Abstract
Interleukin (IL)-1B reportedly promotes the stemness and invasiveness of colon cancer cells. Several studies have investigated the association between IL-1B gene polymorphisms and colorectal cancer (CRC) risk, but report conflicting findings. Here, this association was explored in a hospital-based case-control study involving 527 CRC cases and 639 controls from two Chinese Han populations. Genotyping was done by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. The IL-1B expression in CRC patients and controls were obtained from the GEPIA database and the mRNA expressions of different genotypes were downloaded from the GTEx portal database. The relationship of two IL-1B gene loci with clinical parameters and overall survival were analyzed using the Chi-square test and Kaplan-Meier analysis with the log-rank test respectively. It was found that the IL-1B mRNA levels in CRC patients were significantly higher than in controls. Bioinformatic analysis suggested that rs1143634 and rs1143623 polymorphisms decreased the IL-1B mRNA expression. The two polymorphisms were associated with decreased risk for CRC. Stratified analyses revealed the IL-1B gene rs1143623 and rs1143634 polymorphisms decreased the risk of CRC among females, smokers and drinkers. Moreover, the CC and/or GC genotype of rs1143623 polymorphism were correlated with decreased risk among CRC patients with tumor size ≥5cm, TNM stage III+IV, and rectal cancer. For rs1143634 polymorphism, the CT genotype reduced the risk of colorectal adenocarcinoma. The CRC patients carrying CC genotype of rs1143623 polymorphism were associated with better overall survival. In conclusion, IL-1B gene rs1143623 and rs1143634 polymorphisms are associated with decreased risk for CRC patients and thereby play important roles in the etiology of CRC.
Keywords: IL-1B, colorectal cancer, two-center case-control study
Introduction
Colorectal cancer (CRC) ranks third in incidence and second in mortality among all cancers [1]. Over 1.8 million new CRC patients and 881,000 deaths were estimated to occur in 2018 [1]. The incidence and mortality of CRC in China are increasing in the recent decade. However, the etiology of CRC is still poorly understood but may be attributed to dietary patterns, smoking, lifestyle factors, drinking and other factors [2,3]. Moreover, the elevated expression of proinflammatory cytokines is associated with the tumorigenesis of sporadic CRC [4].
Chronic inflammation is one of the hallmarks of CRC, which arises following prolonged inflammation [5,6]. Any substantial shift of the bacterial population could considerably affect inflammatory responses and contribute to CRC development [7]. Interleukin (IL)-1 is a group of potent proinflammatory cytokines including IL-1B which is activated by caspase-1 upon inflammasome activation in tumor cells [8]. IL-1B induces a host of growth factors and angiogenic factors and promote tumor growth and metastasis [8]. A mouse CRC model shows IL-1B arising from tumor-infiltrating neutrophils plays an pivotal role in tumorigenesis [9].
Single-nucleotide polymorphisms (SNPs) in the promoter regions of cytokine genes may affect the protein IL-1 expressions, thereby influencing the risk of cancer. Up to date, several studies have investigated the association between IL-1B gene polymorphisms and CRC risk, but report conflicting findings. In this study, we selected two SNPs (rs1143634, rs1143623 polymorphisms). The rs1143623 polymorphism is located at the transcription factor binding site of the IL-1B gene, and nucleotide changes (G to C) may affect the transcription factor binding. The rs1143634 polymorphism causes synonymous mutation when the nucleotide changes from C to T. A Danish study [10] firstly found the IL-1B gene rs1143623 polymorphism increased the risk of CRC and a Russian study [11] suggested was not associated with CRC risk. Regarding rs1143634 polymorphism, an American study and a Romanian study found no association between this SNP and CRC risk [12,13], while a Chinese study [14] showed that it was related to increased risk of CRC. To validate the inconsistences among these studies, we designed this two-center case-control study to clarify the potential association between two IL-1B gene variants (rs1143634, rs1143623 polymorphisms) and CRC risk. In addition, we explored the links of the IL-1B gene variants with clinical features and overall survival (OS) of CRC.
RESULTS
Characteristics of the study population
Baseline characteristics of the study population and their statistical significance were summarized in Table 1. The CRC patients and healthy controls were aged 56.46±11.70 and 56.00±10.59 years, respectively. The male-female ratios in the cases and controls were 1.45:1 and 1.39:1 respectively. No significant between-group difference was found in smoking, drinking or family history of cancers. Most CRC patients were rectal carcinoma or adenocarcinoma and in the TNM stage II and III. Other clinical parameters (tumor size, CEA, CA199 and differentiation) were also recorded.
Table 1. Patient demographics and risk factors in colorectal cancer.
