Abstract
The purpose of the study was to determine whether low‐high fidelity medical simulation improves learning and long‐lasting retention of pharmacology knowledge, compared to lecture alone, in undergraduate medical students. Ninety students, before a 45‐minute lecture, were randomized into three groups ‐ sham (S), low (LF), and high fidelity (HF) simulation ‐ to participate in an interactive simulation session. To evaluate immediate and long‐lasting retention, a 20‐item structured questionnaire on inotropic agents was administered to 90 students before and after a 45‐minute lecture, after simulation, and 3 months later. In all groups, the rate of correct answers increased after lecture, while no difference was observed between different groups (P = 0.543). After simulation, students in the HF group provided more correct answers compared to S or LF group (P > 0.001). After 3 months, a significant decrease in the number of correct answers was observed in S (P < 0.001) and LF (P < 0.001) groups, but not in the HF group (P = 0.066). Moreover, HF simulation resulted in an increased number of correct answers compared to the LF (P < 0.001) or S simulation (P < 0.001). These data suggest that advanced medical simulation teaching applied to pharmacology is associated with more effective learning and long‐lasting retention compared to lecture alone.
Keywords: clinical skills, medical education research, pharmacology, simulation
Abbreviations
- BLS
basic life support
- HF
high fidelity
- LF
low fidelity
1. INTRODUCTION
Traditional lectures in pharmacology for medical students are nowadays a matter of debate.1 The study and comprehension of pharmacological properties of the active principles of drugs will determine their correct use in daily practice. Indeed, the acquisition of theoretical knowledge is commonly promoted by lectures. Lectures, in fact, provide “information” useful to answer “who,” “what,” “where,” and “when” questions. However, “knowledge” needs the implementation of information that allows one to answer the “how” questions. Moreover, “understanding” is an essential crossing‐point, ie, comprehension of “why” we act. Finally, the ability to evaluate understanding in different contexts refers to “wisdom,” that allows us to make choices considering most of the possible variables.2
In this context, lectures represent the cultural background for the future physician. However, medical students need to acquire information on pharmacodynamics, pharmacokinetic, and toxicological issues, but they also need the appropriate clinical reasoning skills for long‐term retention of the “knowledge” regarding drug action, kinetics, and safety. The aim was to teach how to manage the complex interplay between patient condition, evaluated by vital signs and physical assessment, and drug efficacy and safety. Therefore, undergraduate medical students should combine basic pharmacological knowledge with the acquisition of clinical skills to improve the quality of care in daily clinical practice.1, 2, 3 To reach this target, an educational program that integrates the learning of pharmacology with clinical simulation of technical skills must also be effective and should be appropriately allocated during the 6‐year course in medicine, leading to the improvement inpharmacology knowledge, skills and aptitude of medical students.4
In this context, medical simulation represents an efficacious educational tool for medical students’ training, boosting patient‐centered medical learning, and improving aptitude and knowledge.4, 5, 6, 7, 8, 9, 10 In the education of undergraduate medical students, simulation appears to be valid, facilitates the acquisition of clinical reasoning skills, and minimizes clinical risk for the patient.11, 12 In fact, simulation offers a relatively realistic setting where medical students can familiarize themselves with standardized clinical scenarios, and may repeatedly perform practice procedures without any risk for patients.
