Abstract
Introduction
Cardiac complications associated with influenza infection can occur either via a direct effect of the virus on the heart or through exacerbation of preexisting cardiovascular disease. We present a case of a 57-year-old man with acute influenza infection complicated by pericardial effusion and cardiac tamponade.
Case Presentation
A 57-year-old white man presented to the Emergency Department with sudden onset of severe, nonexertional, retrosternal, pressure-like chest pain for a few hours and with fever and muscle aches for 2 days. The patient was initially admitted because of suspected acute coronary syndrome. The next morning, he complained of acute-onset shortness of breath and had hypotension and tachycardia. On examination, his peripheral extremities were cold and heart sounds were distant. Pulsus paradoxus was 20 mmHg. The electrocardiogram showed low-voltage QRS complex with electrical alternans. An urgently performed bedside echocardiogram showed moderate pericardial effusion with a small right ventricular cavity with diastolic collapse. Emergent pericardiocentesis was performed, with removal of 250 mL of fluid from the pericardial space. The patient’s hemodynamic status immediately improved. Analyses of pericardial fluid demonstrated no bacteria, acid-fast bacilli, or malignant cells. The result of a rapid influenza diagnostic test with polymerase chain reaction was positive for influenza A virus, with other viral panels yielding normal results. The patient was treated with oseltamivir for 5 days.
Discussion
Pericardial involvement is a rare and perhaps underreported complication of influenza infection. Early recognition of cardiac symptoms and appropriate diagnostic workup in a patient presenting with influenza-like symptoms is important to avoid life-threatening complications.
Keywords: cardiac tamponade, influenza, flu, pericardial effusion, pericarditis
INTRODUCTION
Acute respiratory illness caused by influenza A or B virus occurs in outbreaks, mostly during the winter season, presenting with upper and/or lower respiratory tract infection along with signs and symptoms of systemic illness such as fever, headache, myalgia, and weakness. Cardiac complications associated with acute influenza infection can involve the pericardium, myocardium, and coronary arteries, resulting in worsening ischemic heart disease.1 The association between influenza epidemics and increased rates of acute coronary syndrome, especially non-ST-elevation myocardial infarction, is well established.2 Pericardial syndrome with pericarditis complicated by cardiac tamponade is a rare complication of acute influenza infection.3
We present a case of a 57-year-old man with acute influenza infection who presented with pericardial effusion and cardiac tamponade.
CASE PRESENTATION
Presenting Concerns
A 57-year-old white man presented to our Emergency Department with sudden onset of severe, nonexertional, retrosternal, pressurelike chest pain for the last 24 hours. The pain was nonradiating but associated with numbness in his left arm. The patient also reported 2 days of fever with muscle aches. He had hypertension but no history of pedal edema, palpitations, orthopnea, or syncope. He reported current tobacco use and occasional alcohol use but no use of illicit drugs. On presentation, he was afebrile and had a blood pressure of 120/70 mmHg, heart rate of 87 beats/min, respiration rate of 18 breaths/min, and oxygen saturation of 97% on room air. Results of the physical examination were unremarkable.
Initial laboratory findings showed an elevated hemoglobin level of 17.1 g/L with a normal white blood cell count and platelet count. Results of a basic metabolic panel showed hyponatremia (sodium level of 130 mEq/L), but potassium level and renal functions were normal. An electrocardiogram showed sinus tachycardia, and the initial troponin measurement was slightly elevated at 0.06 ng/mL (normal is < 0.04). A chest radiograph was normal. A repeat troponin level was 0.12 mg/mL after 6 hours.
Therapeutic Intervention and Treatment
Because of his presentation and risk factors for coronary artery disease, a decision was made to admit the patient to the hospital for management of acute coronary syndrome. The patient received aspirin, nitroglycerin, and a therapeutic dose of enoxaparin. His chest pain was relieved after a few hours.
The next day, the patient complained of acute onset of shortness of breath. He became hypotensive (blood pressure of 100/60 mmHg) and tachycardic (heart rate of 110/min). His peripheral extremities were cold, and heart sounds were distant. Pulsus paradoxus was 20 mmHg.
