Abstract
Oxidative damage is the causal link to a multitude of pathologies, such as diabetes, arthritis, neuropathy, heart disease, and asthma. These conditions affect hundreds of millions of people nationwide, and billions worldwide. Even in otherwise healthy individuals, oxidative stress is a natural byproduct of metabolism that is augmented in “healthy” activities such as athletics. In many disease states, the pharmacological agents used to treat these conditions can induce oxidative damage and vitamin depletion. It is underappreciated by many that many of the most common medications prescribed result in oxidative stress. Therefore, physicians need to carefully scrutinize which medications their patients are on before surgery and treatment and during the recovery stage to obtain optimal healing results. We provide a review of the current literature of how oxidative damage and inflammation are linked to bone damage, Charcot neuroarthropathy, delayed wound healing, diabetic complications, and delayed flap consolidation. Where available, antioxidant intervention literature is offered to offset these conditions.
1. Background
1.1. General Oxidative Stress
Reactive oxygen species (ROS) consist of radical and nonradical chemical forms. Oxidative stress (OS) is present when ROS cannot be adequately balanced by the level of antioxidants. This imbalance can occur due to many factors including aging and hormonal changes, radiation exposure, certain drug therapies, certain diseases, and physiological events and an increase of metabolic activity/physical exercise [1–3]. ROS are also produced during normal cellular metabolism following the activation of various enzymes such as NADPH oxidase, mitochondrial oxidases, and superoxide dismutase [4, 5]. ROS levels are also pivotal to induce cell signaling which has a role in cell proliferation, differentiation, apoptosis, and inflammation [2, 6].
Three lines of defense are needed to protect cells from the damaging effects of OS: low molecular weight ROS scavengers, antioxidative enzymes, and proteases for proteolytic degradation of irreversibly damaged proteins. Some of these low molecular weight antioxidants are various vitamins and minerals, co-enzyme Q10 (CoQ10), thiol compounds such as glutathione (GSH), alpha-lipoic acid, N-acetyl cysteine, and polyphenols. The ratio of the reduced form of glutathione (GSH) to the oxidized form of glutathione (GSSG) is an important measure of oxidative stress [7, 8]. Further, GSH has the ability to positively influence the activity of certain transcription factors [1, 9, 10] while other reduced thiol forms can act as antioxidant [11] scavengers and regenerate other antioxidants [12, 13]. OS can also damage cell membranes and proteins which can decrease organ function and result in systemic events [13], resulting in nonunion bone fractures, delayed union bone fractures, poor skin viability, poor flap viability, and poor arterial viability. Therefore, understanding how the adverse effects of OS could be abolished by altering the nutritional status of patients is paramount.
A side effect of drug therapy, prescription and over the counter, is depletion of vitamins, minerals, and antioxidants [14]. Many of these depletions affect antioxidants directly, but all may influence overall physiology stressing antioxidant defenses. For instance, corticosteroids function to depress the immune response; however, it leads to increased OS [15]. This may be a function of depletion of melatonin, leading to sleep disruption, and depletion of selenium, which directly relates to glutathione peroxidase activity.
Table 1 indicates the extent of micronutrient depletion that often accompanies both prescription and OTC medication ([16, 17] and references in each). The effect of this depletion has many far-reaching effects, of particular interest to this study, delayed wound healing [18]. An often overlooked weapon in recovery from bone, wound, and surgical tissue damage is repletion of these micronutrients. Few products replete multiple depletions. One notable exception would be Red Ox+.
Table 1.
Effects of prescription and over-the-counter medications on micronutrient levels in patients, including vitamins, minerals, and antioxidants ([16, 17] and references in each).
| Drug class | Nutrients depleted |
|---|---|
| Prescription medications | |
| Antibiotics (fluoroquinolones): Levaquin, Avelox, Cipro, Floxin, Noroxin, Penetrex, Trovan | Biotin, B1, B2, B3, B6, B12, zinc, and healthy intestinal bacteria |
| Antibiotics (macrolides): erythromycin, azithromycin, Biaxin, Zithromax | Healthy intestinal bacteria, B1, B2, B3, B6, and B12 |
| Antibiotics (penicillins): amoxicillin, Amoxil, Trimox, penicillin | Healthy intestinal bacteria, B1, B2, B3, B6, B12, vitamin k, folic acid, biotin, and inositol |
| ACE inhibitors: lisinopril, Altace, Accupril, Capoten, Prinivil, Zestril, Vasotec | Zinc |
| Beta-2 adrenergic receptor agonists: albuterol aerosol, Brethine, Proventil, Tornalate, Ventolin, Xopenex | Potassium and possibly calcium-magnesium and phosphorus |
| Beta-blockers: atenolol, Corgard, Lopressor, Tenormin, Toprol XL, metoprolol | Coenzyme Q10, chromium, and melatonin |
| Biguanides: metformin, Glucophage | Folic acid, B12 |
| Bisphosphonates: Fosamax, Actonel, Boniva, Didronel, Skelid | Calcium-magnesium and phosphorus |
| Calcium channel blockers: amlodipine, felodipine, nifedipine, nimodipine, nisoldipine | Vitamin D |
| Cardiac glycosides: digoxin, Digitek, Lanoxin, Lanoxicaps | Calcium-magnesium, phosphorus, potassium, and B1 |
| Conjugated estrogens: Premarin hormone replacement therapy, birth control pills | B6, vitamin D, calcium-magnesium, zinc, folic acid, and B12 |
| Corticosteroids: Flonase, Beclovent, Beconase, QVar, Vancenase, Vanceril, prednisone, Deltasone, Celestone, Cortisone, Cortef, Cortone, dexamethasone, Decadron, Hydrocortone, Medrol, methylprednisolone | Beta-carotene, B6, folic acid, vitamin C, vitamin D, calcium-magnesium, potassium, selenium, zinc, and melatonin |
| Loop diuretics: furosemide, Lasix, ethacrynic acid, Edecrin, Bumex | B1, B6, vitamin C, calcium-magnesium, phosphorus, potassium, and zinc |
| Opiates: hydrocodone/acetaminophen, oxycodone | Folic acid, vitamin C, iron, and potassium |
| Potassium sparing diuretics: amiloride, spironolactone, triamterene, aldactone, dyazide, Dyrenium, Maxzide | Calcium, magnesium, and phosphorus |
| Proton pump inhibitors: omeprazole, Prilosec, Prevacid, Nexium, Protonix, Aciphex | Beta-carotene, B1, B12, folic acid, calcium, and zinc |
| Statins: Lipitor, Crestor, Lescol, Pravachol, Zocor, Mevacor | Coenzyme Q10 |
| Sulfonylurea: glyburide, glipizide, glimepiride, Amaryl, Diabeta, Glucotrol, Glynase, Micronase | Coenzyme Q10 |
| Thiazide diuretics: hydrochlorothiazide | Vitamin D, calcium-magnesium, phosphorus, potassium, zinc, and coenzyme Q10 |
| Tricyclic antidepressants: Amitriptyline, clomipramine, doxepin, imipramine, Anafranil, Asendin, Elavil, Tofranil, Vivactil | Coenzyme Q10, B2, and sodium |
|
| |
| Over-the-counter medications | |
| Acetaminophen: Tylenol | Coenzyme Q10 and glutathione |
| Antacids: Amphojel, Basaljel, aluminum hydroxide plus magnesium, Gaviscon, Gelusil, Maalox, Mylanta | Beta-carotene, folic acid, vitamin D, calcium-magnesium, chromium, iron, zinc, and phosphorus |
| Aspirin | Folic acid, vitamin C, iron, potassium, and zinc |
| Laxatives with bisacodyl: Carter's little pills, Correctol, Dulcolax, Feen-A-Mint, PMS-Bisacodyl | Calcium and potassium |
| NSAIDs: ibuprofen, naproxen | Folic acid |
| OTC proton-pump inhibitors: famotidine, pepcid, Tagamet, Zantac | Folic acid, B1, B12, vitamin D, calcium, iron, and zinc |
Herein, we provide a review of the role of oxidative damage in bone remodeling and wound healing, and micronutrient (especially antioxidant) adjunctive therapy and how this may positively affect limb lengthening and microsurgical reconstruction.
