Abstract
Objectives
The shift to the patient-centred care (PCC) model as a healthcare delivery paradigm calls for systematic measurement and evaluation. In an attempt to develop patient-centred quality indicators (PC-QIs), this study aimed to identify quality indicators that can be used to measure PCC.
Methods
Design: scoping review. Data Sources: studies were identified through searching seven electronic databases and the grey literature. Search terms included quality improvement, quality indicators, healthcare quality and PCC. Eligibility Criteria: articles were included if they mentioned development and/or implementation of PC-QIs. Data Extraction and Synthesis: extracted data included study characteristics (country, year of publication and type of study/article), patients’ inclusion in the development of indicators and type of patient populations and point of care if applicable (eg, in-patient, out-patient and primary care).
Results
A total 184 full-text peer-reviewed articles were assessed for eligibility for inclusion; of these, 9 articles were included in this review. From the non–peer-reviewed literature, eight documents met the criteria for inclusion in this study. This review revealed the heterogeneity describing and defining the nature of PC-QIs. Most PC-QIs were presented as PCC measures and identified as guidelines, surveys or recommendations, and therefore cannot be classified as actual PC-QIs. Out of 502 ways to measure PCC, only 25 were considered to be actual PC-QIs. None of the identified articles implemented the quality indicators in care settings.
Conclusion
The identification of PC-QIs is a key first step in laying the groundwork to develop evidence-based PC-QIs. Research is needed to continue the development and implementation of PC-QIs for healthcare quality improvement.
Keywords: patient-centred care, quality indicators, healthcare quality, quality improvement
Strengths and limitation of this study.
Transparent and rigorous search strategy.
Involvement of patient partner in the study.
Study informed by a previously published protocol.
Search strategy using only English terms.
We did not assess the quality of the measures and/or indicators identified.
Introduction
Patient-centred care (PCC) is one of the six dimensions of healthcare and was formally described by the Institute of Medicine in 2001 as healthcare that respects and responds to the preferences, needs and values of the individual patients throughout all healthcare decisions. 1 PCC is an approach that has become central to policies and programming to improve healthcare efficiencies and address patient safety issues.2
PCC is a model in which healthcare providers are encouraged to partner with patients and families to design and deliver individualised care. PCC models have been linked to positive patient experiences and improved outcomes, such as increased adherence to care and treatment.3–5 In the literature, a PCC approach has been found to benefit patients and healthcare organisations in reducing costs, for instance through decreasing the length of hospital stays and readmission rates.6 7 However, PCC is conceptualised differently among different stakeholders, impacting effective implementation in care settings.8 The adoption of a PCC model requires first, the identification of appropriate indicators to measure the quality of PCC, and second, the assessment of the impact of delivering PCC on healthcare system and patient outcomes.9
Quality indicators are tools that measure system performance and healthcare quality, and demonstrate the extent to which improvement efforts have led to desirable change, or contributed to unintended results.10 As identified from the Agency for Healthcare Research and Quality (AHRQ), a quality indicator consists of a specific aspect of quality being captured, and a method for how concepts of quality are captured (which includes data source, measure type, observable event, specification and risk adjustment).11 While various quality indicators have been developed to measure healthcare safety, effectiveness and access,12 they typically do not incorporate the priorities and experiences of patients and family caregivers. To truly evaluate the impact of patient-centredness, indicators must reflect the patient and family caregiver perspective.
This scoping review aimed to synthesise existing literature on quality indicators used in the evaluation of PCC. This review was guided by the questions: ‘What PC-QIs have been developed to measure patient-centred care?’ ‘How are patient-centred quality indicators defined?’ and ‘ Have existing PC-QIs been implemented and evaluated across various points-of-care settings, processes of care and at the systems level to measure patient-centred care?’ The information gained from this study will inform the development of PCC quality indicators that could be implemented to drive healthcare improvement valued by patients and families.
Methods
We employed a scoping review protocol that was previously published,13 using methodology based on Arksey and O’Malley’s scoping review framework14 and Levac et al’s methodological enhancement.15 We searched the peer-reviewed published and grey literature for either proposed or existing quality indicators that have been developed and/or implemented across various points-of-care settings to measure PCC. For this scoping review, the AHRQ16 definition of a quality indicator was adapted to incorporate a patient and family focus. Specifically, a PC-QI was defined as the unit of measurement of healthcare system, organisational or individual performance, that quantifies patients’ and families’ experiences with the care received and the experience of any individual who needs to contact with healthcare services. In contrast, PCC measures are in the form of a survey, guideline or recommendation.
