Abstract
A clear role for cellular metabolism in regulating immune cell function has recently been established. In a recent issue of Cell, Geiger et al. (2016) demonstrate a role for intracellular arginine abundance in T cells for the promotion of oxidative metabolism, increased cell viability, persistence, and in vivo antitumor response.
With the increased clinical utility of T cell mediated anticancer therapies including checkpoint inhibitor blockade, chimeric antigen receptor (CAR) T cells, and adoptive cell transfer (ACT) as therapies against melanoma, non-small cell lung cancer, various leukemias, lymphomas, and other types of tumors (Klebanoff et al. (2016), there has been growing interest in understanding the metabolic characteristics of T cells associated with efficacious antitumor responses. In new findings recently published in Cell, Lanzavecchia and colleagues (Geiger et al., 2016) describe a novel role for arginine metabolism in regulating T cell persistence, survival, and antitumor function.
T cells are not a homogeneous population of cells, instead existing as a variety of T cell subsets, each with a unique immune function. There is now a broad understanding that various subsets of immune cells exhibit metabolic profiles that serve to promote their specific cellular functions and that these metabolic programs often serve as a distinguishing phenotypic mark that may play an important role in maintaining the functionality and lineage stability of the cell (O’Neill et al., 2016). Recent work in the ACT setting has shown that specific subsets of T cells that have the capacity for long lifespans and increased self-renewal potential, such as Th17 CD4+ T cells and central memory-like CD8+ T cells, mediate effective antitumor responses (Klebanoff et al., 2005; Muranski et al., 2008). Further work characterizing the metabolic phenotype of these T cell subsets has shown that they possess a metabolic program of moderated glycolysis, with increased usage of mitochondrial oxidative metabolism. This program promotes cell longevity and is critical for sustained and effective T cell responses against pathogens and tumors. Conversely, terminally differentiated effector T cells that heavily rely on a glycolytic metabolic program exhibit reduced cell longevity and decreased antitumor response (Sukumar et al., 2013, 2016). Showing a broader role for metabolism in regulating the efficacy of antitumor T cells, longevity in CAR T cells may also be associated with an oxidative metabolic phenotype (Kawalekar et al., 2016). Therefore, as in numerous other immune settings, metabolism may play a key role in regulating the antitumor response of T cells.
One metabolic pathway known to play a role in the regulation of immune cell function is that of arginine metabolism in the macrophage setting. In inflammatory macrophages, arginine is directed toward the nitric oxide synthesis pathway, while tolerogenic macrophages that are associated with immunosuppression and wound healing metabolize arginine through the arginase pathway (Rath et al., 2014). The effects of arginine on T cell biology have been studied less thoroughly, although previous studies suggest that arginine plays a role in T cell function (O’Neill et al., 2016).
Using a combined proteomics and metabolomics analysis, Geiger et al. (2016) identified shifts in arginine metabolism during T cell activation that resulted in reduced intracellular L-arginine concentrations while downstream metabolites such as ornithine and citrulline were increased. The authors found that arginine plays an important role in regulating the T cell metabolic program, as supplementation of the culture medium with L-arginine resulted in decreased protein expression of glycolytic enzymes while TCA cycle and serine biosynthesis pathway enzyme expression was increased. Functionally, this resulted in reduced glucose consumption and increased mitochondrial oxidative phosphorylation, a metabolic phenotype consistent with increased T cell persistence and antitumor response.
While the proliferation rate of T cells cultured in L-arginine-supplemented medium was largely unaffected, Geiger et al. (2016) noted substantial decreases in the secretion of IFN-γ in T cells cultured under these conditions, indicating reduced effector character in these cells (Klebanoff et al., 2005). Further, the authors found that T cells cultured with increased L-arginine exhibited markers of a central memory phenotype such as increased CCR7 expression. Increased arginine levels in the culture medium also resulted in heightened T cell survival and accumulation in an in vivo antigen response model.
In an adoptive cell therapy model of T cell response to melanoma, Geiger et al. (2016) found that culturing T cells in medium supplemented with L-arginine resulted in improved tumor control and increased overall survival time. The authors observed that while the initial levels of IFN-γ production were reduced in T cells cultured in increased L-arginine, these cells exhibited an increased potential to produce IFN-γ upon subsequent stimulations. Additionally, the oral administration of L-arginine improved T cell-mediated antitumor activity in an in vivo melanoma model.
Mechanistically, Geiger et al. (2016) found that the effects of L-arginine on T cell survival were mediated in part by the nuclear proteins BAZ1B, PSIP1, and TSN. The authors hypothesize that these proteins act as arginine sensors in the cell, based on the observation that the proteins exhibited altered conformations in the presence of L-arginine. Additionally, the CRISPR-mediated deletion of these genes was sufficient to abrogate the effects of arginine on T cell survival. While these proteins are thought to be involved in regulating gene expression, their functional role in T cells, along with how arginine modulates their activities in regulating T cell biology, remains unclear.
