Abstract
A 60-year-old woman presented with pulsatile tinnitus in the left ear. MRI and CT imaging suggested a soft-tissue mass in the middle ear. Exploratory tympanotomy and biopsy confirmed Schneiderian (inverted) papilloma. Endoscopic and radiological assessment showed no evidence of sinonasal lesions. The patient proceeded to mastoid surgery with removal of the ossicles for disease clearance. The small number of cases published to date of isolated middle ear inverted papilloma suggest a high recurrence and malignant transformation rate and aggressive management is therefore warranted.
Keywords: ear, nose and throat/otolaryngology; otolaryngology/ent
Background
This is only the 15th case ever reported in the literature of Schneiderian papilloma occurring purely with the tympanomastoid/middle ear cleft. The literature to date suggests a high rate of malignant transformation and aggressive surgical clearance of the lesion is therefore warranted.
Case presentation
A 60-year-old woman clerical worker presented to the otolaryngology department with pulsatile tinnitus and hearing loss in the left ear. There was no history of otorrhoea, otalgia or vertigo and she had no history of otological disease or surgery. Her medical history was significant only for pulmonary sarcoidosis some 20 years previously which had been quiescent for many years.
Otoscopy revealed an intact tympanic membrane on the left side with a pink fleshy appearance suggestive of a middle ear lesion. The contralateral ear was unremarkable. Facial power was normal bilaterally. The remainder of the clinical examination of the head and neck, including nasendoscopy, was normal. Audiogram showed a 40 dB conductive hearing loss in the affected left ear and normal contralateral hearing.
Investigations
Given the suspicion of a middle ear mass lesion, the patient underwent CT scanning of the temporal bones in the first instance (figure 1). This showed a soft-tissue density lesion of the middle ear cleft with no evidence of bony erosion of the fallopian canal, tegmen tympani or lateral semicircular canal. Subsequent contrast-enhanced MRI scanning showed mild enhancement with gadolinium and moderate T2 signal intensity (figure 2).
Figure 1.
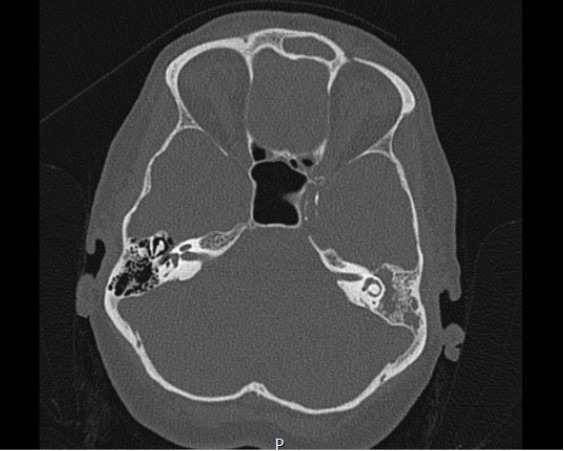
Axial CT scan of temporal bones showing confluent soft-tissue density opacification of the mastoid air cells with preservation of the lateral semicircular canal.
Figure 2.
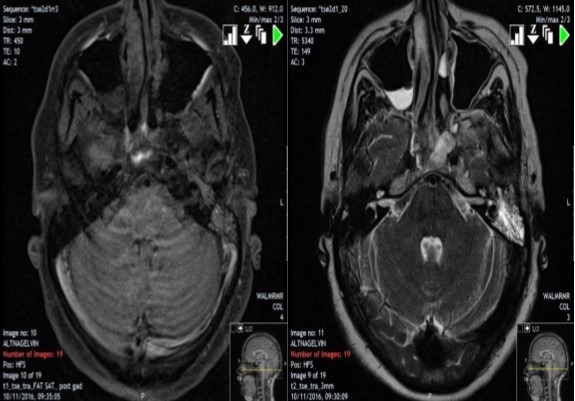
L: Postgadolinium T1 axial MRI scan of temporal bones showing mild enhancement with gadolinium. R: T2 axial MRI scan of temporal bones showing moderate signal intensity.
Exploratory tympanotomy revealed a fleshy lesion in the middle ear surrounding the ossicles. Histopathological analysis showed inverted papilloma (IP) (figure 3).
Figure 3.
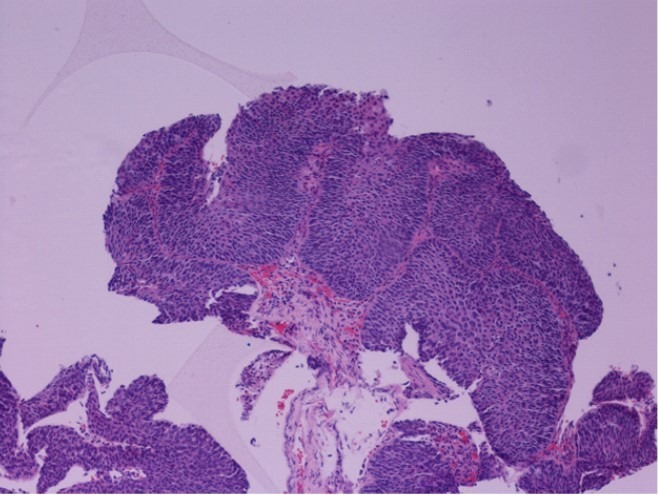
H&E staining of biopsy from middle ear showing transitional type epithelium with no evidence of cytological atypia.
