Abstract
Acute disseminated encephalomyelitis (ADEM) is a rare inflammatory-demyelinating disease of central nervous system. Several viral infections and vaccines act as precipitating factor for ADEM. We report an 8-year-old girl presenting with acute-onset flaccid paraparesis and bilateral painless vision loss. MRI brain showed extensive multifocal patchy demyelination and she made good clinical recovery with steroids and intravenous immunoglobulin therapy. She had history of bilateral parotid swelling before the onset of neurological symptoms and diagnosis of mumps was confirmed by positive ELISA in serum. Mumps, usually a benign and self-limited viral infection, rarely can cause severe neurological complications. Hence, we report this case to emphasise the importance of mumps vaccination and the need to strengthen the health policy system for the prevention of disease.
Keywords: infection (neurology), neuroimaging, vaccination/immunisation, paediatrics
Background
Mumps virus is a neurotropic virus with evidence of central nervous system (CNS) involvement in ~30% cases. CNS manifestations of mumps are protean; varies from aseptic meningitis (10%), to acute encephalitis (<0.5%), polyneuropathy, postinfectious demyelination, deafness and neuroretinitis.1 2 We report an 8-year-old unimmunised girl who developed acute disseminated encephalomyelitis (ADEM) following mumps parotitis.
Case presentation
An 8-year-old girl presented with acute-onset weakness of both the lower limbs with urinary retention. She was noted to have right side painful parotid swelling with odynophagia 6 days prior to the onset of neurological symptoms. Her neurological symptoms progressed over next 48 hours so much so that she became bed bound. She was also noted to have blurring of vision in both eyes. On examination, she was drowsy, had low Glasgow Coma Scale of −9/15, bilateral external ophthalmoplegia, weak gag, right hypoglossal nerve palsy, flaccid quadriparesis, exaggerated reflexes, extensor plantar and positive meningeal signs. She was unimmunised for mumps in her childhood.
Investigations
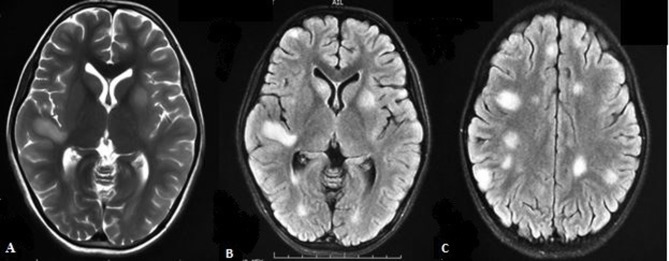
In view of preceding history of parotitis, a strong clinical possibility of postinfective ADEM was considered. MRI brain showed patchy, multifocal T2/fluid attenuation inversion recovery (FLAIR) white matter hyperintensities (figure 1) and MRI spine showed T2/FLAIR hyperintensities involving cervicodorsal cord suggestive of ADEM with longitudinally extensive transverse myelitis (figure 2). Visual evoked potentials were normal. Lumbar cerebrospinal fluid (CSF) analysis was acellular, protein was 70 mg/dL and glucose was 56 mg/dL. CSF gram stain and cultures were sterile. CSF oligoclonal band and antiaquaporin-4 antibodies were negative. Mumps serology done by IgM ELISA (IBL International, Germany) was positive in serum.
Figure 1.
Axial T2-weighted (A) and fluid attenuation inversion recovery (FLAIR), (B and C) images showing multifocal patchy, T2/FLAIR hyperintense lesions involving cerebral white matter (including centrum semiovale) and deep grey structures (right caudate and left putamen).
Figure 2.
