Abstract
Introduction
There is a lack of research into the perspectives of patients, parents, and clinicians regarding strategies for vaccine-related pain and syncope prevention that may improve the adolescent vaccination experience and encourage future vaccination.
Objective
To develop an intervention on the basis of preference for strategies to reduce pain and prevent syncope associated with adolescent vaccination.
Methods
We conducted focus groups and interviews with 8 recently vaccinated Kaiser Permanente Northwest (KPNW) members aged 11 to 17 years and their parents to explore perceptions of pain and syncope after vaccination as well as receptivity to potential interventions. Additionally, we interviewed 7 clinical staff who routinely vaccinate children. We conducted content analysis to identify promising interventions and conducted a data synthesis workshop to select a final intervention for piloting.
Results
All participants expressed willingness to use previsit education, breathing exercises, social support or distraction, and water consumption. Patients and parents expressed a need for verbal education and messaging about potential vaccine-related outcomes, and clinicians noted a need to identify patients who are anxious before a vaccination visit. Most participants suggested a “comfort menu” intervention, to include comfort and distraction items that medical staff offer adolescents before and during vaccination.
Conclusion
Patients, parents, and clinicians acknowledged the value of interventions to reduce pain and syncope after adolescent vaccination. Stakeholders identified a comfort menu as the intervention to be piloted at 2 KPNW pediatric clinics. Further research is needed to test the effectiveness of the “Vaccination Comfort Menu” intervention in improving vaccination experiences and continued receipt of vaccinations.
Keywords: adolescent medicine, adolescent vaccination, adverse effects, prevention, qualitative research, vaccination, vaccination comfort menu
INTRODUCTION
The Centers for Disease Control and Prevention currently recommends several vaccinations for adolescents, including meningococcal conjugate vaccine; tetanus, diphtheria, and acellular pertussis vaccine; HPV; and influenza vaccine.1,2 Although these vaccines are safe and effective, their administration may result in acute pain at the injection site, dizziness, and, rarely, syncope (fainting) among preteen and teen patients.3–5 In fact, syncope after vaccination is thought to occur approximately 1 time per 1000 doses administered among adolescents and young adults.6,7 These vaccine reactions may serve as barriers to vaccine initiation and completion of recommended vaccination schedules.8,9
A variety of interventions are recommended to prevent the acute pain associated with vaccination in infants and young children.10–22 However, there is limited research about pain or syncope prevention strategies among adolescents or the perspectives of patients, parents, and clinicians regarding the management of pain and syncope after vaccination or strategies that might improve the vaccination experience and support future receipt of vaccinations.19,23
We sought to fill this knowledge gap by gathering qualitative feedback about strategies to prevent vaccination-related pain and syncope from recently vaccinated adolescent patients and their parents and from clinicians who administer adolescent vaccinations. Our study led to the development of an intervention to be piloted in pediatric clinics.
METHODS
Study Setting, Participants, and Recruitment
We collected information from recently vaccinated patients age 11 to 17 years and their parents between December 2015 and April 2016. We used electronic health record (EHR) data to identify youth who were vaccinated in the previous 12 months at Kaiser Permanente Northwest (KPNW), an integrated health care delivery system in Oregon and Washington. We used a purposeful sampling method to identify a sample of individuals for recruitment to focus groups and interviews. We attempted to prioritize the recruitment of patients who had evidence of pain or syncope after a vaccination. However, on identifying few patients who met that criterion, we preferentially recruited patients with the most recent vaccination visit to increase the likelihood that they would recall specific aspects of their vaccination experience, including possible pain or syncope.24 We sent 181 recruitment letters to the parents of recently vaccinated patients, with the goal of recruiting 12 to 16 participants. We followed these letters with telephone calls. Participants received compensation (two $15 gift cards to a local store for each family) and provided written informed consent before data collection.
We also generated a list of 20 pediatric clinic staff known to our research team or referred by other clinicians, with the intent of interviewing 12 clinical staff. Recruitment efforts focused on those who provide patient care during vaccination (eg, physicians, medical assistants, and nurse practitioners), would be involved in or affected by an intervention, or had participated in prior vaccination-related research at KPNW. Clinicians gave verbal consent and were not compensated for participation.
Data Collection and Analysis
Focus Groups and Interviews
Trained qualitative methodologists (JS and AF) and 2 trained interviewers conducted the focus groups and interviews. We developed a patient-parent focus group and interview guide and a clinician interview guide using the expertise of the study team, literature review, and clinician input. The guides are available as supplemental materials on request. In addition to the guide, we presented all participants with documentation of interventions that are currently recommended for the management of acute pain after vaccination (Table 1).19,23,25 Because there is limited evidence around strategies specifically tailored to the reduction of syncope related to vaccination, we included strategies recommended for the prevention of syncope related to blood donation (Table 1).22, 26–35 We believe that this approach was appropriate because of the common occurrence of a vasovagal response—or syncope—following medical procedures, including vaccination and blood donation.36
Table 1.