In future work, it will be important to determine whether the presence of other amino acids and small molecule metabolites may exert influences similar to those of arginine on T cell function. It will also be interesting to determine whether the tumor microenvironment exhibits alterations in arginine availability, as this could certainly contribute to T cell dysfunction in that setting. For instance, high rates of tumor cell arginine uptake could reduce the intratumoral concentration of arginine to an extent that T cell metabolism and function are compromised, resulting in reduced T cell antitumor efficacy. Examining the mechanism through which T cell-mediated antitumor activity is improved will also be important, as increased intratumoral L-arginine levels may influence other resident immune cell subsets or perhaps even the properties of tumor cells. The authors propose that the arginine-mediated increase in survival and number of T cells is driven by elevated intracellular L-arginine concentrations, as preventing further cellular processing of arginine through the inhibition of arginase activity also increased T cell survival. The finding that the genetic deletion or inhibition of arginase with the small molecule nor-NOHA resulted in increased T cell persistence raises the possibility that pharmacologically or genetically targeting Arg2 may impact the antitumor T cell response.
Taken together, the exciting results of Geiger et al. (2016) show a role for L-arginine in modulating the metabolic profile and functionality of T cells to promote increased T cell survival and antitumor response through the maintenance of a T cell memory phenotype (Figure 1). These findings highlight the profound impact that metabolic pathways can have upon T cell biology and illustrate that the modulation of T cell metabolism presents a promising avenue toward the generation of more effective antitumor responses.
Figure 1. Arginine Promotes T Cell Memory Phenotype Acquisition.
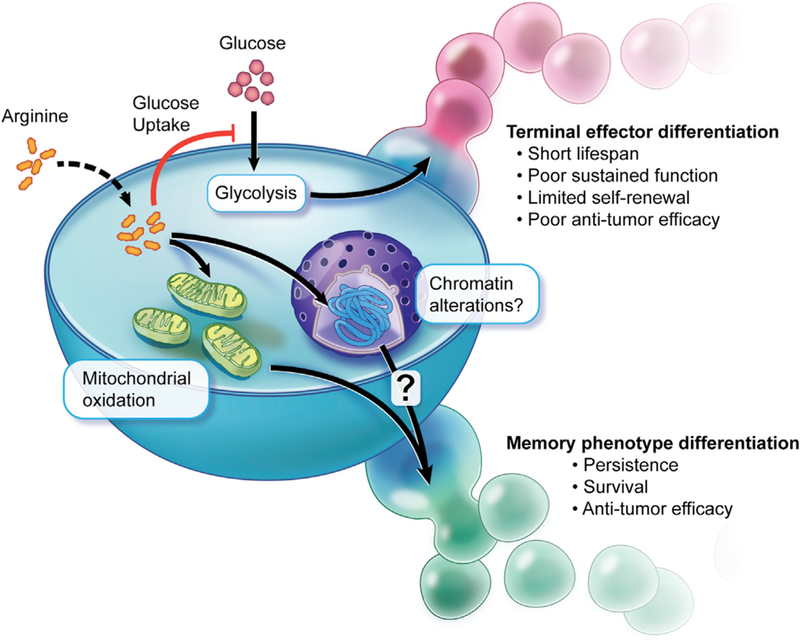
Increased levels of arginine in T cells result in the inhibition of glucose uptake and the promotion of mitochondrial oxidative metabolism. Concurrently, arginine modulates the conformation of several proteins involved in chromatin regulation. Together, these alterations in cell metabolism and perhaps gene expression driven by arginine promote the acquisition of a memory phenotype in T cells. This phenotype results in increased T cell survival, persistence, and an improved antitumor response.
REFERENCES
- Geiger R, Rieckmann JC, Wolf T, Basso C, Feng Y, Fuhrer T, Kogadeeva M, Picotti P, Meissner F, Mann M, et al. (2016). Cell 167, 829–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawalekar OU, O’Connor RS, Fraietta JA, Guo L, McGettigan SE, Posey AD Jr., Patel PR, Guedan S, Scholler J, Keith B, et al. (2016). Immunity 44, 380–390. [DOI] [PubMed] [Google Scholar]
- Klebanoff CA, Gattinoni L, Torabi-Parizi P, Kerstann K, Cardones AR, Finkelstein SE, Palmer DC, Antony PA, Hwang ST, Rosenberg SA, et al. (2005). Proc. Natl. Acad. Sci. USA 102, 9571–9576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanoff CA, Rosenberg SA, and Restifo NP (2016). Nat. Med 22, 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muranski P, Boni A, Antony PA, Cassard L, Irvine KR, Kaiser A, Paulos CM, Palmer DC, Touloukian CE, Ptak K, et al. (2008). Blood 112, 362–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill LA, Kishton RJ, and Rathmell J (2016). Nat. Rev. Immunol 16, 553–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rath M, Müller I, Kropf P, Closs EI, and Munder M (2014). Front. Immunol 5, 532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukumar M, Liu J, Ji Y, Subramanian M, Crompton JG, Yu Z, Roychoudhuri R, Palmer DC, Muranski P, Karoly ED, et al. (2013). J. Clin. Invest 123, 4479–4488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukumar M, Liu J, Mehta GU, Patel SJ, Roy choudhuri R., Crompton JG, Klebanoff CA, Ji Y, Li P, Yu Z, et al. (2016). Cell Metab 23, 63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]