| Characteristics | Case (N=527) | Control (N=639) | P |
| Age | 56.46±11.70 | 56.00±10.59 | 0.490 |
| Gender | 0.733 | ||
| Female | 215(40.8%) | 267(41.8%) | |
| Male | 312(59.2%) | 372(58.2%) | |
| Smoking | 0.371 | ||
| Yes | 286(54.3%) | 330(51.6%) | |
| No | 241(45.7%) | 309(48.4%) | |
| Drinking | 0.156 | ||
| Yes | 308(58.4%) | 347(54.3%) | |
| No | 219(41.6%) | 292(45.7%) | |
| Family history of cancer | 0.106 | ||
| Yes | 65(12.3%) | 100(15.6%) | |
| No | 462(88.4%) | 539(84.7%) | |
| Tumor size | |||
| <5cm | 306(58.1%) | — | |
| ≥5cm | 221(41.9%) | — | |
| CEA | |||
| Positive | 143(27.1%) | — | |
| Negative | 384(72.9%) | — | |
| CA199 | |||
| Positive | 152(28.8%) | — | |
| Negative | 375(71.2%) | — | |
| Tumor location | |||
| Rectum | 303(57.5%) | — | |
| Colon | 224(42.5%) | — | |
| Differentiation | |||
| Well | 244(58.3%) | — | |
| Moderate | 204(41.7%) | — | |
| Poor | 79(59.3%) | — | |
| Adenocarcinoma | |||
| Yes | 301(57.1%) | — | |
| No | 226(42.9%) | — | |
| TNM classification | |||
| I | 65(16.9%) | — | |
| II | 197(34.0%) | — | |
| III | 162(41.0%) | — | |
| IV | 103(8.1%) | — |
CEA: carcino-embryonic antigen; CA199: carbohydrate antigen 19-9; TNM: tumor node metastasis.
Bioinformatic analysis
GEPIA database analysis based on data from The Cancer Genome Atlas (TCGA) showed the IL-1B mRNA levels in the CRC patients were significantly higher than in the controls (Figure 1). The data from the International HapMap Project and GTEx portal showed the mutant genotype of the two polymorphisms could decrease IL-1B gene expression (Figure 2). We hypothesized the IL-1B rs1143623 and rs1143634 polymorphisms conferred susceptibility to CRC by altering the IL-1B expression.
Figure 1.
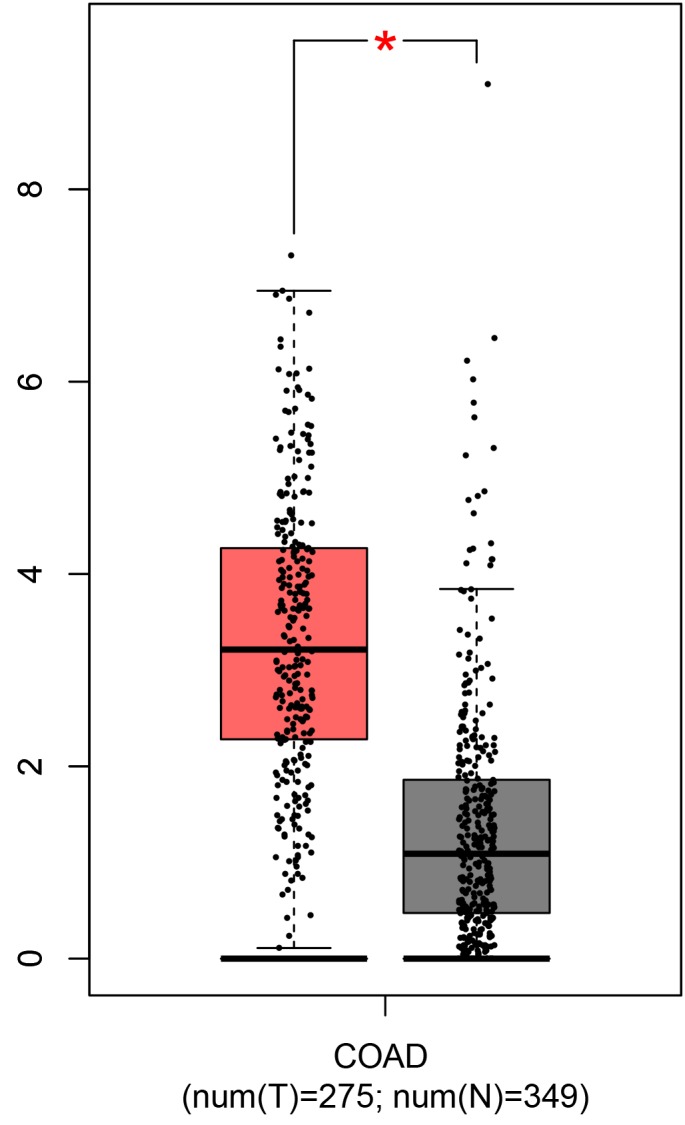
TCGA data confirmed the IL-1B expressions in rectal cancer patients were significantly higher than in the control, which was analyzed by GEPIA. T: tumor samples; N: paired normal tissues.
Figure 2.