Data sources and search strategy
In order to identify studies assessing quality indicators for PCC, search strategies were developed that combined terms from two concepts: PCC and PC-QIs (online supplementary file 1). The Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, MEDLINE, PsycINFO, Social Services Abstracts and Social Work Abstracts were searched from inception to May 2017. A search of the Google search engines, and the websites of relevant quality improvement and patient-centric organisations enabled the identification of relevant grey literature. Grey literature searches were conducted in duplicate by both a researcher and patient partner. The reference lists of included studies were also scanned to identify any other studies of relevance.
bmjopen-2018-023596supp001.pdf (80.1KB, pdf)
Citation management
All references were imported into a custom-written Java software application, Synthesis for reference management and data collection.17 Duplicate citations were removed automatically by the software, with any mismatched duplicates removed manually if detected.
Study selection and data abstraction
To be eligible for inclusion, the study/article had to (1) identify quality indicators for PCC and/or (2) identify PC-QI in performance measurement (eg, validation). The title and abstract of each citation identified was screened for eligibility independently by two reviewers (M-JS and ML). The full text of any abstract selected by either reviewer was retrieved and assessed for eligibility. Any full-text articles for which there was inter-rater discord were reviewed a second time, and final disagreements about study eligibility were resolved through discussion.
Data collection and classification of indicators
A data collection tool was developed and tested on a sample of papers to determine its practicality prior to the full review (online supplementary file 2). Extracted data included study characteristics (country, year of publication and type of study/article), patients’ inclusion in the development of indicators and type of patient populations and point of care if applicable (eg, in-patient, out-patient and primary care).
bmjopen-2018-023596supp002.pdf (165.3KB, pdf)
All extracted indicators were classified collaboratively by two authors (M-JS and SA) according to a person-centred care framework18 developed by the team and guided by the Donabedian model of quality of care.19 This framework provides a roadmap for healthcare systems to implement and measure PCC at the level of structure (the healthcare system/organisational level), process (the patient-healthcare provider interaction level) and outcome (the patient-health care provider and healthcare systems interaction level).18
Patient involvement
Levac et al recommend the involvement of stakeholders in the scoping review methodology.15 We worked closely with our patient-research partner (SZ) in the design of the study who also aided in the search strategy. Our patient research partner aided in the clarification of research questions as well. The involvement of patient research partners allows for suggestions of additional references as well as the provision of insights beyond those in the literature.15
Results
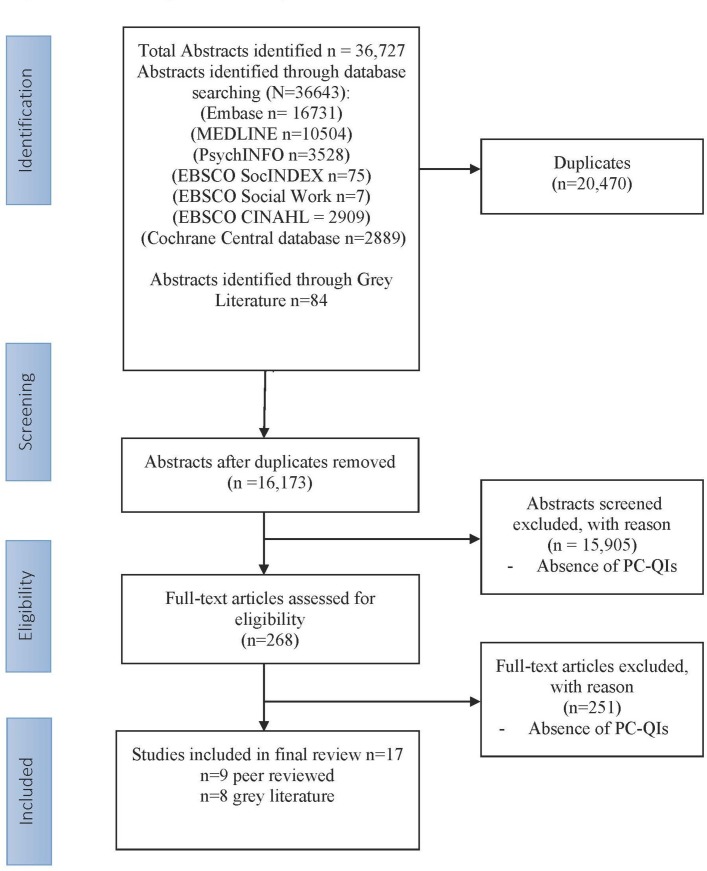
A total of 36 643 citations were retrieved, and on duplicate removal, a total of 16 173 citations were reviewed at the title and abstract stage for inclusion (figure 1). A total 184 full-text peer-reviewed articles were assessed for eligibility for inclusion; of these, 9 articles were included in this review (figure 1). From the non–peer-reviewed literature, following the title and document review, eight documents met the criteria for inclusion in this study (figure 1). The most common reason for excluding articles (n=15 905) was the absence of indicators for PCC.
