Dear Editor,
I am Dr. Erick Hernandez-Bogantes from the Department of Cornea and Refractive Surgery, Conde of Valenciana Foundation Institute of Ophthalmology, Mexico City, Mexico. The purpose of this letter is to present 3 cases (6 eyes) of toxic anterior segment syndrome (TASS) after same day implantation of a posterior phakic implantable collamer lens (ICL; V4c Visian ICL; STAAR Surgical, Monrovia, CA, USA).
TASS is a rare condition characterized by postoperative inflammation mostly after uneventful anterior segment surgery that occurs within the first 12-48h after surgery[1]. Overall, between 3 and 20 cases of TASS occurs each year in the USA[2]. Besides cataract surgery, TASS has also been reported after various types of anterior segment procedures such as anterior phakic intraocular lens (pIOL) implantation[3], penetrating keratoplasty[4], deep anterior lamellar keratoplasty[5] and triple Descemet's stripping automated endothelial keratoplasty[6]. Several etiologies including retained lens material, viscosurgical devices, glove talc, intracameral antibiotics and endotoxin contamination of balanced salt solution have been identified[7].
After awareness of our successive cases of TASS following the implantation of a lens consisting of a biocompatible collagen copolymer V4c Visian ICL we decided to document these cases in order to find out possible causes. To the best of our knowledge, this is the first case series of TASS after a posterior pIOL implantation.
The first case is a 34-year-old female with high myopia and keratoconus with previous intracorneal ring segment implantation presented for bioptics refractive surgery. Preoperative best-corrected visual acuity (BCVA) was 0.1 logMAR (20/25) and underwent uneventful V4c Visian ICL implantation surgery. On the first day follow-up, the patient complained of decreased vision and photophobia. Her vision was 0.3 logMAR (20/40) and presented with conjunctival hyperemia, mild corneal edema, 2+ cells with no hypopyon and normal fundus examination. The lens had multiple white deposits located at the concave posterior surface area showed by optical coherence tomography (Figure 1). Hourly topical prednisolone 1% was started and tapered according to her symptoms and follow-up. At week 6 the BCVA returned to 0.1 logMAR (20/25) with no signs of inflammation and the deposits on the lens decreased significantly (Figure 2).
Figure 1. Anterior segment optical coherence tomography plot.
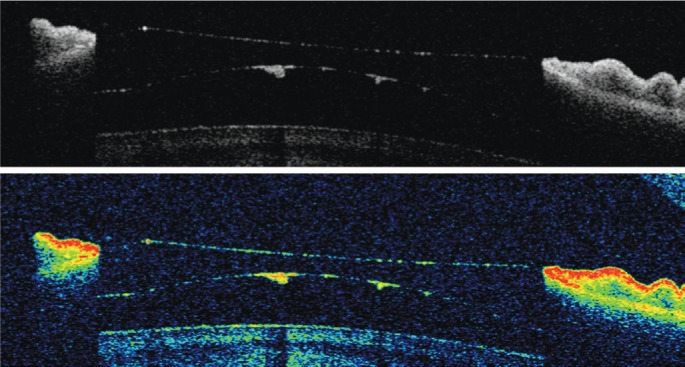
Deposits are placed in the posterior concave surface of the lens.
Figure 2. Consecutive clinical retro-illumination slit-lamp photographs of the left eye.
