Abstract
Background:
Surgical reconstruction of the anterior cruciate ligament (ACL) is one of the most common orthopaedic procedures, with an estimated 100,000 to 175,000 procedures performed annually. Recently, the all-inside reconstruction technique has come into favor and is theorized to be superior to the complete tibial tunnel technique.
Purpose:
To compare clinical and patient-reported outcomes (PROs) for hamstring autograft ACL reconstruction (ACLR) performed with an all-inside versus a complete tibial tunnel technique.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients who underwent hamstring autograft ACLR via either an all-inside approach (femoral and tibial sockets) or a complete tibial tunnel approach (femoral socket and full-length, transtibial tunnel) at a single institution between July 2011 and July 2015 were reviewed. Demographic information, preoperative comorbidities, surgical details, physical examination findings, and follow-up outcomes were extracted from the medical record. Physical examination data included pivot-shift, Lachman, and range of motion examinations, whereas PROs included the Tegner activity scale, Lysholm score, and International Knee Documentation Committee (IKDC) score at a minimum of 2 years after surgery. Return to sport and risk factors for failure were analyzed.
Results:
A total of 82 patients (mean ± SD age, 25.8 ± 10.2 years) who underwent all-inside reconstruction (median PRO follow-up, 30.1 months; range, 24.7-72.9 months) and 54 patients (mean ± SD age, 21.1 ± 7.3 years) who underwent complete tibial tunnel reconstruction (median PRO follow-up, 25.8 months; range, 23.9-74.5 months) met the inclusion criteria. PRO scores at latest follow-up were comparable between the all-inside versus the complete tibial tunnel groups (Lysholm score, 93.8 vs 94.4, P = .621; IKDC score, 93.5 vs 93.3, P = .497; Tegner activity score, 6.4 vs 6.8, P = .048). Complications (including graft failure) were experienced by 20% of patients in the all-inside group compared with 24% in the complete tibial tunnel group (P = .530). Graft failure before the final follow-up was experienced by 10% of patients in the all-inside group compared with 19% in the complete tibial tunnel group (P = .200). Mean return to sport was 12.5 months in the all-inside group versus 9.9 months in the complete tibial tunnel group (P = .028).
Conclusion:
All-inside and complete tibial tunnel hamstring autograft ACLR resulted in excellent physical examination findings and PROs at minimum 2-year follow-up. Both techniques successfully restored knee stability and patient function.
Keywords: anterior cruciate ligament reconstruction; ACL; all-inside; complete tibial tunnel
Surgical reconstruction of the anterior cruciate ligament (ACL) is one of the most common orthopaedic procedures, with an estimated 100,000 to 175,000 ACL reconstructions (ACLRs) performed annually.5,9,10,17,20,24 The number of ACLR procedures performed in the United States has increased significantly since the mid-1990s, owing in part to a dramatic increase in the number of ambulatory procedures undergone by female patients.5,9,13 Recently, the all-inside reconstruction technique has come into favor and is theorized to be superior to the complete tibial tunnel technique. All-inside reconstruction uses a socket for both the femur and tibia that accommodates the intraosseous length of the graft. Advantages of all-inside reconstruction include preservation of femoral and tibial bone mass, less cortical bone periosteal disruption, decreased postoperative pain, and, in most cases, a single hamstring tendon harvest that produces a larger diameter graft.2,15,23,30,31 However, possible disadvantages of all-inside reconstruction include, but may not be limited to, the surgical learning curve, more extensive ACL tibial stump excision, and suspensory cortical tibial fixation.