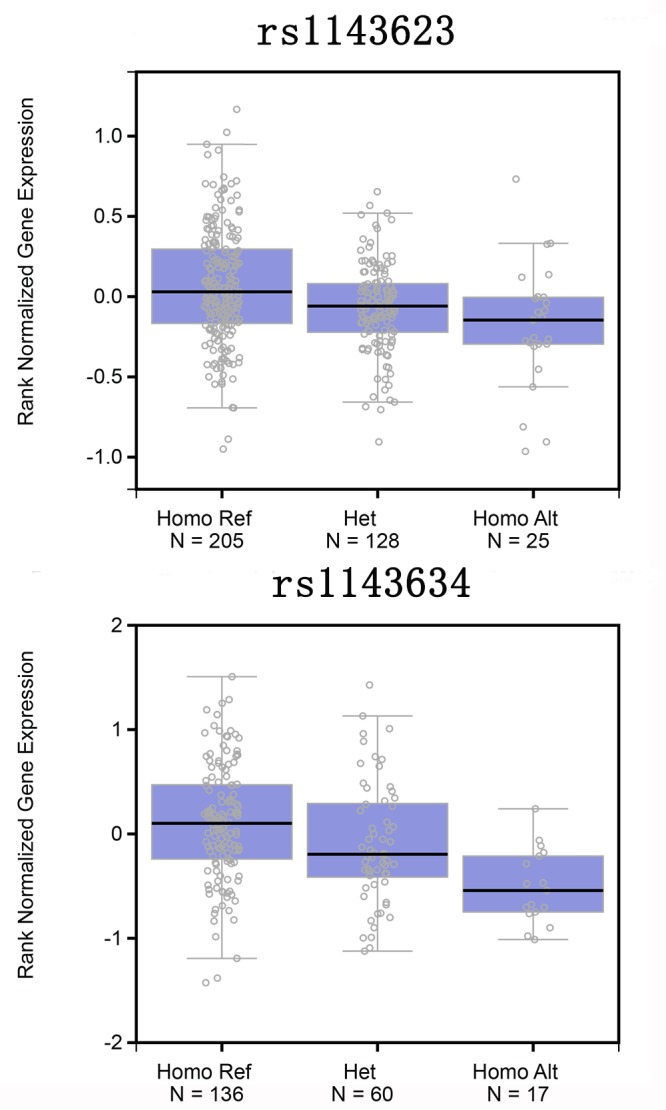
A association between IL-1B mRNA expression levels and genotypes of rs1143623 or rs1143634 polymorphisms. Data about genotypes and mRNA expression in esophagus-mucosa were obtained from the public GTEx portal database.
Association of IL-1B gene polymorphisms with CRC risk and clinical parameters of CRC
Table 2 shows the genotype and allele distributions of the two polymorphisms (rs1143623, rs1143634) polymorphisms in CRC cases and controls. No significant deviation from HWE was found for the either SNP in the controls. The rs1143623 polymorphism was associated with the decreased risk of CRC in the homozygous, dominant and allelic models. Similar findings were observed for the rs1143634 polymorphism, as it decreased the risk of CRC under the five models. This association remained true after the adjustment of sex and age.
Table 2. Genotype frequencies of IL-1B gene polymorphisms in colorectal cancer cases and controls.
| Models | Genotype | Case (n, %) | Control (n, %) | OR (95% CI) | P-value | Adjusted OR (95% CI)* | P-value |
| rs1143623 | |||||||
| Co-dominant | GG | 306 (58.1%) | 329 (51.5%) | 1.00(reference) | - | 1.00(reference) | - |
| Heterozygote | GC | 188 (35.7%) | 251 (39.3%) | 0.81(0.63,1.03) | 0.083 | 0.76(0.47,1.22) | 0.256 |
| Homozygote | CC | 32 (6.1%) | 57 (8.9%) | 0.60(0.38,0.96) | 0.032 | 0.61(0.38,0.97) | 0.036 |
| Dominant | GG | 306 (58.1%) | 329 (51.5%) | 1.00(reference) | - | 1.00(reference) | - |
| GC+CC | 220 (41.7%) | 308 (48.2%) | 0.77(0.61,0.97) | 0.026 | 0.77(0.61,0.97) | 0.026 | |
| Recessive | GC+GG | 494 (93.7%) | 580 (90.8%) | 1.00(reference) | - | 1.00(reference) | - |
| CC | 32 (6.1%) | 57 (8.9%) | 0.66(0.42,1.03) | 0.069 | 0.84(0.66,1.08) | 0.183 | |
| Allele | G | 800 (75.9%) | 909 (71.1%) | 1.00(reference) | - | ||
| C | 252 (23.9%) | 365 (28.6%) | 0.78(0.65,0.95) | 0.011 | |||
| Rs1143634 | |||||||
| Co-dominant | CC | 399 (75.7%) | 447 (70.0%) | 1.00(reference) | - | 1.00(reference) | - |
| Heterozygote | CT | 119 (22.6%) | 168 (26.3%) | 0.79(0.61,1.04) | 0.094 | 0.79(0.60,1.04) | 0.089 |
| Homozygote | TT | 8 (1.5%) | 22 (3.4%) | 0.41(0.18,0.93) | 0.032 | 0.41(0.18,0.94) | 0.036 |
| Dominant | CC | 399 (75.7%) | 447 (70.0%) | 1.00(reference) | - | 1.00(reference) | - |
| CT+TT | 127 (24.1%) | 190 (29.7%) | 0.75(0.58,0.97) | 0.031 | 0.75(0.58,0.97) | 0.030 | |
| Recessive | CT+CC | 518 (98.3%) | 615 (96.2%) | 1.00(reference) | - | 1.00(reference) | - |
| TT | 8 (1.5%) | 22 (3.4%) | 0.43(0.19,0.98) | 0.044 | 0.44(0.19,1.00) | 0.049 | |
| Allele | C | 917 (87.0%) | 1062 (83.1%) | 1.00(reference) | - | ||
| T | 135 (12.8%) | 212 (33.2%) | 0.74(0.58,0.93) | 0.010 |
*Adjusted for sex and age. Bold values are statistically significant (P < 0.05)
Stratified analyses according to age, sex, smoking and drinking were also conducted (Table 3). The IL-1B gene rs1143623 polymorphism decreased the risk of CRC among female, but not among male. The significant findings were further confirmed among the individuals <50 years, smokers and drinkers. Subgroup analyses by age revealed the rs1143634 decreased risks in individuals ≥ 50 years but not in < 50 years. This association held true in females, smokers and drinkers.
