Abstract
Text messages may sustain post-counseling gains in behavioral improvements and reduce HIV/STI incidence. However, their effectiveness may depend on the messages’ time perspective and characteristics of the individual. We evaluated the impact of time perspective on a text messaging intervention designed to maintain improvements in safer sex practices among drug-using and non-drug-using female sex workers (FSWs) in Tijuana (n=141) and Cd. Juarez (n=129), Mexico. FSWs received the efficacious Mujer Segura intervention, and were randomized to receive safer sex maintenance text messages with either a short-term or future-oriented time perspective. The outcome was HIV/STI incidence rate over 6-month follow-up. In Tijuana, combined HIV/STI incidence density was lower among FSWs in the FUTURE group (31.67 per 100 py) compared to women in the SHORT-TERM group (62.40 per 100 py). Conversely, in Cd. Juarez, HIV/STI incidence density was lower (although non-significant) among FSWs in the SHORT-TERM group (19.80 per 100 py) compared to those in the FUTURE group (35.05 per 100 py). These findings suggest that future-oriented text messages may sustain post-counseling improvements in sexual risk behavior among FSWs, but findings may vary by FSWs’ characteristics (e.g., drug use), and by region and context.
Keywords: Female sex workers, Mexico, texting intervention, behavior maintenance, time perspective
Introduction
HIV prevalence among Mexican female sex workers (FSWs) along the US-Mexico border has been reported as 6.0% (Patterson et al., 2008b) compared to the Mexican national average of 0.1% among women age 15–49 years (UNAIDS, 2016). In 2006–2008, a brief sexual risk reduction intervention known as Mujer Segura was conducted among FSWs in Tijuana and Ciudad (Cd.) Juarez and found to be efficacious in terms of reducing HIV/STI incidence and increasing condom use with clients over a six-month period (Patterson et al., 2008a). However, treatment effects of health behavior interventions erode, often with lapses in positive behavior change occurring more than 50% of the time within 6 months, perhaps because the processes that sustain behavior change differ from those that favor behavior acquisition (Berrigan et al., 2003; Foster et al., 2010; Ngugi et al., 2007; Vrijens et al., 2008; Yadav et al., 2005). Text messaging interventions that reinforce safer sex counseling messages and provide behavioral maintenance strategies may help sustain post-counseling improvements in risk behavior and reduce HIV/STI incidence. However, in marginalized populations such as FSWs, the effectiveness of these text messages may depend on their time perspective (short-term vs. future-oriented) and characteristics of the individual receiving the texts (e.g., drug user vs. non-drug user).
The long-term health benefits of engaging in safer sex practices (e.g., consistent use of condoms) include longer life expectancy, reduced risk of contracting HIV and other sexually transmitted infections (STIs), and decreased risk of developing certain types of cancers (e.g., cervical) (Center for Disease Control and Prevention, n.d.). Despite the long-term benefits of safer sex, many FSWs report inconsistent use of condoms with male clients, even after participating in a sexual risk reduction intervention (Bailey & Figueroa, 2017; Ngugi et al., 2007; Yadav et al., 2005; Zhang et al., 2017). Adding to this problem is the lack of behavioral interventions designed to maintain positive behavior changes associated with efficacious HIV/STI prevention interventions, particularly among FSWs (Feldman et al., 2014).
There are many reasons why FSWs have difficulty maintaining safer sex practices with their clients over time. Descriptive studies have identified the following reasons for non-maintenance of safer sex practices (i.e., lapses in condom use) with clients, including low perception of risk based on a client’s appearance and perceived wealth, blurred relationship lines between client versus regular male partner, feelings of closeness and intimacy with certain clients, use of alcohol or drugs with clients, offers of higher rates of pay for sex without condoms, as well as lack of work experience and risk awareness among some FSWs (Bailey & Figueroa, 2017; Davis et al., 2009; Duncan et al., 2010; Eldemire-Shearer & Bailey, 2008; Ngugi et al., 2012; Syvertsen et al., 2013). What continues to be missing from the literature is a psychological or cognitive construct that provides a basis for understanding sexual risk behavior and lapses in condom use among FSWs in the context of having knowledge about the long-term health benefits of maintaining safer sex practices with clients.
Future time perspective is a cognitive-psychological construct that may be useful in terms of understanding non-maintenance of safer sex practices among FSWs who have participated in a sexual risk reduction intervention program (Ngugi et al., 2007). A short-term time perspective entails “considering only a limited period into the future” (Teuscher & Mitchell, 2011). It has been associated with a focus on present needs, which for FSWs is likely to involve providing for basic necessities, such as food, shelter, and clothing for oneself and dependent children. In the case of FSWs who are drug or alcohol-dependent, present needs may entail the immediate need for drugs or alcohol. A short-term time perspective has also been associated with “negative attitudes toward the future” (e.g., hopelessness), as well as a range of adverse health outcomes, including addiction behaviors, risky decision-making, impulsivity, delinquency, and criminal offending (Teuscher & Mitchell, 2011). In contrast, a future-oriented time perspective has been defined as a “general orientation to the future that includes planning for future goals,” often while deferring immediate needs or wants (Teuscher & Mitchell, 2011; Zimbardo & Boyd, 1999). A future time perspective has been associated with positive health outcomes.
A number of studies have reported that substance use is strongly associated with having a short-term time perspective (Teuscher & Mitchell, 2011). Research has documented more short-term and less future-oriented time perspectives among substance-using populations, including alcohol dependent and hazardous drinkers (MacKillop et al., 2007), drug and alcohol treatment inpatients (Klingemann, 2001), and opiate-dependent individuals (Teuscher & Mitchell, 2011). In our previous work conducted with participants in the Mujer Segura intervention in Tijuana and Cd. Juarez, we identified high rates of substance use (Patterson et al., 2006). Among 924 FSWs, 93% reported alcohol consumption in the past month, of whom 77% met criteria for hazardous drinking. Approximately half of the FSWs reported use of ‘heavy’ drugs in the past month (i.e., cocaine, methamphetamine, heroin, or a combination), and 29% reported injection drug use. These findings, considered in the context of the time perspective literature, indicate the important role that substance use may play in determining the influence of time perspective variations on the efficacy of safer sex behavioral maintenance interventions for FSWs.
FSWs, especially those in low- to middle-income countries (LMIC) like Mexico, may also be susceptible to a shortened time perspective because they live and work in disadvantaged environments characterized by violence, stigma, discrimination, economic insecurity, substance abuse, and other risk-related behaviors (Basnyat, 2014; Gurnani et al., 2011). We were unable to identify any studies of time perspective among FSWs in LMIC or developed countries; however, there is a substantial body of literature that links time perspective to a range of problem behaviors, including substance use disorders, sexual risk behavior, pathological gambling, eating disorders, and Internet addiction (Abousselam et al., 2016; Cheong et al., 2014; Garcia et al., 2017; Hodgins & Engel, 2002; Iwanicka et al., 2017; Kim et al., 2017; Sailer et al., 2014). In all of these studies, a short-term time perspective has been associated with harmful behaviors and poor health outcomes, while a future-oriented time perspective has been shown to have a protective effect on health behaviors and psychological well-being.
The concept of time perspective is related to, yet different from the construct of delay discounting for which there is a large body of literature (Amlung et al., 2017; Dierst-Davies et al., 2011; Kirby et al., 1999). Studies of delay discounting are typically conducted in laboratory settings, and assess an individual’s preference for obtaining a small reward immediately over a larger reward offered at a later time (Teuscher & Mitchell, 2011). In the majority of studies, a steep or heightened rate of discounting is associated with a shortened time perspective and more adverse health outcomes in high-risk populations, particularly drug users (Camchong et al., 2011; Johnson et al., 2015a; Johnson et al., 2015b; Kirby & Petry, 2004; Koffarnus et al., 2016; Petry & Casarella, 1999). The present study did not assess delay discounting, but rather focused solely on time perspectives. Although delay discounting may be a relevant issue for FSWs, the present study focused on time perspective because it is influenced by external forces (e.g., life stressors and events) (Dany et al., 2016; Holman et al., 2016), and thus may be more amenable to change through psychological and cognitive interventions. In contrast, delay discounting, which has been described as internal and a personality trait (Albein-Urios et al., 2014; Anokhin et al., 2015) may be more difficult to change in the context of ongoing drug use (Hulka et al., 2015; Teuscher & Mitchell, 2011).
The aim of this study was to evaluate the impact of messages differing by time perspective (short-term vs. future-oriented) on a real-time text messaging intervention designed to maintain behavioral improvements in safer sex practices among drug-using FSWs (i.e., injection drug users and non-injection users of heavy drugs, such as heroin and cocaine) and their non-drug using FSW counterparts in a LMIC. The intervention was conducted in Tijuana and Cd. Juarez, two Mexico-US border cities that continue to be sites of escalating HIV epidemics (Brouwer et al., 2006; Iñiguez-Stevens et al., 2009). Sexually-risky FSWs initially received the efficacious Mujer Segura intervention and were randomized to receive safer sex maintenance text messages (over a six-month period) with either a short-term or future-oriented time perspective. We hypothesized that FSWs who received text messages with a short-term time perspective would have fewer incident cases of HIV/STIs compared to FSWs who received text messages with a future-oriented time perspective, regardless of drug use status. The value of short-term versus future-oriented time perspective text messages in terms of sustaining improvements in post-counseling behavior change was measured by their ability to reduce HIV/STI incidence density at 6-month follow-up.
Methods
Participants and Setting
Participants were 302 FSWs recruited in Tijuana and Cd. Juarez, Mexico for a randomized controlled trial of a brief, single-session sexual risk reduction intervention with a text messaging component (known as Mujer Saludable Siempre [MSS] or Healthy Women Always), which was designed to maintain improvements in sexual behavior change with male clients over time. Consistent with our study aims, half of the sample was randomly assigned to receive safer sex maintenance texts with a short-term time perspective and the other half was randomly assigned to receive texts with a future-oriented time perspective. To be eligible for the study, a woman had to be biologically female, at least 18 years of age, self-identify as a female sex worker, report having traded sex for drugs, money, shelter or other material benefit in the previous 2 months, have had unprotected vaginal or anal sex with a client at least once during the previous 2 months, have no previous HIV-positive test result (either tested negative or not ever tested), own a cell phone, and agree to be tested for HIV and STIs at baseline and follow-up assessments.