Recommended interventions to reduce injection-site pain or prevent syncope associated with preteen and teen vaccinationa
| Technique | Description |
|---|---|
| Pain reduction19,23,25 | |
| Preparation | In advance, give the patient an information sheet that discusses the steps of the vaccination procedures and what to expect |
| Breathing exercises | Tell the patient to take slow breaths and focus on deep breathing from the diaphragm rather than the chest (eg, pretend to inflate or deflate a tire through inhaling/exhaling) |
| Distraction techniques | Use techniques that take attention away from pain to specific counteractivities |
| Order of injections | When 2 vaccines are being given during the same visit, administer the vaccine associated with the most injection-site pain last |
| Positioning | Ask the patient to sit upright or stand against the examination table during vaccination |
| Rapid injection of vaccine | Give vaccination quickly |
| Tactile stimulation | Rub or stroke the arm near the injection site before and during vaccine injections |
| Topical anesthetic agents | Apply a topical agent containing pain reliever on the skin where the vaccine will be injected ahead of time (up to 1 hour ahead at home or on arrival to the appointment) |
| Syncope prevention | |
| Patient education32 | Before visit: Provide an educational brochure about ways to prepare for the visit and prevent potential symptoms of faintness or dizziness During visit: Ask about history of fainting with medical procedures; discuss concerns and how to prevent future reactions |
| Water consumption28,29,31–33 | Tell the patient to drink 500 mL (approximately 16 oz) of water 30 min before vaccination |
| Sodium consumption32,33 | Suggest that the patient eat salty food or take a salt tablet (sodium chloride) before vaccination |
| Caffeine consumption26 | Recommend consuming 250 mg of caffeine (equivalent to about 2.5 cups of coffee) 45 min to 1 h before vaccination |
| Applied muscle tension22,28,32–34 | Examples include the patient gripping and contracting a rubber ball with the hand of the nonvaccinated side, tensing of the nonvaccinated arm, or leg crossing/tensing |
| Reclining during and after vaccination | Advise the patient to sit or lie down while the shot is given and for 15–20 min after |
| Social support30 | Have a medical assistant, parent, or friend provide encouragement and reassurance and make small talk during the vaccination |
This list was developed using a literature review that identified interventions used to reduce pain and syncope among children during vaccination and among blood donors. Interventions were included if they were contained in the scientific literature, although the size of the effect of the intervention on outcomes was not considered.
The patient-parent focus groups lasted from 90 minutes to 120 minutes, and interviews lasted approximately 1 hour. Both focus groups and interviews emphasized the adolescent perspective but also incorporated parent feedback related to vaccination experiences and thoughts about potential approaches to preventing or reducing negative reactions to vaccination. The clinician interviews lasted roughly 30 minutes to 45 minutes and sought feedback about the occurrence of adverse reactions to vaccinations among adolescent patients; approaches clinicians currently take to help prevent these adverse reactions; and the recommended strategies to prevent adverse reactions to adolescent vaccinations. We also asked clinicians about the acceptability and feasibility of implementing strategies in the real-world clinical setting. All sessions were audiorecorded and transcribed. Interviewers also took detailed notes.
Our qualitative research was focused on the quality of participant responses and the development of our intervention rather than theme saturation or the generation of theoretical constructs. Thus, we sought to explore participant experiences and reach a level of “descriptive saturation” of their experiences. To accomplish this, we used standard qualitative summarizing techniques to analyze the data, using content analysis to identify key themes.37,38 Our 2 trained qualitative methodologists (JS and AF) reviewed the focus group and interview guides, focus group and interview transcripts, and verbatim notes to develop a code book. Because we used the same guide for the patient-parent focus groups and interviews, focus group and interview data were combined and analyzed together. Our qualitative methodologists then applied the codes and met on a weekly basis to discuss questions. This coded text was grouped together and rereviewed through a weekly iterative process with the entire research team until refined themes were developed.37,38
Data Synthesis Workshop
We held a data synthesis workshop, during which the research team and key stakeholders further refined and developed intervention prototypes for future pilot implementation. Nine stakeholders attended the workshop, including 5 parents, health system administrators, and clinicians and 4 researchers. We provided a summary of the qualitative findings from the focus groups and interviews and asked attendees to meet in small groups to brainstorm possible answers to the following question: “How might we reduce pain and syncope associated with vaccination?” Each small group presented their favorite intervention idea to the larger group, who discussed the pros and cons of each idea; the materials and training that would be needed for implementation; and possible implementation barriers. We then asked participants to vote for up to 3 of the intervention prototypes. We next invited 17 additional clinicians, health system staff, and parents who did not attend the workshop to complete a follow-up survey that sought to identify 1 final pilot intervention from the 3 prototypes recommended by data synthesis workshop participants. KPNW’s institutional review board approved the study protocol, consent forms, and all data collection tools.