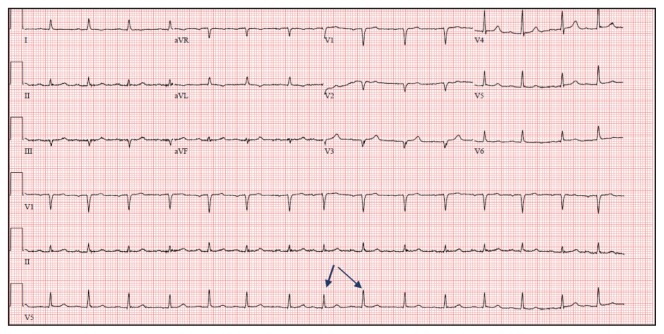
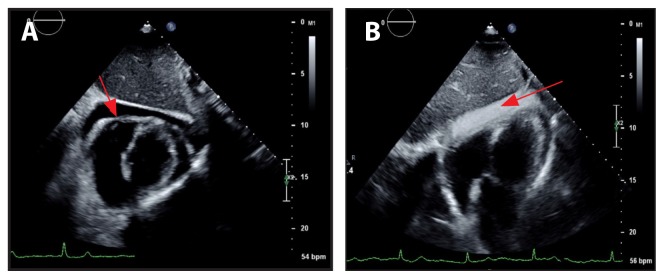
Repeat electrocardiogram showed low-voltage QRS complex with electrical alternans along with sinus tachycardia (Figure 1). An echocardiogram was urgently obtained at the bedside and showed moderate pericardial effusion with a small right ventricular cavity with diastolic collapse (Figure 2). Shortly thereafter, the patient’s condition became unstable. He had severe dyspnea and clinically significant hypotension with systolic blood pressure dropping to the 80 mmHg range. An emergent pericardiocentesis was performed, with removal of 250 mL of serosanguinous fluid from the pericardial space. The patient experienced immediate improvement of hemodynamic status. A repeat echocardiogram performed the next day showed resolution of pericardial effusion and no signs of right ventricular collapse.
Figure 1.
Electrocardiogram showing low voltage and electrical alternans (arrows highlighting the electrical alternans).
Figure 2.
Two-dimensional echocardiograms showing a moderately sized pericardial effusion (Figure 2A, arrow) and agitated saline injection in the pericardial space (Figure 2B, arrow) during pericardiocentesis.
Analysis of pericardial fluid showed leukocytosis with lymphocytic predominance (748/μL with 65% lymphocytes, 20% macrophages, 4% monocytes, and 4% neutrophils), and a culture was negative for bacteria. Cytologic results showed no malignant cells, acid-fast bacilli stain and culture were negative, HIV 1 and 2 antibodies along with HIV-1 p24 antigen were negative, and the hepatitis screen had normal results. The result of a rapid influenza diagnostic test with polymerase chain reaction was positive for influenza A virus, and other viral studies (cytomegalovirus, Epstein-Barr virus, coxsackievirus, parvovirus, and paramyxovirus) yielded normal results.
Follow-up and Outcomes
After the pericardiocentesis, the patient recovered well without any recurrences. Treatment with ibuprofen and colchicine was initiated. With the diagnosis of influenza, the patient was treated with oseltamivir for 5 days.
DISCUSSION
Every year, influenza infection places a substantial burden on health care services worldwide. The US Centers for Disease Control and Prevention estimated that in the US influenza infection has caused between 9.2 million and 35.6 million illnesses, 140,000 to 710,000 hospitalizations, and 12,000 to 56,000 deaths annually since 2010.4 Although acutely debilitating, influenza is a self-limited infection in the general population, meaning that it usually resolves without intervention. However, it is associated with increased morbidity and mortality in certain high-risk populations.5,6
Although the respiratory system is most commonly affected during influenza infection, cardiac involvement is also known to occur. This can occur either via direct effect of the virus on the heart or through exacerbation of preexisting cardiovascular disease.7 Direct myocardial involvement presenting as myocarditis can present in a range from asymptomatic to fulminant myocarditis leading to cardiogenic shock and death.8 Similarly, pericardial involvement presentations can range from pericarditis to pericardial effusion and cardiac tamponade.3 Cardiovascular mortality is shown to be increased during influenza epidemics in patients with preexisting coronary artery disease,9 and cardiovascular mortality is reduced after influenza vaccination in high-risk patients.10 Results of many studies have shown that there is an increase in rates of myocardial infarction during influenza outbreaks. An association between laboratory-confirmed influenza infection and acute myocardial infarction has been confirmed by recent study findings.2
Involvement of the pericardium is one of the rare complications of influenza infection. The incidence of pericardial effusion and cardiac tamponade in patients with influenza infection is not fully known and is perhaps underreported. Only a few cases have been reported so far, to our knowledge. Cases presentations ranging from self-limiting pericarditis11 to acute pericardial effusion and cardiac tamponade requiring emergent pericardiocentesis have been reported.3 A case report of chronic pericardial effusion requiring pericardiectomy has also been described.12 In the recently reported case of cardiac tamponade secondary to influenza infection, a 22-year-old woman with no known cardiac history but with preceding symptoms of influenza-like illness presented with tachycardia, hypotension, and jugular venous distension requiring emergent pericardiocentesis.3 In our case, the patient initially presented with pericardial chest pain and experienced pericardial effusion leading to cardiac tamponade overnight.