All-inside reconstruction has been biomechanically assessed. Outcomes of all-inside and complete tibial tunnel techniques using an allograft tendon are comparable.15 Additional case series have shown improved functional outcomes between baseline and 2-year clinical follow-up when the all-inside technique is used.23,31 However, a cohort comparison of all-inside hamstring autograft reconstruction versus complete tibial tunnel reconstruction has not been reported in the literature. Regardless of graft type, failure and revision rates are reported to be higher in younger patients, likely because of their active lifestyle and quicker return to sport.1,14,21,22
The purpose of this study was to compare clinical results and patient-reported outcomes (PROs) of a large group of patients who underwent hamstring autograft ACLR by an all-inside technique versus those who received a complete tibial tunnel during ACLR. We hypothesized that outcomes of ACLR using hamstring autograft with the all-inside technique would be comparable to outcomes of the complete tibial tunnel technique.
Methods
This retrospective cohort study was performed at a single institution after approval was obtained from an institutional review board. The medical record database was queried for all patients who underwent ACLR from July 2011 to July 2015 by 1 of the senior authors (M.J.S., D.L.D., B.A.L., or A.J.K.). Patients were included only if they had primary ACLR with semitendinosus or semitendinosus/gracilis autograft. A total of 210 patients were initially identified for this study. Exclusion criteria consisted of revision ACL procedures, the use of allografts or patellar tendon autografts, concomitant posterior cruciate or collateral ligament surgery, and a lack of minimum 2-year patient follow-up. Patients were not excluded on the basis of age. Overall, 12 patients with revision ACLR, 2 patients with multiligament reconstruction, 1 patient with a combined allograft-autograft construct, and 1 patient with reactive arthritis were excluded. Of the 194 eligible patients, 136 (70.1%) were contacted at minimum 2-year follow-up (Figure 1).
Figure 1.
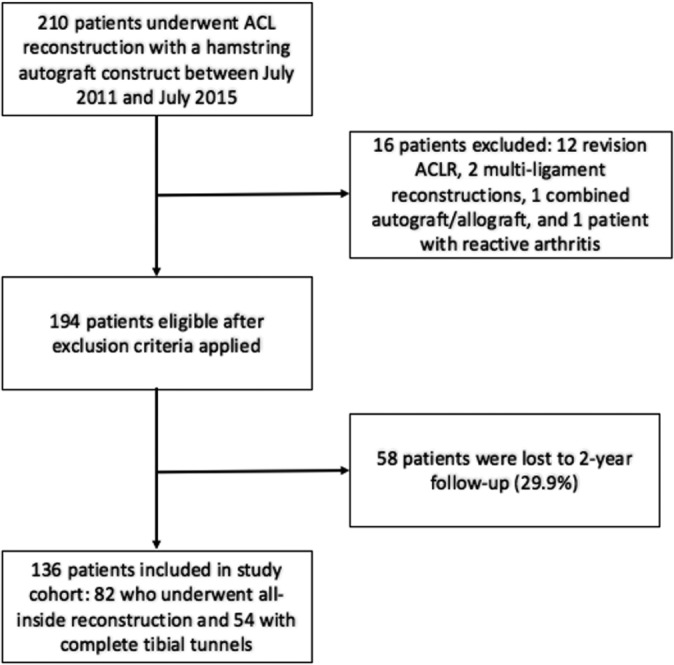
Flow of patients through the study. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Each patient’s operative note was manually reviewed to confirm the surgical technique performed, including the graft type, graft construct, fixation technique, and other intraoperative details such as concomitant procedures. The patients were assigned to 1 of 2 groups: all-inside technique or complete tibial tunnel technique. Medical records of all patients were reviewed to obtain the patient demographic characteristics, injury details, physical examination findings, graft diameter, complications, return-to-sport time, and clinical outcomes. Patients were contacted via telephone when necessary. Failure was defined as graft rupture and/or requirement for revision reconstruction.
Surgical Technique
Patients in this study underwent primary ACLR with either an all-inside or a complete tibial tunnel technique according to the individual surgeon’s preference. The graft constructs were composed of quadrupled semitendinosus tendon or combined doubled semitendinosus and doubled gracilis tendons. Further folding of the semitendinosus tendon strands and/or augmentation with additional hamstring strands was required in 4 cases (2 patients with a 6-strand gracilis-semitendinosus construct and 2 patients with a 7-strand gracilis-semitendinosus construct) to achieve the necessary graft thickness.