Our primary analysis compared FSWs in the short-term text messages condition with those in the future-oriented text messages condition in terms of laboratory confirmed sexually transmitted infections (HIV/STIs), while controlling for drug use status (heavy drug users or IDUs vs. non-drug users). Injection drug use and heavy drug use were assessed over the past month. Heavy drug use was defined as non-injection use of methamphetamine, cocaine, heroin, or a combination of these drugs. The baseline and six-month follow-up data used in these analyses were collected between January 2016 and July 2016. All study procedures were approved by ethics committees at the University of California, San Diego, Xochicalco University in Tijuana, and SADEC-FEMAP in Cd. Juarez. Written informed consent was obtained from all participants.
Recruitment
Time-location sampling was used to recruit 302 FSWs (~150 per site). This sampling strategy had previously been effective in recruiting difficult-to-reach populations, including FSWs and FSW-IDUs, in both Tijuana and Cd. Juarez (Patterson et al., 2008b; Strathdee et al., 2013). Outreach workers at each site compiled a map of bars, brothels, hotels and motels, shooting galleries, alleys, and street corners, and they subsequently canvassed those venues to locate prospective participants. Women who appeared eligible and were willing to speak with our outreach workers were informally asked a few screening questions (e.g., age, sex worker status), and if interested in our study were provided a study card and asked to present it when they visited our study offices. Formal eligibility screening was conducted in-office and included questions that matched study eligibility criteria (see Participants and Setting).
Participants were recruited with the target goal of achieving one-third membership in each of the following drug use groups in each site: injection drug use, non-injection drug use, and non-drug use. Interested women were referred for a screening interview at our office in Tijuana’s Zona Roja (red light district) and to our office at Salud y Desarollo Comunitario de Ciudad Juarez, A.C. and Federación Méxicana de Asociaciones Privadas, A.C. (SADEC-FEMAP) located in downtown Cd. Juarez. Women who were eligible for the study were scheduled for a two-hour baseline visit, which included the consent procedure, a 60-minute face-to-face interview administered via CAPI (Nova Software, MD, USA), the 30-minute Mujer Segura safer sex counseling session, and the 15-minute safer injection practices component for FSWs who reported injection of drugs in the past month (Patterson et al., 2008a). FSWs were reimbursed the equivalent of $30 USD for the baseline interview and counseling session.
At both sites, MSS had a staff psychologist available to immediately interview and intervene with any participant who was moderately to extremely depressed (based on a score of 20 or more on the Beck Depression Inventory, BDI-II) or was threatening self-harm. Psychologists referred participants to the nearest public health center for mental health care follow-up. In Tijuana, participants were referred to the Institute of Psychiatry operated by the state of Baja California. In Cd. Juarez, participants were referred to Instituto Estatal de Salud Mental.
Overview of Mujer Segura Counseling Session
All FSWs received the 30-minute efficacious Mujer Segura intervention (Patterson et al., 2008a), which combines principles of Motivational Interviewing (MI), Social Cognitive Theory (SCT), and Theory of Reasoned Action (TRA) (Ajzen & Fishbein, 1980; Bandura, 1986, 1989; Beck, 1967, 1976; Miller & Rollnick, 1991). To promote readiness for behavior change, counselors queried participants about their risk behaviors with clients, as well as their perceived need to change, self-efficacy for change, and stated intentions to change. Motivational interviewing techniques were used to elicit information on personal motivations for behavior change. Counselors helped participants to develop a plan of action, define achievable goals, and problem-solve barriers to safer sex. Behavior change strategies were discussed, negotiation of safer sex was role played, proper use of condoms was demonstrated, and free condoms were distributed. Positive feedback was used throughout to promote participant self-efficacy. Because it would have been unethical to withhold education on safer injection practices from those who injected drugs, MSS counselors conducted a 15-minute counseling session that provided information on the dangers of sharing “works,” the location of local syringe exchange programs, and methods for cleaning ‘works’ with bleach.
Description of time perspective text messages.
Upon completion of the Mujer Segura counseling session, the participant was then randomized to one of two text-message-based maintenance conditions (SHORT-TERM vs. FUTURE) (See Statistical analysis for details). Text messages were developed by our bi-national team of investigators, and were designed to capture cognitive and behavioral processes for maintaining safer sex practices (Voils et al., 2014) with clients and to reinforce safer sex skills learned in the Mujer Segura counseling session. Previously-established cognitive, behavioral, and motivational strategies (Beck, 1976; Beck, 2007) were applied to the maintenance of safer sex and injection practices. The feasibility of using text messages to deliver a health intervention in a difficult-to-reach population of drug users was demonstrated by team members in a previous study (Montoya et al., 2014).
The success of text messaging programs is dependent upon careful attention to the design of text messages that make them more engaging to the target population (Bull & Ezeanochie, 2016; Devine et al., 2015; Head et al., 2013). Important aspects of text message design that have been identified in previous studies include a strong theoretical foundation and approved content for text messages, developing messages that are both tailored and targeted to demographic and psychosocial variables, personalized to the participant’s situation, individualized, flexibility in delivery of the message (number, frequency, and schedule of text delivery), two-way communication between the project and the participant, as well as gain-framed and loss-framed messages (Bull & Ezeanochie, 2016; Devine et al., 2015; Head et al., 2013).
Our research team conducted focus groups with 25 FSWs in Tijuana where participants provided feedback on the content and relevance of the text messages, and indicated their preferences for each of the text message features described above (e.g., delivery schedule, bi-directional communication, customized delivery of messages). FSW focus groups also helped us to ensure that the language in each text message was clearly worded, culturally-sensitive, appealing, relevant to FSWs, consistent with Mujer Segura counseling messages, and did not pose a risk for disclosure of their sex worker status (an issue that was identified in the focus groups). To protect FSWs’ privacy and confidentiality, all text messages referred to clients generically as “partners” and syringes were referred to euphemistically as “personal items”. All text messages were translated and back-translated in Spanish.
Text messages with a short-term time perspective focused on HIV prevention rewards that are rooted in the present, with little to no concern for future rewards associated with maintaining consistent condom use with clients. Examples (translated to English for this manuscript) of short-term safer sex behavioral maintenance text messages include: “Friend, before you go out, think about all the advantages of using condoms with your sexual partners. Doing so will help to keep you safe tonight.”; “Friend, call your best girlfriend today and talk about the benefits of using condoms. Sharing will strengthen your friendship bond.” An example of a “short-term” safer injection maintenance text message for FSWs who inject drugs is “Friend, if you have trouble finding free clean personal items, tell yourself, ‘no choice’, I will pay for new ones rather than share with others.”
Text messages with a future-oriented time perspective focused on HIV prevention rewards that point to a good future, and a life marked by long-term goal achievement. Examples of future-oriented safer sex behavioral maintenance text messages include: “Friend, condoms cost money, but what a great way to invest in your long-term health”; “Friend, if you have sex without a condom, remember that you have the skills to get back on track. Think of how much your long-term health means to your family.” An example of a future-oriented safer injection maintenance text message for FSWs who inject drugs is “Friend, stick to your plan and never borrow others’ personal items. Avoiding unhealthy behaviors now will pay off in the years to come.”
Text messages were delivered using Twilio, a cloud communications service that allows software developers to create web-based interfaces that automate the sending and receiving of text messages. Our systems engineer designed an interface that allowed counselors to schedule the delivery of text messages on days and times specified by the participant. All participants received two text messages per day for 5 days each week (including weekends if requested by the participant) over a 6-month period. A two-way text messaging protocol was adopted whereby participants received messages and were asked to reply to each one with an “S” or “Si” (yes) to indicate that they had read the message.
Measures
Four broad categories of covariates, selected on the basis of previous research on time perspective among disadvantaged populations, were examined in these analyses (Abousselam et al., 2016; Cheong et al., 2014; Iwanicka et al., 2017). They included socio-demographic factors, work context variables, texting habits, and selected psychosocial and behavioral characteristics of the FSWs. HIV/STI incidence rate over a six-month period was treated as the outcome of interest.
Socio-Demographics
Age, number of years having worked as a sex worker, and number of years of texting experience were treated as continuous variables. Partner status (has a spouse or steady partner = 1, no spouse or steady partner = 0), level of education grade school or less (yes = 1, no = 0), whether the FSW lives with at least one child under 18 years (yes = 1, no = 0), whether FSW lives with a spouse or steady partner (yes = 1, no = 0), and sex work is main source of income (yes=1, no = 0) were treated as dichotomous variables. Monthly income from all sources was reported as a categorical variable and collapsed into a binary variable (1=≥3500 pesos, 0= ≤3499 pesos).
Substance Use Factors
Severity of alcohol use during the last year was measured by the 10-item Alcohol Use Disorders Test (AUDIT-10) (Saunders et al., 1993). The AUDIT is a reliable alcohol screening instrument that measures frequency and quantity of alcohol consumption. Summary scores were used to create a dichotomous variable (hazardous drinking = 1, non-hazardous drinking = 0), where a score of 8 or more for women indicated hazardous drinking (Conigrave et al., 1995; Saunders et al., 1993). Participants were also asked about their use of common street drugs (e.g., cocaine, methamphetamine, heroin) during the past month. Frequency of use was rated on a scale from 1 (never) to 6 (every day), and responses were recoded as 1 (does use) or 0 (does not use). Participants were also asked to report the method of administration for each of the drugs mentioned above. Injection drug use in the past month was coded 1= yes, 0 = no. Injection needle sharing combined two items that asked the participant how often she injected with a borrowed needle or used a syringe that someone else had already used. Response categories were coded as 1 (once in a while to very often) and 0 (never). Binge use of drugs in the past month (i.e., “used large quantities of a drug for a period of time – until you ran out or just couldn’t physically do it anymore”) was coded 1 = yes or 0 = no.