Unlike in chronic pericardial effusion, rapid accumulation of pericardial fluid in the inelastic pericardial sac can lead to cardiac tamponade even with a minimal amount of fluid. Cardiac tamponade occurs when intrapericardial pressure exceeds intracardiac pressure. The rapidity of fluid accumulation is a greater factor in the development of tamponade than is the amount of fluid accumulation.13 Some authors describe cardiac tamponade as a continuum of severity ranging from asymptomatic intrapericardial pressure elevation to clinical tamponade with signs and symptoms of dyspnea, tachycardia, jugular venous distension, pulsus paradoxus, and right ventricular diastolic collapse on echocardiography with hypotension and shock in severe cases.14 The echocardiographic sign of right ventricular diastolic collapse has been shown to occur early in the course of cardiac tamponade, which demonstrates the importance of bedside ultrasonography in the early detection of cardiac tamponade.15 The mechanism of pericardial effusion in influenza infection is not well known. Research findings have shown that there is elevation of vascular endothelial growth factor and basic fibroblast growth factor levels in pericardial fluid in viral pericardial effusion, which is thought to play a role in the pathogenesis of pericardial inflammation and effusion.16
Removal of pericardial fluid, which relieves the intrapericardial pressure, is the definitive treatment of clinically significant cardiac tamponade. Supportive care with intravenous normal saline and, if needed, vasopressors should be used initially to stabilize the hemodynamic status but should not be a substitute for drainage of the effusion.17
Oseltamivir and zanamivir are antiviral agents that are recommended for the treatment and prophylaxis of influenza infection.18–20 Oseltamivir and zanamivir have been shown to reduce the duration of uncomplicated influenza A and B virus illness by approximately 1 day, when used within the 48-hour window from the onset of symptoms.21–23 There are limited data regarding use of neuraminidase inhibitors in preventing serious influenza-related complications,24 and there are no data available, of which we are aware, regarding the use of neuraminidase inhibitors in the prevention and treatment of influenza-related cardiac complications. Although initiation of antiviral agents after 48 hours of illness has shown minimal or no benefit in uncomplicated influenza,25 oseltamivir has been shown to reduce severe clinical outcomes in patients hospitalized with influenza. Benefit was observed even after 48 hours of initiation of antiviral agents.26 Antiviral treatment with oseltamivir or zanamivir has been recommended for all eligible individuals with suspected or confirmed influenza requiring hospitalization regardless of previous health or vaccination status.19–21
CONCLUSION
Our case presents one of the rare and probably underreported complications of influenza infection. Early recognition of cardiac symptoms and appropriate diagnostic workup in a patient presenting with influenzalike symptoms is important to avoid life-threatening complications. Our case also highlights the importance of bedside echocardiography in the early recognition of clinically significant cardiac tamponade.
Acknowledgment
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Mamas MA, Fraser D, Neyses L. Cardiovascular manifestations associated with influenza virus infection. Int J Cardiol. 2008 Nov;130(3):304–9. doi: 10.1016/j.ijcard.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 2.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018 Jan 25;378(4):345–53. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 3.Sidhu RS, Sharma A, Paterson ID, Bainey KR. Influenza H1N1 infection leading to cardiac tamponade in a previously healthy patient: A case report. Res Cardiovasc Med. 2016 Jul 16;5(3):e31546. doi: 10.4103/2251-9572.218741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Disease burden of influenza [Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2018. May 22, [cited 2018 Sep 28]. Available from: www.cdc.gov/flu/about/disease/burden.rtf. [Google Scholar]
- 5.Memoli MJ, Athota R, Reed S, et al. The natural history of influenza infection in the severely immunocompromised vs nonimmunocompromised hosts. Clin Infect Dis. 2014 Jan;58(2):214–24. doi: 10.1093/cid/cit725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dugan VG, Blanton L, Elal AIA, et al. Update: Influenza activity—United States, October 1–November 25, 2017. MMWR Morb Mortal Wkly Rep. 2017 Dec 8;66(48):1318–26. doi: 10.15585/mmwr.mm6648a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madjid M, Aboshady I, Awan I, Litovsky S, Casscells SW. Influenza and cardiovascular disease: Is there a causal relationship? Tex Heart Inst J. 2004;31(1):4–13. [PMC free article] [PubMed] [Google Scholar]