RESULTS
We completed a focus group with 2 patient-parent dyads and 6 family interviews with 1 patient-parent dyad each. The mean time from last date of vaccination to the focus group or interview date was 120 days (range: 45–251 days). Of the 8 adolescent participants, 5 were male and 3 were female. All 8 parents who participated were female. We completed interviews with 7 clinical staff, including 3 pediatric primary care physicians, 2 medical assistants, and 2 nurses. Nine stakeholders attended the data synthesis workshop, and an additional 10 stakeholders (of the 17 invited) completed the follow-up survey.
Focus Groups and Interviews
We summarized the results in 4 main topic areas: 1) previous vaccination experiences and reactions that can contribute to future negative reactions; 2) current vaccination practices and techniques to minimize negative experiences during adolescent vaccination; 3) willingness to consider recommended pain and syncope prevention techniques not currently being used; and 4) other suggestions.
Topic 1: Previous Vaccination Experiences and Reactions That Can Contribute to Future Negative Reactions
Most adolescents (5 of 8) expressed anxiety about receiving vaccines, fear of needles, or worry about pain during or after vaccination. All described some pain and swelling after shots, with half (4 of 8) indicating it was intense initially and lasted for several days. None of our participants reported fainting with vaccination, although 2 described presyncope symptoms such as dizziness. Adolescents also reported being hungry or dehydrated at their clinic visits, especially visits occurring after school, and commented this might contribute to negative reactions after vaccination.
All clinicians noted that, although patient anxiety and worry about vaccinations are common, they rarely observed any adverse physical reactions during visits. Clinicians also noted that nearly every patient experiences some pain related to vaccination, but fear of that pain or of needles is a greater issue for some patients than for others. Most clinicians (5 of 7) noted that age was a factor in negative vaccination reactions, with clinicians relating that patients aged 11 to 14 years seemed to be “more challenging” than older patients. Parallel to adolescent and parent comments, 5 of 7 clinicians noted that dehydration, lack of food, or both before a vaccination was perceived as a factor in adverse reactions. Finally, 2 clinicians observed that the attitude or approach of a parent can affect the patient’s reaction. For example, parental anxiety can exacerbate the adolescent patient’s anxiety.
Topic 2: Current Vaccination Practices and Techniques to Minimize Negative Experiences during Adolescent Vaccination
Most patients and their parents (7 of 8 dyads) reported vaccinations being delivered at the end of the visit, although 3 patients said they would have preferred to receive them at the beginning of visit to “get it over with.” When referring to the recommended techniques, 4 of 8 patients recalled reviewing an information sheet about side effects but did not recall any upfront discussion with the clinician on how to prevent adverse reactions. Three patients recalled staff trying to comfort them during the vaccination with conversation or distraction and efforts to be “quick about” their shots. Two additional patients recalled their clinician suggesting that they rub or ice the area afterward to reduce soreness. Adolescents and parents recalled positioning such as reclining or sitting during their vaccination. All believed that these techniques were helpful. When asked about preparation for visits, some parents did not want to discuss the vaccination with their child before the visit because of concerns that it might increase anxiety. However, other parents expressed desire for receiving more upfront education on ways they could support their adolescent and counter any negative reactions.
All clinicians said they have adolescents sit or lie down if they are feeling faint, and they planned to continue that practice. It was noted that they never have adolescents stand during vaccination. All clinicians also related that they try to “plant a positive seed” and distract adolescents before and during vaccination, especially if the patient seems anxious or worried. Most clinicians said they administered the most painful shot last; provided vaccinations at the start of the visit rather than near the end of the visit if the patient was clearly anxious; and did not preface the visit with conversation about vaccinations when they believed that these discussions would increase patient anxiety. Generally, clinicians noted the value of preparing and educating adolescents and parents but expressed a need to balance this information with the potential for creating or increasing anxiety. Finally, 2 physicians and 1 nurse said they recommended using ibuprofen or applying either a warm washcloth or ice to relieve postvaccination injection-site pain.
Topic 3: Willingness to Consider Pain and Syncope Prevention Techniques Not Currently Implemented In Usual Care
Pain prevention techniques (Table 2)
Table 2.
Youth, parent, and practitioner reaction to and endorsement of pain prevention techniques not currently implemented in usual care
| Technique | Youth (Y)/Parent (P) | Clinician endorsements/reactions | |
|---|---|---|---|
| Level of support, no. in favor of technique | Reactions | ||
| Prepare patients and children with education | 6Y/4P | Desire more information regarding what to look for, how to respond to pain and swelling; some received suggestions during visit to use ice, massage, or warm shower or washcloth to reduce pain | YES, if educational information is given or sent before visit with no impact on clinic workflow |
| Breathing | 4Y/5P | No experience with this technique; seems like it would be helpful | YES, this seems reasonable if clinic workflow not affected |
| Tactile stimulation near injection site | 5Y/3P | May help; believe they have experienced this | YES, willing to do this if clinic workflow not overly affected |
| 2Y/2P | Do not believe this will help reduce pain | ||
| Topical anesthetics | 4Y/5P | Unsure topical anesthetic would help reduce pain; difficult to administer before a visit | NO; most convinced this does not help; no time or resources to implement this |
| 3Y/1P | Believe could help and maybe could reduce anxiety | ||
Four of 8 of the adolescents and parents recalled a clinician engaging in tactile stimulation (eg, rubbing injection site with pressure before vaccination), with 2 of them saying it helped reduce pain. In turn, 4 of 7 clinicians related that they engage in tactile stimulation often but not consistently because of time pressures, workflow, or the needs of specific patients. Most adolescents and parents did not recall engaging in breathing exercises during their vaccine visit, although 4 of 8 dyads felt it was a reasonable and logical technique that might be helpful. Most clinicians said they do not do this or do not do it very often. Regarding both tactile stimulation and breathing exercises, clinicians were willing to incorporate these into their practice if there was evidence of benefit and if these practices did not take too much time during the visit.