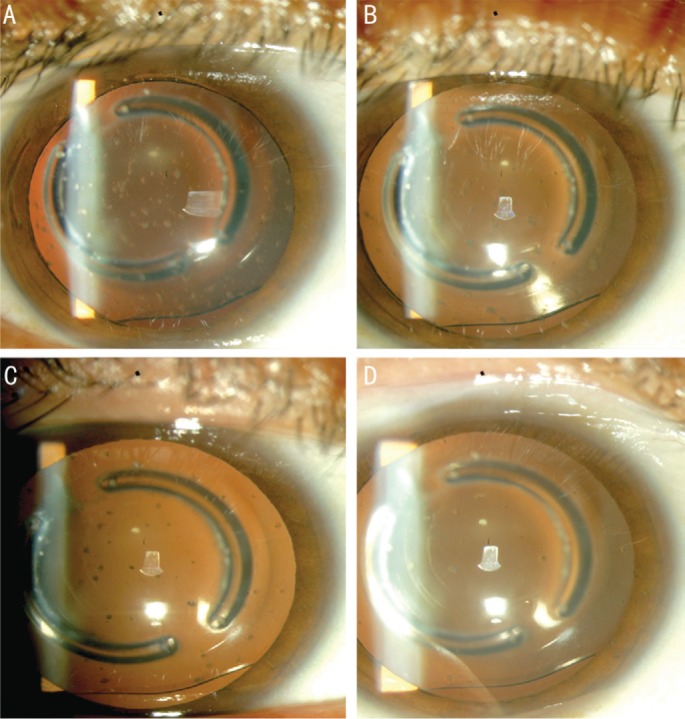
A: The white deposits were numerous during the first day of diagnosis; B, C, D: After only intense topical steroid treatment the deposits decreased over time until the ICL almost become clear.
The second case is a 27-year-old patient with high myopia who had previously consulted for a second opinion regarding posterior phakic collamer intraocular lens procedure. Twenty-four hours after the surgery the left eye presented with a decrease in vision and severe intraocular inflammation. Biomicroscopy examination revealed conjunctival hyperemia, corneal edema, 3+ cells, flare and a pupillary membrane. Treatment consisted in topical prednisolone 1% every hour, and a one-time 2 mg betamethasone periocular injection and cyclopegic drops, which resulted in a completed detachment of the pupillary membrane. Five weeks after treatment there was no sign of intraocular inflammation, however, the BCVA declined to 0.2 logMAR (20/30).
Lastly a 25-year-old Caucasian male with high myopia presented for refractive surgery options. Two days after posterior pIOL implantation, white deposits on the lens optic were found during biomicroscopy examination (Figure 3). The patient was aymptomatic with neither corneal edema nor signs of inflammation with a visual acuity of 0.0 logMAR (20/20). Intensive topical steroids and cyclopegic drops were started and one week after treatment deposits decreased in size and density.
Figure 3. Clinical biomicroscopy image of the white deposits throughout the lens.
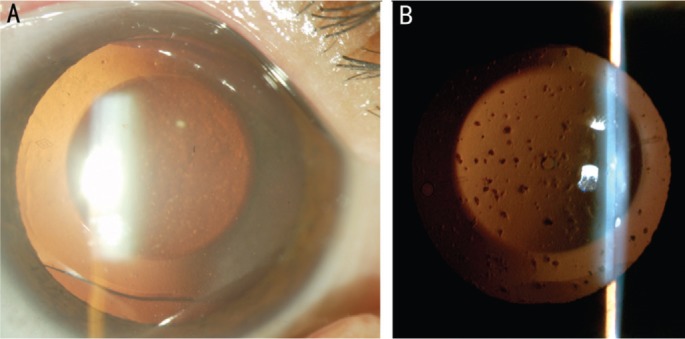
A: Corneal edema and white deposits are notices; B: Retro-illumination shows the density of these deposits.
Currently, there have been more than 775 000 ICL implanted worldwide. In 2014, Gomez-Bastar et al[8] retrospectively reviewed 349 eyes of 216 patients with ICL implantation reporting low incidences of postoperative complications with only one eye (0.29%) presenting TASS. A long-term retrospective study by Moya et al[9] of 144 eyes reported no cases of TASS. Few reports of TASS after pIOL have been published, most of them from anterior chamber pIOL cases[3],[10]–[11] and only one case-report following ICL[7].
In this case series, all surgeries were performed by the same surgeon (Hernandez-Bogantes E) on the same day without any associated complications. In our analysis the most probable cause was the handling of the ICLs or instrument tips with powdered-gloves as reported by the surgeon. Bodnar et al[12] reported that 21% of TASS could be caused by the inadequate manipulation of IOLs and surgical instruments with powdered gloves. Another potential factor could have been intracameral fluids and medications used during the surgeries, such as the use of preserved epinephrine, ophthalmic viscoelastic devices and topical anesthetic agents. Also, the sterilization technique was completely reviewed to avoid future breakdowns. Other eyes that underwent ICL implantation on the same day using the same balanced salt solution lot did not develop TASS.