Table 3. Stratified analyses between IL-1B gene polymorphisms and risk of colorectal cancer.
| Variable | case/control | Homozygous model | Dominant model | Recessive model | ||
| Rs1143623 | GG | GC | CC | CC vs. GG | CC+GC vs. GG | CC vs. GC+GG |
| Age (years) | ||||||
| <50 | 101/94 | 65/74 | 8/18 | 0.44(0.21,0.91); 0.024 | 0.90(0.64,1.26); 0.530 | 0.44(0.21,0.90); 0.024 |
| ≥50 | 205/235 | 123/177 | 24/39 | 0.75(0.41,1.37); 0.351 | 0.67(0.48,0.92); 0.014 | 0.89(0.50,1.61); 0.709 |
| Sex | ||||||
| Female | 122/152 | 84/90 | 9/25 | 0.45(0.20,1.00); 0.049 | 1.01(0.70,145); 0.967 | 0.42(0.19,0.93); 0.032 |
| Male | 184/177 | 104/161 | 23/32 | 0.69(0.39,1.23); 0.208 | 0.63(0.47,0.86); 0.003 | 0.84(0.48,1.47); 0.550 |
| Smoking | ||||||
| No | 146/169 | 81/118 | 14/21 | 0.77(0.38,1.57); 0.475 | 0.79(0.56,1.11); 0.180 | 0.84(0.42,1.69); 0.631 |
| Yes | 160/160 | 107/133 | 18/36 | 0.50(0.27,0.92); 0.025 | 0.74(0.54,1.02); 0.064 | 0.55(0.30,0.99); 0.046 |
| Drinking | ||||||
| No | 122/156 | 83/123 | 14/13 | 1.38(0.62,3.04); 0.428 | 0.91(0.64,1.30); 0.608 | 1.47(0.67,3.19); 0.334 |
| Yes | 184/173 | 105/128 | 18/44 | 0.39(0.21,0.69); 0.001 | 0.67(0.49,0.92); 0.012 | 0.43(0.24,0.76); 0.004 |
| Rs1143634 | CC | CT | TT | TT vs. CC | TT+CT vs. CC | TT vs. CT+CC |
| Age (years) | ||||||
| <50 | 128/133 | 45/47 | 1/6 | 0.34(0.09,1.25); 0.104 | 0.88(0.60,1.27); 0.484 | 0.34(0.09,1.26); 0.108 |
| ≥50 | 271/314 | 74/121 | 7/16 | 0.46(0.16,1.34); 0.155 | 0.64(0.44,0.93); 0.018 | 0.51(0.18,1.47); 0.212 |
| Sex | ||||||
| Female | 155/185 | 55/66 | 4/15 | 0.32(0.10,0.98); 0.046 | 0.87(0.58,1.29); 0.490 | 0.32(0.10,0.98); 0.045 |
| Male | 244/262 | 64/102 | 4/7 | 0.61(0.18,2.12); 0.440 | 0.67(0.47,0.95); 0.025 | 0.68(0.20,2.33); 0.534 |
| Smoking | ||||||
| No | 181/225 | 56/74 | 4/9 | 0.55(0.17,1.82); 0.330 | 0.90(0.61,1.32); 0.587 | 0.56(0.17,1.84); 0.341 |
| Yes | 218/222 | 63/94 | 4/13 | 0.31(0.10,0.98); 0.045 | 0.64(0.45,0.91); 0.014 | 0.35(0.11,1.07); 0.066 |
| Drinking | ||||||
| No | 170/206 | 45/79 | 3/7 | 0.52(0.13,2.04); 0.348 | 0.68(0.45,1.02); 0.060 | 0.57(0.15,2.22); 0.417 |
| Yes | 229/241 | 74/89 | 5/15 | 0.35(0.13,0.98); 0.046 | 0.80(0.57,1.13); 0.202 | 0.36(0.13,1.01); 0.053 |
Bold values are statistically significant (P < 0.05)
We explored the association between IL-1B gene polymorphisms and clinical characteristics (Table 4). The CC and/or GC genotype of rs1143623 polymorphism was correlated with decreased risk for patients with tumor size ≥ 5cm, TNM stage III+IV, and rectal cancer. Moreover, the CT genotype of rs1143634 polymorphism reduced the risk of colorectal adenocarcinoma compared to other subtypes of CRC. Similar result was found in the CT+TT genotype.
Table 4. The associations between IL-1B gene polymorphisms and clinical characteristics of colorectal cancer.