1.2. Bone Remodeling
Current research demonstrates that oxidative stress can negatively impact bone remodeling [19–22]. Bone remodeling is a complex cycle, which lasts approximately 6 months, and harbors three main cells (osteoclasts, osteoblasts, and osteocytes), which under normal circumstances will be harmoniously regulated with the aid of cytokines, growth factors, and hormones. Oxidative stress activates the differentiation of pre-osteoclasts to adult osteoclasts while inducing apoptosis of osteoblasts and osteocytes and augmenting bone resorption [3, 21].
Oxidative stress has also been shown to upregulate RANKL and downregulate osteoprotegerin. Osteoprotegerin is a decoy receptor for the RANK by competing with RANKL. Osteoprotegerin is directly correlated with estrogen levels [23]. When estrogen levels are low, osteoprotegerin is also low which leads to increased bone resorption. RANKL binds to RANK, which triggers differentiation and activation of osteoclasts. This system is balanced by the relative expression of osteoprotegerin to RANKL, which are highly regulated by many factors including hormones, immune signals, and growth factors. An overexpression of RANKL can cause an overproduction and activation of osteoclasts as shown in primary cell culture from human samples as well as immortal cell line models [9, 13, 24].
Recent literature has displayed that osteocytes constitute 90% of the bone cell population and are essential for bone remodeling. Oxidative stress causes osteocyte apoptosis. These apoptotic osteocytes release sclerostin. Sclerostin is a protein that blocks bone formation by osteoblasts by binding to the Wnt co-receptors and low-density lipoprotein receptors (LRP) 4, 5, and 6 [25, 26]. This decreases the Wnt signaling pathway which, when active, stimulates osteoprotegerin [27–30]. Thus, the outcome of sclerostin upregulation of bone resorption is due, at least in part, by inhibiting the Wnt signaling pathway. Nitrogen bisphosphonates are widely used to control osteoporosis. However, they may contribute to increased OS, particularly when coupled with comorbidities such as diabetes mellitus (DM) and cancer [31]. Thus, the beneficial use of nitrogen bisphosphonates on bone density may also lead to potential negative side effects during high dose or long-term use in cases such as cancer treatment. In these cases, outcomes such as osteonecrosis and atypical long bone fractures have been observed [32]. This may be linked to the OS caused by the nitrogen bisphosphonates and/or their depletion of CoQ10. For instance, it has been found that nitrogen bisphosphonates, as well as statins, inhibit cellular synthesis of the antioxidant CoQ10 [33–35]. Nitrogen bisphosphonate use has also been shown to decrease serum antioxidant vitamin E and CoQ10 levels in postmenopausal women [35]. CoQ10 has been found to reverse spinal cord injury osteoporosis in rats by restoring bone mineral density and bone mineral content while increasing SOD [36]. CoQ10 was also shown to upregulate osteoblast-specific gene core-binding factor alpha 1 [36] and reduce osteoclastogenesis mediated through RANKL while also reducing inflammation in rheumatoid arthritic mice and augmenting the number of T-regulatory cells which directly decreases the number of T-helper 17 cells which are inflammatory [37]. T-regulatory cells are immunosuppressive and help maintain tolerance to self-antigens by preventing autoimmune diseases. Antioxidants, particularly CoQ10, would seem to be a protective adjunct therapy for each of the conditions outlined above.
1.3. Wound Healing
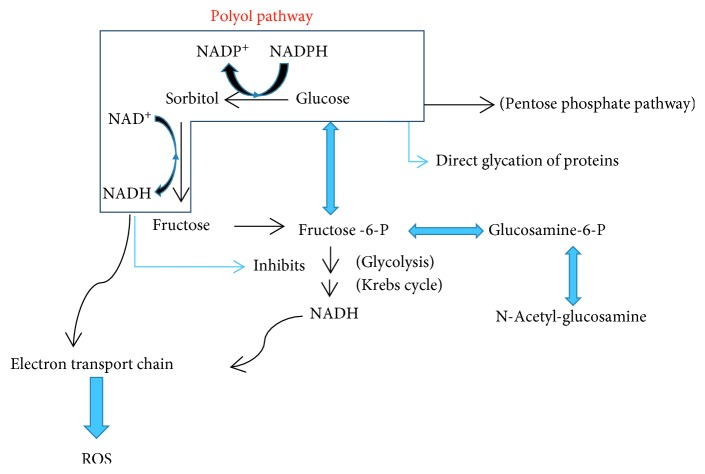
Under normal circumstances, cells utilize glucose for energy via glycolysis which commences using the enzyme hexokinase. However, it has been long known that glucose challenge induces ROS production [38]. There are other fates of glucose such as the pentose phosphate pathway which is generally employed to generate NADPH reducing power and is able to create ribose-5-phosphate for nucleic acid synthesis (Figure 1).
Figure 1.
Metabolic fates of glucose relevant to the current focus.