Adolescents and parents had no recollection of topical anesthetic use, and most did not believe that this would help reduce pain, although several thought it might. Furthermore, parents were resistant to topical anesthetic use because they felt it would be difficult for them to remember to apply before the visit. All clinicians indicated they do not use or encourage the use of topical anesthetics because of a lack of confidence in their efficacy and time and resource constraints. Clinicians were not supportive of topical anesthetic use as an option they would want to implement.
Syncope prevention techniques (Table 3)
Table 3.
Youth, parent, and practitioner reaction to and endorsement of syncope prevention techniques not currently implemented in usual care
| Technique | Youth (Y)/Parent (P) | Clinician endorsements/reactions | |
|---|---|---|---|
| Level of Support, no. in favor of technique | Reactions | ||
| Patient education | 3Y/2P | Unsure if education would affect fainting/syncope outcomes | YES, if educational information is given or sent before visit with no impact on clinic workflow |
| 4Y/2P | Support providing education materials; proactive approach | ||
| Water consumption | 8Y/5P | No experience but willing to try before visit; teens admitted not being well hydrated | YES, willing to offer water at check-in; not realistic to wait 30 min during visit before vaccination |
| Sodium consumption | 8Y/5P | Some concern about increased sodium for general health; willing to try salty snack before visit | NO, had never heard of this and skeptical of it; possibly willing to offer salty food at time of check-in |
| Caffeine consumption | 3Y | Likes drinking cola; open to this idea | NO, had never heard of this and skeptical of it; do not want to promote caffeine consumption by youth |
| 4Y/5P | Concern about increased “jitteriness” or creating an adverse reaction to the shot; concern about caffeine on health, physical development | ||
| Applied muscle tension | 7Y/4P | Unsure of potential benefit beyond distraction; open to this idea, squeeze stress ball | Maybe, if no time impact; unsure if this would be helpful and could increase tension in arm |
| 2Y | Already practice this technique on own | ||
Adolescents and parents indicated that they had not experienced, and were unsure about, applied muscle tension during vaccination. This was mirrored by clinicians, who were not aware of recommendations to use applied muscle tension. Clinicians expressed concern, because increased tension in the arm may cause more pain, despite the recommendation calling for tensing to occur in the nonvaccinated arm or other parts of the body. Parents did not want to encourage caffeine consumption, and adolescents believed the caffeine would increase anxiety and jitteriness during the visit. Adolescents and parents were more open to eating a salty snack; however, parents were concerned they would forget to give this snack before the visit. Clinicians had not considered caffeine consumption as a strategy to reduce syncope related to vaccination and, like patients and parents, overwhelmingly did not want to promote caffeine use among adolescents. Although clinicians were also skeptical of sodium consumption, they were slightly more willing to offer a “salty” snack at the visit if evidence showed this would be helpful.
Adolescents and parents endorsed water consumption given earlier comments about the tendency of adolescents to be dehydrated at the time of visits. Patients and parents also endorsed a prompt to drink water at appointment check-in. Clinicians were unaware of water consumption as a strategy to reduce syncope and had not been actively encouraging prevaccination water consumption; however, they did feel positive about offering water at appointment check-in or encouraging adolescents to drink water before they arrive for their visit.
Parents tended to prefer minimal discussion immediately before vaccination; however, they expressed a general desire for more information on how to prepare for and prevent fainting or pain. They felt this information was not provided during or at the end of the visit or in materials they receive after the visit. Parents suggested multiple times that they would appreciate more previsit education, perhaps in the form of an educational mailer or through the Health Plan Web site. Clinicians indicated they do not generally provide education before or at vaccination visits unless prompted by a parent or a patient. Clinicians observed that too much talking about the vaccination before administration actually created more patient anxiety. However, they endorsed educating parents more on ways to prepare for the vaccination or how to treat side effects and generally suggested that education could occur during appointment setup and reminder calls, or through the Health Plan Web site.
Topic 4: Other Suggestions
Patient, parent, and clinician participants independently suggested the use of a “comfort menu” offered during appointment check-in, with options for items such as bottled water, a stress ball, or a salty snack. Clinicians expressed a desire for support in identifying, before a visit, adolescents who might be anxious and need more support during vaccination. They also believed that additional training on approaches to interacting with anxious adolescents and parents would be beneficial to them.