- 8.Rezkalla SH, Kloner RA. Influenza-related viral myocarditis. WMJ. 2010 Aug;109(4):209–13. [PubMed] [Google Scholar]
- 9.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016 Jun 1;1(3):274–81. doi: 10.1001/jamacardio.2016.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Estabragh ZR, Mamas MA. The cardiovascular manifestations of influenza: A systematic review. Int J Cardiol. 2013 Sep 10;167(6):2397–403. doi: 10.1016/j.ijcard.2013.01.274. [DOI] [PubMed] [Google Scholar]
- 11.Knežević Praveček M, Hadžibegović I, Coha B, Samardžić P, Mišić B, Jandrić Balen M. Pericardial effusion complicating swine origin influenzae A (H1N1) infection in a 50-year-old woman. Med Glas (Zenica) 2013 Feb;10(1):173–6. [PubMed] [Google Scholar]
- 12.Martin-Lázaro JF, Homs C, Benito R, Pedro AS, Suárez MA. Chronic pericardial effusion secondary to a influenza virus A (H1N1)/2009 infection. Turk Kardiyol Dern Ars. 2013 Mar;41(2):157–60. doi: 10.5543/tkda.2013.18827. [DOI] [PubMed] [Google Scholar]
- 13.Butala A, Chaudhari S, Sacerdote A. Cardiac tamponade as a presenting manifestation of severe hypothyroidism. BMJ Case Rep. 2013 Feb 5;2013 doi: 10.1136/bcr-12-2011-5281. bcr2012005281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sagristà-Sauleda J, Mercé AS, Soler-Soler J. Diagnosis and management of pericardial effusion. World J Cardiol. 2011 May 26;3(5):135–43. doi: 10.4330/wjc.v3.i5.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh S, Wann LS, Klopfenstein HS, Hartz A, Brooks HL. Usefulness of right ventricular diastolic collapse in diagnosing cardiac tamponade and comparison to pulsus paradoxus. Am J Cardiol. 1986 Mar 1;57(8):652–6. doi: 10.1016/0002-9149(86)90853-2. [DOI] [PubMed] [Google Scholar]
- 16.Karatolios K, Moosdorf R, Maisch B, Pankuweit S. Cytokines in pericardial effusion of patients with inflammatory pericardial disease. Mediators Inflamm. 2012;2012 doi: 10.1155/2012/382082. 382082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003 Aug 14;349(7):684–90. doi: 10.1056/NEJMra022643. [DOI] [PubMed] [Google Scholar]
- 18.Fiore AE, Fry A, Shay D, et al. Centers for Disease Control and Prevention (CDC) Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011 Jan 21;60(1):1–24. [PubMed] [Google Scholar]
- 19.Writing Committee of the WHO Consultation on Clinical Aspects of Pandemic (H1N1) 2009 Influenza. Bautista E, Chotpitayasunondh T, Gao Z, et al. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010 May 6;362(18):1708–19. doi: 10.1056/NEJMra1000449. [DOI] [PubMed] [Google Scholar]
- 20.What you should know about flu antiviral drugs [Internet] Atlanta, GA: Centers for Disease Control and Prevention; 2018. Jun 20, [cited 2018 Aug 22]. Available from: www.cdc.gov/flu/antivirals/whatyoushould.rtf. [Google Scholar]
- 21.Hayden FG, Osterhaus AD, Treanor JJ, et al. Efficacy and safety of the neuraminidase inhibitor zanamivir in the treatment of influenzavirus infections. GG167 Influenza Study Group. N Engl J Med. 1997 Sep 25;337(13):874–80. doi: 10.1056/NEJM199709253371302. [DOI] [PubMed] [Google Scholar]
- 22.Nicholson KG, Aoki FY, Osterhaus AD, et al. Efficacy and safety of oseltamivir in treatment of acute influenza: A randomised controlled trial. Neuraminidase Inhibitor Flu Treatment Investigator Group. Lancet. 2000 May 27;355(9218):1845–50. doi: 10.1016/s0140-6736(00)02288-1. [DOI] [PubMed] [Google Scholar]
- 23.Treanor JJ, Hayden FG, Vrooman PS, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: A randomized controlled trial. US Oral Neuraminidase Study Group. JAMA. 2000 Feb 23;283(8):1016–24. doi: 10.1001/jama.283.8.1016. [DOI] [PubMed] [Google Scholar]
- 24.Kaiser L, Wat C, Mills T, Mahoney P, Ward P, Hayden F. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med. 2003 Jul 28;163(14):1667–72. doi: 10.1001/archinte.163.14.1667. [DOI] [PubMed] [Google Scholar]
- 25.Cowling BJ, Chan KH, Fang VJ, et al. Comparative epidemiology of pandemic and seasonal influenza A in households. N Engl J Med. 2010 Jun 10;362(23):2175–84. doi: 10.1056/NEJMoa0911530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanshaoworakul W, Simmerman JM, Narueponjirakul U, et al. Severe human influenza infections in Thailand: Oseltamivir treatment and risk factors for fatal outcome. PLoS One. 2009 Jun 25;4(6):e6051. doi: 10.1371/journal.pone.0006051. [DOI] [PMC free article] [PubMed] [Google Scholar]