Learning based on simulation, in particular the use of high‐fidelity mannequins to enhance medical training, has gained an important role in the last decade in the teaching of several disciplines in medicine leading to error reduction and improved safety, as well as in other health professions such as pharmacy and nursing.12, 13, 14, 15, 16, 17 Medical simulation favors the acquisition of critical thinking, problem solving, and teamwork skills in medical students.18 It allows the reproduction of several disease states 11 and offers the opportunity to operate with safety, bridging the gap between theory and practice.19
Fidelity in simulation has traditionally been defined as “the degree to which the simulator replicates reality”. Using this definition, low fidelity has been defined as simulations that are static and lack realism. Examples of low fidelity would be what are referred to as “task trainers” technology such as a prosthetic arm that can be used to learn how to administer intramuscular injections or take blood pressure readings.20
High fidelity simulation includes computerized mannequins that are operated by a technician from another location to produce audible sounds and to alter and manage physiological changes within the mannequins such as altering the heart rate, respiration, chest sounds, and saturation of oxygen, for example.21
There are few published data on the application of the simulation method to the pharmacology discipline in medical school, nor comparative data with traditional teaching.22, 23, 24, 25
High fidelity simulators are now being used with increasing frequency in the pharmacological training of medical students as they enable students to develop and refine medical competency in a nonthreatening, safe environment. Therefore, high fidelity patient simulators might be a valuable tool in helping to improve pharmacology knowledge in medical students.26
In light of these observations, we investigated whether low and high fidelity medical simulation might be more effective than traditional lectures in inducing effective learning and long‐lasting retention of pharmacology knowledge in undergraduate medical students.
2. MATERIALS AND METHODS
2.1. Study design, study population, and exposure definition
A parallel group, randomized study was used in this research. The study population consisted of fifth year students of the medical school of the University of Messina, attending the mandatory course “Pharmacology, Toxicology and Evidence – Based Medicine”. During the course, students were invited to attend a seminar on “Positive Inotropic Drugs.” They were unaware of the lecture topic and had not been previously exposed to it in their medical school curriculum. Before starting the lecture, students were asked to participate voluntarily in the study.
From a total of 225 students, 90 students accepted to participate in the study and underwent a 45‐minute traditional lecture on inotropic agents. At the end of the lecture, students were randomized into three groups: sham simulation (Sham), low‐fidelity simulation (LF), and high‐fidelity simulation (HF) and underwent a 45‐minute interactive simulation training in an operating room scenario. Sham students were exposed to a basic life support (BLS) retraining scenario with a full‐body Resusci Anne unit (Laerdal), during which no reference to medications was made. LF and HF students were exposed to a cardiogenic shock scenario during which they were asked to identify, diagnose, and suggest pharmacological therapy. Three different simulators were used: a task trainer for the Sham group, an adult, full‐body basic simulation training unit (Laerdal) for the LF group, and a high‐fidelity adult, full‐body ALS Simulator with wireless SimPad System (Laerdal) for the HF group.
Student learning on inotropic drugs was evaluated at basal time, after lecture, after simulation, and 90 days following the simulation.
2.2. Learning evaluation
To assess effective learning and long‐lasting retention, a 20 multiple‐choice‐question questionnaire on positive inotropic drugs was administered at several time intervals: at baseline, after lecture, immediately after simulation (either Sham or LF or HF) and 3 months after simulation to obtain information on long‐lasting retention, as previously suggested.27, 28 A 20‐minute period was allowed to complete the questionnaire.
To minimize biases due to consultation of other sources of learning, students involved in the study were briefed about the test only 10 minutes before administering the questionnaire. Moreover, the order of the same 20 questions was randomly assigned for each questionnaire, on each test. Students were blinded on how they performed on the previously administered tests.
The scores obtained in the four evaluation sessions were recorded and evaluated. The score was estimated assuming 1 for each correct and 0 for each wrong answer. The total score was calculated, for each student, as the sum of correct answers.
All results were expressed as median with inter quartile range for continuous variables, absolute and percentage frequencies for categorical variables. Between‐groups at each time point and within‐group comparisons were performed.
The result scored by a larger population of students attending the course of Pharmacology in the previous year was 12 + 4 correct answers. Consequently, we assumed a mean of 12 ± 4 correct answers after lecture in all groups of student and an increase of correct answers of 25% in students exposed to HF simulation compared to the Sham group. The minimum number needed to detect an 80% power with an α of 0.05, and a β error of 0.20 was 28 per group. Therefore, 30 students in each arm were considered to be an adequate number of study subjects.