For the all-inside reconstructions, the femoral socket was created with a low-profile reamer and drilled in anterograde fashion from within the joint or in a retrograde fashion by use of a FlipCutter (Arthrex) to an osseous depth of at least 20 mm. The transportal offset guide was positioned to create the socket at the insertion site of the direct ACL fibers with a 1-mm proximal wall. The tibial socket was created in a retrograde fashion by use of a FlipCutter. The guide was positioned to create the socket aperture adjacent to the lateral meniscal anterior horn attachment. The graft was passed into the knee through the anteromedial portal, the femoral button was engaged on the lateral femoral cortex, and the graft was advanced into the femur through use of TightRope (Arthrex) shortening strands. The distal end of the graft was then passed into the tibial socket, and the TightRope button was engaged on the medial tibial cortex. The entire construct (GraftLink; Arthrex) was tensioned in full extension, the knee was flexed and extended, and the graft was retensioned on both the tibial and femoral sides.
For the complete tibial tunnel technique, a low-profile reamer was used to create a femoral socket that was at least 20 mm long. The transportal offset guide was positioned to create the socket at the insertion site of the direct ACL fibers with a 1-mm proximal wall. The tibial tunnel was created by means of a rigid reamer or a FlipCutter. The guide was positioned to create the tunnel aperture adjacent to the lateral meniscal anterior horn attachment. The graft was passed into the tibial tunnel, through the intra-articular space, and into the femoral socket. The cortical fixation device, either Endobutton (Smith & Nephew), TightRope, or RetroButton (Arthrex), was engaged on the femoral cortex. The graft was tensioned in full extension; the knee was flexed and extended and then fixed with a tibial Bio-Compression Screw (Arthrex). The screw diameter matched the tunnel size, creating a line-to-line fit.
All patients underwent a standardized postoperative rehabilitation program, including immediate knee extension equal to the preoperative measurement, return to running at 3 months, and return to cutting and pivoting sports at 9 to 12 months.
Statistical Analysis
Patient characteristics including demographic factors, time from injury to surgery, duration of in-clinic and patient-reported follow-up, physical examination findings, complication rates, and final outcomes were summarized by use of descriptive statistics including mean, standard deviation, range, and percentage when necessary. The appropriate hypothesis testing (Fisher exact test, Wilcoxon rank-sum test, and Pearson chi-square test when applicable) was performed via JMP Pro 10.0.0 to assess for statistically significant differences in group demographics, complications, failure rates, physical examination findings, and PROs as well as to compare results across surgical technique, graft diameter, graft construct, and fixation device. Kaplan-Meier survival analysis was used to compare time to failure between both patient groups. P values less than .05 were considered to be statistically significant.
Results
A total of 82 patients in the all-inside group and 54 patients in the complete tibial tunnel group had a minimum follow-up of 2 years and met all inclusion criteria. Demographic characteristics of both groups are provided in Table 1. Concomitant injuries and operations at the time of index surgery in the 2 patient groups are described in Tables 2 and 3. Presence of a lateral meniscal tear in more patients from the all-inside group was the only difference between the groups that reached statistical significance, however this difference likely did not affect overall outcomes.
TABLE 1.
Demographic Characteristics of the Study Groups
| Characteristic | All-Inside Group (n = 82) | Complete Tibial Tunnel Group (n = 54) | P |
|---|---|---|---|
| Age, y, mean ± SD | 25.8 ± 10.2 | 21.1 ± 7.3 | .008a |
| Preinjury Tegner score, mean (range) | 6.6 (4-8) | 7.0 (5-9) | .056 |
| Sex, % male | 59.8 | 57.4 | .859 |
| Mean body mass index | 25.1 | 25.1 | .838 |
| Laterality, % right-sided | 51.2 | 57.4 | .489 |
| Time from injury to reconstruction, mo, median (range) | 2.3 (0.26-180.7) | 2.0 (0.5-34.7) | .263 |
| Duration of clinical follow-up, mo, median (range) | 23.9 (0.7-59.9) | 24.6 (1.7-61.5) | .122 |
| Duration of follow-up for patient-reported outcomes, mo, median (range) | 30.1 (24.7-72.9) | 25.8 (23.9-74.5) | .713 |
aStatistically significant difference between groups (P < .05).