Data Synthesis Workshop and Follow-up Survey
The workshop brainstorming session resulted in the identification of 4 interventions to reduce pain associated with vaccination: 1) providing information to parents on pain-reduction techniques before or after the visit; 2) ethyl chloride “freezing spray” to numb the injection site; 3) providing items from a comfort menu offered at visit check-in; and 4) distraction with videos or music.
Approaches identified to reduce syncope were similar to those for pain and included 1) parent and patient educational information; 2) distraction, relaxation, or comfort measures; 3) water loading or salt consumption; 4) clinician education about recognizing and managing patient anxiety; and 5) ensuring that patients lie down after their vaccination and are provided with adequate waiting time in the examination room before they leave.
The workshop participants observed the overlap between pain and syncope intervention ideas. They decided that interventions that could prevent both types of adverse reactions would be the most cost-effective, attractive to clinicians, and possibly generalizable to other medical procedures, such as allergy skin-prick testing.
Ultimately, workshop participants endorsed 3 intervention prototypes for potential implementation in KPNW pediatric clinics (Table 4): 1) A “comfort caddy”: A small, transportable caddy that includes comfort or distraction items (eg, stress balls, cold packs, water) and that medical staff can take into examination rooms during vaccination; 2) patient and parent educational materials before the vaccination visit or in the examination room; and 3) ways for clinicians to identify and manage patient anxiety (eg, building prompts into the EHR, and a clinician training module on anxiety management).
Table 4.
Additional suggestions emphasized by interviewees and endorsed during data synthesis workshop
| Suggestion | Youth and parent perspective | Clinician perspective |
|---|---|---|
| Previsit education | “One of the things that would have been helpful, I think, is having … the highlights of … the potential side effects [of vaccination] and what to do if it happens.” | “I like the idea of some education about the fainters, if the parents want information before … . You know, for these shots just say, ‘It looks like shots are kind of a little hard on your body, and these are the things you could do before your next shots.’” |
| List of interventions to choose from (“Comfort Menu”) | “Maybe a menu at check-in with these things as an option—check off what you find most suitable for yourself.” | “Maybe a comfort menu .… Develop a handout with some different things for people like ‘16 oz of fluids in 30 min, and salt [intake]’, and that kind of thing. … It would be nice and make them feel a little TLC.” |
| Recognizing and managing anxiety (practitioner endorsement only) | Not applicable | “I think what’s feasible is … training nurse staff to be prepared to manage anxiety … making sure that all the staff is … good at explaining the shots—that they have some talking points and some language about the vaccination and some strategies … and that they’re able to anticipate what the problem might be.” |
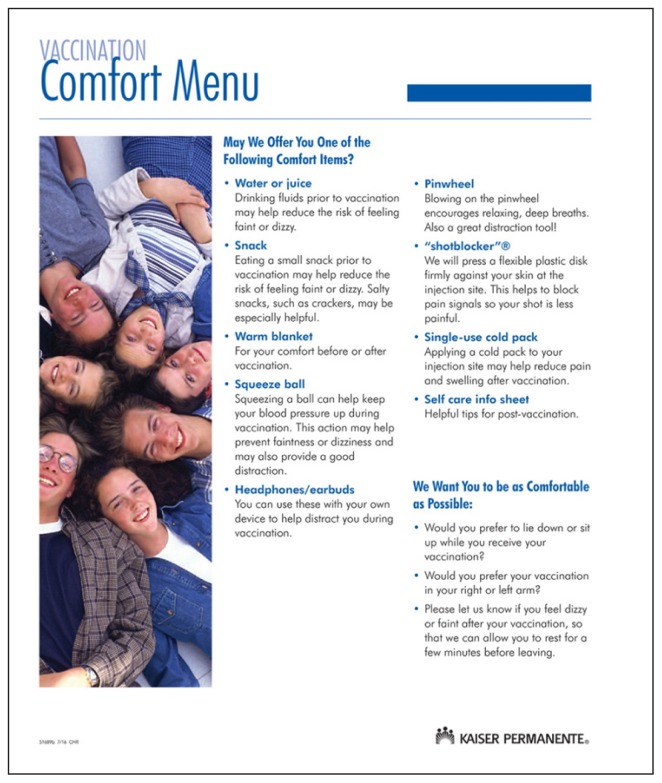
Ten stakeholders who did not attend the workshop completed the follow-up survey. Nine of these 10 respondents to the stakeholder survey endorsed a comfort caddy or cart as the first intervention to test. The selection of our final intervention—the Vaccination Comfort Menu—further incorporated feedback from pilot intervention clinics regarding preferences for design and feasibility of implementation (Figure 1). Pilot clinic staff believed that the use of a menu format with supplies stored in a central location would result in the least amount of disruption of clinical workflow.
Figure 1.
Vaccination Comfort Menu.
DISCUSSION
Patients, parents, and clinicians generally acknowledged the value of interventions to reduce pain and syncope related to adolescent vaccination. However, we found varying levels of enthusiasm and support for potential interventions to reduce these effects. Patients, parents, and clinicians were mutually willing to use verbal education and messaging about potential outcomes after vaccination before and during a vaccination visit, breathing exercises, social support or distraction, and water consumption as potential interventions to reduce adverse vaccination effects. There were mixed reactions to topical anesthetics and mostly negative reactions for caffeine consumption.