Figure 1.
Flow diagram for study inclusion. PC-QIs, patient-centred quality indicators.
Article description
Table 1 presents the characteristics of the full-text articles included in the study. The years of publication ranged from 1996 to 2015. Included studies were published in Belgium (n=1), USA (n=2), Canada (n=3), UK (n=4), the Netherlands (n=4) and three sources did not include a country of publication. Sources were varied and included original peer-reviewed research (n=8), guest editorial (n=1), reports (n=4), discussion paper (n=1), working paper (n=1), literature review (n=1) and a website (n=1). The study populations varied in the peer-reviewed literature (eg, cancer, fertility care and home parenteral nutrition, HPN) and no specific populations were identified in the non–peer-reviewed literature.
Table 1.
Characteristics of articles on patient-centred quality indicators
| Study identifier (first author) | Country | Year | Study type | Population | Patients involved | Number of indicators and ways to measure PCC |
| Peer-reviewed literature (n=9) | ||||||
| den Breejen et al 42 | The Netherlands | 2013 | Focus groups/interviews/consensus meetings | Fertility care | Yes | 34 |
| Dreesen et al 29 | Belgium | 2014 | Focus groups/interviews/consensus meetings | Home parenteral nutrition (HPN) patients | Yes | 33 |
| Ouwens et al 30 | The Netherlands | 2010 | Focus groups/interviews/consensus meetings | Cancer: non–small-cell lung carcinoma | Yes | 54 |
| Sewitch et al 43 | Canada | 2013 | Focus groups/interviews/consensus meetings; surveys | Colonoscopy patients-adult | Yes | 20 |
| Uphoff et al 31 | The Netherlands | 2012 | Focus groups/interviews/consensus meetings | Cancer | Yes | 21 |
| Wensing et al 20 | The Netherlands | 1996 | Focus groups/interviews/consensus meetings; surveys | Chronically ill patients (chronic obstructive pulmonary disease, diabetes, cardiovascular disease, migraine and chronic disease of locomotor system) | Yes | 41 |
| Zimmerman et al 32 | USA | 2014 | Focus groups/interviews/consensus meetings | Community-based, assisted living support patients | Yes | 43 |
| Cox and Gray44 | UK | 2014 | Guest editorial | – | – | 4 |
| Carinci et al 28 | UK | 2015 | Modified Delphi approach/consensus meeting | – | – | 12 |
| Non–peer-reviewed literature (n=8) | ||||||
| Lewis26 | Canada | 2009 | Discussion paper | – | – | 6 |
| RNAO25 | Canada | 2002 | Guidelines document/report | – | – | 18 |
| Silow-Carroll et al 45 | USA | 2006 | Report | – | – | 6 |
| Kelley and Hurst (OECD)24 | – | 2006 | Working papers | – | Yes | 7 |
| OECD27 | – | 2006 | OECD website | – | Yes | 8 |
| Essence of care – patient focused benchmarks for clinical governance (NHS)22 | UK | 2003 | Report | – | Yes | 116 |
| Davies et al 23 | UK | 2009 | Report | – | – | 10 |
| IAPO21 | – | 2012 | Literature review | – | – | 69 |
IAPO, International Alliance of Patients’ Organizations; NHS, National Health Service; OECD, Organization for Economic Co-operation and Development; PCC, patient-centred care; RNAO, Registered Nurses Association Ontario.