TABLE 2.
Concomitant Injuries at Index Surgerya
| Injury | All-Inside Group (n = 82) | Complete Tibial Tunnel Group (n = 54) | P |
|---|---|---|---|
| None | 18 (22.0) | 19 (35.2) | .115 |
| Medial meniscal injury | 36 (43.9) | 21 (38.9) | .598 |
| Lateral meniscal injury | 36 (43.9) | 14 (25.9) | .045b |
| Chondromalacia/chondral defect | 19 (23.2) | 9 (16.7) | .394 |
| Medial collateral ligament sprain | 3 (3.7) | 5 (9.3) | .264 |
| Otherc | 2 (2.4) | 1 (1.9) | .999 |
aValues are expressed as n (%).
bStatistically significant difference between groups (P < .05).
cOther injuries included 1 patient with a tibial plateau fracture and 1 patient with a bony avulsion in the all-inside group and 1 patient with previous tibial hardware in the complete tibial tunnel group.
TABLE 3.
Concomitant Surgeries at Index Surgerya
| Surgery | All-Inside Group (n = 82) | Complete Tibial Tunnel Group (n = 54) | P |
|---|---|---|---|
| None | 21 (25.6) | 22 (40.7) | .089 |
| Meniscal repair/meniscectomy | 51 (62.2) | 30 (55.6) | .478 |
| Chondral defect repair/chondroplasty | 17 (20.7) | 7 (13.0) | .245 |
| Otherb | 3 (3.7) | 1 (1.9) | .999 |
aValues are expressed as n (%).
bOther surgeries included 1 high tibial osteotomy, 1 loose body removal, and 1 meniscal allograft transplant in the all-inside group and 1 tibial hardware removal in the complete tibial tunnel group.
The most commonly used graft construct and fixation in the all-inside group was a quadrupled semitendinosus autograft (74.4% of procedures), and 100% of procedures used the TightRope fixation device. The most commonly used graft in the complete tibial tunnel group was a combined double semitendinosus with double gracilis (92.6% of procedures); 65% of procedures used the Endobutton, 34% the TightRope, and 1% the RetroButton fixation devices. The mean graft diameter was 9.0 mm (range, 8.0-10.5 mm; SD, 0.6 mm) in the all-inside group versus 8.3 mm (range, 7.0-10.0 mm; SD, 0.7 mm) in the complete tibial tunnel group (P < .0001).
Physical examination data at the latest in-clinic visit for those patients who did not experience failure are displayed in Tables 4 and 5. At a mean 2-year follow-up, the mean range of motion in the all-inside group was 0.2° of hyperextension (range, –5° to 10°; SD, 2.1°) to 136.4° of flexion (range, 115° to 155°; SD, 7.0°), and in the complete tibial tunnel group it was 0.3° of hyperextension (range, –5° to 5°; SD, 1.9°) to 132.9° of flexion (range, 130° to 145°; SD, 4.7°).
TABLE 4.
Data for the All-Inside Group at the Latest Physical Examinationa
| Lachman | Pivot Shift | ||
|---|---|---|---|
| Negative | 73 (98.6) | Negative | 61 (82.4) |
| 1+ | 1 (1.4) | 1+ | 0 (0.0) |
| 2+ | 0 (0.0) | 2+ | 0 (0.0) |
| No data | 0 (0.0) | No data | 13 (17.6) |
| Total | 74 (100.0) | Total | 74 (100.0) |
aThese data are for patients whose grafts did not fail. Values are expressed as n (%).
