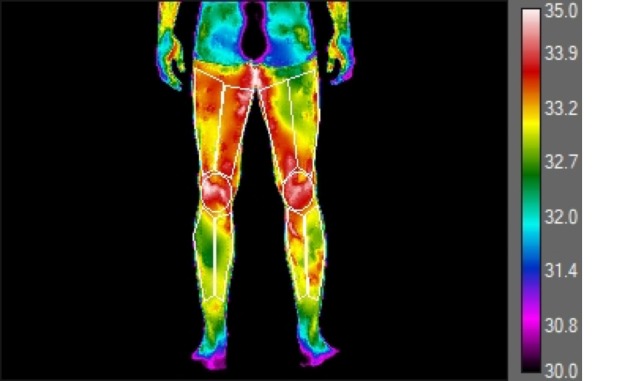
Evaluations were performed before training. Knowing that frequency of the evaluation of athletes and the number of region of interest (ROI) should be as high as possible to be successful, 12 ROIs were defined: 7 anterior and 5 posterior of lower limbs (figures 1 and 2). Images were obtained twice a week (48 hours after game).
Figure 1.
Thermogram with ROIs—anterior view prevention programme. ROI, region of interest.
Figure 2.
Thermogram with ROIs—posterior view. ROI, region of interest.
The examiner analysed the evolution of the same area over time and examined the asymmetries between contralateral ROI (ie, left vs right side). Table 1 shows the reference values of asymmetry between contralateral limbs used to facilitate decisions, regarding the relevance of thermal asymmetry on injury prevention protocols, based on the research by Gómez Carmona.13
Table 1.
Reference values of asymmetry
| Difference of temperature | Medical conduct |
| 0.3°C–0.4°C | Following up |
| 0.5°C–1.0°C | Preventive measures |
| 1.1°C–1.5°C | Alarm! (Injury risk)+Preventive measures |
| >1.5°C | Severe asymmetry |
A difference up to 0.3 was considered normal.13 The reason for that is to account the error of the camera, the error of capture, the shape of the body (that is not flat), the variability of the definition of left and right ROI and, also, the fact that in sports with dominant sides (tennis, football, judo and so on) the laterality of the athletes should be considered, since specialisation generates thermal asymmetries that are completely normal.13 A difference between 0.3 and 0.4 was followed up and the health team was alerted.
For differences of 0.5°C–1.0°C, preventive measurements were performed even if the athlete did not manifest symptoms of discomfort or injury, mainly when the thermal asymmetries had progressed from lower values in previous evaluations.13
Values from 1.0°C to 1.5°C, in most cases, were interpreted as indicating high injury risk and when values were above 1.5°C, risk was considered even higher.13
Prevention protocol
Prevention protocol was based on:
Cryotherapy.
Physiotherapy.
Reduction of training load.
Change in training load.
Massage.
Use of recovery boots.
The decision of what kind of therapy was performed for each athlete was made by the team’s physician.
Risk analysed
Thermographic study is a non-invasive procedure and it offers minimal risk to athlete.
Results
During 2 years of research, a total of 28 players, who participated regularly in games (first team) were followed: 14 players in 2015 and 14 players in 2016 season. Seven players participated in both seasons in first team.
The group was homogeneous in terms of age, body weight, height and percentage body fat. Table 2 shows means and standard deviation (SD) values.
Table 2.
Players and injuries characteristics
| 2015 | 2016 | P value | |
| Number of players | 14 | 14 | |
| Players anthropometrics, mean±SD | |||
| Age, years | 27.15±4.30 | 26.5±3.27 | 0.06 |
| Height, cm | 1.78±0.06 | 1.79±0.06 | 0.42 |
| Weight, kg | 77.62±7.12 | 77.94±7.18 | 0.18 |
| Percentage body fat, % | 11.8±1.86 | 10.4±1.86 | 0.22 |
| Exposure training, hour/player/season | 384 | 390 | |
| Exposure match, hour/player/season | 106,5 | 99 | |
| Number of muscle injuries | 11 | 4 | 0.04 |
| Total muscle injury incidence/player | 0.78 | 0.28 | |
| Injury incidence, training | 0.09 | 0 | |
| Injury incidence, match | 0.91 | 1.0 | |
| Injury severity (%) | |||
| Minimal (1–3 days) | 0 | 0 | |
| Mild (4–7 days) | 2 (18.2) | 1 (25) | |
| Moderate (8–28 days) | 9 (81.8) | 3 (75) | |
| Severe (>28 days) | 0 | 0 | |
| Days of absence, days | 189 | 62 | |
| Days of absence/injury, mean±SD | 17.18±8.02 | 15.5±5.80 |
2015 season had a higher number of games (71) than 2016 season (66), but there is no statistically significant difference (p=0.11).
A total of 585 images were analyses during 2016, and 150 (26%) presented at least one ROI altered (asymmetry>0.4°C). Preventive protocol was applied for the players who had this asymmetry.
In 2015, the total number of muscle injuries was 11. In 2016, the total number of muscle injuries was 4 (p=0.04). It represents an incidence/player of 78% in 2015 and 28% in 2016, corresponding to a decrease of 64% in 2016.