A dichotomously-scored variable was computed to represent heavy drug use or IDU (henceforth referred to as “heavy drugs/IDU”) in the past month. Participants who injected drugs or reported non-injection use of methamphetamine, cocaine, heroin, or a combination of these drugs were coded 1 (used heavy drugs/IDU) and 0 (no drug use) in the past month. Use of alcohol or drugs before or during sex with clients was assessed using two separate questions that asked participants how often in the past month they had used alcohol or drugs before or during sex with a client. Response categories (never, sometimes, often, always) were recoded (1 = did use, 0 = did not use).
Context or Micro-Level Environment
Participants were presented with a list of nine types of sex worker (barmaid, dance hostess, taxi girl, brothel worker, street worker, lover, call girl or escort, companion for parties and vacations, other) and asked to indicate the one that best described their work situation. Sex worker type was dichotomized as street worker = 1, all other types = 0. Another question asked the FSW how many of her clients in the past 6 months were Mexican. Participants who responded most or all Mexican clients were coded 1, other response categories were coded 0. Participants were also queried regarding the number of times they had ever been arrested for sex work. Number of arrests was recoded as a dichotomous variable (ever arrested = 1, never arrested = 0).
Sexual Risk Behaviors
The number of unprotected vaginal and anal sex acts with male clients in the past month was computed by subtracting the total number of times a condom was used during vaginal and anal sex from the total number of vaginal and anal sex acts. Participants also reported the numbers of male client partners (regular and non-regular) in the past month. These numbers were summed to create a variable for total number of clients in the past month. Amount of money earned for engaging in condomless vaginal or anal sex was asked in separate questions (On average, how much money do you earn in pesos/US dollars each time you perform vaginal/anal sex without a condom?).
Psychosocial Factors
The 21-item Beck Depression Inventory (BDI-II), which has undergone extensive reliability and validation studies was used to measure depressed mood (Beck, 1967, 1976). A summary score for the BDI was computed. A score of 20 or more on the BDI-II defined moderate-to-severe levels of clinical depression (Beck et al., 1996). Currently under the care of a psychologist or psychiatrist was coded as yes = 1 and no = 0. Five items from the Personal Feelings Questionnaire (PFQ2) were used to assess shame and guilt in relation to stigmatized identities (Harder & Zalma, 1990). The participant was presented with five adjective checklist items and asked to rate on a 4-point scale (never to continuously or almost continuously) how common the feeling has been for her in the past six months (i.e., humiliation, embarrassment, deserving of criticism, remorse, regret). Forced or coerced sex perpetrated by clients was measured by a single item (i.e., In the past six months, how many different times have you been forced or coerced into having sex against your will with a client?). Number of times forced or coerced into sex by client was recoded as a dichotomous variable (forced/coerced sex = 1, no forced/coerced sex = 0).
HIV and STI Testing
HIV/STI testing was performed on all participants at baseline and 6-month follow-up. The blood draw and rapid HIV and syphilis testing took place at our project offices in Tijuana and Cd. Juarez. For rapid HIV testing, we used the Advanced Quality™ Rapid Anti-HIV (1&2) Test by InTec Products, Inc., which has high sensitivity and specificity (InTec Products, 2002). For rapid syphilis testing, we used the One Step Syphilis rapid test by InTec Products, Inc. In addition, urine was collected using the Aptima® Combo 2 collection device (Genprobe) for culturing gonorrhea and chlamydia. All blood samples that yielded a positive result on the rapid HIV or syphilis tests (or both) were shipped, along with the urine samples, to the San Diego County Public Health Laboratory (SDCPHL). To confirm HIV, the SDCPHL performed EIA and IFA or Multispot. Confirmatory syphilis testing involved an RPR Panel that included qualitative, quantitative, and TPPA. HIV/STI test results were provided to participants by nurses within one week of testing. Those testing HIV-positive were referred to the municipal clinic in their city for free medical care, and those who tested positive for another STI on a rapid test were treated presumptively in our project offices.
Statistical Analysis
We examined differences between intervention groups (SHORT-TERM vs. FUTURE) using chi-square tests for binary outcomes, and Mann-Whitney tests for continuous outcomes. These tests were also used to compare the two interview locations, Tijuana and Cd. Juarez, to determine whether stratification by location was necessary for the outcome analyses. The outcome for these analyses (HIV/STI incidence rate) was calculated by taking the ratio between the combined number of incident cases and the number of person-years at risk accumulated over the 6-month study period for participants who had a 6-month follow-up visit. Incident cases were assumed to have occurred at the mid-point between the baseline and the 6-month follow-up interval. For the participants who did not contract any incident STIs during the follow-up, the “time at risk” was represented by the time from baseline to the time of the 6-month follow-up. The number of person years at risk was calculated by summing the “time at risk” for each participant. Finally, the incidence density per 100 person years was calculated by taking the ratio between the number of incident cases and number of person years at risk and multiplying it by 100. To evaluate the impact of the intervention (SHORT-TERM vs. FUTURE) on HIV/STI incidence, we conducted Poisson regression with robust variance estimation via Generalized Estimating Equations (GEE), using the logarithm of the time (years) spent at risk as an offset variable to account for the varying length of time at risk per subject.
We first examined the main effects of intervention group (SHORT-TERM vs. FUTURE), study location (Tijuana vs. Cd. Juarez), and the interaction between the two, respectively. Because the interaction between the intervention group and study location was significant, we subsequently performed analyses stratified by study location, where the main effect investigated was the effect of the intervention group (SHORT-TERM vs. FUTURE) on the HIV/STI incidence outcome. GEE with robust variance estimation was chosen as the analytical method for evaluating the primary outcome to correct for moderate over-dispersion. After stratification, we examined intervention group effect on the HIV/STI incidence. Variables that differed by group at baseline and variables that yielded a p≤ 0.10 in univariate analyses were considered as potential covariates. In the final multivariate models for Tijuana and Cd. Juarez, interactions among all the variables included in a model were evaluated to ensure the model integrity (p≤0.10). Multi-collinearity was assessed for each model and ruled out by the appropriate values of the Variance Inflation Factors and the Condition Indexes.
Randomization Procedures
Of 439 women who were screened for eligibility, 302 (68.8%) met the eligibility criteria, provided informed consent, and were enrolled in the study (153 in Tijuana and 149 in Cd. Juarez). All enrollees underwent interviewer-administered surveys and provided biological samples, and after the completion of the survey, each woman was classified, based on her drug-use behavior in the past 30 days, into one of the three groups: IDUs (n=102), non-IDU drug users (n=93), or non-drug users (n=107). Then, participants from each of the three drug-use groups were randomized to one of the two active intervention groups: FUTURE (n=149) and SHORT-TERM (N=153).
A block randomization (in blocks of 10—e.g., of every 10 IDUs, 5 were assigned to the SHORT-TERM group and 5 to the FUTURE group) was used to ensure balanced randomization by drug use status. Seventeen participants who reported light drug use (marijuana, hashish, ecstasy) only in the past month were excluded from these analyses. Furthermore, given that our outcome was incident HIV/STIs, the analysis was restricted to only those who completed the 6-month follow-up visit (n=270, distributed 52% in Tijuana and 48% in Cd. Juarez), of which 49.3% received the FUTURE and 50.7% received the SHORT-TERM intervention (Figure 1). Among the full sample of 302 FSWs, there were no participant withdrawals between baseline assessment and 6-month follow-up.
Figure 1.
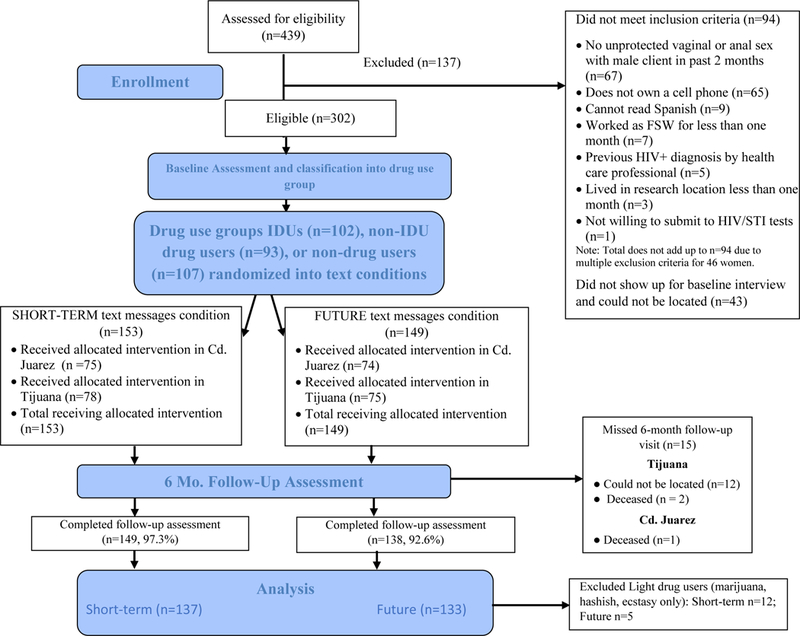
CONSORT diagram summarizing participant flow through the study.
A comparison between those lost to follow-up (n=15) and those who were not (n=270) indicated that a higher percentage of those lost to follow-up were from the FUTURE group (80% vs. 47.8%, p=0.02), as opposed to the SHORT-TERM group. Those lost to follow-up were also less likely to have a spouse/steady partner (6.7% vs. 30.4%, p=0.05) and to have children (80% vs. 96.7%, p=0.002), had a smaller number of clients (median: 20 vs. 60 per month, p=0.01), a smaller number of vaginal and anal sex acts with clients (25 vs. 64 acts per month, p=0.009), and a smaller number of unprotected vaginal and anal sex acts with clients (5 vs. 21.5, p=0.01). Furthermore, those lost to follow-up were less likely to have ever had an HIV test (40% vs. 70%, p=0.01) and more likely to test positive for gonorrhea at baseline (33.3% vs. 7%, p<0.001).
