Abstract
Synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome was first described as chronic recurrent multifocal osteomyelitis. Because of its rarity, a thorough description of its clinical manifestations is lacking. Herein, we describe the clinical manifestations and imaging features, especially the enthesopathy in bilateral Achilles tendons, of a middle-aged Asian woman with SAPHO syndrome, who improved after diclofenac treatment.
Keywords: musculoskeletal syndromes, radiology (diagnostics), musculoskeletal and joint disorders
Background
Synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome was known as chronic recurrent multifocal osteomyelitis (CRMO) from 1972 until the term ‘SAPHO’ was coined in 1987.1 2 This acronym is an attempt to include various names that have been used in the literature for the last 45 years to describe the aforementioned clinical presentations. These terms include ‘bilateral clavicular osteomyelitis with palmar and plantar pustulosis’, ‘intersternocostoclavicular ossification’, ‘arthro-osteitis with follicular occlusion’, ‘subacute and chronic symmetric osteomyelitis’, ‘sternoclavicular hyperostosis’, ‘sterile osteitis’, ‘pustulotic arthro-osteitis’, ‘CRMO’, ‘Koehler’s disease’, ‘pyogenic sterile arthritis’, ‘acquired hyperostosis syndrome’ and ‘spondyloarthritis hyperostotica pustulo-psoriatica’.3–7 We report a female patient with symptoms that had persisted for 5 years but which were rapidly recognised and successfully treated on our first encounter.
Case presentation
A 59-year-old woman experienced chronic pain initially in the right clavicle and eventually in both clavicles for 5 years, accompanied by morning stiffness in both hands with tenderness but no fever. In addition, the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints were swollen, suggesting joint effusion, and onycholysis was noted in both hands as well as pustulosis in the right foot. After a series of laboratory examinations, chronic osteomyelitis was suspected and oral empirical dicloxacillin was administered for 4 weeks; however, this failed to control the pain. Subsequently, 75 mg of diclofenac in a sustained-release tablet was administered daily, which completely alleviated the pain within 2 weeks.
Investigations
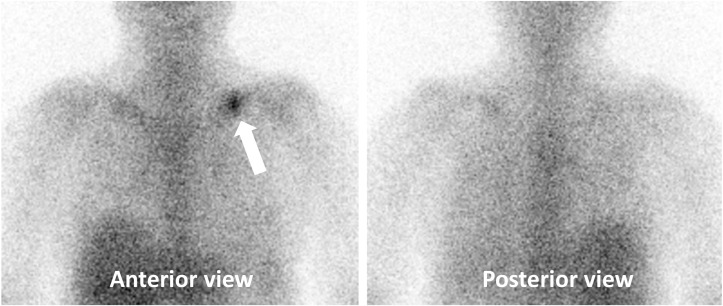
Peripheral venous blood analysis revealed that the white cell count, C reactive protein and erythrocyte sedimentation rate were all normal. Musculoskeletal ultrasound demonstrated polyarticular effusion in the MCP and PIP joints. A whole-body bone scan (figure 1) revealed multifocal uptake in the clavicles and bony reaction in the sternal xiphoid process. A Gallium (Ga)-67 three phase bone scan.
Figure 1.

Whole-body bone scan showing increased uptake in both clavicles (more prominent on the left, arrow) and bone reaction in both clavicles as well as the sternum (xiphoid side, arrowhead).
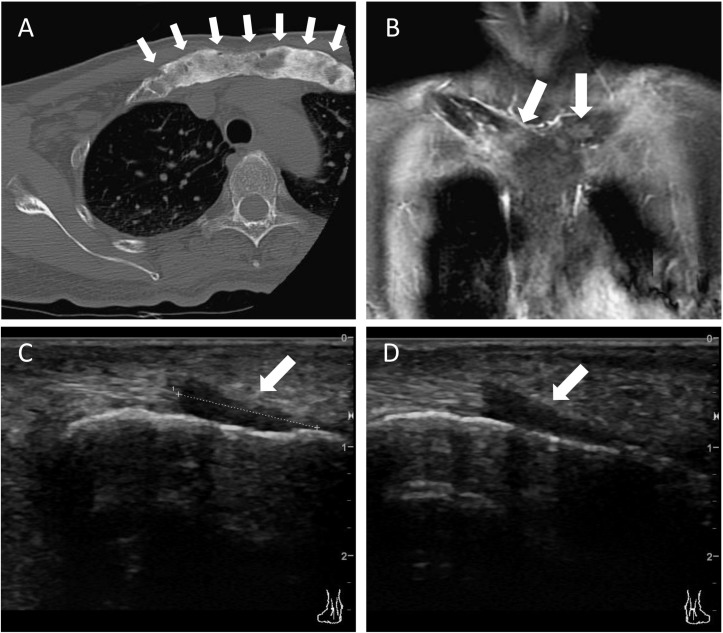
Figure 2 showed increased blood pooling in the middle of the left clavicle shaft, suggesting osteomyelitis. Computed tomography (CT), magnetic resonance imaginf (MRI) and follow-up ultrasound demonstrated osteitis and hyperostosis in the clavicles and sternum, and a unique feature of enthesopathy in both Achilles tendons (figure 3).