What PC-QIs have been developed to measure patient centred care?
From the sources included, a total of 502 ways of measuring PCC were explicitly identified as quality indicators by studies’ authors. However, only 25 were classified as actual indicators by our research team.
PCC measurement varied between articles. While all sources used the term ‘quality indicator’, not all were quantifiable and measurable. Most sources presented quality indicators as guidelines or recommendations for healthcare practitioners. Wensing et al presented indicators as survey items, such as ‘Does the GP pay attention to patients’ needs?’20 Actual indicators were presented as percentages and proportions, and identified from six grey literature sources.21–26 For instance, one study outlined an example of a structure indicator—‘percent of nurses attending education sessions (orientation, organization professional development opportunities) on client-centred care’.25
Study populations included cancer patients (n=2), colonoscopy patients (n=1), HPN patients (n=1), chronically ill (n=1), fertility care (n=1) and assisted living support patients (n=1) (table 1). For the development of PCC measures, 7 studies used focus groups, interviews and/or consensus meetings, 10 studies included patients and family caregivers in the development of PCC measures and 1 article developed measures through the authors’ clinical and research work. Two sources developed ways to measure PCC from patient-reported experience surveys,24 27 and two studies used a framework.25 28
Some studies grouped ways to measure PCC according to domains of PCC that were based on previously defined frameworks or through consensus (eg, access to care, communication and information). Domains identified from the person-centred care framework are categorised according to structure, process and outcome.18 Here table 2 presents examples of measuring PCC classified according to the person-centred care framework,18 and table 3 presents the actual indicators classified according to the same framework.18
Table 2.
Examples of patient-centred care (PCC) measurement classified according to the person-centred care framework18
| PCC measure classification | Domain | Example of ways to measure PCC |
| Structure (n=80) | Supporting a workforce committed to PCC. | |
| Providing a supportive and accommodating PCC environment. | ||
| Process (n=343) |
Cultivating communication. | |
| Respectful and compassionate care. | ||
| Outcome (n=79) |
Patient-reported outcomes. |
Table 3.
Identified PC-QIs from the literature classified according to the person-centred care framework as actual indicators18
| Type of indicator | Domain | PCC indicators (n=25) |
| Structure | Creating a PCC culture |
|
| Supporting a workforce committed to PCC | ||
| Process | Cultivating communication |
|
| Respectful and compassionate care | ||
| Engaging patients in managing their care |
|
|
| Integration of care |
|
|
| Access to care |
|
|
| Outcome | Patient-reported experiences |
|
GP, general practitioner; HER, health electronic record; NHS, National Health Service; PCC, patient-centred care; PC-QIs, patient-centred quality indicators; PHC, primary healthcare.
How are PC-QIs defined?
The definition of a PC-QI was not clearly articulated in the studies identified (table 4). Ten of the included studies provided no such definition of a quality indicator (table 4). Sources where the definition of a quality indicator was mentioned defined indicators as something to be measured, and developed through consensus (table 4).23 29–31 Of those four sources where the definition of a PC-QI was clear, two included actual indicators.21 23 The National Health Service report described indicators as ‘items that patients, carers and professionals believed were important in achieving the benchmarks of best practice’.22
Table 4.
Definition of quality indicator used by authors
| Study identifier (first author, year) | Definition of quality indicator used |
| den Breejen et al (2013),42 Sewitch et al (2013),43 Uphoff et al (2012),31 Zimmerman et al (2014),32 Cox and Gray (2015),44 Lewis (2009),26 RNAO (2002),25 Silow-Carroll et al (2006),45 Kelley and Hurst (2006),24 OECD website (2006)27 and Carinci et al (201528 | Definition not included. |
| Dreesen et al (2014)29 | A quality indicator as a measurable element of practice performance for which there is evidence or consensus that it can be used to assess the quality of care, and hence change the care provided.46 |
| Ouwens et al (2010)30 and Uphoff et al (2012)31 | Quality indicators are ‘measurable elements of practice performance for which there is evidence or consensus that they can be used to assess the quality of care’.47 |
| Davies et al (2011)23 | An explicit measurable statement of the quality of care given. Relates to a single outcome or process of medical care. Clearly defined and unambiguous.47 48 |
| NHS (2003)22 | Items that patients, caregivers and professionals believed were important in achieving the benchmarks of best practice.22 |
| IAPO (2012)21 | Can be measures of structure, process and outcome, either as generic measures relevant for all diseases, or disease-specific measures that describe quality of patient care related to a specific diagnosis.49 |
IAPO, International Alliance of Patients’ Organizations; NHS, National Health Service; OECD, Organization for Economic Cooperation and Development.