Results
Among the 302 participants who received MSS counseling and maintenance text messages, 32 were excluded from this analysis either because they were identified as light drug users (n=17) or were missing 6 month follow-up data (n=15). Among the 270 participants who were included in this analysis, the average age was 37.5 (SD=10.2, median=37.0, range 18–70), and 84.6% reported an educational level of secondary school or less. Sixty-one percent reported their marital status as single. The majority lived alone (49.5%), and 13.3% lived with another adult who was not a sexual partner. Twenty-four percent lived with a spouse or steady partner. Ninety-six percent had at least one child, of whom 70% were under the age of 18 years. Forty-four percent lived with at least one child under the age of 18 years. The average number of children was 3.2 (SD = 1.7, range 1–10). The average number of financial dependents was 2.1 (SD = 1.6, range 0–7). Sixty-eight percent described themselves as a street-based sex worker, 27% identified as a barmaid or dance hostess, while only 1.1% identified as a brothel worker. Only two FSWs tested HIV-positive at six-month follow-up, both of whom resided in Tijuana. The 17 FSWs (light drug users) who were excluded from the analyses did not differ from the overall sample on any of these characteristics.
Univariate Analyses
Compared to Tijuana participants, FSWs in Cd. Juarez had less education (53.5% vs. 38.3% ≤ grade school education, p=0.01), were more likely to live with children under 18 years of age (55.8% vs. 30.5%, p<0.001), were more likely to earn over 3500 pesos monthly (93.8% vs. 57.4%, p<0.001), and had significantly more texting experience (median: 7.5 vs. 2.1 years, p<0.001). Also, a higher proportion of Cd. Juarez participants used non-injection heavy drugs (71.3% vs. 53.9%, p=0.003), and were more likely to have injected drugs (45.7% vs. 26.2%, p<0.001), and used alcohol before/during sex with a male client in the past month (58.9% vs. 36.2%, p<0.001). FSWs in Cd. Juarez also had more male clients (median: 80 vs. 40 per month, p<0.001), with a higher percentage of clients being Mexican clients (99.2% vs. 71.6% most or all Mexican clients, p<0.001), had more condom-unprotected vaginal/anal sex (median: 40 vs. 10 sex acts per month, p<0.001), but earned less per unprotected vaginal sex act (median: 11.2 vs. 16.8 USD per act, p<.001) compared to their counterparts in Tijuana (Table 1).
Table 1.
Descriptive Statistics of Participants by Intervention Group, at Baseline, by Study Site (n=270)
| Tijuana | Cd. Juarez | Tijuana vs. Cd. Juarez |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Future (n=69) | Short Term (n=72) | Total (n=141) |
Future (n=64) |
Short Term (n=65) |
Total (n=129) |
Test statistic and p-value |
| Age (Median (IQR) | 36.0(28.0,45.0) | 40.0(32.0,45.5) | 38.0(30.0,45.0) | 37.0(28.0,45.0) | 36.0(28.0,45.0) | 37.0(28.0,45.0) | −.80Z (.43) |
| # of years since first started sex work (Median (IQR) | 6.0(3.8,10.5) | 7.0(4.0,15.5) | 6.4(4.0,12.5) | 7.5(4.0,15.0) | 7.0(3.0,12.0) | 7.0(3.5,15.0) | .44Z (.66) |
| Has grade school education or less | 24(34.8%) | 30(41.7%) | 54(38.3%) | 36(56.3%) | 33(50.8%) | 69(53.5%) | 6.27C (.01) |
| Has a spouse or steady partner | 22(31.9%) | 26(36.1%) | 48(34.0%) | 18(28.1%) | 16(24.6%) | 34(26.4%) | 1.88 C (.17) |
| Lives with children under 18 | 24(34.8%) | 19(26.4%) | 43(30.5%) | 35(54.7%) | 37(56.9%) | 72(55.8%) | 17.66 C (<.001) |
| Lives with opposite sex spouse/steady sexual partner | 15(21.7%) | 16(22.2%) | 31(22.0%) | 9(14.1%) | 9(13.8%) | 18(14.0%) | 2.93 C (.09) |
| Earns on average > 3500 pesos monthly | 40(58.0%) | 41(56.9%) | 81(57.4%) | 59(92.2%) | 62(95.4%) | 121(93.8%) | 47.25 C (<.001) |
| Main source of income: sex workb | 68(98.6%) | 72(100%) | 140(99.3%) | 64(100%) | 62(95.4%) | 126(97.7%) | 1.21 C (.27) |
| Texting experience (years; (Median (IQR)) | 2.2(0.3,10.0) | 2.0(0.3,5.3) | 2.1(0.3,8.0) | 7.0(4.3,10.0) | 8.0(5.0,10.0) | 7.5(5.0,10.0) | 6.35 Z (<.001) |
| Used non-injection heavy drugsa | 38(55.1%) | 38(52.8%) | 76(53.9%) | 46(71.9%) | 46(70.8%) | 92(71.3%) | 8.69 C (.003) |
| Injected any drugsa | 16(23.2%) | 21(29.2%) | 37(26.2%) | 29(45.3%) | 30(46.2%) | 59(45.7%) | 11.17 C (<.001) |
| Binge used drugsa | 8(21.1%) | 11(28.2%) | 19(24.7%) | 2(4.3%) | 1(2.2%) | 3(3.3%) | <.001F |
| Receptive needle sharing (among IDUs)b | 11(61.1%) | 15(68.2%) | 26(65.0%) | 15(48.4%) | 17(56.7%) | 32(52.5%) | 1.55 C (.21) |
| Used drugs before/during sex with male clientb | 34(49.3%) | 29(40.3%) | 63(44.7%) | 31(48.4%) | 35(53.8%) | 66(51.2%) | 1.13 C (.29) |
| Harmful hazardous drinking, past year | 33(47.8%) | 28(38.9%) | 61(43.3%) | 28(43.8%) | 22(33.8%) | 50(38.8%) | 0.56 C (.45) |
| Used alcohol during sex with male clienta | 24(34.8%) | 27(37.5%) | 51(36.2%) | 40(62.5%) | 36(55.4%) | 76(58.9%) | 13.99 C (<.001) |
| Arrested (ever) for working as a FSW | 24(34.8%) | 17(23.6%) | 41(29.1%) | 21(32.8%) | 24(36.9%) | 45(34.9%) | 1.05 C (.31) |
| Worked as a FSW on the streetb | 49(71.0%) | 56(77.8%) | 105(74.5%) | 9(14.1%) | 4(6.2%) | 13(10.1%) | <.001 F |
| Has most or all Mexican clients | 52(75.4%) | 49(68.1%) | 101(71.6%) | 63(98.4%) | 65(100%) | 128(99.2%) | 39.83 C (<.001) |
| # of male clients per month (Median (IQR) | 37.5(13.3,61.0) | 40.0(9.6,60.6) | 40.0(10.0,60.7) | 72.0(44.0,93.8) | 80.0(48.0, 135) | 80.0(48.0, 112) | 7.28 Z (<.001) |
| # of times had vaginal and anal sex with clientsa (Median (IQR) | 40.0(24.0,80.0) | 43.0(21.0,86.0) | 41.0(24.0,85.0) | 76.0(55.0,97.5) | 85.0(62.0, 117) | 80.0(57.0, 105) | 6.16Z (<.001) |
| # of times you had unprotected vaginal and anal sex with clientsa (Median (IQR) | 10.0(3.0,21.0) | 9.5(4.0,27.5) | 10.0(4.0,24.0) | 40.0(20.0,63.0) | 41.0(16.0,75.0) | 40.0(16.0,66.0) | 7.53Z (<.001) |
| Amount earned per vaginal sex act without a condom (USD) (Median (IQR) | 18.2(11.2,30.0) | 16.8(11.2,39.2) | 16.8(11.2,33.6) | 11.2(8.4,16.8) | 12.6(8.4,18.2) | 11.2(8.4,16.8) | −5.49Z (<.001) |
| Amount earned per anal sex act without a condom (USD) (Median (IQR) | 33.6(14.0,56.0) | 15.9(9.8,33.6) | 16.8(11.2,44.8) | 15.4(8.4,19.6) | 14.0(8.4,22.4) | 14.0(8.4,19.6) | 1.64Z (.10) |
| Forced sex by clientsb | 5(7.2%) | 9(12.5%) | 14(9.9%) | 1(1.6%) | 3(4.6%) | 4(3.1%) | .02 F |
| Currently under the care of a psychologist or psychiatrist | 1(1.4%) | 3(4.2%) | 4(2.8%) | 1(1.6%) | 3(4.6%) | 4(3.1%) | .90 F |
| Score on Beck depression scale (Median (IQR) | 15.0( 8.0,22.0) | 19.5(13.0,25.0) | 17.0( 9.0,24.0) | 11.0( 4.0,19.5) | 14.0(5.0,18.0) | 13.0(5.0,19.0) | −4.03Z ( <.001) |
| Meets criteria for moderate or severe depression* | 23(33.3%) | 36(50.0%) | 59(41.8%) | 16(25.0%) | 14(21.5%) | 30(23.3%) | 10.53 C (.001) |
| Score for feelings of stigmatized identity scale (Median (IQR) | 1.6(0.8, 2.0) | 1.6(1.0, 2.2) | 1.6(0.8, 2.0) | 1.2(0.4, 1.8) | 1.2(0.8, 2.0) | 1.2(0.6, 2.0) | −2.31 Z (.021) |
| Ever has been tested for HIV | 48(69.6%) | 47(65.3%) | 95(67.4%) | 43(67.2%) | 51(78.5%) | 94(72.9%) | 0.97 C (.33) |
| Currently has any vaginal symptoms | 28(40.6%) | 29(40.3%) | 57(40.4%) | 19(29.7%) | 13(20.0%) | 32(24.8%) | 7.44 C (.006) |
| Tested positive for gonorrhea at baseline | 13(18.8%) | 9(12.5%) | 22(15.6%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 21.91 C (<.001) |
| Tested positive for chlamydia at baseline | 13(18.8%) | 19(26.4%) | 32(22.7%) | 7(10.9%) | 3(4.6%) | 10(7.8%) | <.001 F |
| Tested positive for lifetime syphilis at baseline | 14(20.3%) | 12(16.7%) | 26(18.4%) | 14(21.9%) | 18(27.7%) | 32(24.8%) | 1.62 C (.20) |
| Syphilis titers >=1:8, among lifetime syphilis cases | 3(21.4%) | 1(8.3%) | 4(15.4%) | 0(0.0%) | 2(11.1%) | 2(6.3%) | .39 F |
| Tested positive for any STI at baseline | 27(39.1%) | 30(41.7%) | 57(40.4%) | 19(29.7%) | 20(30.8%) | 39(30.2%) | 3.05 C (.08) |
past month
past 6 months
Future vs short p<0.05 (Tijuana Site only)
Chi-Square test statistic
Z statistic for the normal approximation to the Mann-Whitney U test
p-value corresponding to Fisher’s
Compared to FSWs in Cd. Juarez, FSWs in Tijuana were significantly more likely to have worked as a street-based sex worker in the previous 6 months (74.5% vs. 10.1%, p<0.001), and to report binge drug use (24.7% vs. 3.3%, p<0.001), and to have experienced forced sex by a client in this time period (9.9% vs. 3.1%, p=0.02). Also, Tijuana participants scored significantly higher on the Beck depression scale (median: 17 vs. 13, 0<0.001), and the feelings of stigmatized identity scale (median: 1.6 vs. 1.2, p=0.02). Tijuana participants were also marginally more likely to test positive for a STI (40.4% vs. 30.2%, p=0.08), with significantly higher prevalence of gonorrhea (15.6% vs. 0%, p<0.001) and chlamydia (22.7% vs. 7.8%, p<0.001).