| Characteristics | Genotype distributions | |||
|
rs1143623 Tumor size |
GG | GC | CC | GC+CC |
| ≥5cm /<5cm | 139/167 | 73/115 | 8/24 | 81/139 |
| OR (95%CI); P-value | 1.0 (reference) | 0.83(0.57,1.20); 0.310 | 0.40(0.17,0.92); 0.027 | 0.70(0.49,1.00); 0.048 |
| CEA | ||||
| Positive/ Negative | 86/220 | 45/143 | 11/21 | 56/164 |
| OR (95%CI); P-value | 1.0 (reference) | 0.86(0.57,1.31); 0.480 | 1.34(0.62,2.90); 0.456 | 0.87(0.59,1.29); 0.499 |
| CA199 | ||||
| Positive/ Negative | 85/221 | 55/133 | 12/20 | 67/153 |
| OR (95%CI); P-value | 1.0 (reference) | 1.08(0.72,1.61); 0.723 | 1.56(0.73,3.33); 0.247 | 1.14(0.78,1.67); 0.504 |
| Differentiation | ||||
| Poor/Well+moderate | 43/263 | 32/156 | 4/28 | 36/184 |
| OR (95%CI); P-value | 1.0 (reference) | 1.26(0.76,2.07); 0.372 | 0.87(0.29,2.62); 0.809 | 1.20(0.74,1.94); 0.464 |
| TNM classification | ||||
| III+IV/I+II | 151/154 | 105/83 | 9/23 | 114/106 |
| OR (95%CI); P-value | 1.0 (reference) | 1.29(0.90,1.86); 0.171 | 0.40(0.18,0.89); 0.021 | 1.10(0.78,1.55); 0.601 |
| Adenocarcinoma | ||||
| Yes/No | 176/130 | 109/79 | 16/16 | 125/95 |
| OR (95%CI); P-value | 1.0 (reference) | 1.02(0.71,1.47); 0.920 | 0.74(0.36,1.53); 0.414 | 0.97(0.69,1.38); 0.873 |
| Rectal cancer | ||||
| Yes/No | 239/135 | 129/59 | 14/18 | 143/77 |
| OR (95%CI); P-value | 1.0 (reference) | 1.23(0.85,1.79); 0.267 | 0.44(0.21,0.91); 0.024 | 1.05(0.74,1.49); 0.788 |
| rs1143634 | CC | CT | TT | CT+TT |
| Tumor size | ||||
| ≥5cm /<5cm | 159/240 | 58/61 | 4/4 | 62/65 |
| OR (95%CI); P-value | 1.0 (reference) | 1.44(0.95,2.17); 0.085 | 1.51(0.37,6.12); 0.562 | 1.44(0.96,2.15); 0.074 |
| CEA | ||||
| Positive/ Negative | 103/296 | 37/82 | 2/6 | 39/88 |
| OR (95%CI); P-value | 1.0 (reference) | 1.30(0.83,2.03); 0.255 | 0.96(0.19,4.82); 0.958 | 1.27(0.82,1.98); 0.279 |
| CA199 | ||||
| Positive/ Negative | 120/279 | 30/89 | 1/7 | 31/96 |
| OR (95%CI); P-value | 1.0 (reference) | 0.78(0.49,1.25); 0.304 | 0.33(0.04,2.73); 0.282 | 0.75(0.48,1.19); 0.219 |
| Differentiation | ||||
| Poor/Well+moderate | 55/344 | 21/98 | 3/5 | 24/103 |
| OR (95%CI); P-value | 1.0 (reference) | 1.34(0.77,2.32); 0.296 | 3.75(0.87,16.1); 0.057 | 1.46(0.86,2.47); 0.160 |
| TNM classification | ||||
| III+IV/I+II | 200/199 | 58/61 | 6/2 | 64/63 |
| OR (95%CI); P-value | 1.0 (reference) | 0.95(0.63,1.43); 0.791 | 2.99(0.60,14.97); 0.164 | 1.01(0.68,1.51); 0.958 |
| Adenocarcinoma | ||||
| Yes/No | 243/156 | 55/64 | 2/6 | 57/70 |
| OR (95%CI); P-value | 1.0 (reference) | 0.55(0.37,0.83); 0.004 | 0.21(0.04,1.07); 0.063 | 0.52(0.35,0.78); <0.001 |
| Rectal cancer | ||||
| Yes/No | 287/112 | 87/32 | 7/1 | 94/33 |
| OR (95%CI); P-value | 1.0 (reference) | 1.06(0.67-1.68); 0.801 | 2.73(0.33-22.46); 0.330 | 1.11(0.71-1.75); 0.647 |
Bold values are statistically significant (P <0.05)
Finally, a prediction model of CRC was built using GRS and used to evaluate the effects of GRS on the CRC risk in a Chinese population (Table 5). Weighted GRS indicated the risk of CRC decreased in the tertiles quartile compared with the first quartile.
Table 5. The association of genetic risk score of IL-1B with risk of colorectal cancer.
| Variable | Case (n = 527) | Control (n = 639) | OR (95% CI) | P value | Adjusted OR (95% CI)* | P value | ||||||
| N (%) | N (%) | |||||||||||
| Weighted GRS | ||||||||||||
| First (0) | 227 (43.1%) | 227 (35.5%) | 1 | 1 | ||||||||
| Second (0) | 247 (46.9%) | 307 (51.2%) | 0.81(0.63, 1.03) | 0.087 | 0.81(0.63, 1.03) | 0.090 | ||||||
| Third (0-0.5) | 51 (9.7%) | 101 (15.8%) | 0.51(0.34, 0.74) | <0.001 | 0.51(0.34, 0.74) | <0.001 | ||||||
The genotyping for rs1143623 and rs1143634 was successful in: 526 cases and 637 controls. *Adjusted for sex and age. Bold values are statistically significant (P < 0.05).