Have the existing PC-QIs been implemented and evaluated across various points-of-care settings, processes of care and at the system level to measure PCC?
None of the articles mentioned actual implementation of indicators in the settings for which they were developed. Similarly, many of the sources (15/17) did not evaluate the indicators according to any set criteria. The two studies that did evaluate indicators used two different approaches.28 30 The study by Ouwens et al assessed guidelines for psychometric characteristics and only 26 out of 56 guidelines were found to be reliable.30 The study by Carinci et al used a modified Delphi approach with expert Organization for Economic Co-operation and Development members to rate the PCC measures, using validity, reliability, relevance, actionability, international feasibility and international comparability as the criteria.28 Uphoff et al recommended using the Gol and Grimshaw model for evaluating indicators,31 while a future direction for Zimmerman et al was the evaluation of the indicators.32 The working paper by Kelley and Hurst presented criteria that can be used to select indicators.24 These included the importance of what is being measured (which includes policy importance), scientific soundness and feasibility of the measure.24
Discussion
This review specifically examined existing PC-QIs in the academic and grey literature. PCC has been increasingly adopted by many jurisdictions; however, this review revealed there to be gaps in the conceptualisation of PC-QIs. Out of the 17 articles that met the inclusion criteria, only 9 were peer reviewed, and looked at specific conditions. Additionally, the heterogeneity of the PCC literature relates to the variety of definitions on PC-QIs, and a diverse type of indicators developed for different patient population and care-settings. For instance, all included articles in the review used the term ‘indicator,’ but not all presented actual indicators as defined by the AHRQ.16
The absence of a standard definition of what a PC-QI is in the literature has posed challenges in identifying the literature sources for inclusion in this review. ‘Quality’ means different things to different people, and despite the standard definition of PCC by the Institute of Medicine,1 PCC continues to be operationalised and measured differently.33 Most sources identified in the literature did not explicitly define what a quality indicator is, which may explain the differences in approaches to indicator development. The absence of a definition for quality indicators results in inconsistencies for how an indicator should be presented and also what makes for a good indicator. Previous reviews have also found variability in quality indicator definitions, such as indicators for hip fracture patient care.34 The absence of a standard definition of PC-QIs poses concerns for standardised measurement of PCC, and for implementation of PC-QIs in healthcare settings.
In compliance with quality improvement agencies, quality councils and organisations such as the AHRQ, quality indicators should be presented as a unit of measurement—as a percentage or proportion.16 Our review revealed inconsistencies in the definition of indicators. Only few sources in the non–peer-reviewed literature included PC-QIs as quantifiable units, such as percentages, incorporating a numerator and denominator in the unit of measurement.35 Most of the identified indicators were actually domains included in PCC measures and guidelines. The lack of defined units of measurement impedes comparisons across facilities, and benchmarking, and does not allow for longitudinal evaluation and overall measurement of care that is patient-centred. Without this unit of measurement for PC-QIs, it is difficult to target specific improvements needed for PCC.
The review revealed that when incorporating the patient and caregiver perspective in quality improvement, a difficulty exists in translating perceptions and subjective experiences into standardised objective indicators. Measures of well-being are both necessary and important to incorporating a PCC model of care. The study by Carr et al suggests that perceptions of health and its meaning vary between individuals and across time, as do their experiences and expectations of healthcare.36 In order to capture various perspectives on quality care, it is vital to include patients and families. Including the patient and family perspective is necessary to ensure quality PCC.