We found some areas of misalignment in the views of patients, parents, and clinicians. First, clinicians acknowledged that pain and syncope occur after vaccination; however, they believed that serious adverse events were rare. In turn, they commented that patient anxiety, as well as the interaction between patient and parent anxiety, might be more important issues to address. Clinicians expressed an interest in the development of tools, possibly included in the EHR, that would flag patients who have vaccination-related anxiety and allow clinicians to tailor the visit to account for that anxiety. Second, although all participants endorsed a need for some form of additional education about adverse vaccination-related outcomes, we received inconsistent feedback regarding the timing and delivery of education. There was an expressed need to strike a balance between offering interventions before vaccination and increasing adolescents’ and even parents’ anxiety. There was also concern regarding the preparation needed for some of the strategies. For example, some of the interventions—water and sodium consumption—required action in advance of the vaccination. Finally, clinicians consistently stated their willingness to implement techniques, but only if there was evidence of benefit and if the techniques did not affect time constraints already present in busy pediatric clinics.
There are potential limitations to our study. First, because of lack of evidence on strategies to reduce syncope after vaccination, we focused on strategies recommended for the prevention of syncope related to blood donation. Thus, it was reasonable for patients and parents to not experience these strategies or for clinicians to not recognize the application of these syncope prevention strategies to vaccination. However, there was positive feedback regarding specific strategies from the blood donation literature, especially in response to water consumption. Furthermore, although we based our selection of potential interventions on existing evidence, we did not distinguish between the strength of evidence for an intervention, such as the size of the effect it had on pain or syncope outcomes. Thus, there may be variation in the effectiveness of the selected interventions. For instance, water consumption before vaccination was supported by our participants; however, a recent clinical trial found that drinking water before vaccination did not have an effect on postvaccination presyncope in subjects aged 11 to 21 years.39
Next, the generalizability of our qualitative results may be reduced because of our small sample size, because there is a risk that we did not collect the full range of patient, parent, and clinician perspectives. However, given consistency of feedback, we believe we were able to ascertain which interventions would most benefit patients and parents while also considering clinician and health care system barriers to implementation. In addition, our consistent use of an interview guide, the use of a formal content analysis, and the review of findings by the data-synthesis workshop stakeholders help lessen these limitations.24 Additionally, we designed our qualitative research approach to focus on the collection of high-quality feedback from focus group and interview participants that would help us develop our intervention rather than focusing on theme saturation. We, therefore, used focus group and interview guides to ensure that the same content area was being explored with each participant; talked with a range of stakeholders to hear different perspectives; created and modified a code book that was based on a review of the transcripts; used 2 trained qualitative staff to code and review transcripts and discuss interpretation with the study team; and used multiple rounds of feedback, including a data-synthesis workshop.
Finally, perceptions of experiences and practices related to vaccination may vary by race; however, we did not consider participant race or ethnicity during our participant recruitment. This may limit the generalizability of our results to more diverse populations in different settings than in KPNW.
With input from patients and clinicians, we developed the Vaccination Comfort Menu to be provided to adolescent patients at the time of vaccination. We feel there are benefits to this approach. First, the menu incorporates into 1 source many recommended approaches to reducing pain and syncope. For instance, ear buds, pinwheels, and squeeze balls represent distraction techniques. Other menu items address concerns voiced by interview participants, such as the self-care information sheet, which addresses a desire for more information about potential adverse effects and actions to take if they occur. Second, the menu allows patients to individualize their use of interventions and select 1 or more items that they believe will improve their vaccination experience. Third, some KPNW clinical departments, including KPNW dental offices, currently use a more general comfort menu to improve their patients’ experiences. Thus, there is some preliminary experience that suggests the feasibility of implementing our intervention in busy clinical settings.
CONCLUSION
We created a comfort menu intervention, basing it on patients’, parents’, and clinicians’ preferences for and acceptance of strategies that have the potential to reduce pain and prevent syncope associated with adolescent vaccination. A pilot study conducted at KPNW pediatric clinics during Fall 2016 examined patients’ and parents’ perceptions of the intervention and its impact on pain and syncope after vaccination and the vaccination experience. The pilot study also examined the feasibility of future implementation of this intervention, including its impact on clinical workflow. Additional large-scale research is needed to test the direct impact of this and other interventions on the occurrence of pain and syncope after vaccination among adolescent patients and on completion of vaccination series.