2.3. Questionnaire content
A 20 multiple‐choice‐question test on inotropic agents was used. A panel of experts composed of six faculty members reviewed the questionnaire content for accuracy and provided appropriate modifications to ensure validity of the poll. Experts included pharmacologists, anesthesiologists, and cardiologists with wide prior experience in using inotropic agents. Moreover, a statistician and education and simulation specialists were involved.
2.4. Ethical considerations
Participation was voluntary, anonymous, and independent. Confidentiality of information was ensured; informed consent was obtained and no financial incentive to participate in the study was offered. Since all data were de‐identified and reported in aggregate, the local Ethics Committee deemed the study exempt from institutional review approval.
2.5. Statistical analysis
Descriptive statistical analyses were performed to evaluate the characteristics of students at basal time.
The Kolmogorov‐Smirnov test for normality was performed to evaluate normal distribution of numerical variables. Due to non‐normal distribution of some numerical variables and low sample size, which did not guarantee valid asymptotic results, a nonparametric approach was used.
To verify the efficacy of different interventions, differences among groups were evaluated. The Chi‐squared test and the Kruskal‐Wallis test for independent samples were applied to compare the exposition groups (Sham, LF, and HF) according to the characteristics of subjects, and the numerical score obtained from the test at the different time points (basal, after lecture, after simulation, and 90 days later). The Mann‐Whitney U test corrected by Bonferroni procedure was performed to realize the two‐by‐two comparisons of exposition groups for only covariates which were significant at the Kruskal‐Wallis test.
The Mann‐Whitney U test was also applied to assess the existence of significant differences between males and females with reference to the number of correct answers in each group, at all time points of observation.
To verify the learning curve in each group, differences in score during the study as paired measurements were evaluated. Differences between paired measurements in each group were tested by the Wilcoxon signed‐rank test. A two‐tailed P‐value set at 0.05 was considered to be statistically significant. Statistical analyses were performed using SPSS 20.0 software for the Windows package.
3. RESULTS
Students’ demographics and number of correct answers at the different time points are summarized in Table 1. Of the 90 students, 49 (54.4%) were female and 41 (45.6%) male. The median age of the enrolled participants was 23 (IQ 22‐24) years. The participants were randomized into three groups: Sham simulation students (N = 30), LF simulation students (N = 30), and HF simulation students (N = 30). No difference in age (P = 0.821) and sex (P = 0.956) was observed among groups (Table 1).
Table 1.
Characteristics of students according to exposition
| Sham N (%) | Low Fidelity N (%) | High Fidelity N (%) | P‐valuea | |
|---|---|---|---|---|
| Gender | ||||
| Female n (%) | 17 (56.7) | 16 (53.3) | 16 (53.3) | 0.956 |
| Male n (%) | 13 (43.3) | 14 (46.7) | 14 (46.7) | |
| Age median (IQ range) | 23 (22‐24) | 23 (22‐23) | 23 (22‐23) | 0.821 |
| Test score (0‐20); median (IQ range) | ||||
| Basal | 9 (8‐10.25) | 9 (8‐10) | 9 (8.75‐10) | 0.674 |
| Postlecture | 12 (11‐13) | 13 (12‐13.25) | 12 (11‐13) | 0.543 |
| Postsimulation | 13 (11‐14) | 13.5 (11‐15) | 17 (16‐18) | <0.001 |
| 90 days postsimulation | 11 (9.75‐12) | 11 (9‐12) | 16.5 (15.75‐17) | <0.001 |
Kruskal‐Wallis test for independent samples; between‐groups comparison.
The number of correct answers to questionnaire, at basal time, was similar among the experimental student groups (Table 1). Correct answers significantly increased after lecture, from 9 to 12 (P < 0.01), 9 to 13 (P < 0.01), and 9 to 12 (P < 0.01), in Sham, LF, and HF groups, respectively (Figure 1). However, no significant difference was observed in the performing scores among the different groups (P = 0.543; Figure 2B).
Figure 1.