A comparison of baseline characteristics by intervention condition, stratified by study location (Table 1), suggested that randomization achieved relatively balanced groups, with one notable exception. In Tijuana, participants receiving the short-term intervention had significantly higher scores on the Beck depression Inventory (median score: 17 v. 13, p<.001), with a larger percentage meeting criteria for moderate to severe depression (50% vs. 33.3%, p<0.05).
Since the two study locations were found to differ with respect to a number of characteristics, a Poisson model was used to evaluate the interaction between the intervention and study location. The interaction was found to be statistically significant (p=0.05) (Table 4), indicating that the intervention effect differed by study location (Figure 2). This model controlled for having used injected drugs or non-injected heavy drugs during the previous 30 days, because the short-term group in Cd. Juarez had a significantly higher proportion of such drug users (71% vs. 55%, p=0.05) as compared to the corresponding group in Tijuana. Given that the two study locations were quite different and that the interaction between location and intervention was significant, a stratified analyses by study location was deemed necessary.
Table 4.
Interaction between study site and intervention group
| Predictor | Adjusted Relative Risk |
95% CI | p-value |
|---|---|---|---|
| Study Site (Tijuana vs. Ciudad Juarez) | 1.02 | 0.41, 2.53 | 0.01 |
| Intervention Group (Short Term vs. Future) | 0.56 | 0.21, 1.53 | 0.26 |
| Injected or used heavy drugs (past month) | 2.47 | 1.23, 4.97 | 0.01 |
| Interaction between Study Site & Intervention | 3.51 | 0.99, 12.53 | 0.05 |
Figure 2.
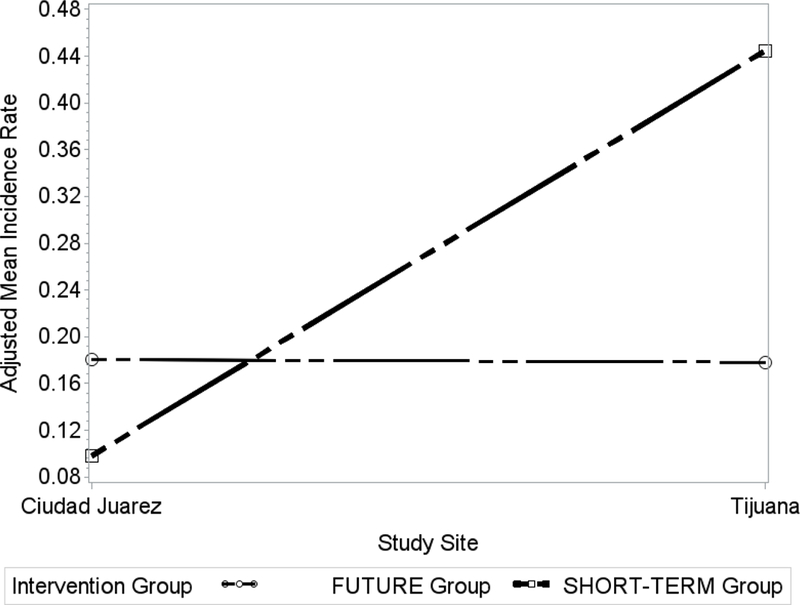
Interaction between study site and intervention group
Multivariate Analyses
Regarding the main outcome, in Tijuana, the HIV/STI incidence density was lower among FSWs randomized to the future-oriented group (31.67 per 100 py, respectively) compared to women in the short-term group (62.40 per 100 py) (Table 2). The final Poisson regression model for Tijuana (Table 3) found that the adjusted HIV/STI incidence rate for FSWs assigned to the future-oriented group was significantly lower than women assigned to short-term group [i.e., Adjusted relative incidence rate (ARIR): 0.46 (95% CIs: 0.22, 0.97]. This model controlled for currently being under the care of a psychiatrist and having used drugs with a client in the previous 6 months. Conversely, in Cd. Juarez, HIV/STI incidence density was lower among the women in the short-term group (19.80 per 100 py) compared to those in the future-oriented group (35.05 per 100 py, respectively) (Table 2). However, this difference was not found to be statistically significant (Table 3).
Table 2.
HIV/STI incidence rate over 6 months: Overall, by intervention group and site.
| Group | # of incident cases |
# of persons at risk |
# of py at risk |
Incidence density per 100 py (95% CI) |
|---|---|---|---|---|
| Entire Sample | 45 | 270 | 119.31 | 37.72(26.70,48.74) |
| Future | 19 | 129 | 56.95 | 33.36(18.36,48.36) |
| Short Term | 26 | 141 | 62.36 | 41.70(25.67,57.72) |
| Tijuana | 29 | 135 | 60.47 | 47.96(30.50,65.41) |
| Future | 9 | 62 | 28.42 | 31.67(10.98,52.36) |
| Short Term | 20 | 73 | 32.05 | 62.40(35.05,89.75) |
| Cd. Juarez | 16 | 135 | 58.84 | 27.19(13.87,40.52) |
| Future | 10 | 67 | 28.53 | 35.05(13.33,56.77) |
| Short Term | 6 | 68 | 30.31 | 19.80( 3.96,35.64) |
Table 3.
Intervention effects on HIV/STI incidence after 6 months: Tijuana and Cd. Juarez
| Tijuana Model | |||
| Predictor | Adjusted Relative Risk | 95% CI | p-value |
| Intervention Group (Short Term vs. Future) | 0.46 | 0.22, 0.97 | 0.04 |
| Used drugs with clients during sex (past 6-months) | 4.12 | 1.79, 9.49 | <0.001 |
| Currently under care of a psychologist or psychiatrist | 5.26 | 1.48, 18.69 | 0.01 |
| Cd. Juarez Model | |||
| Predictor | Adjusted Relative Risk | 95% CI | p-value |
| Intervention Group (Short Term vs. Future) | 2.33 | 0.23, 23.47 | 0.47 |
| Emotional support from family and friends | 0.08 | 0.03, 0.26 | <0.0001 |
| The amount of money (US dollars) earns each time performs anal sex using a condom | 0.93 | 0.90, 0.96 | <0.0001 |
Discussion
This study found partial support for the hypothesis that time perspective variations (short-term vs. future-oriented) in text messages delivered in a safer sex behavioral maintenance intervention have a significant influence on HIV/STI incidence among FSWs in Mexico. Specifically, FSWs in Tijuana, where there was a lower percentage of heavy drug users/IDU, benefited from future-oriented time perspective text messages that focused on the advantages of long-term safer sex maintenance practices in order to achieve future-oriented goals. In contrast, FSWs in Cd. Juarez, where there was a higher percentage of heavy drug users/IDUs, did not benefit from either the short-term nor future-oriented time perspective text messages. Overall, our findings contribute to a growing literature that shows the value of time perspective variations in HIV prevention intervention messages, particularly in high-risk populations, such as FSWs who use drugs. These findings suggest the positive impact of text messages with varying time perspectives on STI incidence is diminished by participants’ use of heavy drugs/IDU and by psychological symptoms (e.g., depression) necessitating psychological care. These findings also highlight differences in FSWs’ characteristics, which may differ by study location and point to the importance of considering local variations in participants’ responses to text-based intervention messages with varying time perspectives.
An important finding in this study was the reverse relationship observed between time perspective and STI incidence in the two study locations. Specifically, future-oriented text messages were associated with reduced STI incidence density in Tijuana, whereas short-term time perspective messages were associated with this outcome in Cd. Juarez. This may be explained by differences between FSWs in the two sites, particularly differences in their reported drug use. We contend that the relationship between short-term time perspective text messages and lower STI incidence density in Cd. Juarez (although not statistically significant) may be related to the higher proportion of drug-using FSWs in that city compared to Tijuana.
Persons who misuse substances are more likely to have a shortened time perspective (Teuscher & Mitchell, 2011), which would presumably make them more responsive to short-term behavioral maintenance text messages. Studies of the lived experiences of individuals who meet criteria for drug dependence or addiction, including those who inject drugs, report multiple factors that may shorten their time perspective and interfere with planning for the future, including fear of overdose (non-fatal) and death from overdose, worries about declining physical and mental health, housing instability, fear of arrest and incarceration, and reliving of traumatic experiences (Bazazi et al., 2015; Dunne et al., 2015; Hsieh et al., 2017; Moskalewicz, 2016; Obong’o et al., 2017; Richert, 2015).