Glucose may also react with aldose reductase in what is known as the polyol pathway to form sorbitol using NADPH as a reductant. Subsequently, the sorbitol is oxidized to fructose by catalysis with sorbitol dehydrogenase and production of NADH. This, in turn, slows glycolysis by inhibiting glyceraldehyde-3-dehydrogenase which prolongs the diversion of glucose away from glycolysis toward the polyol pathway [39]. Furthermore, the high NADH levels induce NADH oxidase activity which may form superoxide radicals as a byproduct [40]. When blood glucose is normal (about 100 mg/dl), aldose reductase has a low affinity for glucose which limits the polyol pathway utilization. However, in diabetics, particularly in chronically poorly controlled glucose patients, glucose levels saturate hexokinase (the first step in glycolysis) and the polyol pathway is engaged. In these chronic hyperglycemic conditions where the polyol pathway is active (Figure 1), there is a decrease in reduced NADPH which leads to decreased synthesis of reduced glutathione, nitric oxide, myo-inositol, and taurine, all of which are important for proper nerve function. Exacerbating this consumption of NADPH in diabetics is lower glucose-6-phosphate dehydrogenase (rate-limiting step in pentose phosphate pathway) activity which prevents NADPH from being produced as demonstrated in a rat model [41].
Reduced glutathione maintains glutathione peroxidase, vitamin C and E in their reduced forms, as well as facilitates proper DNA and protein synthesis [42] and has a vital function in iron metabolism. The decreased NADPH levels due to the polyol pathway compromise these vital reductive functions. Glutathione peroxidase is essential to limiting ROS. The increased sorbitol will augment the production of advanced glycation endproducts (AGEs), reducing kidney function and inducing an inflammatory response while increasing the hemoglobin A1C (HbA1c). This increase in ROS leads to leukocyte adhesion and immigration of inflammatory mediators into the wound bed [43], inhibits re-epithelialization [44], and favors a rich biofilm which may harbor anaerobic bacteria not found in culture [45, 46]. Matrix metalloproteinases (MMPs) are capable of degrading extracellular matrix proteins, releasing apoptotic ligands and are increased in chronic wounds. They are regulated by tissue inhibitors of metalloproteinases. Gencer et al. showed that the expression of MMPs was increased in cells exposed to H2O2, and that removal of the oxidative stress decreased the expression of the MMPs [47]. Oxidized low-density lipoproteins were also shown to activate MMPs [48]. This appears to offer an intuitive intervention wherein topical antioxidants in conjunction with dietary or otherwise internal antioxidants could limit the amount of tissue damage from damage including surgical.
In a study by Dhall et al., they used the db/db diabetic mouse model of impaired healing and demonstrated that the diabetic mice were subject to chronic wounds with an abundance of free radicals. They then showed that they could reverse this chronicity with the antioxidants vitamin E and N-acetylcysteine by decreasing wound healing time, decreasing biofilm concentration, and increasing sensitivity to antibiotics while granulation tissue was formed with proper collagen deposition and remodeling [49]. In fact, diabetic mice, with OS, took over 100 days for their wounds to heal while wild-type mice without OS took on average 15 days for their wounds to heal [49]. When antioxidants were administered, the diabetic mice with OS took only 53 days on average for their wounds to heal [49]. Christman et al. showed that, for each 1.0% point increase in HbA1c, above 7.0%, the wound-area healing rate decreased by 0.028 cm2/day in humans with diabetes [50], and with the addition of antioxidants, the HbA1c was able to decrease [51]. The Akt pathway is a signal transduction pathway that promotes cell survival including cell proliferation, cell migration, and angiogenesis. In diabetics with elevated glucose and OS, Akt phosphorylation and gingival wound healing was shown to be impaired. When supplemented with N-acetyl-L-cysteine, Akt phosphorylation and gingival wound healing improved as did fibroblast proliferation and migration [52]. Toshiki et al. demonstrated in a rat model that they could significantly increase soft tissue wound healing in the mouth with application of CoQ10. They found that CoQ10 increased the expression of TIMP-1 and FGF while decreasing the expression of MMP-3 [53].
Prolonged OS can also produce psychological maladies including noncompliance and general compromised emotional status [54]. Oxidative damage may also be at the root of some of other psychological maladies such as autism [55]. Patient noncompliance such as not showing up for appointments, inconsistency in taking the medication, or not understanding the severity of their conditions may be due to these psychological OS-driven deficits.
1.4. Charcot Neuroarthropathy
Charcot neuroarthropathy (CNA) is caused by an interaction between diabetes, neuropathy, and an inflammatory response [56] which results in bone lysis, mircobone damage, and bone deformity. The “French Theory” (neurovascular theory) suggests that CNA results from a damaged central nervous system which leads to uncontrolled blood flow and prolonged inflammation while the “Germanic Theory” suggests CNA results from trauma secondary to neuropathy which leads to inflammation.
In either case, OS causes the progression of inflammation eventually leading to bone lysis, microfracture, and bone deformity. AGEs are known to be augmented in CNA patients [57]. AGEs are produced during OS [58] and cause apoptosis of osteoblasts [59]. Receptor for advanced glycation endproducts (RAGE) is a transmembrane receptor that binds to AGEs and has been linked to number of neurodegenerative diseases such amyotrophic lateral sclerosis; Alzheimer's, Parkinson's, Huntington's, and Creutzfeldt-Jakob diseases; depression; and CNA [60, 61]. RAGE is known to increase the activity of RANKL leading to osteoclastogenesis in bone [62] and has been associated with atherosclerotic lesions and vascular calcification by increasing the expression of bone morphogenetic protein 4 in arteries [63, 64] and is thought to cause a phenotypic switch of VSMCs to an osteoblast-like phenotype [65]. This pathway is upregulated in CNA [66].
Vascular calcification (VC) is linked to CNA and is associated with OS [67]. VC is four times more likely to be present in diabetic patients then healthy subjects [68], and VC is a significant predictor of stroke, amputation, and myocardial infarction [69]. OS potentiates inflammation by augmenting tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), and C-reactive protein [70]. CNA patients usually present with augmented serum inflammatory markers with a red hot swollen limb [71]. TNF-α, IL-6, and C-reactive protein have all been linked to VC [70] and nerve damage [72], indicting that VC and neuropathy are associated with inflammation. Diabetes is associated with an increase rate of lipoperoxidation [73], while VC is associated with an increased number of oxidized LDLs [74]. Excess mitochondrial ROS are also known to cause VC [29] and are the main cause of nerve damage in diabetics with good glucose control [75].
Brodeur et al. demonstrated that they could decrease calcification in the femoral artery of diabetic rats with the antioxidants: 4-hydroxy-tempol, alpha-lipoic acid, and apocynin. However, only apocynin significantly reduced femoral artery calcification [76]. Kim et al. found that alpha-lipoic acid significantly decreased aortic calcification in mice by inhibiting VSMC apoptosis by preserving mitochondrial function [77].
Related to the DM-induced CNA describe above, vitamin D has been shown by a number of methods to protect pancreatic beta cells from oxidative stress by inducing endogenous antioxidant pathways [78]. Therefore, drug-induced depletion of vitamin D would likely compromise pancreatic stress response.