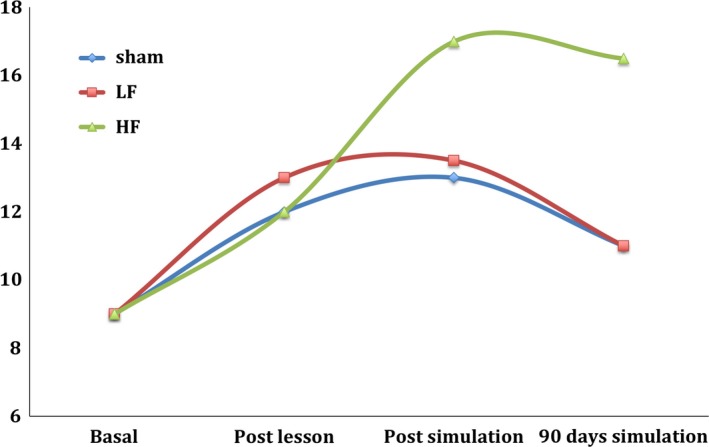
Correct answers (median), at each time point, stratified by group. Wilcoxon rank test; Within group comparison Sham group: lecture vs basal (W = −4.836; P < 0.01); simulation vs lecture (W = −0.685; P = 0.494); retention vs simulation (W = −3.965; P < 0.001) LF group: lecture vs basal (W = −4.810; P < 0.01); simulation vs lecture (W = −1.128; P = 0.259); retention vs simulation (W = −4.214; P < 0.001) HF group: lesson vs basal (W = −4.834; P < 0.01); simulation vs lecture (W = −4.727; P < 0.001); retention vs simulation (W = −1.837; P = 0.066)
Figure 2.
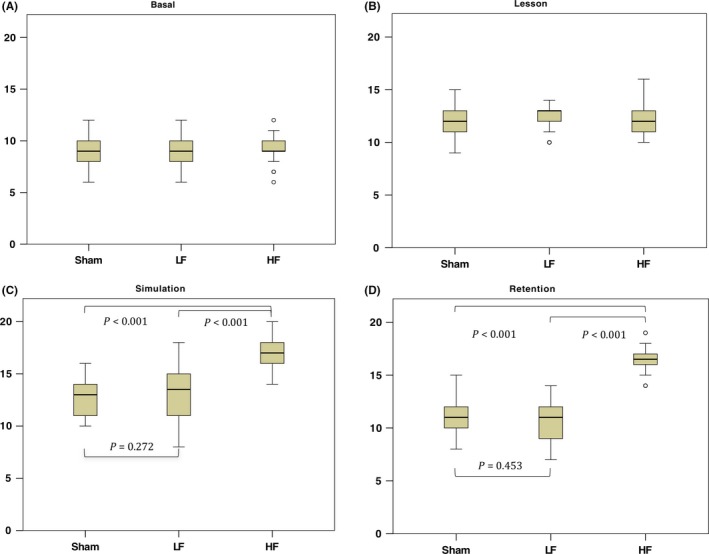
Correct answers reported (median plus interquartile range): between‐groups comparison at basal (A), after lecture (B), after simulation (C), 90 days thereafter (D). Mann‐Whitney U test for independent samples: between‐groups comparison
No differences were observed after the simulation in Sham (P = 0.494) and LF (P = 0.259) exposed students. On the contrary, HF simulation significantly increased the number of students’ correct answers (P < 0.001; Figure 1). Moreover, after simulation, a significant difference was observed among groups (P < 0.001; Table 1). In particular, the number of correct answers was significantly higher in the HF group compared to both Sham (P < 0.001) and LF (P < 0.001) groups, while no differences were observed between the Sham and LF groups (P = 0.272; Figure 2C).
The number of correct answers 90 days after the simulation significantly decreased in Sham (P < 0.001) and LF (P < 0.001) groups, while a lower but not significant decrease was observed in the HF group (P = 0.066; Figure 1).