Acknowledgments
This study was funded by the US Department of Health and Human Services National Vaccine Program Office (Grant Number VSRNV000002), Washington, DC.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Robinson CL, Romero JR, Kempe A, Pellegrini C Advisory Committee on Immunization Practices (ACIP) Child/Adolescent Immunization Work Group. Advisory Committee on Immunization Practices recommended immunization schedule for children and adolescents aged 18 years or younger—United States, 2017. MMWR Morb Mortal Wkly Rep. 2017 Feb 10;66(5):134–5. doi: 10.15585/mmwr.mm6605e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016 Dec 16;65(49):1405–8. doi: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- 3.Chang S, O’Connor PM, Slade BA, Woo EJ. US postlicensure safety surveillance for adolescent and adult tetanus, diphtheria and acellular pertussis vaccines: 2005–2007. Vaccine. 2013 Feb 27;31(10):1447–52. doi: 10.016/j.vaccine.2012.10.097. [DOI] [PubMed] [Google Scholar]
- 4.Gee J, Naleway A, Shui I, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: Findings from the Vaccine Safety Datalink. Vaccine. 2011 Oct 26;29(46):8279–84. doi: 10.1016/j.vaccine.2011.08.106. [DOI] [PubMed] [Google Scholar]
- 5.Li R, Stewart B, McNeil MM, et al. Post licensure surveillance of influenza vaccines in the Vaccine Safety Datalink in the 2013–2014 and 2014–2015 seasons. Pharmacoepidemiol Drug Saf. 2016 Aug;25(8):928–34. doi: 10.1002/pds.3996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braun MM, Patriarca PA, Ellenberg SS. Syncope after immunization. Arch Pediatr Adolesc Med. 1997 Mar;151(3):255–9. doi: 10.1001/archpedi.1997.02170400041007. [DOI] [PubMed] [Google Scholar]
- 7.Macartney KK, Chiu C, Georgousakis M, Brotherton JM. Safety of human papillomavirus vaccines: A review. Drug Saf. 2013 Jun;36(6):393–412. doi: 10.1007/s40264-013-0039-5. [DOI] [PubMed] [Google Scholar]
- 8.Taddio A, Ipp M, Thivakaran S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine. 2012 Jul 6;30(32):4807–12. doi: 10.1016/j.vaccine.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Taddio A, Ilersich AF, Ilersich AN, Wells J. From the mouth of babes: Getting vaccinated doesn’t have to hurt. Can J Infect Dis Med Microbiol. 2014 Jul;25(4):196–200. doi: 10.1155/2014/470261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gray L, Miller LW, Philipp BL, Blass EM. Breastfeeding is analgesic in healthy newborns. Pediatrics. 2002 Apr;109(4):590–3. doi: 10.1542/peds.109.4.590. [DOI] [PubMed] [Google Scholar]
- 11.Gray L, Watt L, Blass EM. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics. 2000 Jan;105(1):e14. doi: 10.1542/peds.105.1.e14. [DOI] [PubMed] [Google Scholar]
- 12.Dilli D, Küçük IG, Dallar Y. Interventions to reduce pain during vaccination in infancy. J Pediatr. 2009 Mar;154(3):385–90. doi: 10.1016/j.jpeds.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 13.Taddio A, Nulman I, Goldbach M, Ipp M, Koren G. Use of lidocaine-prilocaine cream for vaccination pain in infants. J Pediatr. 1994 Apr;124(4):643–8. doi: 10.1016/s0022-3476(05)83150-6. [DOI] [PubMed] [Google Scholar]
- 14.Taddio A, Ilersich AL, Ipp M, Kikuta A, Shah V HELPinKIDS Team. Physical interventions and injection techniques for reducing injection pain during routine childhood immunizations: Systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin Ther. 2009;31( Suppl 2):S48–76. doi: 10.1016/j.clinthera.2009.07.024. [DOI] [PubMed] [Google Scholar]
- 15.Taddio A, Ipp M, Vyas C, et al. Teaching parents to manage pain during infant immunizations: Laying the foundation for better pain management practices. Clin J Pain. 2014 Nov;30(11):987–94. doi: 10.1097/ajp.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 16.Hogan ME, Probst J, Wong K, Riddell RP, Katz J, Taddio A. A randomized-controlled trial of parent-led tactile stimulation to reduce pain during infant immunization injections. Clin J Pain. 2014 Mar;30(3):259–65. doi: 10.1097/ajp.0b013e318296079e. [DOI] [PubMed] [Google Scholar]
- 17.Chambers CT, Taddio A, Uman LS, McMurtry CM HELPinKIDS Team. Psychological interventions for reducing pain and distress during routine childhood immunizations: A systematic review. Clin Ther. 2009;31( Suppl 2):S77–S103. doi: 10.1016/j.clinthera.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 18.Shah V, Taddio A, McMurtry CM, et al. HELPinKIDS Team. Pharmacological and combined interventions to reduce vaccine injection pain in children and adults: Systematic review and meta-analysis. Clin J Pain. 2015 Oct;31(10 Suppl):S38–63. doi: 10.1097/AJP.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taddio A, McMurtry CM, Shah V, et al. Reducing pain during vaccine injections: Clinical practice guideline. CMAJ. 2015 Sep 22;187(13):975–82. doi: 10.1503/cmaj.150391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taddio A, Parikh C, Yoon EW, et al. Impact of parent-directed education on parental use of pain treatments during routine infant vaccinations: A cluster randomized trial. Pain. 2015 Jan;156(1):185–91. doi: 10.1016/j.pain.0000000000000021. [DOI] [PubMed] [Google Scholar]