Survival analysis of CRC patients with IL-1B gene rs1143634 or rs1143623 polymorphism
Considering the protective roles of the two polymorphisms in CRC patients, we aimed to explore the relationship between SNPs and the prognosis of CRC patients. The 96 CRC patients enrolled in the first year of this study were followed up for a median period of 39 months. For rs1143623 polymorphism, the Kaplan-Meier single factor analysis showed that CRC patients carrying CC genotype versus GG genotype enjoyed longer OS (HR, 0.47, 95%CI, 0.23-0.97; log-rank P = 0.041, Figure 3). However, no difference in OS was found between the CRC patients carrying IL-1B rs1143634 TT and CC genotypes (HR, 0.78, 95%CI, 0.30-2.04; log-rank P = 0.649, Figure 3).
Figure 3.
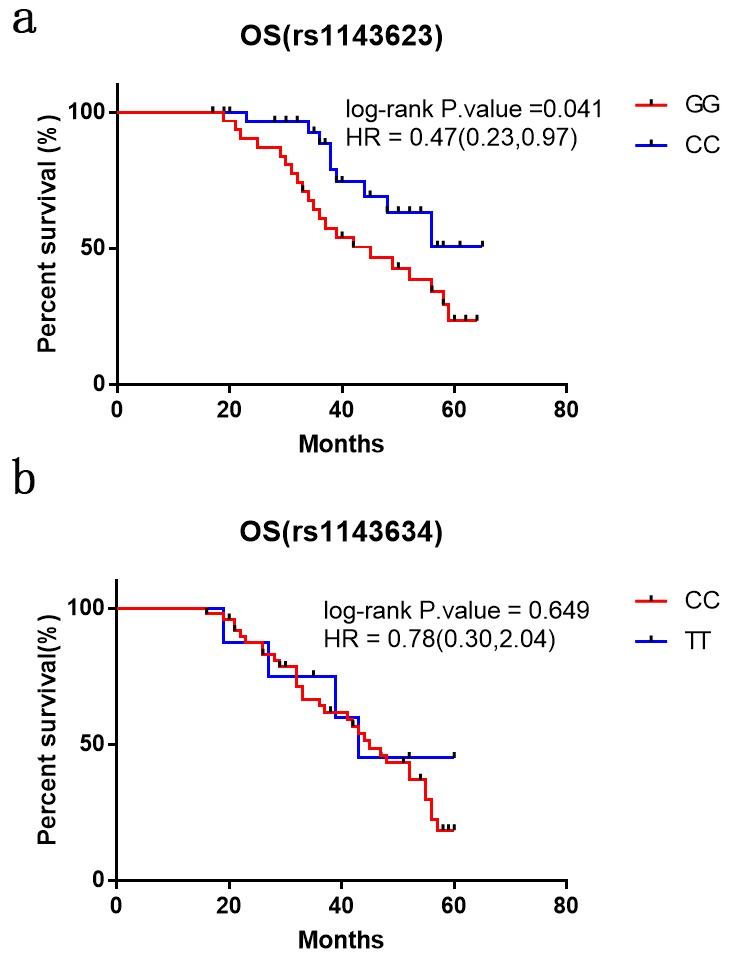
Kaplan–Meier analysis of overall survival of CRC patients with IL-1B rs1143623 and rs1143634 polymorphisms. Differences in the overall survival of the patients with different genotypes of polymorphisms (a) rs1143623 and (b) rs1143634.
DISCUSSION
The two IL-1B gene variants (rs1143634, rs1143623 polymorphisms) were found to decrease risk of CRC. Stratified analyses of age, sex, smoking, and drinking also showed positive findings. The rs1143623 polymorphism was associated with a larger tumor size, and TNM III+IV stages in CRC patients. Furthermore, the CC genotype of IL-1B gene rs1143623 polymorphism was related to better OS of CRC.
Many studies explored the association between IL-1B gene polymorphisms and CRC risk, but report conflicting findings. A prospective Danish case-cohort showed IL-1B gene rs1143623 polymorphism was associated with risk of CRC [10], but found no interaction between this SNP and diet or lifestyle factors [10]. A study from Russia observed similar findings in rectal cancer [11], and provided rs1143623 polymorphism was implicated in rectal cancer development, but not in CRC, gastric cancer, or ovarian cancer [11]. However, no association between rs1143634 polymorphism and CRC risk was found in a Caucasian population [12]. Burada et al. also failed to replicate significant finding in Romania [13], and found no positive results in the tumor site subgroup of CRC [13]. However, IL-1B gene rs1143634 polymorphism was associated with increased risk for CRC in a Chinese Han population [14]. Inconsistent with the above studies, our study showed both rs1143634 and rs1143623 polymorphisms of IL-1B gene provided protective roles in CRC development. We thought the conflict among the above studies may be attributed to the following factors. Firstly, genetic heterogeneity for CRC existed among races. Secondly, clinical heterogeneity was a potential factor. For example, the study from Russia only obtained significant findings in rectal cancer [11], while our study observed positive association in CRC, and the tumor sites were different between two studies. Thirdly, the sample sizes varied among these studies. Fourthly, diverse lifestyles and diets may also contribute to it. Fifthly, the differences of inclusion and exclusion criteria may contribute to the above conflict findings. The 244 CRC patients from Russia were verified by two experienced pathologists [11], but the study from Romania [13] involved standard diagnostic procedures including physical, digital rectal examination, fecal occult blood tests, sigmoidoscopy, colonoscopy, bariumenema, and imaging. The cases and controls from Denmark selected from The Diet, Cancer and Health Study did not mention the inclusion or exclusion criteria [10]. The study from China [14] indicated all CRC patients were diagnosed and histologically identified. To our knowledge, we are the first from China to uncover the protective effects of IL-1B gene rs1143623 and rs1143634 polymorphisms on CRC development.