1.5. Flap Consolidation
Numerous studies have shown that oxidative stress can cause inflammatory changes causing decreased blood supply resulting in flap necrosis [79–81]. The increase in OS can cause ischemia reperfusion injury. Necrosis to the distal region of random flaps is a major problem. Ischemia reperfusion injury occurs when the reperfusion creates and harbors oxygen-derived free radicals which are deleterious to the tissues [82]. This is due to increased Fenton chemistry that accompanies reoxidation of iron [83]. Flaps in diabetics present their own risk as OS, an important factor in diabetes mellitus (DM) complications, is already significantly elevated in this population [58] and diminishes the microvascular supply resulting in necrosis [84]. DM also increases AGEs which damage tissue structure which decreases perfusion [85, 86]. One important clinical feature of decreased perfusion, common in diabetics, would be erectile dysfunction (ED) [87, 88]. Antioxidant therapy shows great promise in reversing or preventing ED concurrent with improved blood flow [89, 90].
Calcitriol, a metabolite of vitamin D, is an antioxidant known that has many anti-inflammatory properties. In a random skin flap model, using rats, calcitriol was shown to increase SOD, thereby decreasing OS. This decrease in OS was shown to reduce inflammation and upregulate vascular endothelial growth factor in the flaps which significantly increased flap survival by decreasing edema and increasing angiogenesis [91]. Ufuk et al. showed that random flaps in DM mice exhibited greater OS and necrosis compared to controls while supplementing with long-term antioxidant vitamin E reduced OS and necrosis while increasing hyalinization of arterioles in the flaps [92]. In another study, aminoguanidine, an antioxidant which is known to halt AGEs, was given to DM rats before skin flaps were elevated. Aminoguanidine administration significantly increased flap viability in the diabetic rats by decreasing necrosis [93]. The antioxidants from grape seed extract (proanthocyanidin) and tomato extract (lycopene) were also shown to significantly decrease flap necrosis and inflammation when given two weeks before surgery and two weeks prior surgery [94] in rats. Naringin, the antioxidant found in citrus fruits, was found to significantly increase flap survival by increasing VEGF and SOD while decreasing TNF-α and IL-6 [95]. CoQ10 was also shown to significantly increase flap viability in rats while the highest serum level of CoQ10 was obtained with oral administration [96].
2. Discussion
Although antioxidants may not cure the root causes of the conditions explored above, many studies have shown that mitigation of the inflammatory products may allow for host recovery and more limited damage [13, 18, 36, 37, 42, 49, 51, 78, 81, 84, 86, 89, 90, 92–94, 96]. Furthermore, starting patients on antioxidants prophylactically could prevent damage from starting. One example would be the vitamin D protection of pancreatic beta cells referred to above [78]. Others would be CoQ10 upregulating osteoblast activity in bone remodeling [36, 37] or antioxidants improving mental disturbances such as autistic behavior, also referred to above [55].
The seven well-known signs of oxidative stress are increased fatigue, memory loss and/or brain fog, muscle and/or joint pain, wrinkles and grey hair, decreased eye sight, headaches and sensitivity to noise, and susceptibility to infections. However, we noted that there are many more signs and symptoms which start at the cellular level and are less obvious for a physician to diagnose such as increased inflammatory mediators resulting in Charcot neuroarthropathy, delayed wound healing, failed surgical outcomes, erectile dysfunction, and poor bone stock.
Physicians should start to examine the GSH/GSSG levels as this will give you a definitive way to quantify oxidative stress. Choosing organic foods and avoiding nicotine and toxic chemicals may prevent some exogenous radicals from entering our body. However, as we age, it is inevitable that the constant bombardment of these radicals, from even natural internal metabolic pathways, will cause a cumulative damage [1, 4, 83]. Many conditions are also fueled by OS, such as rheumatoid arthritis, osteoporosis, and heart disease. We have also referenced evidence that diabetics are subject to OS when increased levels of glucose will enter the polyol pathway [41, 42]. However, we have yet to scrutinize why some individuals with well-controlled blood glucose levels and HbA1c's in the proper range develop neuropathy, Charcot neuroarthropathy, and chronic wounds while some uncontrolled diabetics never have complications. Perhaps, these patients already consume a diet low in oxidative additives, have fortunate genetics, or have some other unknown mechanism that reduces these radicals.
Even the healthiest athlete is subject to OS as exercise will augment the rate of metabolism as food is processed to provide energy at the cellular level. An inevitable side effect of metabolism is the production of ROS and “free radicals” that can damage DNA and other cellular constituents. This damage can lead to cancer, advanced aging, and as we have displayed and increased susceptibility of delayed wound healing and bone remodeling (stress fractures). Osteoporosis is seen daily, whether it is in the elderly, diabetic, postmenopausal female or a consequence of the female athlete triad; these patients are under extreme OS. Bisphosphonates (Table 1) are usually given to counter osteoporosis but could be causing more harm by depleting calcium-magnesium, phosphorus, and Coq10 [14, 16, 17]. Further, starting these patients on steroids or NSAIDs might decrease the discomfort but will cause OS and could potentially make the condition worse. The classic diabetic patient is on a biguanide and or sulfonylurea which both inhibit CoQ10 (Table 1) and have shown to cause neuropathy. Although the diabetes was the initial cause of the neuropathy, it may well be that the prolonged treatment causes enhanced OS leading to further neuropathy. Furthermore, the diabetic patient with many comorbidities is usually taking a statin, ACE inhibitor, beta-blocker, and perhaps an antibiotic for their chronic wound. All these drugs deplete important nutrients (Table 1), potentiating the OS already present from the disease.
Hemodialysis is another process often associated with chronic diabetes patients that leads to loss of nutrients. Chronic kidney disease, as mentioned above, can be a result of the AGEs reducing kidney function. These hemodialysis patients are already at a disadvantage with the retention of toxins and rapid depletion of antioxidants during hemodialysis. According to Liakopoulos et al., the process of iron infusion, length of hemodialysis therapy, anemia, and the central venous catheter all augment OS [97]. Physicians commonly prescribe CoQ10 therapy for a common statin side effect but ignore other depletions such as vitamins B1, B6, B12, C, calcium, magnesium, phosphorus, potassium, zinc, beta-carotene, and folic acid (Table 1). Clearly, with common situations such as this, single vitamin or electrolyte therapies would be insufficient. One would require a more robust formula of all the potential vitamins, electrolytes, and antioxidants to replete the patient such as Red Ox+. There are many more drugs that deplete important nutrients that induce OS. Clinicians need to examine the drugs their patients are on and supplement accordingly. This is especially important for the preoperative and postoperative patient as we have shown through many studies that ameliorating OS will aid in bone remodeling, wound and soft tissue healing, and arterial and muscle and soft tissue flap consolidation. The combination of vitamins, minerals, and antioxidants is an essential weapon clinicians should have in their arsenal that needs to be used on a regular basis.