Additionally, this review found large variances for domains to categorise approaches to measuring PCC. In an attempt to organise our findings and understand the ways of measuring PCC, we used a previously published person-centred care framework18 to classify them into healthcare quality domains. From this classification, most strategies for measuring PCC were found to relate to domains associated with healthcare processes (eg, cultivating communication). These findings are consistent with the current measurement landscape, for instance trauma indicators,37 and AHRQ PC-QIs38 which mainly assess processes and outcomes. For PCC, structures, such as policies and education programmes can provide an important basis to improve PCC practice.18 39 Structure indicators provide the necessary foundations for the assessment of process and outcome indicators, for instance through creating a PCC culture, supporting the workforce to deliver PCC and providing an accommodating environment for patients.18 In this review, structure indicators were lacking.
Finally, there is scarce evidence in the literature on how to implement indicators for PCC, and how to evaluate their implementation. PCC measurement has, to date, primarily focused on specific disease conditions and healthcare sectors. However, recent initiatives (National Health Service) reveal a more generic approach to measurement (Family and Friend Test).40 In order to create a standardised set of PC-QIs, indicators must be developed across the continuum of care. Santana and Stelfox also found a lack of implementation of indicators in care settings in their review.37 Before indicators are implemented, they must be evaluated according to standard set criteria. What constitutes as a good indicator has been outlined by health quality organisations, such as National Quality Forum. As outlined by the National Quality Forum, quality indicators should be evaluated through a set criterion including importance, scientific acceptability, feasibility, and usability and use.41 Our review did not identify any studies where such evaluations were implemented. In the development and implementation of quality indicators, the guideline set by the National Quality Forum should be adhered to.
The gaps identified in the literature for PC-QIs provide directions for future research. First, there needs to be consensus on a standard definition of PC-QI to guide future measurement of PCC. Second, there is a need to develop a standard set of PC-QIs that could be implemented in various healthcare settings. Third, PC-QIs need to be evaluated according to a set criteria. Finally, PC-QIs need to be implemented across healthcare settings for monitoring and evaluation of PCC.
Strengths and limitations
Our scoping review used robust and transparent methods guided by a protocol previously published,13 and supported by a research librarian with expertise in knowledge synthesis and scoping reviews (DLL). We worked closely with our patient research partner (SZ) in the study design, research questions, search strategy and manuscript preparation.
This review may not have identified all relevant sources in the published and grey literature as we conducted the search using only English terms. As we are following the scoping review methodology, the quality of the studies was not assessed.
Conclusions
In summary, our review is the first to examine the literature pertaining to quality indicators that are patient-centric. Our findings will further the development of validated healthcare tools assessing healthcare quality from a patient-centred approach. Future research should focus on developing and refining PC-QIs that are ready to implement and evaluate following the criteria set forth by the National Quality Forum.41
Supplementary Material
Acknowledgments
We would like to acknowledge the contributions of Lisa Goodman, who provided support for the grey literature search for this scoping review.
Footnotes
Patient consent for publication: Not required.
Contributors: M-JS conceived the study, and all authors identified key literature to be included in the review. M-JS led the drafting of the manuscript and key discussion points with support from DL, RJJ, SA, ML and KM. SA managed the design of the tables (with feedback from all authors), and management of references. All authors provided important intellectual contribution and guidance throughout the development of the manuscript. HQ, DL, SZ and ML provided guidance on the presentation of the findings and guidance on final revisions. All of the authors contributed to critical review and revisions to the manuscript, agreeing on the final version.
Funding: M-JS secured funding from the M.S.I Foundation (Grant #886) based in Alberta, Canada. ML acknowledges the support from the Alberta’s Strategy for Patient Oriented Research (SPOR).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data available.