Moreover, after 3 months, medical students who had undergone HF simulation gave a higher number of right answers (P < 0.001) than the others. Conversely, no differences were observed between Sham and LF exposed groups (P = 0.453; Figure 2D).
No differences were observed in the median number of correct answers corrected by sex and age, in each group, at all observation times.
4. DISCUSSION
The current study investigated whether low‐ and high‐fidelity medical simulation are more effective than traditional lectures in inducing effective learning and long‐lasting retention of pharmacology knowledge in undergraduate medical students.
Our study suggests that lectures induced a marked improvement in knowledge regarding inotropic drugs (the topic of the lecture). Indeed, a marked increase in the number of correct answers was observed in the postlecture test compared to baseline. This result confirms the value of lectures in inducing theoretical knowledge of pharmacology in undergraduate medical students. Previously published data suggest positive effects of education with high‐fidelity simulation in both medical and nursing students, as well as postgraduate students and residents.28, 29
In agreement with these findings, in our study, students exposed to high‐fidelity simulation significantly increased the number of correct answers to the questionnaire compared to the lecture. Surprisingly, low‐fidelity simulation, similar to Sham simulation, was unable to improve the effective learning of theoretical pharmacology knowledge. These results suggest that, at least when pharmacology knowledge needs to be integrated with a clinical practice intervention, a low fidelity scenario is insufficient to create significant improvement in learning.
Knowledge acquisition and maintenance are important. Several findings highlight that after a 3‐month period, in absence of reminders, the risk of knowledge and skill loss is consistent.29, 30 Accordingly, the number of correct answers decreased at 90 days in Sham and LF groups. By contrast, the number of positive answers, though reduced, was not significantly decreased in the HF simulation exposed students. This highlights that HF simulation is better than lecture alone or lecture plus low‐fidelity simulation in inducing long‐term retention of pharmacological knowledge, while the use of low‐fidelity simulation is inadequate.
We also investigated several factors that may predict correct answers to the questionnaire. We found that HF simulation is strongly associated with the final end‐point of the study, independently from other variables, such as age or sex.
Some limitations in our study should also be taken into account. It could be argued that the higher score observed in the HF simulation group might be due to the previous curriculum: in particular, difference in the scores of previous exams might have influenced the final results and concur to determine a better performance. Indeed, this issue was not evaluated for privacy reasons, therefore generating a potential bias. However, no significant difference in the number of right answers among the groups was observed at either baseline or after lecture, thus confirming that medical students had the same degree of pharmacology knowledge, and ruling out the hypothesis that differences in previous performances might have influenced the results of the questionnaire.
The repetition of the same questions in the tests between sessions represents the correct methodological approach to analyze the efficacy of exposure. However, it is possible that, after the first test, some students may have discussed the questions/answers, resulting in the increase in correct test answers at the second test. Nevertheless, differences among groups were shown after the simulation and long‐term retention assessment and are unlikely that a differential bias was generated. In addition, although the structured questionnaire was internally validated based on consensus of the experts, it was never tested for reliability. We do not know if a longer time‐frame of more than 90 days, in the absence of reminders, could reduce the effectiveness of high fidelity simulation.
We did not evaluate costs for the simulation. As a consequence, we did not establish the cost benefit relationship in using high‐fidelity versus low‐fidelity versus lecture. However, faculty number and time was similar in high and low fidelity simulation.
In conclusion, in the learning environment considered, and with possible limitations related to the physical locations, contexts, and cultures in which students learn, the association of high fidelity simulation scenarios to traditional pharmacology education programs promote more effective pharmacology learning retention than the traditional lecture alone. These results are in accordance with the developing international literature supporting the use of simulation in the pharmacology education of undergraduate students.31, 32, 33 However, while our results support the use of high‐fidelity simulation, low‐fidelity simulation does not significantly improve student retention. More extensive research is needed to look at long‐term effects of simulation interventions regarding retention of knowledge and acquired skills.