It is known, however, that the cast of two seasons in a soccer club is not the same, but seven players composed the first team in both seasons. Considering this sample, there was a reduction from 8 (in 2015) to 3 (in 2016) lesions, corresponding to a decrease of 62.5% in the incidence of lesions using thermographic monitoring (p=0.06).
It is known that the number of hours spent in practice and game is critical to calculate the injury rate (IR) per 1000 hours of athlete-exposure (AE). The IR per 1000 AE was calculated by dividing the number of injuries by the number of AE (1 AE is defined as 1 player participating in 1 hour of match or 1 hour of practice session). Overall injury incidence was 1.6/1000 hour, in 2015 and 0.5/1000 hour, in 2016.
All injuries affected the lower extremities. A calculated 87% of injuries occurred in posterior thigh region (hamstring) and 13% in calf muscle. Fifty-three per cent of muscle injuries affected the dominant leg (preferred kicking leg), and 47% affected the non-dominant leg.
Three athletes had reinjury in 2015. All athletes who had muscle injury in the first year (2015) did not report lesions at the same site the following year.
The period of time lost was defined as the time of injury until the time the athlete was released to participate in team practice and was used to classify the injuries as minimal (1–3 days), mild (4–7 days), moderate (8–30 days) or severe (>31 days). In both seasons, 3 muscle injuries were classified as mild, 12 as moderate and no one was classified as severe. In 2015, 18% of injuries were mild, and 82% moderate, while in 2016, 25% of injuries documented were mild and 75% moderate.
During the 2015 season, muscle strain resulted in a mean of 189 days lost. Knowing that there was a total of 11 muscular injuries in 2015, the mean of days lost due to injury was 17.18 days.
During the 2016 season, muscle strain resulted in a mean of 62 days lost. Knowing that there was a total of 4 muscular injuries in 2016, the mean of days of absence due to injury was 15.5 days.
Discussion
To guarantee the internal validity of the study, it was necessary to standardise data collection, to define the population of the same team that submitted to the same protocols of technical and medical committee, that were at same environment and were submitted to the same training load in both seasons. In addition, the groups in seasons were homogenous for age, weight, height, body composition and training level (all of the subjects participated of First Division of Brazilian’s Soccer Championship) and there was no significant difference between number of games and time of exposure to training.
Thus, difference between both years was only introduction of thermographic analysis with the orientation of a prevention protocol, starting from an altered thermal result.
An epidemiological study in 51 soccer teams, comprising 2299 players, registered 2908 muscle injuries. On average, during a season, a player sustained 0.6 muscle injuries and a squad of 25 players can thus expect about 15 muscle injuries.1
In the present study, in 2015, the total number of 11 muscle injuries documented in 14 players was higher than Ekstrand’s study, and, it represented that a player sustained 0.78 muscle injury. In 2016, the total number of muscle injuries decreased to 4 in 14 players and, it represented that a player sustained 0.28 muscle injury (reduction of 64% with p value analysis of 0.04).
Overall, 6867 hours of exposure (5376 hours of training and 1491 hours of match play) were registered in 2015. In 2016, 6762 hours of exposure (5376 hours of training and 1386 hours of match play) were registered. Thus, injury incidence was 1.6/1000 hour in 2015 and 0.5/1000 hour in 2016.
We found that muscle injuries were reduced in 2016. The only difference in athletes training routine, during 2 years (2015 and 2016), was thermographic analysis and intervention with a load reduction programme in cases where we identified an ‘abnormal’ signal. Although we cannot attribute cause to this association, we respectfully suggest that possibility need to be considered—that the studied method and the prevention protocol reduced injuries.
Considering the players who remained with the team for both seasons, we observed an important reduction in the incidence of injuries. Due to this small sample (seven athletes), there was no statistically significant reduction between both years (p=0.06). However, there was a large reduction (63%), which is very close to reduction in full group (64%).
Our findings extend existing literature4 as the greatest number of muscular injuries detected occurred during soccer games (93% of muscles injuries) than during training. In 2015 and 2016, 91% and 100%, respectively, of lesions occurred during matches.
Literature shows that 92% of muscle injuries affected the lower extremities. The hamstring (37%), adductor (23%), quadriceps (19%) and calf (13%) muscles were the most common injury locations. Injury to the hamstring muscle group was the most common single injury subtype, representing 12% of all injuries. The majority of quadriceps strains (60%) affected the dominant leg (preferred kicking leg), 33% affected the non-dominant leg and 7% affected both legs or the leg dominance was unknown (p<0.05). The dominance of muscle injuries to the kicking leg was less obvious in other muscle groups (hamstrings, 50%; adductors, 54% and calf muscles, 51%).1 The present study reported a result of 87% of injuries occurred in hamstring with a dominance of 53%, as literature showed.
A systematic review about injury incidences in soccer players showed six studies where the majority of injuries were considered moderate and four studies where the majority of injuries were mild.14 Although most players were able to return to full training and match play within 4 weeks, muscle injuries are a substantial problem for the players and their clubs. A team of 25 players at the elite level can expect about 15 muscle injuries each season, with approximately 2 weeks missed for each injury. This quantity of time loss could be devastating because players sidelined due to injury limit the possibility of optimal performance by the team.1 The present study revealed that majority of injuries were mild.