3. Conclusion
Oxidative stress is at the heart of a myriad of maladies. Antioxidants are depleted by many of the medications that were intended to solve these health issues. Robust antioxidants at therapeutic levels would be an excellent way to reverse these ill effects, whether caused by medication-related depletion or directly from the disease state. Doctors should note patient medication profiles and add appropriate supplements accordingly.
More clinical outcomes of antioxidant and vitamin therapy to offset the depletion caused by pharmaceutical intervention should be examined, particularly with respect to markers such as oxidative stress levels, bone density, surgical and wound healing rates, and complete blood cell counts, as well as neuropathy.
Acknowledgments
This work was supported by the University Hospitals and John Carroll University.
Conflicts of Interest
BMS and DPM own a stake in Wire-2-WireLLC, makers of Red Ox+.
References
- 1.Valko M., Leibfritz D., Moncol J., Cronin M. T. D., Mazur M., Telser J. Free radicals and antioxidants in normal physiological functions and human disease. International Journal of Biochemistry & Cell Biology. 2007;39(1):44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Ray P. D., Huang B.-W., Tsuji Y. Reactive oxygen species (ROS) homeostasis and redox regulation in cellular signaling. Cellular Signalling. 2012;24(5):981–990. doi: 10.1016/j.cellsig.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tilg H., Moschen A. R., Kaser A., Pines A., Dotan I. Gut, inflammation and osteoporosis: basic and clinical concepts. Gut. 2008;57(5):684–694. doi: 10.1136/gut.2006.117382. [DOI] [PubMed] [Google Scholar]
- 4.Circu M. L., Aw T. Y. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radical Biology and Medicine. 2010;48(6):749–762. doi: 10.1016/j.freeradbiomed.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aw N. S. R., Seronello S., Wang S. H., et al. Hepatocyte NAD(P)H oxidases as an endogenous source of reactive oxygen species during hepatitis C virus infection. Hepatology. 2010;52(1):47–59. doi: 10.1002/hep.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catarzi S., Romagnoli C., Marcucci G., Favilli F., Iantomasi T., Vincenzini M. T. Redox regulation of ERK1/2 activation induced by sphingosine 1-phosphate in fibroblasts: involvement of NADPH oxidase and platelet-derived growth factor receptor. Biochimica et Biophysica Acta (BBA)-General Subjects. 2011;1810(4):446–456. doi: 10.1016/j.bbagen.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Romagnoli C., Marcucci G., Favilli F, et al. Role of GSH/GSSG redox couple in osteogenic activity and osteoclastogenic markers of human osteoblast-like SaOS-2 cells. FEBS Journal. 2013;280:867–879. doi: 10.1111/febs.12075. [DOI] [PubMed] [Google Scholar]
- 8.Jones D. P. [11] redox potential of GSH/GSSG couple: assay and biological significance. Protein Sensors and Reactive Oxygen Species-Part B: Thiol Enzymes and Proteins. 2002;348:93–112. doi: 10.1016/s0076-6879(02)48630-2. [DOI] [PubMed] [Google Scholar]
- 9.Romagnoli C., Marcucci T., Picariello L., Tonelli F., Vincenzini M. T., Iantomasi T. Role of N-acetylcysteine and GSH redox system on total and active MMP-2 in intestinal myofibroblasts of Crohn’s disease patients. International Journal of Colorectal Disease. 2012;28(7):915–924. doi: 10.1007/s00384-012-1632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iantomasi T., Favilli F., Catarzi S., Vincenzini M. T. GSH role on platelet-derived growth factor receptor tyrosine phosphorylation induced by H2O2. Biochemical and Biophysical Research Communications. 2001;280(5):1279–1285. doi: 10.1006/bbrc.2001.4274. [DOI] [PubMed] [Google Scholar]
- 11.Blanco R. A., Ziegler T. R., Carlson B. A., et al. Diurnal variation in glutathione and cysteine redox states in human plasma. American Journal of Clinical Nutrition. 2007;86(4):1016–1023. doi: 10.1093/ajcn/86.4.1016. [DOI] [PubMed] [Google Scholar]
- 12.Franco R., Schoneveld O. J., Pappa A., Panayiotidis M. I. The central role of glutathione in the pathophysiology of human diseases. Archives of Physiology and Biochemistry. 2008;113(4-5):234–258. doi: 10.1080/13813450701661198. [DOI] [PubMed] [Google Scholar]
- 13.Fontani F., Marcucci G., Iantomasi T., Brandi M. L., Vincenzini M. T. Glutathione, N-acetylcysteine and lipoic acid down-regulate starvation-induced apoptosis, RANKL/OPG ratio and sclerostin in osteocytes: involvement of JNK and ERK1/2 signalling. Calcified Tissue International. 2015;96(4):335–346. doi: 10.1007/s00223-015-9961-0. [DOI] [PubMed] [Google Scholar]
- 14.Pelton R. Drug-Induced Nutrient Depletion Handbook. 2nd. Hudson, OH, USA: Lexi-Comp’s Clinical Reference Library, Lexi-Comp; 2001. [Google Scholar]
- 15.Feng Y.-L., Tang X.-L. Effect of glucocorticoid-induced oxidative stress on the expression of Cbfa1. Chemico-Biological Interactions. 2014;207:26–31. doi: 10.1016/j.cbi.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Mohn E., Kern H., Saltzman E., Mitmesser S., McKay D. Evidence of drug-nutrient interactions with chronic use of commonly prescribed medications: an update. Pharmaceutics. 2018;10(1):36–81. doi: 10.3390/pharmaceutics10010036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samaras D., Samaras N., Lang P.-O., Genton L., Frangos E., Pichard C. Effects of widely used drugs on micronutrients: a story rarely told. Nutrition. 2013;29(4):605–610. doi: 10.1016/j.nut.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Russell L. The importance of patients’ nutritional status in wound healing. British Journal of Nursing. 2001;10(6):S42–S49. doi: 10.12968/bjon.2001.10.sup1.5336. [DOI] [PubMed] [Google Scholar]
- 19.Baek K. H., Oh K. W., Lee W. Y., et al. Association of oxidative stress with postmenopausal osteoporosis and the effects of hydrogen peroxide on osteoclast formation in human bone marrow cell cultures. Calcified Tissue International. 2010;87(3):226–235. doi: 10.1007/s00223-010-9393-9. [DOI] [PubMed] [Google Scholar]
- 20.Yousefzadeh G., Larijani B., Mohammadirad A., et al. Determination of oxidative stress status and concentration of TGF-β1 in the blood and saliva of osteoporotic subjects. Annals of the New York Academy of Sciences. 2006;1091(1):142–150. doi: 10.1196/annals.1378.062. [DOI] [PubMed] [Google Scholar]