Treatment
The patient proceeded to left mastoid exploration. A posterior tympanomeatal flap was elevated via a postauricular incision. The incudostapedial joint was found to be deficient at the lenticular process with the tumour encasing the ossicular chain; as such the incus and malleus head were removed to facilitate disease clearance. Tumour was removed in a piecemeal fashion from the middle ear cleft. Initially, a front-to-back atticotomy approach was taken, but it was evident there was significant disease extension posteriorly into the mastoid system. A cortical mastoidectomy was therefore performed and all gross disease cleared from the mastoid air cells and antrum. The bony coverings of the horizontal semicircular canal and tegmen tympani were thinned but intact. Disease was also cleared from infra cochlear cells and the eustachian tube orifice. Tensor tympani tendon was divided to allow visualisation of the medial surface of the tympanic membrane which was seen to be clear of macroscopic disease. Endoscopic assessment was carried out using both 0° and 30° endoscopes. Potassium titanyl phosphate (KTP) laser at a setting of 1.5 W was used to any areas of dubious clearance, except for a small area in around the stapes footplate where a lower setting of 1.0 W was used. A second look procedure at 3 months showed some recurrent/residual disease around the eustachian tube orifice which was again addressed using KTP laser. At the time of writing, the patient is awaiting a third look procedure.
Outcome and follow-up
The patient will be closely followed up at regular outpatient visits with serial MRI scanning to assess for disease recurrence and/or malignant transformation.
Discussion
IP—also known as Schneiderian cell papilloma or transitional cell papilloma—is a rare benign epithelial tumour most commonly arising in the sinonasal cavities. The most common site is the lateral nasal wall and middle meatus. The lesion is characterised by ingrowth of the neoplastic epithelium into the underlying stroma with human papilloma virus types 6 and 11 thought to play some role in the pathogenesis.1 Inadequate surgery can lead to high rates of recurrence and there exists a risk of malignant transformation. It is thought to comprise around 0.4%–4% of all primary nasal neoplasms.2
Primary IP of the middle ear—in the absence of a previous or concurrent sinonasal lesion—is extremely rare. This is the 15th case ever reported in the literature. Clearly the potential exists for the direct spread of a primary sinonasal lesion into the middle ear via the eustachian tube. Isolated, primary middle ear IP however may be due to an embryological inclusion phenomenon whereby part of the Schneiderian membrane (an ectodermal structure) becomes entrapped into the middle ear mucosa (endodermal). The data published to date suggest that these lesions display higher rates of recurrence and malignant transformation than lesions in the sinonasal tract. Aggressive surgery is therefore required. Of the 14 cases of primary middle ear IP published to date, a simple tympanotomy and excision (three reported cases) was associated with 100% recurrence rates, whereas more extensive mastoidectomy and/or temporal bone resection approaches reduced the recurrence rate to 39%.3 This remains higher than published recurrence rates reported in large series of sinonasal IP disease of around 15%.4
Learning points.
Primary Schneiderian (inverted) papilloma of the middle ear cleft is an extremely rare entity.
Patients may present with hearing loss (usually conductive) and tinnitus which may be pulsatile.
Rates of recurrence and malignant transformation are significantly higher than in the more usual sinonasal lesions and aggressive surgical clearance is therefore required.
Footnotes
Contributors: The lead author MA wrote the main body of the article. CS and SH contributed to the discussion and literature review.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Browning GG, Burton MJ, Clarke R, et al. Head & Neck Surgery. 7th Ed London: Edward Arnold, 2008:209. [Google Scholar]
- 2. Brors D, Draf W. The treatment of inverted papilloma. Curr Opin Otolaryngol Head Neck Surg 1999;7:33–8. 10.1097/00020840-199902000-00008 [DOI] [Google Scholar]
- 3. Schaefer N, Chong J, Griffin A, et al. Schneiderian-type papilloma of the middle ear: A review of the literature. Int Surg 2015;100:989–93. 10.9738/INTSURG-D-14-00242.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Woodworth BA, Bhargave GA, Palmer JN, et al. Clinical outcomes of endoscopic and endoscopic-assisted resection of inverted papillomas: a 15-year experience. Am J Rhinol 2007;21:591–600. 10.2500/ajr.2007.21.3086 [DOI] [PubMed] [Google Scholar]