Our stratified analyses suggested IL-1B gene rs1143623 and rs1143634 polymorphisms decreased the risk of CRC among females, smokers and drinkers, indicating these groups were more prone to the risk factors. However, these results should be interpreted with caution given the small sample size. Furthermore, we lso revealed the significant association between CC and/or GC genotype of rs1143623 polymorphism and clinical characteristics of CRC (tumor size ≥5cm, TNM III+IV stage and rectal cancer). No significant association between rs1143623 polymorphism and colon cancer was found, suggesting this SNP may be a specific locus for rectal cancer. Last but not least, the rs1143623 polymorphism was related to longer OS of CRC patients. Our data suggest rs1143623 and rs1143634 polymorphisms play protective roles in the pathogenesis of CRC but the underlying mechanisms are unclear. Bioinformatics analysis of the TCGA database showed the IL-1B gene mRNA levels were significantly increased in CRC patients compared with the controls. In addition, data from the International HapMap Project and GTEx portal showed IL-1B rs1143623 and rs1143634 polymorphisms could decrease the IL-1B expression. It is reasonable to assume that IL-1B rs1143623 and rs1143634 polymorphisms may contribute to the risk of CRC by altering the IL-1B expression.
This study has several limitations. Firstly, the sample size was not large enough, especially for the subgroup analyses. Secondly, the pathogenesis of CRC cannot be explained by only two SNPs in IL-1B gene and should be confirmed by other SNPs and gene variants. Thirdly, possible gene-gene or gene-environment interactions were not investigated. Fourthly, the findings may be inapplicable to other races. Fifthly, the association between these two SNPs and IL-1B protein should be explored. Sixthly, we did not follow up all patients due to the staff shortage.
In conclusion, IL-1B gene rs1143623 and rs1143634 polymorphisms are associated with decreased risk for CRC. Further studies in other ethnicities are needed to validate this finding.
MATERIALS AND METHODS
Study subjects
A total of 527 CRC patients were recruited at the Jiangsu Provincial of Traditional Chinese Medicine and the Third Affiliated Hospital of Nantong University. The diagnosis of CRC was confirmed by histopathological examination of the biopsy. The individuals with familial polyposis, inflammatory bowel disease or metastatic carcinoma were excluded. CRC patients were staged according to the American Joint Committee on Cancer/International Union against Cancer tumor-node-metastasis (TNM) staging system. The 639 healthy controls were selected from the volunteers undergoing general health check-up in the above two hospitals. The medical and follow-up data of patients, including age, gender, lymph node metastases, TNM stage, and location and differentiation degree of primary tumor were retrieved from hospital records and interviews. As for lifestyle factors, alcohol drinker was defined as an individual consuming alcohol more than once per day for ≥3 months, while smoker was defined as smoking at least once a day for ≥1 year.
This study was approved by the institutional review broads of the two hospitals and conducted in accordance with the Helsinki declaration. Written informed consent was obtained from all participants.
Bioinformatic analysis
Data of IL-1B expression in CRC patients and healthy controls was extracted from GEPIA (http://gepia.cancer-pku.cn/index.html) [15], which is based on public data available from TCGA and is a web server for cancer and normal gene expression profiling and interactive analyses.
Genotype and mRNA expression data of the two IL-1B gene polymorphisms were cited from the International HapMap Project and GTEx portal (https://www.gtexportal.org/home/) [16], respectively.
DNA extraction and Genotyping
In brief, 2mL of peripheral blood was collected in vacuum tubes containing 5% EDTA and frozen at -80 °C until use. Genomic DNA was extracted using a DNA Purification Kit (Tiangen Biotech) according to the manufacturer’s instructions. and the concentration and purity were estimated using NanoDrop at two optical density (OD) wavelengths 260 and 280 nm. Genotyping was done by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOFMS) using a MassARRAY system (Sequenom, San Diego, CA, USA). Completed genotyping reactions were spotted onto a 384-well spectroCHIP (Sequenom) using a MassARRAY nano dispenser (Sequenom) and analyzed by MALDI-TOFMS. Genotype were called in real time on MassARRAY RT 3.1 (Sequenom) and analyzed on MassARRAY Typer 4.0 (Sequenom). For quality control, 10% of randomly-selected samples were analyzed repeatedly.
Statistical analysis
All statistical analyses were performed on the SAS package (var. 9.1.3; SAS Institute, Cary, NC, USA). Deviation from the Hardy-Weinberg equilibrium (HWE) between observed and expected frequencies among controls was investigated using goodness-of-fit Chi-square test. Differences in demographic characteristics and lifestyle-related factors between cases and controls were compared by Chi-square test (for categorical variables) and Student’s t-test (for continuous variables). The impacts of different genotypes on other parameters were further evaluated via one-way analysis of variance (ANOVA). The odds ratio (OR) and 95% confidence interval (CI) were calculated to evaluate the SNPs-associated disease risk by binary logistic analysis. The effect size of each SNP was estimated using crude ORs. The weighted genetic risk scores (GRS) was equivalent to the sum of (log OR of SNP) × (number of risk alleles carried by the individual) across two SNPs. The GRS was subsequently divided into tertiles based on the normalized value. The association between GRS and CRC risk was then calculated by binary logistic regression. Univariate survival analyses were conducted via the Kaplan-Meier method. The overall survival (OS) was defined as date from diagnosis (colonoscopy or surgery) to death or the date last known alive. P ≤ 0.05 was considered statistically significant [17].