Several researches reported on recurrent injuries in soccer players. Prior muscle injury is commonly suggested as risk factor for soccer players. Reinjury incidences range between 9% and 30% in professional adult soccer players and cause longer absences than new injuries. Findings from this study show that athletes who had muscle injury in the first year (2015) did not present lesions at the same site the following year. Thus, the early identification of the risk of injury, through thermography and the preventive protocol applied, was important because there was no reinjury. Thus, the severity of lesions and time away in 2016 was lower.
As important as number of injuries is the time away of the athlete to treat the injury. The results showed that in 2015, players spent 189 days in Medical Department to treat muscle injuries. As early as 2016, the time taken for treatment was 62 days. Thus, in 2016, more players were available to play and train than there were in 2015.
Understanding the commercial value of an athlete in game conditions, it is important to consider the cost of an athlete in medical department. Considering that, mean salary of cast is U$75,000,00/month, cost of players absence as a result of muscle injuries was, in 2015, U$472,500,00, instead U$ 155,000,00, in 2016.
Conclusion
Our pilot data provide a promising catalyst for a rigorous RCT that could examine whether thermography can contribute to a muscle injury prevention programme.
Acknowledgments
This research was realised without any financial agency. Thanks are given for all participants who volunteered for this study.
Footnotes
Contributors: All authors were important and contributed equally to this paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Ethics approval: Ethics Committee of Medicine School of University of São Paulo.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 2011;39:1226–32. 10.1177/0363546510395879 [DOI] [PubMed] [Google Scholar]
- 2. Andersen TE, Tenga A, Engebretsen L, et al. . Video analysis of injuries and incidents in Norwegian professional football. Br J Sports Med 2004;38:626–31. 10.1136/bjsm.2003.007955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bjørneboe J, Bahr R, Andersen TE. Gradual increase in the risk of match injury in Norwegian male professional football: a 6-year prospective study. Scand J Med Sci Sports 2014;24:189–96. 10.1111/j.1600-0838.2012.01476.x [DOI] [PubMed] [Google Scholar]
- 4. Waldén M, Hägglund M, Ekstrand J. Injuries in Swedish elite football-a prospective study on injury definitions, risk for injury and injury pattern during 2001. Scand J Med Sci Sports 2005;15:118–25. 10.1111/j.1600-0838.2004.00393.x [DOI] [PubMed] [Google Scholar]
- 5. Dupont G, Nedelec M, McCall A, et al. . Effect of 2 soccer matches in a week on physical performance and injury rate. Am J Sports Med 2010;38:1752–8. 10.1177/0363546510361236 [DOI] [PubMed] [Google Scholar]
- 6. Brink MS, Frencken W GP, Jordet G, et al. . Coaches' and players' perceptions of training dose: not a perfect match. Int J Sports Physiol Perform 2014;9:497–502. 10.1123/ijspp.2013-0009 [DOI] [PubMed] [Google Scholar]
- 7. Deehan DJ, Bell K, McCaskie AW. Adolescent musculoskeletal injuries in a football academy. J Bone Joint Surg Br 2007;89:5–8. 10.1302/0301-620X.89B1.18427 [DOI] [PubMed] [Google Scholar]
- 8. Côrte ACRe, Hernandez AJ. Termografia médica infravermelha aplicada medicina do esporte. Revista Brasileira de Medicina do Esporte 2016;22:315–9. 10.1590/1517-869220162204160783 [DOI] [Google Scholar]
- 9. Merla A, Mattei PA, Di Donato L, et al. . Thermal imaging of cutaneous temperature modifications in runners during graded exercise. Ann Biomed Eng 2010;38:158–63. 10.1007/s10439-009-9809-8 [DOI] [PubMed] [Google Scholar]
- 10. Ring EF, Ammer K. Infrared thermal imaging in medicine. Physiol Meas 2012;33:R33–R46. 10.1088/0967-3334/33/3/R33 [DOI] [PubMed] [Google Scholar]
- 11. Fuller CW, Ekstrand J, Junge A, et al. . Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports 2006;16:83–92. 10.1111/j.1600-0838.2006.00528.x [DOI] [PubMed] [Google Scholar]
- 12. Hildebrandt C, Raschner C, Ammer K. An overview of recent application of medical infrared thermography in sports medicine in Austria. Sensors 2010;10:4700–15. 10.3390/s100504700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Carmona P. Influencia de la información termográfica infrarroja en el protocolo de prevención de lesiones de un equipo de fútbol profesional español, 2012. [Google Scholar]
- 14. Pfirrmann D, Herbst M, Ingelfinger P, et al. . Analysis of Injury Incidences in Male Professional Adult and Elite Youth Soccer Players: A Systematic Review. J Athl Train 2016;51:410–24. 10.4085/1062-6050-51.6.03 [DOI] [PMC free article] [PubMed] [Google Scholar]