References
- 1. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century: National Academy Press, 2001. [PubMed] [Google Scholar]
- 2. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570 10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. Fam Pract 2000;49:796–804. [PubMed] [Google Scholar]
- 4. Fung CH, Lim Y-W, Mattke S, et al. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med 2008;148:111–23. 10.7326/0003-4819-148-2-200801150-00006 [DOI] [PubMed] [Google Scholar]
- 5. Epstein RM, Fiscella K, Lesser CS, et al. Why the nation needs a policy push on patient-centered health care. Health Aff 2010;29:1489–95. 10.1377/hlthaff.2009.0888 [DOI] [PubMed] [Google Scholar]
- 6. Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med 2011;24:229–39. 10.3122/jabfm.2011.03.100170 [DOI] [PubMed] [Google Scholar]
- 7. Delaney LJ. Patient-centred care as an approach to improving health care in Australia. Collegian 2017;25:119 123. [Google Scholar]
- 8. Fix GM, VanDeusen Lukas C, Bolton RE, et al. Patient-centred care is a way of doing things: How healthcare employees conceptualize patient-centred care. Health Expect 2018;21:300–7. 10.1111/hex.12615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12:CD003267 10.1002/14651858.CD003267.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Braithwaite J, Hibbert P, Blakely B, et al. Health system frameworks and performance indicators in eight countries: a comparative international analysis. SAGE Open Med 2017;5:20 10.1177/2050312116686516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agency for Healthcare Research and Quality. Quality indicator measure development, implementation, maintenance, and retirement. Rockville, MD: Agency for Healthcare Research and Quality: Center for Health Policy Center for Primary Care and Outcomes Research & Battelle Memorial Institute, 2011. [Google Scholar]
- 12. Hughes RG. Tools and strategies for quality improvement and patient safety. 2008. [PubMed]
- 13. Jolley RJ, Lorenzetti DL, Manalili K, et al. Protocol for a scoping review study to identify and classify patient-centred quality indicators. BMJ Open 2017;7:e013632 10.1136/bmjopen-2016-013632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 15. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Agency for Healthcare Research and Quality. Quality Improvement and monitoring at your fingertips. Secondary Quality Improvement and monitoring at your fingertips. https://www.qualityindicators.ahrq.gov/ (Accessed 01 Oct 2017).
- 17. Synthesis. Secondary Synthesis. 2016. http://synthesis.info/ (Accessed 01 Oct 2017).
- 18. Santana MJ, Manalili K, Jolley RJ, et al. How to practice person-centred care: a conceptual framework. Health Expect 2018;21 10.1111/hex.12640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Donabedian A. Quality assessment and monitoring. Retrospect and prospect. Eval Health Prof 1983;6:363–75. 10.1177/016327878300600309 [DOI] [PubMed] [Google Scholar]
- 20. Wensing M, Grol R, van Montfort P, et al. Indicators of the quality of general practice care of patients with chronic illness: a step towards the real involvement of patients in the assessment of the quality of care. Qual Health Care 1996;5:73–80. 10.1136/qshc.5.2.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. International Alliance of Patients’ Organizations(IAPO). Patient-centred healthcare indicators review. 2012. http://iapo.org.uk/sites/default/files/files/IAPO%20Patient-Centred%20Healthcare%20Indicators%20Review.pdf.
- 22. NHS Dignity Care. Essence of Care Patient-focused benchmarks for clinical governance 2003. https://www.dignityincare.org.uk/_assets/Resources/Dignity/OtherOrganisation/Essence_of_Care.pdf. [Google Scholar]
- 23. Davies P, Wye L, Horrocks S, et al. Developing quality indicators for community services: the case of district nursing. Qual Prim Care 2011;19:155. [PubMed] [Google Scholar]
- 24. Kelley E, Hurst J. Health care quality indicators project. OECD HEALTH WORKING PAPERS NO. 23 2006. https://www.oecd.org/els/health-systems/36262363.pdf. [Google Scholar]
- 25. Registered Nurses Association of Ontario. Client centred care. Toronto, Ontario, 2002. [Google Scholar]
- 26. Lewis S. Patient-centered care: an introduction to what it is and how to achieve it. Saskatchewan: Ministry of Health, 2009. [Google Scholar]
- 27. OECD. Health care quality indicators - responsiveness and patient experiences. Secondary health care quality indicators - responsiveness and patient experiences. 2006. http://www.oecd.org/els/health-systems/hcqi-responsiveness-and-patient-experiences.htm (Accessed 01 Oct 2017).