- 21.Taddio A, Shah V, Leung E, et al. Knowledge translation of the HELPinKIDS clinical practice guideline for managing childhood vaccination pain: Usability and knowledge uptake of educational materials directed to new parents. BMC Pediatr. 2013 Feb 8;13:23. doi: 10.1186/1471-2431-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taddio A, Shah V, McMurtry CM, et al. HELPinKids&Adults Team. Procedural and physical interventions for vaccine injections: Systematic review of randomized controlled trials and quasi-randomized controlled trials. Clin J Pain. 2015 Oct;31(10 Suppl):S20–37. doi: 10.1097/AJP.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birnie KA, Chambers CT, Taddio A, et al. HELPinKids&Adults Team. Psychological interventions for vaccine injections in children and adolescents: Systematic review of randomized and quasi-randomized controlled trials. Clin J Pain. 2015 Oct;31(10 Suppl):S72–89. doi: 10.1097/AJP.0000000000000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silverman D. Doing qualitative research: A practical handbook. 4th ed. Thousand Oaks, CA: Sage Publications; 2010. [Google Scholar]
- 25.Taddio A, Appleton M, Bortolussi R, et al. Reducing the pain of childhood vaccination: An evidence-based clinical practice guideline. CMAJ. 2010 Dec 14;182(18):E843–55. doi: 10.1503/cmaj.101720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sauer LA, France CR. Caffeine attenuates vasovagal reactions in female first-time blood donors. Health Psychol. 1999 Jul;18(4):403–9. doi: 10.1037//0278-6133.18.4.403. [DOI] [PubMed] [Google Scholar]
- 27.Eder AF. Current efforts to reduce the risk of syncope among young blood donors. Curr Opin Hematol. 2012 Nov;19(6):480–5. doi: 10.1097/MOH.0b013e328358b15c. [DOI] [PubMed] [Google Scholar]
- 28.France CR, Ditto B, Wissel ME, et al. Predonation hydration and applied muscle tension combine to reduce presyncopal reactions to blood donation. Transfusion. 2010 Jun;50(6):1257–64. doi: 10.1111/j.1537-2995.2009.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hanson SA, France CR. Predonation water ingestion attenuates negative reactions to blood donation. Transfusion. 2004 Jun;44(6):924–8. doi: 10.1111/j.1537-2995.2004.03426.x. [DOI] [PubMed] [Google Scholar]
- 30.Hanson SA, France CR. Social support attenuates presyncopal reactions to blood donation. Transfusion. 2009 May;49(5):843–50. doi: 10.1111/j.1537-2995.2008.02057.x. [DOI] [PubMed] [Google Scholar]
- 31.Ando S, Kawamura N, Matsumoto M, et al. Simple standing test predicts and water ingestion prevents vasovagal reaction in the high-risk blood donors. Transfusion. 2009 Aug;49(8):1630–6. doi: 10.1111/j.1537-2995.2009.02189.x. [DOI] [PubMed] [Google Scholar]
- 32.Marchiondo KJ. Recognizing and treating vasovagal syncope. Am J Nurs. 2010 Apr;110(4):50–3. doi: 10.1097/01.naj.0000370159.10352.a6. [DOI] [PubMed] [Google Scholar]
- 33.Wieling W, France CR, van Dijk N, Kamel H, Thijs RD, Tomasulo P. Physiologic strategies to prevent fainting responses during or after whole blood donation. Transfusion. 2011 Dec;51(12):2727–38. doi: 10.1111/j.537-2995.011.03202.x. [DOI] [PubMed] [Google Scholar]
- 34.Maggi R, Brignole M. Update in the treatment of neurally-mediated syncope. Minerva Med. 2007 Oct;98(5):503–9. [PubMed] [Google Scholar]
- 35.Ditto B, France CR, Albert M, Byrne N, Smyth-Laporte J. Effects of applied muscle tension on the likelihood of blood donor return. Transfusion. 2009 May;49(5):858–62. doi: 10.1111/j.1537-2995.2008.02067.x. [DOI] [PubMed] [Google Scholar]
- 36.McMurtry CM, Riddell RP, Taddio A, et al. Far from “just a poke”: Common painful needle procedures and the development of needle fear. Clin J Pain. 2015 Oct;31(Suppl 10):S3–S11. doi: 10.1097/AJP.0000000000000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernard HR, Ryan GW. Analyzing qualitative data: Systematic approaches. 1st ed. Thousand Oaks, CA: Sage Publications; 2010. [Google Scholar]
- 38.Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. 3rd ed. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- 39.Kemper AR, Barnett ED, Walter EB, et al. Drinking water to prevent postvaccination presyncope in adolescents: A randomized trial. Pediatrics. 2017 Nov;140(5):e20170508. doi: 10.1542/peds.2017-0508. [DOI] [PMC free article] [PubMed] [Google Scholar]