- 21.Lean J. M., Jagger C. J., Kirstein B., Fuller K., Chambers T. J. Hydrogen peroxide is essential for estrogen-deficiency bone loss and osteoclast formation. Endocrinology. 2005;146(2):728–735. doi: 10.1210/en.2004-1021. [DOI] [PubMed] [Google Scholar]
- 22.Almeida M., Han L., Martin-Millan M., et al. Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. Journal of Biological Chemistry. 2007;282(37):27285–27297. doi: 10.1074/jbc.m702810200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krakauer T. Nuclear factor-κb: fine-tuning a central integrator of diverse biologic stimuli. International Reviews of Immunology. 2009;27(5):286–292. doi: 10.1080/08830180802317957. [DOI] [PubMed] [Google Scholar]
- 24.Filaire E., Toumi H. Reactive oxygen species and exercise on bone metabolism: friend or enemy? Joint Bone Spine. 2012;79(4):341–346. doi: 10.1016/j.jbspin.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Wijenayaka A. R., Kogawa M., Lim H. P., Bonewald L. F., Findlay D. M., Atkins G. J. Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS One. 2011;6(10) doi: 10.1371/journal.pone.0025900.e25900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim J. H., Liu X., Wang J., et al. Wnt signaling in bone formation and its therapeutic potential for bone diseases. Therapeutic Advances in Musculoskeletal Disease. 2013;5(1):13–31. doi: 10.1177/1759720x12466608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henriksen K., Neutzsky-Wulff A. V., Bonewald L. F., Karsdal M. A. Local communication on and within bone controls bone remodeling. Bone. 2009;44(6):1026–1033. doi: 10.1016/j.bone.2009.03.671. [DOI] [PubMed] [Google Scholar]
- 28.Bonewald L. F. The amazing osteocyte. Journal of Bone and Mineral Research. 2011;26(2):229–238. doi: 10.1002/jbmr.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wauquier F., Leotoing L., Coxam V., Guicheux J., Wittrant Y. Oxidative stress in bone remodelling and disease. Trends in Molecular Medicine. 2009;15(10):468–477. doi: 10.1016/j.molmed.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Jilka R. L., Noble B., Weinstein R. S. Osteocyte apoptosis. Bone. 2013;54(2):264–271. doi: 10.1016/j.bone.2012.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khamaisi M., Regev E., Yarom N., et al. Possible association between diabetes and bisphosphonate-related jaw osteonecrosis. Journal of Clinical Endocrinology & Metabolism. 2007;92(3):1172–1175. doi: 10.1210/jc.2006-2036. [DOI] [PubMed] [Google Scholar]
- 32.Khosla S., Burr D., Cauley J., et al. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American society for bone and mineral research. Journal of Bone and Mineral Research. 2007;22(10):1479–1491. doi: 10.1359/jbmr.0707onj. [DOI] [PubMed] [Google Scholar]
- 33.Dallner G., Sindelar P. J. Regulation of ubiquinone metabolism. Free Radical Biology and Medicine. 2000;29(3‐4):285–294. doi: 10.1016/s0891-5849(00)00307-5. [DOI] [PubMed] [Google Scholar]
- 34.Brault M., Ray J., Gomez Y.-H., Mantzoros C. S., Daskalopoulou S. S. Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metabolism. 2014;63(6):735–745. doi: 10.1016/j.metabol.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 35.Kalyan S., Huebbe P., Esatbeyoglu T., et al. Nitrogen-bisphosphonate therapy is linked to compromised coenzyme Q10 and vitamin E status in postmenopausal women. Journal of Clinical Endocrinology & Metabolism. 2014;99(4):1307–1313. doi: 10.1210/jc.2013-3648. [DOI] [PubMed] [Google Scholar]
- 36.Zhang X.-X., Qian K.-J., Zhang Y., et al. Efficacy of coenzyme Q10 in mitigating spinal cord injury-induced osteoporosis. Molecular Medicine Reports. 2015;12(3):3909–3915. doi: 10.3892/mmr.2015.3856. [DOI] [PubMed] [Google Scholar]
- 37.Jhun J., Lee S. H., Byun J.-K., et al. Coenzyme Q10 suppresses Th17 cells and osteoclast differentiation and ameliorates experimental autoimmune arthritis mice. Immunology Letters. 2015;166(2):92–102. doi: 10.1016/j.imlet.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 38.Mohanty P., Hamouda W., Garg R., Aljada A., Ghanim H., Dandona P. Glucose challenge stimulates reactive oxygen species (ROS) generation by leucocytes. Journal of Clinical Endocrinology & Metabolism. 2000;85(8):2970–2973. doi: 10.1210/jc.85.8.2970. [DOI] [PubMed] [Google Scholar]
- 39.Tang W. H., Martin K. A., Hwa J. Aldose reductase, oxidative stress, and diabetes mellitus. Frontiers in Pharmacology. 2012;3 doi: 10.3389/fphar.2012.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paravicini T. M., Touyz R. M. NADPH oxidases, reactive oxygen species, and hypertension: clinical implications and therapeutic possibilities. Diabetes Care. 2008;31(2):S170–S180. doi: 10.2337/dc08-s247. [DOI] [PubMed] [Google Scholar]
- 41.Xu Y., Osborne B. W., Stanton R. C. Diabetes causes inhibition of glucose-6-phosphate dehydrogenase via activation of PKA, which contributes to oxidative stress in rat kidney cortex. American Journal of Physiology-Renal Physiology. 2005;289(5):F1040–F1047. doi: 10.1152/ajprenal.00076.2005. [DOI] [PubMed] [Google Scholar]
- 42.Sen C. K., Roy S. Redox signals in wound healing. Biochimica et Biophysica Acta (BBA)-General Subjects. 2008;1780(11):1348–1361. doi: 10.1016/j.bbagen.2008.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kishimoto T., Jutila M., Berg E., Butcher E. Neutrophil Mac-1 and MEL-14 adhesion proteins inversely regulated by chemotactic factors. Science. 1989;245(4923):1238–1241. doi: 10.1126/science.2551036. [DOI] [PubMed] [Google Scholar]
- 44.Ponugoti B., Xu F., Zhang C., Tian C., Pacios S., Graves D. T. FOXO1 promotes wound healing through the up-regulation of TGF-β1 and prevention of oxidative stress. Journal of Cell Biology. 2013;203(2):327–343. doi: 10.1083/jcb.201305074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.James G. A., Swogger E., Wolcott R., et al. Biofilms in chronic wounds. Wound Repair and Regeneration. 2007;16(1):37–44. doi: 10.1111/j.1524-475x.2007.00321.x. [DOI] [PubMed] [Google Scholar]
- 46.Bjarnsholt T., Kirketerp-Møller K., Jensen P. Ø., et al. Why chronic wounds will not heal: a novel hypothesis. Wound Repair and Regeneration. 2008;16(1):2–10. doi: 10.1111/j.1524-475x.2007.00283.x. [DOI] [PubMed] [Google Scholar]