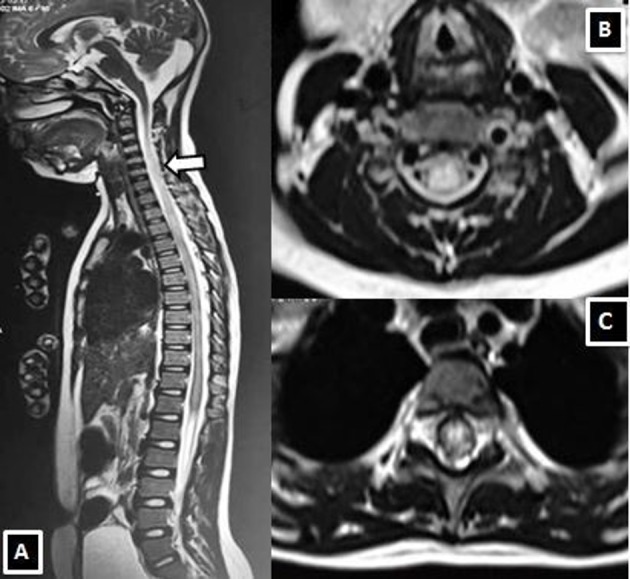
MRI spine T2-weighted sagittal (A) and T2 weighted axial images at mid-cervical (B) and thoracic spinal cord (C) demonstrating longitudinally extensive transverse myelitis in the cervicodorsal cord (white arrow).
Treatment
She was treated with methylprednisolone at 30 mg/kg/day for 5 days, however, in view of poor neurological recovery monitored with Expanded Disability Status Score, second course of methylprednisolone 30 mg/kg/day for 5 days and intravenous immunoglobulin 2 g/kg were given. Bladder care and physiotherapy advised during follow-up.
Outcome and follow-up
Presently at 6 months of follow-up, the child is ambulatory with no residual motor deficits, however, she continues to have bladder dysfunction with significant postvoid residual urine requiring regular clean intermittent catheterisation. She has been kept on regular follow-up for bladder complications.
Discussion
Neurological complications in mumps can occur before, in association or after parotitis, within first 2 weeks of illness. Aseptic meningitis is the most common neurological manifestation of mumps, present in 10% patient with mumps-related neurological complication.1 Other reported neurological complications are encephalitis, ADEM, brain stem encephalitis, sensory neural hearing loss, Guillain-Barré syndrome and peripheral neuropathy.1 2 ADEM is frequently preceded by an antecedent viral or bacterial infection in 75% of cases. However, ADEM following mumps infection has rarely been reported in children.3 Kumar et al 3 reported acute haemorrhagic leucoencephalitis following mumps in a 30-year-old man.4 The main pathogenesis hypothesised is an immune-mediated injury to the nervous system triggered by a parainfectious process.2 Unlike the previously reported case series where children with mumps associated myelitis responded to oral steroids or resolved spontaneously, index child required aggressive immunomodulation.3 Hence, we report this case to emphasise the importance of mumps vaccination and the need to strengthen the health policy system for the prevention of disease.5
Learning points.
Acute disseminated encephalomyelitis is a rare neurological complication of mumps.
Aggressive immunomodulation can restore a near normal functional ability to the child, minimising the neurological disabilities.
Importance of mumps vaccination and the need to strengthen health policy system to prevent resurgence of mumps infection in the children and adolescent age groups.
Footnotes
Contributors: AB: clinical management and preparation of manuscript. RS: patient management and clinical incharge, revision and final approval of manuscript. SV: radiology input. MPS: virology assay.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Didel S, Suthar R, Sahoo D, et al. Mumps associated acute motor axonal polyneuropathy. Indian J Pediatr 2017;84:724 10.1007/s12098-017-2351-z [DOI] [PubMed] [Google Scholar]
- 2. Menge T, Hemmer B, Nessler S, et al. Acute disseminated encephalomyelitis: an update. Arch Neurol 2005;62:1673–80. 10.1001/archneur.62.11.1673 [DOI] [PubMed] [Google Scholar]
- 3. Kumar R S, Kuruvilla A. Teaching NeuroImages: Acute hemorrhagic leukoencephalitis after mumps. Neurology 2009;73:e98 10.1212/WNL.0b013e3181c2eee3 [DOI] [PubMed] [Google Scholar]
- 4. Jha KK, Chaudhary DP, Dahal S, et al. Acute disseminated encephalomyelitis after mumps infection. J Family Med Prim Care 2016;5:892 10.4103/2249-4863.201170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Demicheli V, Rivetti A, Debalini MG, et al. Vaccines for measles, mumps and rubella in children. Evidence-Based Child Health: A Cochrane Review Journal 2013;8:2076–238. 10.1002/ebch.1948 [DOI] [Google Scholar]