TABLE 5.
Data for the Complete Tibial Tunnel Group at the Latest Physical Examinationa
| Lachman | Pivot Shift | ||
|---|---|---|---|
| Negative | 38 (86.4) | Negative | 36 (81.8) |
| 1+ | 5 (11.4) | 1+ | 6 (13.6) |
| 2+ | 1 (2.3) | 2+ | 0 (0.0) |
| No data | 0 (0.0) | No data | 2 (4.5) |
| Total | 44 (100.0) | Total | 44 (100.0) |
aThese data are for patients whose grafts did not fail. Values are expressed as n (%).
Overall, 8 of 82 patients (9.8%) in the all-inside group and 10 of 54 patients (18.5%) in the complete tibial tunnel group experienced failure prior to final follow-up (P = .200). Complication and reoperation rates are described in Table 6. PRO scores are presented in Table 7.
TABLE 6.
Complication, Reoperation, and Failure Rates in the Study Groupsa
| Complications, Reoperations, and Failures | All-Inside Group (n = 82)b | Complete Tibial Tunnel Group (n = 54) | P |
|---|---|---|---|
| None | 66 (80.5) | 41 (75.9) | .530 |
| Infection (required reoperation) | 1 (1.2) | 0 (0.0) | .999 |
| Arthrofibrosis (required reoperation) | 2 (2.4) | 1 (1.9) | .999 |
| Revision meniscal surgery | 3 (3.7) | 2 (3.7) | .989 |
| Revision ACLR (failure) | 8 (9.8) | 10 (18.5) | .200 |
| Otherc | 3 (3.7) | 0 (0.0) | .277 |
aValues are expressed as n (%). ACLR, anterior cruciate ligament reconstruction.
bOne patient in the all-inside group had 2 reported complications.
cOther complications included 2 chondral defects requiring debridement and 1 case of superficial wound dehiscence requiring reoperative closure.
TABLE 7.
Patient-Reported Outcome Scores for the Study Groupsa
| Scoring System | All-Inside Group | Complete Tibial Tunnel Group | P |
|---|---|---|---|
| Lysholm score | 93.8 (60.0-100) | 94.4 (63.0-100) | .621 |
| IKDC score | 93.5 (62.1-100) | 93.3 (77.8-100) | .497 |
| Tegner activity score | 6.4 (5-8) | 6.8 (5-9) | .048b |
aThese data are for patients whose grafts did not fail. Values are expressed as mean (range). IKDC, International Knee Documentation Committee.
bStatistically significant difference between groups (P < .05).
No statistically significant difference was found in Lysholm and IKDC scores between the 2 groups of patients; however, those in the complete tibial tunnel group had higher Tegner scores at the latest follow-up (P = .048). Differences in failure rates, complications, and reoperation rates between the 2 groups did not reach statistical significance, as shown in Table 6. Furthermore, no statistically significant relationship was found between postoperative outcomes and fixation type, graft diameter, or graft construct. Average time to return to sport was 12.5 months in the all-inside group compared with 9.9 months in the complete tibial tunnel group (P = .028). Graft diameter for the entire group of patients was stratified into 2 size brackets: >9 mm or ≤9 mm. The failure rate in those with a graft diameter >9 mm was 11.43% compared with 15.15% in those with a diameter ≤ 9 mm. Fisher exact test revealed no significant difference in failure rate between the 2 graft diameters (P = .616).
Mean time to failure was 13.59 ± 5.65 months in the all-inside group and 21.44 ± 12.86 months in the complete tibial tunnel group. A survival plot comparing time to failure is shown in Figure 2.
Figure 2.
Survival plot comparing time to failure between both groups of patients shows a mean time to failure of 13.59 ± 5.65 months in the all-inside group and 21.44 ± 12.86 months in the complete tibial tunnel group. Furthermore, the plot illustrates an ultimately higher failure rate in the complete tibial tunnel group; however, this did not reach statistical significance.