Figure 2.
Ga-67 three-phase bone scan showing increased blood pooling in the middle of the left clavicle shaft (arrow, anterior view), suggesting osteomyelitis.
Figure 3.
(A) CT image of the bone window showing osteoblastic change with solid periosteal reaction (arrows) in the proximal clavicles and hyperostosis in the anterior sternoclavicular (SC), costoclavicular and left second chondrosternal joints in the transverse view; (B) Gadolinium-enhanced T1-weighted MRI showing multifocal osteomyelitis in the bilateral clavicles, arthritis in the SC joints, sclerotic or osteoblastic change in the clavicles, solid periosteal reaction in the proximal clavicles, and hyperostosis in the coronal view (arrows), suggesting synovitis, acne, pustulosis, hyperostosis and osteitis syndrome; (C) (right ankle), (D) (left ankle): Sonography image showing hypoechogenicity and loss of the fibrillar structure of the Achilles tendon at the insertion site over the calcaneus, indicating enthesopathy of both feet (arrow).
Differential diagnosis
Differential diagnoses included osteosarcoma and chronic infectious osteomyelitis. However, a series of imaging studies before and after empirical antibiotic therapy virtually excluded both. Although we found no acne, the laboratory data and clinical manifestations were more indicative of classic multifocal sterile chronic osteomyelitis or SAPHO.
Treatment
After the failure of dicloxacillin treatment, a series of examinations including CT, MRI and ultrasound suggested a non-infectious origin of chronic inflammation in the joints and bones. Hence, 75 mg of diclofenac was orally administered daily, which soon alleviated all symptoms within 2 weeks.
Outcome and follow-up
The symptoms did not recur within almost 2 years of follow-up at an outpatient clinic. However, the patient was lost to follow-up thereafter.
Discussion
In this patient, after 1 month of antibiotic treatment, a whole-body bone scan still showed increased uptake in the bilateral clavicles, indicating that the condition was refractory to antibiotics. However, all symptoms were markedly relieved by the subsequent use of an oral non-steroidal antirheumatic drug (diclofenac). This led us to suspect a non-infectious or autonomic inflammatory disease. SAPHO syndrome, which has rarely been encountered since it was first reported approximately 45 years ago,2 fulfilled the characteristic of a non-infectious inflammatory disease in our patient and was thus taken into consideration in our diagnosis. Imaging studies such as three-phase whole-body bone scans and MRI can help earlier diagnose,3 6 as in the present case. CRMO is a paediatric mimic of SAPHO, which is characterised by limb inflammation. Our patient presented with CRMO in the clavicles rather than the peripheral joints or bones, suggesting that the idiopathic inflammatory reaction may occur anywhere in the body. The reason for the predilection for peripheral joints or bones in younger patients may be that the musculoskeletal system is in a growing and proliferative stage at these ages and tends to be invaded by idiopathic or acquired proinflammatory stimuli. The axial skeleton and costosternoclavicular bone are more often involved in adult patients with SAPHO than in paediatric patients.8 The sternoclavicular joints were affected in our patient, which is compatible with previous reports.
The other feature that should be mentioned is that enthesopathy was found in the bilateral Achilles tendons in this patient. The presence of enthesopathy in patients with SAPHO syndrome has been reported only in limited studies. In a study by Queiro et al, ultrasound revealed various degrees of enthesis involvement in 7 of 15 patients with SAPHO syndrome, most of whom were asymptomatic.9 Okuno et al reported the radiographic findings of 67 patients with SAPHO syndrome, 10 of whom (13.4%) were found to have enthesopathy.10 The presence of enthesopathy might be underestimated in patients with SAPHO syndrome, and musculoskeletal ultrasound could be a sensitive and highly accessible modality to detect this pathological feature. Because enthesopathy is well recognised in patients with spondyloarthropathy, some experts have suggested that SAPHO syndrome might be a form of spondyloarthropathy. Recent studies have also found increased Th17 cells in the peripheral blood of patients with SAPHO syndrome,11 and IL-17, IL-8, tumour necrosis factor-α (TNF-α) might be involved in the pathogenesis of the disease.12 The disease seems to be driven by innate immunity, sharing some characteristics with spondyloarthropathy but lacking similar genetic factors.12
Non-steroidal anti-inflammatory drugs and conventional disease-modifying antirheumatic drugs are commonly used for the treatment of SAPHO syndrome, and treatment responses vary. Biologics, including anti-TNF-α, anti-IL-1, anti-IL-6 and anti-IL-17/23, are emerging as potential treatment options for patients with refractory disease.13 SAPHO syndrome should always be considered in the differential diagnosis of chronic refractory osteomyelitis.