It has been reported that people who have substance use disorders are more impulsive (Hayaki et al., 2006; Moeller et al., 2001), and have difficulties turning down immediate rewards and planning for the future (Koffarnus et al., 2016). Impulsivity has also been identified as a characteristic of individuals who have a shortened time perspective (Petry et al., 1998; Teuscher & Mitchell, 2011), which may be related to deficits in executive functioning performance, specifically planning ability (Martoni et al., 2017). Impulsivity was not measured in the parent study; hence, we were unable to take this factor into account in our time perspective analyses. Future studies of time perspective and risk behavior among FSWs, particularly drug users, should address the role of impulsivity in determining sexual risk behavior and STI outcomes. Also, it is possible that a combination of FSW characteristics (i.e., drug use, impulsivity, and shortened time perspective) was more common among FSWs in Cd. Juarez, thus making them more responsive to the short-term time perspective text messages. This would help to account for the observation that the relationship between time perspective and the STI incidence density in Cd. Juarez was in the opposite direction of the one observed in Tijuana where future-oriented text messages were associated with lower STI incidence.
Also, FSWs in Cd. Juarez had lower levels of education and were more likely to be parenting children under the age of 18 years, both of which could have bolstered their response to short-term text messages that focused on immediate rewards for sustaining positive behavior change. Low education is common among FSWs in LMIC (Andrews et al., 2015; Tamene et al., 2015; Trout et al., 2015) and may be associated with deficits in ability to plan for and achieve future-oriented goals (Köstering et al., 2015; Martoni et al., 2017). It is plausible that text messages with a short-term time perspective may be more relevant and appealing to FSWs with low levels of education, as evidenced among participants in the Cd. Juarez sample. In addition, maternal role strain is common among FSWs (Rolon et al., 2013; Servin et al., 2017), and entails a variety of stressors related to childrearing (e.g., financial, child behavioral problems, physical and emotional health of children, interpersonal strain) (Semple et al., 2011). It is not unreasonable to suggest that in Cd. Juarez where there was a larger percentage of FSWs with dependent-age children, the immediate problems and needs associated with childrearing may have elevated the value of safer sex text messages with a short-term time perspective as compared to future-oriented text messages.
The present findings provide some evidence as to the efficacy of a future-oriented, technology-enabled text messaging behavioral maintenance intervention designed to sustain post-counseling improvements in sexual risk behavior among FSWs in a LMIC. These findings raise the issue of whether cognitive-motivational or psychological interventions can be successfully developed to extend the future time perspectives of FSWs, thus enabling them to achieve long-term, future goals related to their sexual health and well-being (Teuscher & Mitchell, 2011). To date, a few studies have examined the feasibility of lengthening time perspective by improving negative views of the future, promoting long-term goals as achievable, and motivating health protective behaviors among drug users, disadvantaged youth, and bipolar patients (Cheong et al., 2014; Tse et al., 2014). One intervention conducted with disadvantaged youth used the theory of ‘possible selves’ (Markus & Nurius, 1986) to motivate adolescents and young adults to think of themselves in the future as successful adults (described as positive future selves that embrace motivating ideas about who and what they might become) by avoiding risk behaviors, such as sexual risk and drug use (Clark et al., 2005). The ‘possible selves’ theoretical framework might be a valuable approach to enhancing future time perspective among FSWs in LMIC.
It is also likely that interventions to increase future time perspective in this high-risk population will need to take into account the psychological health and well-being of FSWs. Past research on FSWs, including the present sample, has found high rates of depression and other psychological issues (e.g., suicidal thoughts, unresolved trauma issues) that are associated with increased HIV risk behavior (e.g., inconsistent condom use) and reduced effectiveness of drug treatment (Jeal et al., 2017; Yuen et al., 2016). Thus, interventions that address time perspective (promoting behavior that is organized around future or long-term goals), while targeting both cognitive and psychological factors, may be key to the maintenance of safer sex practices among FSWs in Mexico and other LMIC.
Lastly, our findings support the idea that integration of technological approaches, such as text messaging, can enhance or help to sustain behavioral changes gained through more traditional social science approaches, including the face-to-face social learning theory-based Mujer Segura intervention that FSWs were exposed to in the initial behavior change component of the present study.
Study Limitations
The findings from this study may lack generalizability because FSWs in Tijuana and Cd. Juarez were recruited as convenience samples that may not generalize to other populations of FSWs. Although we attempted to sample as representatively as possible in both locations, it is possible that sampling error rather than true distribution of drug use (which was heavier among FSWs in Cd. Juarez) contributed to differences between study sites. We also found that a higher percentage of participants were lost to follow-up in the future-oriented text messaging group and that these participants differed from those who were not lost to follow-up on several socio-demographic variables and sexual risk behaviors. These differences point to heterogeneity among FSWs that should be considered in the development of behavioral maintenance interventions. In terms of design, our study could have included a no text message control group, which might have resulted in stronger findings. However, we opted for sending safer sex maintenance texts to all of our high-risk FSWs given the importance and potential benefits of promoting maintenance behaviors. Also, a potential source of contamination in this study is cross-talk between FSWs in the two intervention conditions. While our previous work with FSWs in Mujer Segura (Patterson et al., 2008a) did not identify cross talk between FSWs to be problematic, we cannot rule out this potential problem in the present study. Further, this study did not include an objective measure of time perspective, such as the Zimbardo Time Perspective Inventory (Zimbardo & Boyd, 1999), which would have allowed us to quantify and examine this construct directly in relation to protective and risky health behaviors among FSWs in our sample. Also, several published measures of time perspective (Webster, 2011; Zimbardo & Boyd, 1999) specify dimensions or components of this construct that would have permitted a more refined analysis of how these dimensions may relate differentially to STI incidence and other sexual risk outcomes. Both drug use and drug abstinence were assessed through self-reports, which are subject to study bias. Accordingly, we cannot rule out the possibility that some participants were misclassified on the drug use status variable. Also, FSWs who used non-injection heavy drugs and those who injected drugs were combined into a single category because of our limited sample size. It is possible that the findings might be different for these two groups or that differences based on different types of substances (e.g., heroin, methamphetamine) could have emerged. These drug use classification issues should be addressed in future studies, along with additional health outcomes, including sexual risk behaviors and injection drug use practices. Also, the small number of FSWs (n=2) who seroconverted over the six-month study period did not allow us to assess HIV incidence separately from other STIs. Finally, this study did not determine causality in the relationship between time perspective and STI incidence. To this end, future studies should gather prospective data on a larger sample of FSWs over a period of more than 6 months.
Conclusions
This study documented the successful development and delivery of a technology-enabled intervention that used text messages with variations in time perspective to empower high-risk women to achieve maintenance of safer sex practices in a LMIC. The significant relationship between future time perspective text messages and lower HIV/STI incidence density among FSWs in Tijuana provides preliminary evidence that HIV prevention messages that link safer sex maintenance with a positive future are important to preventing condom lapses among FSWs who have undergone sexual risk reduction counseling. Text messaging technology is widely available in developing countries, and therefore, our findings have direct, tangible policy implications for Mexico and other LMIC. This behavioral maintenance intervention that delivered text messages with a time perspective component has the potential to curtail the burgeoning HIV epidemic in the U.S.-Mexico border region and to have applicability elsewhere in Mexico and other LMIC, since the global sex industry is increasing (Ward & Aral, 2006).
Acknowledgements
The authors gratefully acknowledge study staff, participants, Brian Kelly for research assistance, and the Municipal and State Health Departments of Tijuana, Baja California, Mexico and Ciudad Juarez, Chihuahua, Salud y Desarollo Comunitario de Ciudad Juarez A.C. (SADEC) and Federación Méxicana de Asociaciones Privadas A.C. (FEMAP), and Universidad Xochicalco de Tijuana.
Funding
This work was supported by the National Institutes of Health, grants P30 AI036214 (UCSD CFAR Developmental Grant to SV), NIH R01 DA039071 (TLP), R37 DA019829 (SAS), and R01 DA039071–03S1 (AVH).