AUTHOR CONTRIBUTIONS
V. A., F. S., V. F. designed the experiment; M. L., P. O., A. A., B. R., T. V. acquired the data; A. A. l., V. A. performed statistics; V. A., F. S., A. B., D. A., V. F. wrote the paper; I. P. and S. P. critically revised the paper. All the authors have revised and approved the final version of the manuscript.
DISCLOSURE
All the authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
The work was supported by Departmental funding assigned to Prof. F. Squadrito.
Arcoraci V, Squadrito F, Altavilla D, et al. Medical simulation in pharmacology learning and retention: A comparison study with traditional teaching in undergraduate medical students. Pharmacol Res Perspect. 2018;e449 10.1002/prp2.449
Vincenzo Arcoraci and Francesco Squadrito equally contributed to this paper.
REFERENCES
- 1. Gwee MC. Teaching of medical pharmacology: the need to nurture the early development of desired attitudes for safe and rational drug prescribing. Med Teach. 2009;31:847‐854. [DOI] [PubMed] [Google Scholar]
- 2. Corrao S, Arcoraci V, Arnone S, et al. Evidence‐based knowledge management: an approach to effectively promote good health‐care decision‐making in the Information Era. Intern Emerg Med. 2009;4:99‐106. [DOI] [PubMed] [Google Scholar]
- 3. Michel MC, Bischoff A, Jakobs KH. Comparison of problem‐and lecture‐based pharmacology teaching. Trends Pharmacol Sci. 2002;23:168‐170. [DOI] [PubMed] [Google Scholar]
- 4. Fodale V, Penna O, Amato A, et al. Role of advanced simulation in undergraduate and postgraduate medical education. International Archives of Medicine. 2015;8:1‐11. [Google Scholar]
- 5. McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation‐based mastery learning with translational outcomes. Med Educ. 2014;48:375‐385. [DOI] [PubMed] [Google Scholar]
- 6. McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation‐based medical education with deliberate practice yield better results than traditional clinical education? A meta‐analytic comparative review of the evidence. Acad Med. 2011;86:706‐711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation‐based medical education research: 2003‐2009. Med Educ. 2010;44:50‐63. [DOI] [PubMed] [Google Scholar]
- 8. Moreno‐Ger P, Torrente J, Bustamante J, Fernandez‐Galaz C, Fernandez‐Manjon B, Comas‐Rengifo MD. Application of a low‐cost web‐based simulation to improve students’ practical skills in medical education. Int J Med Inform. 2010;79:459‐467. [DOI] [PubMed] [Google Scholar]
- 9. Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg SB. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35:e1511‐e1530. [DOI] [PubMed] [Google Scholar]
- 10. Parekh A, Thorpe T. How should we teach undergraduates in simulation scenarios? Clin Teach. 2012;9:280‐284. [DOI] [PubMed] [Google Scholar]
- 11. Gesundheit N, Brutlag P, Youngblood P, Gunning WT, Zary N, Fors U. The use of virtual patients to assess the clinical skills and reasoning of medical students: initial insights on student acceptance. Med Teach. 2009;31:739‐742. [DOI] [PubMed] [Google Scholar]
- 12. Oliven A, Nave R, Hasson‐Gilad DR, Baruch A. Medical students’ views on the use of virtual patients for teaching and assessment of clinical knowledge and reasoning. Harefuah. 2013;152:257‐261, 310 [PubMed] [Google Scholar]
- 13. Alinier G, Hunt WB, Gordon R. Determining the value of simulation in nurse education: study design and initial results. Nurse Educ Pract. 2004;4:200‐207. [DOI] [PubMed] [Google Scholar]
- 14. Cant RP, Cooper SJ. Simulation‐based learning in nurse education: systematic review. J Adv Nurs. 2010;66:3‐15. [DOI] [PubMed] [Google Scholar]