- 47.Gencer S., Cebeci A., Irmak-Yazicioglu M. B. Matrix metalloproteinase gene expressions might be oxidative stress targets in gastric cancer cell lines. Journal of Cancer Research. 2013;25(3):322–333. doi: 10.3978/j.issn.1000-9604.2013.06.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valentin F., Bueb J.-L., Kieffer P., Tschirhart E., Atkinson J. Oxidative stress activates MMP-2 in cultured human coronary smooth muscle cells. Fundamental and Clinical Pharmacology. 2005;19(6):661–667. doi: 10.1111/j.1472-8206.2005.00371.x. [DOI] [PubMed] [Google Scholar]
- 49.Dhall S., Do D. C., Garcia M., et al. Generating and reversing chronic wounds in diabetic mice by manipulating wound redox parameters. Journal of Diabetes Research. 2014;2014:18. doi: 10.1155/2014/562625.562625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Christman A. L., Selvin E., Margolis D. J., Lazarus G. S., Garza L. A. Hemoglobin A1c predicts healing rate in diabetic wounds. Journal of Investigative Dermatology. 2011;131(10):2121–2127. doi: 10.1038/jid.2011.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Afkhami-Ardekani M. Effect of vitamin c on blood glucose, serum lipids & serum insulin in type 2 diabetic patients. Indian Journal of Medical Research. 2007;126(5):471–474. [PubMed] [Google Scholar]
- 52.Daisuke K., Mizutani K., Takeda K., et al. Impact of diabetes on gingival wound healing via oxidative stress. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0189601.e0189601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoneda T., Tomofuji T., Kawabata Y., et al. Application of coenzyme Q10 for accelerating soft tissue wound healing after tooth extraction in rats. Nutrients. 2014;6(12):5756–5769. doi: 10.3390/nu6125756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vileikyte L., Rubin R. R., Leventhal H. Psychological aspects of diabetic neuropathic foot complications: an overview. Diabetes/Metabolism Research and Reviews. 2004;20(S1):S13–S18. doi: 10.1002/dmrr.437. [DOI] [PubMed] [Google Scholar]
- 55.McGinnis W. R. Oxidative stress in autism. Alternative Therapies in Health and Medicine. 2004;10(6):22–36. [PubMed] [Google Scholar]
- 56.Jeffcoate W. The causes of the Charcot syndrome. Clinics in Podiatric Medicine and Surgery. 2008;25(1):29–42. doi: 10.1016/j.cpm.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 57.Katayama Y., Akatsu T., Yamamoto M., Kugai N., Nagata N. Role of nonenzymatic glycosylation of type I collagen in diabetic osteopenia. Journal of Bone and Mineral Research. 1996;11(7):931–937. doi: 10.1002/jbmr.5650110709. [DOI] [PubMed] [Google Scholar]
- 58.Baynes J. W. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991;40(4):405–412. doi: 10.2337/diabetes.40.4.405. [DOI] [PubMed] [Google Scholar]
- 59.Alikhani M., Alikhani Z., Boyd C., et al. Advanced glycation end products stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone. 2007;40(2):345–353. doi: 10.1016/j.bone.2006.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Franklin T. C., Wohleb E. S., Zhang Y., Fogaça M., Hare B., Duman R. S. Persistent increase in microglial RAGE contributes to chronic stress-induced priming of depressive-like behavior. Biological Psychiatry. 2018;83(1):50–60. doi: 10.1016/j.biopsych.2017.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anzilotti S., Giampà C., Laurenti D., et al. Immunohistochemical localization of receptor for advanced glycation end (RAGE) products in the R6/2 mouse model of Huntington’s disease. Brain Research Bulletin. 2012;87(2–3):350–358. doi: 10.1016/j.brainresbull.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 62.Yaturu S. Diabetes and skeletal health. Journal of Diabetes. 2009;1(4):246–254. doi: 10.1111/j.1753-0407.2009.00049.x. [DOI] [PubMed] [Google Scholar]
- 63.Soro-Paavonen A., Watson A. M. D., Li J., et al. Receptor for advanced glycation end products (RAGE) deficiency attenuates the development of atherosclerosis in diabetes. Diabetes. 2008;57(9):2461–2469. doi: 10.2337/db07-1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Panizo S., Cardus A., Encinas M., et al. RANKL increases vascular smooth muscle cell calcification through a RANK-BMP4-dependent pathway. Circulation Research. 2009;104(9):1041–1048. doi: 10.1161/circresaha.108.189001. [DOI] [PubMed] [Google Scholar]
- 65.Steitz S. A., Speer M. Y., Curinga G., et al. Smooth muscle cell phenotypic transition associated with calcification. Circulation Research. 2001;89(12):1147–1154. doi: 10.1161/hh2401.101070. [DOI] [PubMed] [Google Scholar]
- 66.Santavirta S., Konttinen Y., Nordstrom D., et al. Immunologic studies of nonunited fractures. Acta Orthopaedica. 1992;63(6):579–586. doi: 10.3109/17453679209169713. [DOI] [PubMed] [Google Scholar]
- 67.Petrova N. L., Shanahan C. M. Neuropathy and the vascular-bone axis in diabetes: lessons from Charcot osteoarthropathy. Osteoporosis International. 2013;25(4):1197–1207. doi: 10.1007/s00198-013-2511-6. [DOI] [PubMed] [Google Scholar]
- 68.Moon J.-S., Clark V. M., Beabout J. W., Swee R. G., Dyck P. J. A controlled study of medial arterial calcification of legs. Archives of Neurology. 2011;68(10):1290–1294. doi: 10.1001/archneurol.2011.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lehto S., Niskanen L., Suhonen M., Rönnemaa T., Laakso M. Medial artery calcification. Arteriosclerosis, Thrombosis, and Vascular Biology. 1996;16(8):978–983. doi: 10.1161/01.atv.16.8.978. [DOI] [PubMed] [Google Scholar]
- 70.Donath M. Y., Shoelson S. E. Type 2 diabetes as an inflammatory disease. Nature Reviews Immunology. 2011;11(2):98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 71.Edmonds M., Dew T., Musto R, et al. Serum proinflammatory cytokines TNF-alpha and IL-6 are raised in acute Charcot osteoarthropathy and correlate with a marker of bone resorption. Diabetologia. 2008;51(1):p. S510. [Google Scholar]