Footnotes
Compliance with ethical standards
Human and animal rights and Informed consent
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional committees at the University of California, San Diego and Xochicalco University in Tijuana, Mexico and with the 1964 Helsinki declaration and its later amendments. Written informed consent was obtained from all individual participants included in this study.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Abousselam N, Naudé L, Lens W & Esterhuyse K (2016). The relationship between future time perspective, self-efficacy and risky sexual behaviour in the black youth of central South Africa. Journal of Mental Health, 25(2), 176–183. [DOI] [PubMed] [Google Scholar]
- Ajzen I & Fishbein M (1980). Understanding attitudes and predicting social behaviour. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Albein-Urios N, Martinez-Gonzalez JM, Lozano O & Verdejo-Garcia A (2014). Monetary delay discounting in gambling and cocaine dependence with personality comorbidities. Addictive Behaviors, 39(11), 1658–1662. doi: 10.1016/j.addbeh.2014.06.001 [DOI] [PubMed] [Google Scholar]
- Amlung M, Vedelago L, Acker J, Balodis I & MacKillop J (2017). Steep delay discounting and addictive behavior: A meta-analysis of continuous associations. Addiction, 112(1), 51–62. doi: 10.1111/add.13535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews CH, Faxelid E, Sychaerun V & Phrasisombath K (2015). Determinants of consistent condom use among female sex workers in Savannakhet, Lao PDR. BMC Women’s Health, 15, 63. doi: 10.1186/s12905-015-0215-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anokhin AP, Grant JD, Mulligan RC & Heath AC (2015). The genetics of impulsivity: Evidence for the heritability of delay discounting. Biological Psychiatry, 77(10), 887–894. doi: 10.1016/j.biopsych.2014.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey AE & Figueroa JP (2017). Agency, lapse in condom use and relationship intimacy among female sex workers in Jamaica. Culture, Health & Sexuality, 1–14. doi: 10.1080/13691058.2017.1360944 [DOI] [PubMed] [Google Scholar]
- Bandura A (1986). Social foundation of thought and action: A social-cognitive theory. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Bandura A (1989). Perceived self-efficacy In Mays & Schneider (Eds.), Primary prevention of AIDS: Psychological approaches (pp. 128–141). Newbury Park, CA: SAGE Publications. [Google Scholar]
- Basnyat I (2014). Lived experiences of street-based female sex workers in Kathmandu: Implications for health intervention strategies. Culture, Health & Sexuality, 16(9), 1040–1051. doi: 10.1080/13691058.2014.922620 [DOI] [PubMed] [Google Scholar]
- Bazazi AR, Zelenev A, Fu JJ, Yee I, Kamarulzaman A & Altice FL (2015). High prevalence of non-fatal overdose among people who inject drugs in Malaysia: Correlates of overdose and implications for overdose prevention from a cross-sectional study. International Journal on Drug Policy, 26(7), 675–681. doi: 10.1016/j.drugpo.2014.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT (1967). Depression: Causes and treatment. Philadelphia: University of Pennsylvania. [Google Scholar]
- Beck AT (1976). Cognitive therapy and the emotional disorders: New York, NY: Hoeber. [Google Scholar]
- Beck AT, Steer RA & Brown GK (1996). Manual for the Beck depression inventory-ii (BDI-II). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck JS (2007). The Beck diet solution: Birmingham, Alabama: Oxmoor House, Inc. [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM & Barbash RB (2003). Patterns of health behavior in U.S. Adults. Preventive Medicine, 36(5), 615–623. [DOI] [PubMed] [Google Scholar]
- Brouwer KC, Strathdee SA, Magis-Rodriguez C, Bravo-Garcia E, Gayet C, Patterson TL, Bertozzi SM & Hogg RS (2006). Estimated numbers of men and women infected with HIV/AIDS in Tijuana, Mexico. Journal of Urban Health, 83(2), 299–307. doi: 10.1007/s11524-005-9027-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull S & Ezeanochie N (2016). From Foucault to Freire through Facebook: Toward an integrated theory of mHeatlh. Health Educ Behav, 43(4), 399–411. [DOI] [PubMed] [Google Scholar]
- Camchong J, MacDonald AW 3rd, Nelson B, Bell C, Mueller BA, Specker S & Lim KO (2011). Frontal hyperconnectivity related to discounting and reversal learning in cocaine subjects. Biological Psychiatry, 69(11), 1117–1123. doi: 10.1016/j.biopsych.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (n.d.). October 11, 2017 Retrieved from https://www.cdc.gov
- Cheong J, Tucker JA, Simpson CA & Chandler SD (2014). Time horizons and substance use among African American youths living in disadvantaged urban areas. Addictive Behaviors, 39(4), 818–823. doi: 10.1016/j.addbeh.2013.12.016 [DOI] [PubMed] [Google Scholar]
- Clark LF, Miller KS, Nagy SS, Avery J, Roth DL, Liddon N & Mukherjee S (2005). Adult identity mentoring: Reducing sexual risk for African-American seventh grade students. Journal of Adolescent Health, 37(4), 337. doi: 10.1016/j.jadohealth.2004.09.024 [DOI] [PubMed] [Google Scholar]
- Conigrave KM, Hall WD & Saunders JB (1995). The audit questionnaire: Choosing a cut‐off score. Addiction, 90(10), 1349–1356. [DOI] [PubMed] [Google Scholar]
- Dany L, Roussel P, Laguette V, Lagouanelle-Simeoni MC & Apostolidis T (2016). Time perspective, socioeconomic status, and psychological distress in chronic pain patients. Psychology, Health & Medicine, 21(3), 295–308. doi: 10.1080/13548506.2015.1062900 [DOI] [PubMed] [Google Scholar]
- Davis KC, Stoner SA, Norris J, George WH & Masters NT (2009). Women’s awareness of and discomfort with sexual assault cues: Effects of alcohol consumption and relationship type. Violence Against Women, 15(9), 1106–1125. doi: 10.1177/1077801209340759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine S, Leeds C, Shlay JC, Leytem A, Beum R & Bull S (2015). Methods to assess youth engagement in a text messaging supplement to an effective teen pregnancy program. J Biomed Inform, 56, 379–386. [DOI] [PubMed] [Google Scholar]
- Dierst-Davies R, Reback CJ, Peck JA, Nuno M, Kamien JB & Amass L (2011). Delay-discounting among homeless, out-of-treatment, substance-dependent men who have sex with men. American Journal of Drug and Alcohol Abuse, 37(2), 93–97. doi: 10.3109/00952990.2010.540278 [DOI] [PubMed] [Google Scholar]
- Duncan J, Gebre Y, Grant Y, Wedderburn M, Byfield L, Bourne D, Brown M & Figueroa JP (2010). HIV prevalence and related behaviors among sex workers in Jamaica. Sexually Transmitted Diseases, 37(5), 306–310. doi: 10.1097/OLQ.0b013e3181c6e851 [DOI] [PubMed] [Google Scholar]
- Dunne EM, Burrell LE 2nd, Diggins AD, Whitehead NE & Latimer WW (2015). Increased risk for substance use and health-related problems among homeless veterans. American Journal on Addictions, 24(7), 676–680. doi: 10.1111/ajad.12289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldemire-Shearer D & Bailey A (2008). Determinants of risk behaviour of sex-workers in Jamaica. A qualitative approach. West Indian Medical Journal, 57(5), 450–455. [PubMed] [Google Scholar]
- Feldman MB, Silapaswan A, Schaefer N & Schermele D (2014). Is there life after DEBI? Examining health behavior maintenance in the diffusion of effective behavioral interventions initiative. American Journal of Community Psychology, 53(3–4), 286–313. doi: 10.1007/s10464-014-9629-3 [DOI] [PubMed] [Google Scholar]
- Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C, Stein RI, Mohammed BS, Miller B, Rader DJ, Zemel B, Wadden TA, Tenhave T, Newcomb CW & Klein S (2010). Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: A randomized trial. Annals of Internal Medicine, 153(3), 147–157. doi: 10.7326/0003-4819-153-3-201008030-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia D, Granjard A, Lundblad S & Archer T (2017). A dark past, a restrained present, and an apocalyptic future: Time perspective, personality, and life satisfaction among anorexia nervosa patients. PeerJ, 5, e3801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurnani V, Beattie TS, Bhattacharjee P, Team C, Mohan HL, Maddur S, Washington R, Isac S, Ramesh BM, Moses S & Blanchard JF (2011). An integrated structural intervention to reduce vulnerability to HIV and sexually transmitted infections among female sex workers in Karnataka state, south India. BMC Public Health, 11, 755. doi: 10.1186/1471-2458-11-755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harder DH & Zalma A (1990). Two promising shame and guilt scales: A construct validity comparison. Journal of Personality Assessment, 55(3–4), 729–745. doi: 10.1080/00223891.1990.9674108 [DOI] [PubMed] [Google Scholar]
- Hayaki J, Anderson B & Stein M (2006). Sexual risk behaviors among substance users: Relationship to impulsivity. Psychology of Addictive Behaviors, 20(3), 328–332. doi: 10.1037/0893-164X.20.3.328 [DOI] [PubMed] [Google Scholar]
- Head KJ, Noar SM, Iannarino NT & Harrington NG (2013). Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med, 97, 41–48. [DOI] [PubMed] [Google Scholar]
- Hodgins DC & Engel A (2002). Future time perspective in pathological gamblers. Journal of Nervous and Mental Disease, 190(11), 775–780. doi: 10.1097/01.NMD.0000038173.64197.93 [DOI] [PubMed] [Google Scholar]
- Holman EA, Silver RC, Mogle JA & Scott SB (2016). Adversity, time, and well-being: A longitudinal analysis of time perspective in adulthood. Psychology and Aging, 31(6), 640–651. doi: 10.1037/pag0000115 [DOI] [PubMed] [Google Scholar]
- Hsieh MH, Tsai SL, Tsai CH, Hsu YC & Hsu MT (2017). What is the addiction world like? Understanding the lived experience of the individuals’ illicit drug addiction in Taiwan. Perspectives in Psychiatric Care, 53(1), 47–54. [DOI] [PubMed] [Google Scholar]
- Hulka LM, Vonmoos M, Preller KH, Baumgartner MR, Seifritz E, Gamma A & Quednow BB (2015). Changes in cocaine consumption are associated with fluctuations in self-reported impulsivity and gambling decision-making. Psychological Medicine, 45(14), 3097–3110. doi: 10.1017/S0033291715001063 [DOI] [PubMed] [Google Scholar]
- Iñiguez-Stevens E, Brouwer KC, Hogg RS, Patterson TL, Lozada R, Magis-Rodriguez C, Elder JP, Viani RM & Strathdee SA (2009). [estimating the 2006 prevalence of HIV by gender and risk groups in Tijuana, Mexico]. Gaceta Medica de México, 145(3), 189–195. [PMC free article] [PubMed] [Google Scholar]
- InTec Products. (2002). Advanced quality TM rapid anit-HIV (1 &2) package insert. In (Vol. Cat. No. ITP02002.).