Learning points.
Although rare, synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome should always be considered as a differential diagnosis for patients with symptoms compatible with osteomyelitis refractory to antibiotics.
Enthesopathy might be an underestimated feature of SAPHO syndrome, presenting in 13.4%–46.7% of these patients.
A three-phase whole-body bone scan and MRI are common diagnostic modalities for SAPHO syndrome. Musculoskeletal ultrasound is another sensitive tool for detecting synovitis and enthesopathy.
Footnotes
C-FS and Y-CS contributed equally.
Contributors: C-FS rewrote this manuscript and Y-CS prepared these materials. H-TL provided the pertinent clinical and laboratory data and C-YT supervised the whole study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
References
- 1. Chamot AM, Benhamou CL, Kahn MF, et al. [Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases]. Rev Rhum Mal Osteoartic 1987;54:187–96. [PubMed] [Google Scholar]
- 2. Giedion A, Holthusen W, Masel LF, et al. [Subacute and chronic "symmetrical" osteomyelitis]. Ann Radiol 1972;15:329–42. [PubMed] [Google Scholar]
- 3. Rukavina I. SAPHO syndrome: a review. J Child Orthop 2015;9:19–27. 10.1007/s11832-014-0627-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kerrison C, Davidson JE, Cleary AG, et al. Pamidronate in the treatment of childhood SAPHO syndrome. Rheumatology 2004;43:1246–51. 10.1093/rheumatology/keh295 [DOI] [PubMed] [Google Scholar]
- 5. Assmann G, Simon P. The SAPHO syndrome--are microbes involved? Best Pract Res Clin Rheumatol 2011;25:423–34. 10.1016/j.berh.2011.01.017 [DOI] [PubMed] [Google Scholar]
- 6. Matzaroglou C, Velissaris D, Karageorgos A, et al. SAPHO Syndrome Diagnosis and Treatment: Report of Five Cases and Review of the Literature. Open Orthop J 2009;3:100–6. 10.2174/1874325000903010100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khanna L, El-Khoury GY. SAPHO syndrome--a pictorial assay. Iowa Orthop J 2012;32:189–95. [PMC free article] [PubMed] [Google Scholar]
- 8. Björkstén B, Gustavson KH, Eriksson B, et al. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. J Pediatr 1978;93:227–31. 10.1016/S0022-3476(78)80501-0 [DOI] [PubMed] [Google Scholar]
- 9. Queiro R, Alonso S, Alperi M, et al. Entheseal ultrasound abnormalities in patients with SAPHO syndrome. Clin Rheumatol 2012;31:913–9. 10.1007/s10067-012-1959-7 [DOI] [PubMed] [Google Scholar]
- 10. Okuno H, Watanuki M, Kuwahara Y, et al. Clinical features and radiological findings of 67 patients with SAPHO syndrome. Mod Rheumatol 2018;28:703–8. 10.1080/14397595.2017.1372874 [DOI] [PubMed] [Google Scholar]
- 11. Firinu D, Barca MP, Lorrai MM, et al. TH17 cells are increased in the peripheral blood of patients with SAPHO syndrome. Autoimmunity 2014;47:389–94. 10.3109/08916934.2014.906582 [DOI] [PubMed] [Google Scholar]
- 12. Cianci F, Zoli A, Gremese E, et al. Clinical heterogeneity of SAPHO syndrome: challenging diagnose and treatment. Clin Rheumatol 2017;36:2151–8. 10.1007/s10067-017-3751-1 [DOI] [PubMed] [Google Scholar]
- 13. Daoussis D, Konstantopoulou G, Kraniotis P, et al. Biologics in SAPHO syndrome: A systematic review. Semin Arthritis Rheum 2018. Epub ahead of print 10.1016/j.semarthrit.2018.04.003 [DOI] [PubMed] [Google Scholar]