- 28. Carinci F, Van Gool K, Mainz J, et al. Towards actionable international comparisons of health system performance: expert revision of the OECD framework and quality indicators. Int J Qual Health Care 2015;27:137–46. 10.1093/intqhc/mzv004 [DOI] [PubMed] [Google Scholar]
- 29. Dreesen M, Foulon V, Vanhaecht K, et al. Identifying patient-centered quality indicators for the care of adult home parenteral nutrition (HPN) patients. JPEN J Parenter Enteral Nutr 2014;38:840–6. 10.1177/0148607113495891 [DOI] [PubMed] [Google Scholar]
- 30. Ouwens M, Hermens R, Hulscher M, et al. Development of indicators for patient-centred cancer care. Support Care Cancer 2010;18:121–30. 10.1007/s00520-009-0638-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Uphoff EP, Wennekes L, Punt CJ, et al. Development of generic quality indicators for patient-centered cancer care by using a RAND modified Delphi method. Cancer Nurs 2012;35:29–37. 10.1097/NCC.0b013e318210e3a2 [DOI] [PubMed] [Google Scholar]
- 32. Zimmerman S, Love K, Cohen LW, et al. Person-centeredness in home- and community-based services and supports: domains, attributes, and assisted living indicators. Clin Gerontol 2014;37:429–45. 10.1080/07317115.2014.937548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med 2005;61:1516–28. 10.1016/j.socscimed.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 34. Pitzul KB, Munce SE, Perrier L, et al. Scoping review of potential quality indicators for hip fracture patient care. BMJ Open 2017;7:e014769 10.1136/bmjopen-2016-014769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hermann RC, Mattke S, Somekh D, et al. Quality indicators for international benchmarking of mental health care. Int J Qual Health Care 2006;18:31–8. 10.1093/intqhc/mzl025 [DOI] [PubMed] [Google Scholar]
- 36. Carr AJ, Gibson B, Robinson PG. Measuring quality of life: Is quality of life determined by expectations or experience? BMJ 2001;322:1240–3. 10.1136/bmj.322.7296.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Santana MJ, Stelfox HT. Quality indicators used by trauma centers for performance measurement. J Trauma Acute Care Surg 2012;72:1298–303. 10.1097/TA.0b013e318246584c [DOI] [PubMed] [Google Scholar]
- 38. Agency for Healthcare Research and Quality. Pediatric quality indicators overview. secondary pediatric quality indicators overview 2017. https://www.qualityindicators.ahrq.gov/modules/pdi_resources.aspx (Accessed 01 Oct 2017).
- 39. The Lewin Group. Indicators of cultural competence in health care delivery organizations: an organizational cultural competence assessment profile. 2002. https://www.hrsa.gov/sites
- 40. National Health Services UK. Friends and family test 2017. https://www.england.nhs.uk/fft/ (accessed 20 Dec 2017).
- 41. National Quality Forum. Measure evaluation criteria. Secondary measure evaluation criteria. http://www.qualityforum.org/Measuring_Performance/Submitting_Standards/Measure_Evaluation_Criteria.aspx (Accessed 01 Oct 2017).
- 42. den Breejen EM, Nelen WL, Schol SF, et al. Development of guideline-based indicators for patient-centredness in fertility care: what patients add. Hum Reprod 2013;28:987–96. 10.1093/humrep/det010 [DOI] [PubMed] [Google Scholar]
- 43. Sewitch MJ, Dubé C, Brien S, et al. Patient-identified quality indicators for colonoscopy services. Can J Gastroenterol 2013;27:25–32. 10.1155/2013/574956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cox J, Gray A. NHS at the hustings: four quality indicators for a person centred medicine. Eur J Pers Cent Healthc 2015;3:1–3. 10.5750/ejpch.v3i1.999 [DOI] [Google Scholar]
- 45. Silow-Carroll S, Alteras T, Stepnick L. Patient-centered care for underserved populations: definition and best practices. Washington, DC: Economic and Social Research Institute, 2006. [Google Scholar]
- 46. Lawrence M, Olesen F. Indicators of quality in health care. Eur J Gen Pract 1997;3:103–8. 10.3109/13814789709160336 [DOI] [Google Scholar]
- 47. Campbell SM, Braspenning J, Hutchinson A, et al. Research methods used in developing and applying quality indicators in primary care. Qual Saf Health Care 2002;11:358–64. 10.1136/qhc.11.4.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pencheon D. The good indicators guide: understanding how to use and choose indicators: NHS Institute for Innovation and Improvement, 2008. [Google Scholar]
- 49. Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 2003;15:523–30. 10.1093/intqhc/mzg081 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-023596supp001.pdf (80.1KB, pdf)
bmjopen-2018-023596supp002.pdf (165.3KB, pdf)