- Iwanicka K, Gerhant A & Olajossy M (2017). Psychopathological symptoms, defense mechanisms and time perspectives among subjects with alcohol dependence (ad) presenting different patterns of coping with stress. PeerJ, 5, e3576. doi: 10.7717/peerj.3576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeal N, Macleod J, Salisbury C & Turner K (2017). Identifying possible reasons why female street sex workers have poor drug treatment outcomes: A qualitative study. BMJ Open, 7(3), e013018. doi: 10.1136/bmjopen-2016-013018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR & Johnson PS (2015a). Cocaine dependent individuals discount future rewards more than future losses for both cocaine and monetary outcomes. Addictive Behaviors, 40, 132–136. doi: 10.1016/j.addbeh.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Johnson PS, Herrmann ES & Sweeney MM (2015. b). Delay and probability discounting of sexual and monetary outcomes in individuals with cocaine use disorders and matched controls. PloS One, 10(5), e0128641. doi: 10.1371/journal.pone.0128641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Hong H, Lee J & Hyun MH (2017). Effects of time perspective and self-control on procrastination and internet addiction. Journal of Behavioral Addictions, 6(2), 229–236. doi: 10.1556/2006.6.2017.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN & Petry NM (2004). Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction, 99(4), 461–471. doi: 10.1111/j.1360-0443.2003.00669.x [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM & Bickel WK (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128(1), 78–87. [DOI] [PubMed] [Google Scholar]
- Klingemann H (2001). The time game: Temporal perspectives of patients and staff in alcohol and drug treatment. Time & Society, 10(2–3), 303–328. [Google Scholar]
- Koffarnus MN, Johnson MW, Thompson-Lake DG, Wesley MJ, Lohrenz T, Montague PR & Bickel WK (2016). Cocaine-dependent adults and recreational cocaine users are more likely than controls to choose immediate unsafe sex over delayed safer sex. Experimental and Clinical Psychopharmacology, 24(4), 297–304. doi: 10.1037/pha0000080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köstering L, Schmidt CS, Egger K, Amtage F, Peter J, Klöppel S, Beume LA, Hoeren M, Weiller C & Kaller CP (2015). Assessment of planning performance in clinical samples: Reliability and validity of the Tower of London task (TOL-F). Neuropsychologia, 75, 646–655. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Mattson RE, Anderson Mackillop EJ, Castelda BA & Donovick PJ (2007). Multidimensional assessment of impulsivity in undergraduate hazardous drinkers and controls. Journal of Studies on Alcohol and Drugs, 68(6), 785–788. [DOI] [PubMed] [Google Scholar]
- Markus H & Nurius P (1986). Possible selves. American Psychologist, 41(9), 954–969. [Google Scholar]
- Martoni RM, de Filippis R, Cammino S, Giuliani M, Risso G, Cavallini MC & Bellodi L (2017). Planning functioning and impulsiveness in obsessive-compulsive disorder. European Archives of Psychiatry and Clinical Neuroscience. doi: 10.1007/s00406-017-0803-0 [DOI] [PubMed] [Google Scholar]
- Miller W & Rollnick S (1991). Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press. [Google Scholar]
- Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC & Grabowski J (2001). The impact of impulsivity on cocaine use and retention in treatment. Journal of Substance Abuse Treatment, 21(4), 193–198. [DOI] [PubMed] [Google Scholar]
- Montoya JL, Georges S, Poquette A, Depp CA, Atkinson JH, Moore DJ & Translational Methamphetamine AIDS Research Center Group. (2014). Refining a personalized mHealth intervention to promote medication adherence among HIV+ methamphetamine users. AIDS Care, 26(12), 1477–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskalewicz M (2016). Lived time disturbances of drug addiction therapy newcomers. A qualitative, field phenomenology case study at Monar-Markot Center in Poland. International Journal of Mental Health and Addiction, 14(6), 1023–1038. doi: 10.1007/s11469-016-9680-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngugi E, Benoit C, Hallgrimsdottir H, Jansson M & Roth EA (2012). Partners and clients of female sex workers in an informal urban settlement in Nairobi, Kenya. Culture, Health & Sexuality, 14(1), 17–30. doi: 10.1080/13691058.2011.608436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngugi EN, Chakkalackal M, Sharma A, Bukusi E, Njoroge B, Kimani J, MacDonald KS, Bwayo JJ, Cohen CR, Moses S, Kaul R & Kibera HIV Study Group (2007). Sustained changes in sexual behavior by female sex workers after completion of a randomized HIV prevention trial. Journal of Acquired Immune Deficiency Syndromes, 45(5), 588–594. doi: 10.1097/QAI.0b013e3180f616db [DOI] [PubMed] [Google Scholar]
- Obong’o CO, Alexander AC, Chavan PP, Dillon PJ & Kedia SK (2017). Choosing to live or die: Online narratives of recovering from methamphetamine abuse. Journal of Psychoactive Drugs, 49(1), 52–58. doi: 10.1080/02791072.2016.1262085 [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, Orozovich P, Abramovitz D, De la Torre A & Amaro H (2008a). Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. American Journal of Public Health, 98(11), 2051–2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, Orozovich P, Staines H, Amaro H, Magis-Rodriguez C & Strathdee SA (2006). Comparison of sexual and drug use behaviors between female sex workers in Tijuana and Ciudad Juarez, Mexico. Substance Use and Misuse, 41(10–12), 1535–1549. doi: 10.1080/10826080600847852 [DOI] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, Philbin MM, Pu M, Fraga M, Amaro H, Torre Ade L, Martinez G, Magis-Rodriguez C & Strathdee SA (2008. b). Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. Journal of Infectious Diseases, 197(5), 728–732. doi: 10.1086/527379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Bickel WK & Arnett M (1998). Shortened time horizons and insensitivity to future consequences in heroin addicts. Addiction, 93(5), 729–738. [DOI] [PubMed] [Google Scholar]
- Petry NM & Casarella T (1999). Excessive discounting of delayed rewards in substance abusers with gambling problems. Drug and Alcohol Dependence, 56(1), 25–32. [DOI] [PubMed] [Google Scholar]
- Richert T (2015). Wasted, overdosed, or beyond saving--to act or not to act? Heroin users’ views, assessments, and responses to witnessed overdoses in malmö, sweden. International Journal on Drug Policy, 26(1), 92–99. doi: 10.1016/j.drugpo.2014.07.006 [DOI] [PubMed] [Google Scholar]
- Rolon ML, Syvertsen JL, Robertson AM, Rangel MG, Martinez G, Ulibarri MD, Servin A & Strathdee SA (2013). The influence of having children on HIV-related risk behaviors of female sex workers and their intimate male partners in two Mexico-US border cities. Journal of Tropical Pediatrics, 59(3), 214–219. doi: 10.1093/tropej/fmt009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sailer U, Rosenberg P, Nima AA, Gamble A, Garling T, Archer T & Garcia D (2014). A happier and less sinister past, a more hedonistic and less fatalistic present and a more structured future: Time perspective and well-being. PeerJ, 2, e303. doi: 10.7717/peerj.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR & Grant M (1993). Development of the alcohol use disorders identification test (audit): Who collaborative project on early detection of persons with harmful alcohol consumption‐ii. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Strathdee SA, Zians J & Patterson TL (2011). Methamphetamine-using parents: The relationship between parental role strain and depressive symptoms. Journal of Studies on Alcohol and Drugs, 72(6), 954–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servin AE, Reed E, Brouwer KC, Magis-Rodriguez C, Boyce S, Strathdee SA & Silverman JG (2017). Motherhood and risk for human immunodeficiency virus/sexually transmitted infections among female sex workers in the Mexico-US border region. Sexually Transmitted Diseases, 44(8), 477–482. doi: 10.1097/OLQ.0000000000000634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Abramovitz D, Lozada R, Martinez G, Rangel MG, Vera A, Staines H, Magis-Rodriguez C & Patterson TL (2013). Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: Results from a randomized controlled trial. PloS One, 8(6), e65812. doi: 10.1371/journal.pone.0065812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syvertsen JL, Robertson AM, Palinkas LA, Rangel MG, Martinez G & Strathdee SA (2013). ‘Where sex ends and emotions begin’: Love and HIV risk among female sex workers and their intimate, non-commercial partners along the Mexico-US border. Culture, Health & Sexuality, 15(5), 540–554. doi: 10.1080/13691058.2013.773381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamene MM, Tessema GA & Beyera GK (2015). Condom utilization and sexual behavior of female sex workers in northwest Ethiopia: A cross-sectional study. Pan African Medical Journal, 21, 50. doi: 10.11604/pamj.2015.21.50.6009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teuscher U & Mitchell SH (2011). Relation between time perspective and delay discounting: A literature review. The Psychological Record, 61(4), 613–632. [Google Scholar]
- Trout CH, Dembele O, Diakite D, Bougoudogo F, Doumbia B, Mathieu J, Haidara A, Sangare A, Traore S, Burtner J, Cabral H & Messersmith LJ (2015). West African female sex workers in mali: Reduction in HIV prevalence and differences in risk profiles of sex workers of differing nationalities of origin. Journal of Acquired Immune Deficiency Syndromes, 68 Suppl 2, S221–231. doi: 10.1097/QAI.0000000000000444 [DOI] [PubMed] [Google Scholar]
- Tse S, Yuen YM & Suto M (2014). Expected possible selves and coping skills among young and middle-aged adults with bipolar disorder. East Asian Archives of Psychiatry, 24(3), 117–124. [PubMed] [Google Scholar]
- UNAIDS. (2016). Global report. 11 November 2017. Retrieved from http://www.unaids.org/en/regionscountries/countries/mexico
- Voils CI, Gierisch JM, Yancy WS Jr., Sandelowski M, Smith R, Bolton J & Strauss JL (2014). Differentiating behavior initiation and maintenance: Theoretical framework and proof of concept. Health Education and Behavior, 41(3), 325–336. doi: 10.1177/1090198113515242 [DOI] [PubMed] [Google Scholar]
- Vrijens B, Vincze G, Kristanto P, Urquhart J & Burnier M (2008). Adherence to prescribed antihypertensive drug treatments: Longitudinal study of electronically compiled dosing histories. BMJ, 336(7653), 1114–1117. doi: 10.1136/bmj.39553.670231.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward H & Aral SO (2006). Globalisation, the sex industry, and health. Sexually Transmitted Infections, 82(5), 345–347. doi: 10.1136/sti.2006.023044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster JD (2011). A new measure of time perspective: Initial psychometric findings for the Balanced Time Perspective Scale (BTPS). Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 43(2), 111. [Google Scholar]
- Yadav G, Saskin R, Ngugi E, Kimani J, Keli F, Fonck K, Macdonald KS, Bwayo JJ, Temmerman M, Moses S, Kaul R & Kibera HIVSG (2005). Associations of sexual risk taking among Kenyan female sex workers after enrollment in an HIV-1 prevention trial. Journal of Acquired Immune Deficiency Syndromes, 38(3), 329–334. [PubMed] [Google Scholar]
- Yuen WW, Tran L, Wong CK, Holroyd E, Tang CS & Wong WC (2016). Psychological health and HIV transmission among female sex workers: A systematic review and meta-analysis. AIDS Care, 28(7), 816–824. doi: 10.1080/09540121.2016.1139038 [DOI] [PubMed] [Google Scholar]
- Zhang L, Shah IH, Li X, Zhou Y, Zhang C, Zhang L, Zhang X, Cui Y & Xu J (2017). Does the use of HIV testing and counseling services influence condom use among low-paid female sex workers in Guangxi, China? AIDS Care, 29(3), 335–338. doi: 10.1080/09540121.2016.1220482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimbardo PG & Boyd JN (1999). Putting time in perspective: A valid, reliable individual-differences metric. Journal of Personality and Social Psychology, 6, 1271–1288. [Google Scholar]