In conclusion TASS is a rare complication after ICL implantation. Early diagnosis and management is essential to prevent long-term sequelae. The most important step is prevention with adequate intraoperative manipulation of the ICL, surgical instruments and intracameral fluids. Protocols and guidelines like the TASS Task Force from the Association of Cataract and Refractive Surgeons (http://www.ascrs.org/tass-registry) have been created to help minimize potential risk factors.
Acknowledgments
Conflicts of Interest: Hernandez-Bogantes E, None; Ramirez-Miranda A, None; Olivo-Payne A, None; Abdala-Figuerola A, None; Navas A, None; Graue-Hernandez EO, None.
REFERENCES
- 1.Holland SP, Morck DW, Lee TL. Update on toxic anterior segment syndrome. Curr Opin Ophthalmol. 2007;18(1):4–8. doi: 10.1097/ICU.0b013e3280117d0c. [DOI] [PubMed] [Google Scholar]
- 2.Eydelman MB, Tarver ME, Calogero D, Buchen SY, Alexander KY. The food and drug administration's proactive toxic anterior segment syndrome program. Ophthalmology. 2012;119(7):1297–1302. doi: 10.1016/j.ophtha.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 3.van Philips LA. Toxic anterior segment syndrome after foldable artiflex iris-fixated phakic intraocular lens implantation. J Ophthalmol. 2011;119(7):1297–1302. doi: 10.1155/2011/982410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maier P, Birnbaum F, Bohringer D, Reinhard T. Toxic anterior segment syndrome following penetrating keratoplasty. Arch Ophthalmol. 2008;126(12):1677–1681. doi: 10.1001/archopht.126.12.1677. [DOI] [PubMed] [Google Scholar]
- 5.Sevimli N, Karadag R, Cakici O, Bayramlar H, Okumus S, Sari U. Toxic anterior segment syndrome following deep anterior lamellar keratoplasty. Arq Bras Oftalmol. 2016;79(5):330–332. doi: 10.5935/0004-2749.20160094. [DOI] [PubMed] [Google Scholar]
- 6.Sorkin N, Varssano D. Toxic anterior segment syndrome following a triple descemet's stripping automated endothelial keratoplasty procedure. Case Rep Ophthalmol. 2012;3(3):406–409. doi: 10.1159/000345531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006;32(2):324–333. doi: 10.1016/j.jcrs.2006.01.065. [DOI] [PubMed] [Google Scholar]
- 8.Gomez-Bastar A, Jaimes M, Graue-Hernandez EO, Ramirez-Luquin T, Ramirez-Miranda A, Navas A. Long-term refractive outcomes of posterior chamber phakic (spheric and toric implantable collamer lens) intraocular lens implantation. Int Ophthalmol. 2014;34(3):583–590. doi: 10.1007/s10792-013-9860-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moya T, Javaloy J, Montes-Mico R, Beltran J, Munoz G, Montalban R. Implantable collamer lens for myopia: assessment 12 years after implantation. J Refract Surg. 2015;31(8):548–556. doi: 10.3928/1081597X-20150727-05. [DOI] [PubMed] [Google Scholar]
- 10.Moshirfar M, Whitehead G, Beutler BC, Mamalis N. Toxic anterior segment syndrome after verisyse iris-supported phakic intraocular lens implantation. J Cataract Refract Surg. 2006;32(7):1233–1237. doi: 10.1016/j.jcrs.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Kremer I, Levinger E, Levinger S. Toxic anterior segment syndrome following iris-supported phakic IOL implantation with viscoelastic multivisc BD. Eur J Ophthalmol. 2010;20(2):451–453. doi: 10.1177/112067211002000229. [DOI] [PubMed] [Google Scholar]
- 12.Bodnar Z, Clouser S, Mamalis N. Toxic anterior segment syndrome: update on the most common causes. J Cataract Refract Surg. 2012;38(11):1902–1910. doi: 10.1016/j.jcrs.2012.06.053. [DOI] [PubMed] [Google Scholar]