- 72.Satoh J., Yagihashi S., Toyota T. The possible role of tumor necrosis factor-α in diabetic polyneuropathy. Experimental Diabesity Research. 2003;4(2):65–71. doi: 10.1155/edr.2003.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thomsen S. B., Rathcke C. N., Zerahn B., Vestergaard H. Increased levels of the calcification marker matrix Gla protein and the inflammatory markers YKL-40 and CRP in patients with type 2 diabetes and ischemic heart disease. Cardiovascular Diabetology. 2010;9(1):p. 86. doi: 10.1186/1475-2840-9-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lopes-Virella M. F., Baker N. L., Hunt K. J., et al. Oxidized LDL immune complexes and coronary artery calcification in type 1 diabetes. Atherosclerosis. 2011;214(2):462–467. doi: 10.1016/j.atherosclerosis.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Uttara B., Singh A., Zamboni P., Mahajan R. Oxidative stress and neurodegenerative diseases: a review of upstream and downstream antioxidant therapeutic options. Current Neuropharmacology. 2009;7(1):65–74. doi: 10.2174/157015909787602823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brodeur M. R., Bouvet C., Bouchard S., et al. Reduction of advanced-glycation end products levels and inhibition of RAGE signaling decreases rat vascular calcification induced by diabetes. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0085922.e85922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim H., Kim H.-J., Lee K., et al. α-Lipoic acid attenuates vascular calcification via reversal of mitochondrial function and restoration of Gas6/Axl/Akt survival pathway. Journal of Cellular and Molecular Medicine. 2012;16(2):273–286. doi: 10.1111/j.1582-4934.2011.01294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wei Z., Yoshihara E., He N., et al. Vitamin D switches BAF complexes to protect β cells. Cell. 2018;173(5):1135–1149. doi: 10.1016/j.cell.2018.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Akhavani M. A., Sivakumar B., Paleolog E. M., Kang N. Angiogenesis and plastic surgery. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2008;61(12):1425–1437. doi: 10.1016/j.bjps.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 80.Yang M., Sheng L., Li H., Weng R., Li Q. F. Improvement of the skin flap survival with the bone marrow-derived mononuclear cells transplantation in a rat model. Microsurgery. 2010;30:275–281. doi: 10.1002/micr.20779. [DOI] [PubMed] [Google Scholar]
- 81.Kim H. J., Xu L., Chang K. C., et al. Anti-inflammatory effects of anthocyanins from black soybean seed coat on the keratinocytes and ischemia-reperfusion injury in rat skin flaps. Microsurgery. 2012;32(7):563–570. doi: 10.1002/micr.22019. [DOI] [PubMed] [Google Scholar]
- 82.Angel M. F., Narayanan K., Swartz W. M., et al. Deferoxamine increases skin flap survival: additional evidence of free radical involvement in ischaemic flap surgery. British Journal of Plastic Surgery. 1986;39(4):469–472. doi: 10.1016/0007-1226(86)90115-3. [DOI] [PubMed] [Google Scholar]
- 83.Mascotti D. P., Rup D., Thach R. E. Regulation of iron metabolism: translational effects medicated by iron, heme, and cytokines. Annual Review of Nutrition. 1995;15(1):239–261. doi: 10.1146/annurev.nutr.15.1.239. [DOI] [PubMed] [Google Scholar]
- 84.Im M. J., Manson P. N., Bulkley G. B., Hoopes J. E. Effects of superoxide dismutase and allopurinol on the survival of acute island skin flaps. Annals of Surgery. 1985;201(3):357–359. doi: 10.1097/00000658-198503000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun F., Iwaguchi K., Shudo R., et al. Change in tissue concentrations of lipid hydroperoxides, vitamin C and vitamin E in rats with streptozotocin-induced diabetes. Clinical Science. 1999;96(2):185–190. doi: 10.1042/cs19980189. [DOI] [PubMed] [Google Scholar]
- 86.Thornalley P. J. Use of aminoguanidine (Pimagedine) to prevent the formation of advanced glycation endproducts. Archives of Biochemistry and Biophysics. 2003;419(1):31–40. doi: 10.1016/j.abb.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 87.Maiorino M. I., Bellastella G., Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2014;7:95–105. doi: 10.2147/DMSO.S36455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Redrow G. P., Thompson C. M., Wang R. Treatment strategies for diabetic patients suffering from erectile dysfunction: an update. Expert opinion on pharmacotherapy. 2014;15(13):1827–1836. doi: 10.1517/14656566.2014.934809. [DOI] [PubMed] [Google Scholar]
- 89.Zhang Q., Radisavljevic Z. M., Siroky M. B., Azadzoi K. M. Dietary antioxidants improve arteriogenic erectile dysfunction. International Journal of Andrology. 2010;34(3):225–235. doi: 10.1111/j.1365-2605.2010.01083.x. [DOI] [PubMed] [Google Scholar]
- 90.Zhu D., Deng Y., Pan Y, et al. N-acetylcysteine ameliorates the erectile dysfunction caused by chronic intermittent hypoxia in rats: partly involvement of endoplasmic reticulum stress. Urology. 2015;86(4):e7–e14. doi: 10.1016/j.urology.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 91.Zhou K.-L., Zhang Y.-H., Lin D.-S., Tao X.-Y., Xu H.-Z. Effects of calcitriol on random skin flap survival in rats. Scientific Reports. 2016;6(1):p. 8945. doi: 10.1038/srep18945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ufuk E., Tuncer S., Kabakas F, et al. The effect of short- versus long-term administration of alpha tocopherol on the survival of random flaps in experimental diabetes mellitus. Journal of Diabetes and its Complications. 2004;18(5):249–257. doi: 10.1016/j.jdiacomp.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 93.Ozturk A., Fırat C., Parlakpınar H., Bay-Karabulut A., Kirimlioglu H., Gurlek A. Beneficial effects of aminoguanidine on skin flap survival in diabetic rats. Experimental Diabetes Research. 2012;2012:8. doi: 10.1155/2012/721256.721256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bozkurt M., Kapi E., Kulahci Y., et al. Antioxidant support in composite musculo-adipose-fasciocutaneous flap applications: an experimental study. Journal of Plastic Surgery and Hand Surgery. 2013;48(1):44–50. doi: 10.3109/2000656x.2013.800527. [DOI] [PubMed] [Google Scholar]
- 95.Cheng L., Chen T., Tu Q., et al. Naringin improves random skin flap survival in rats. Oncotarget. 2017;8(55):94142–94150. doi: 10.18632/oncotarget.21589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Asli C., Temel M., Dokuyucu R., Mutaf M. The effect of coenzyme Q10 (ubiquinone) on random pattern skin flap survival in rat model. Annals of Plastic Surgery. 2016;77(2):e9–e14. doi: 10.1097/sap.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 97.Liakopoulos V., Roumeliotis S., Gorny X., Dounousi E., Mertens P. R. Oxidative stress in hemodialysis patients: a review of the literature. Oxidative Medicine and Cellular Longevity. 2017;2017:22. doi: 10.1155/2017/3081856.3081856 [DOI] [PMC free article] [PubMed] [Google Scholar]