- 15. Gordon JA, Wilkerson WM, Shaffer DW, Armstrong EG. “Practicing” medicine without risk: students’ and educators’ responses to high‐fidelity patient simulation. Acad Med. 2001;76:469‐472. [DOI] [PubMed] [Google Scholar]
- 16. McIvor WR. Experience with medical student simulation education. Crit Care Med. 2004;32:S66‐S69. [DOI] [PubMed] [Google Scholar]
- 17. Ray SM, Wylie DR, Shaun Rowe A, Heidel E, Franks AS. Pharmacy student knowledge retention after completing either a simulated or written patient case. Am J Pharm Educ. 2012;76:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high‐fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27:10‐28. [DOI] [PubMed] [Google Scholar]
- 19. Weller JM. Simulation in undergraduate medical education: bridging the gap between theory and practice. Med Educ. 2004;38:32‐38. [DOI] [PubMed] [Google Scholar]
- 20. Seropian MA, Brown K, Gavilanes JS, Driggers B. Simulation: not just a manikin. J Nurs Educ. 2004;43:164‐169. [DOI] [PubMed] [Google Scholar]
- 21. Bray B, Schwartz CR, Weeks DL, Kardong‐Edgren S. Human patient simulation technology: perceptions from multidisciplinary sample of health care educators. Clinical Simulation of Nursing. 2009;5:6. [Google Scholar]
- 22. Hassan Z, DiLorenzo A, Sloan P. Teaching clinical opioid pharmacology with the Human Patient Simulator. J Opioid Manag. 2010;6:125‐132. [DOI] [PubMed] [Google Scholar]
- 23. Mueller MP, Christ T, Dobrev D, et al. Teaching antiarrhythmic therapy and ECG in simulator‐based interdisciplinary undergraduate medical education. Br J Anaesth. 2005;95:300‐304. [DOI] [PubMed] [Google Scholar]
- 24. Seropian M, Dillman D, Lasater K, Gavilanes J. Mannequin‐based simulation to reinforce pharmacology concepts. Simul Healthc. 2007;2:218‐223. [DOI] [PubMed] [Google Scholar]
- 25. Via DK, Kyle RR, Trask JD, Shields CH, Mongan PD. Using high‐fidelity patient simulation and an advanced distance education network to teach pharmacology to second‐year medical students. J Clin Anesth. 2004;16:144‐151. [DOI] [PubMed] [Google Scholar]
- 26. Halm BM, Lee MT, Franke AA. Improving toxicology knowledge in preclinical medical students using high‐fidelity patient simulators. Hawaii Med J. 2011;70:112‐115. [PMC free article] [PubMed] [Google Scholar]
- 27. Maddry JK, Varney SM, Sessions D, et al. A comparison of simulation‐based education versus lecture‐based instruction for toxicology training in emergency medicine residents. J Med Toxicol. 2014;10:364‐368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nimbalkar A, Patel D, Kungwani A, Phatak A, Vasa R, Nimbalkar S. Randomized control trial of high fidelity vs low fidelity simulation for training undergraduate students in neonatal resuscitation. BMC Res Notes. 2015;8:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aqel AA, Ahmad MM. High‐fidelity simulation effects on CPR knowledge, skills, acquisition, and retention in nursing students. Worldviews Evid Based Nurs. 2014;11:394‐400. [DOI] [PubMed] [Google Scholar]
- 30. Varley M, Choi R, Kuan K, et al. Prospective randomized assessment of acquisition and retention of SILS skills after simulation training. Surg Endosc. 2015;29:113‐118. [DOI] [PubMed] [Google Scholar]
- 31. Mieure KD, Vincent WR 3rd, Cox MR, Jones MD. A high‐fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Robinson JD, Bray BS, Willson MN, Weeks DL. Using human patient simulation to prepare student pharmacists to manage medical emergencies in an ambulatory setting. Am J Pharm Educ. 2011;75:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient‐simulation mannequins to teach performance‐based pharmacotherapeutics. Am J Pharm Educ. 2006;70:48. [DOI] [PMC free article] [PubMed] [Google Scholar]