ACKNOWLEDGMENTS
We thank all participants of the Tianjin Brain Study.
Footnotes
AUTHOR CONTRIBUTIONS: Conceptualization, Q.H.H. and B.C.Q.; Methodology, Z.D., Q.H.H. and B.C.Q.; Validation, Q.H.H. and B.C.Q.; Formal Analysis, Q.H.H. and B.C.Q.; Investigation, Q.H.H. and B.C.Q.; Resources, Q.H.H.; Data Curation, Z.D. and Q.H.H.; Writing-Original Draft Preparation, Z.D. and Q.H.H.; Writing-Review and Editing, Z.D., Q.H.H. and B.C.Q.
CONFLICTS OF INTEREST: The authors declare that there are no conflicts of interest.
FUNDING: This study was supported by the Project of Administration of Traditional Chinese Medicine of Jiangsu Province of China (JD201708).
REFERENCES
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Sandhu MS, Dunger DB, Giovannucci EL. Insulin, insulin-like growth factor-I (IGF-I), IGF binding proteins, their biologic interactions, and colorectal cancer. J Natl Cancer Inst. 2002; 94:972–80. 10.1093/jnci/94.13.972 [DOI] [PubMed] [Google Scholar]
- 3.Kerr J, Anderson C, Lippman SM. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017; 18:e457–71. 10.1016/S1470-2045(17)30411-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moossavi S, Bishehsari F. Inflammation in sporadic colorectal cancer. Arch Iran Med. 2012; 15:166–70. [PubMed] [Google Scholar]
- 5.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011; 144:646–74. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 6.Balkwill FR, Mantovani A. Cancer-related inflammation: common themes and therapeutic opportunities. Semin Cancer Biol. 2012; 22:33–40. 10.1016/j.semcancer.2011.12.005 [DOI] [PubMed] [Google Scholar]
- 7.Lasry A, Zinger A, Ben-Neriah Y. Inflammatory networks underlying colorectal cancer. Nat Immunol. 2016; 17:230–40. 10.1038/ni.3384 [DOI] [PubMed] [Google Scholar]
- 8.Dinarello CA. Why not treat human cancer with interleukin-1 blockade? Cancer Metastasis Rev. 2010; 29:317–29. 10.1007/s10555-010-9229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Wang K, Han GC, Wang RX, Xiao H, Hou CM, Guo RF, Dou Y, Shen BF, Li Y, Chen GJ. Neutrophil infiltration favors colitis-associated tumorigenesis by activating the interleukin-1 (IL-1)/IL-6 axis. Mucosal Immunol. 2014; 7:1106–15. 10.1038/mi.2013.126 [DOI] [PubMed] [Google Scholar]
- 10.Andersen V, Holst R, Kopp TI, Tjønneland A, Vogel U. Interactions between diet, lifestyle and IL10, IL1B, and PTGS2/COX-2 gene polymorphisms in relation to risk of colorectal cancer in a prospective Danish case-cohort study. PLoS One. 2013; 8:e78366. 10.1371/journal.pone.0078366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kutikhin AG, Yuzhalin AE, Volkov AN, Zhivotovskiy AS, Brusina EB. Correlation between genetic polymorphisms within IL-1B and TLR4 genes and cancer risk in a Russian population: a case-control study. Tumour Biol. 2014; 35:4821–30. 10.1007/s13277-014-1633-6 [DOI] [PubMed] [Google Scholar]
- 12.Gunter MJ, Canzian F, Landi S, Chanock SJ, Sinha R, Rothman N. Inflammation-related gene polymorphisms and colorectal adenoma. Cancer Epidemiol Biomarkers Prev. 2006; 15:1126–31. 10.1158/1055-9965.EPI-06-0042 [DOI] [PubMed] [Google Scholar]
- 13.Burada F, Dumitrescu T, Nicoli R, Ciurea ME, Angelescu C, Mixich F, Ioana M. IL-1RN +2018T>C polymorphism is correlated with colorectal cancer. Mol Biol Rep. 2013; 40:2851–57. 10.1007/s11033-012-2300-x [DOI] [PubMed] [Google Scholar]
- 14.Wang N, Wang L, Yang H, Zhang HQ, Lan B, He X, Jin TB, Kang LL, Chen C. Multiple genetic variants are associated with colorectal cancer risk in the Han Chinese population. Eur J Cancer Prev. 2015; 24:1–5. 10.1097/CEJ.0000000000000012 [DOI] [PubMed] [Google Scholar]
- 15.Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017; 45:W98–102. 10.1093/nar/gkx247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loo LW, Lemire M, Le Marchand L. In silico pathway analysis and tissue specific cis-eQTL for colorectal cancer GWAS risk variants. BMC Genomics. 2017; 18:381. 10.1186/s12864-017-3750-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gong J, Mei S, Liu C, Xiang Y, Ye Y, Zhang Z, Feng J, Liu R, Diao L, Guo AY, Miao X, Han L. PancanQTL: systematic identification of cis-eQTLs and trans-eQTLs in 33 cancer types. Nucleic Acids Res. 2018; 46:D971–76. 10.1093/nar/gkx861 [DOI] [PMC free article] [PubMed] [Google Scholar]