Discussion
The present study is a comparative analysis of a large group of patients who underwent ACLR by means of hamstring autograft with an all-inside method (GraftLink) or a complete tibial tunnel technique, performed during the same time period (July 2011 to July 2015). Our cohort of 136 patients represents the largest of such studies to date comparing these techniques. The data showed that both all-inside and complete tibial tunnel ACLR techniques resulted in successful restoration of knee ligamentous stability, positive PROs, high return to sport rates, and overall comparable results. Furthermore, the all-inside technique demonstrated a lower failure rate. Our hypothesis was supported in that patients who underwent all-inside ACLR had similarly positive PROs and physical examination results relative to those who underwent complete tibial tunnel reconstruction. Failure rates between the 2 groups were not significantly different; however, the high failure rate observed in the complete tibial tunnel group is concerning.
The mean postoperative Tegner score in the all-inside group was 6.4 (range, 5-8; SD, 0.8) (preinjury score, 6.6 [range, 4-8; SD, 0.8]), and in the complete tibial tunnel group it was 6.8 (range, 5-9; SD, 0.9) (preinjury score, 7.0 [range, 5-9; SD, 0.7]) (P = .048), indicating that patients in both groups returned to near their preinjury levels of activity, which were predominantly nonelite recreational or competitive sport levels.4,27 Although the higher Tegner scores demonstrated by the complete tibial tunnel group reached statistical significance, this finding is likely not clinically significant given the similarity in magnitude of mean scores between the 2 groups. The mean age for both groups fell within that of a relatively active age group, and thus this difference in score is not likely confounded by patient age. Mean postoperative IKDC scores were 93.5 (range, 62.1-100; SD, 8.4) in the all-inside group and 93.3 (range 77.8-100; SD, 7.0) in the complete tibial tunnel group (P = .497), indicating that patients in both cohorts had little to no limitation with daily or sporting activities and minimal or absent symptoms following surgery.7 Mean postoperative Lysholm scores were 93.8 (range, 60-100; SD, 7.8) in the all-inside group and 94.4 (range, 63-100; SD, 7.6) in the complete tibial tunnel group (P = .621) suggesting an excellent level of knee performance.18
The findings of the present study are consistent with those reported in the literature. Volpi et al28 used Tegner, Lysholm, and IKDC scores to compare 20 patients with all-inside reconstruction and 20 patients with traditional transtibial reconstruction; the investigators found comparable outcomes in return to sport and articular function and concluded that all-inside reconstruction did not yield superior results. A randomized controlled trial by Lubowitz et al15 showed no difference in IKDC scores between patients undergoing all-inside versus complete tibial tunnel ACLR, although patients from that study specifically underwent an allograft tissue reconstruction. Benea et al2 randomized 46 patients to undergo either all-inside or complete tibial tunnel ACLR and found no significant difference in mean IKDC subjective scores at 6 months postoperatively.
In the current study, 8 patients (9.8%) in the all-inside group and 10 patients (18.5%) in the complete tibial tunnel group experienced graft failure requiring revision surgery prior to final follow-up. This observation was not statistically significant, but the high failure rate for hamstring autograft ACLR with a full-length tibial tunnel is concerning. Of note, the higher failure rate was not associated with any of the individual contributing surgeons in this study. All-inside ACLR failure rates reported in the literature range from 4.9% to 12.7%.3,8,23,31 The mechanism of failure for all grafts in this study was either sports-related injury or trauma, consistent with the reports of prior studies.23,31 In contrast to our findings, Connaughton et al8 reported a concern for higher graft failure rates in all-inside ACLR; however, the studies used in their analysis entailed allograft reconstructions, which are inherently more prone to failure in the young, active patient population.14,19,22 No conclusive findings regarding graft failure rates with autograft reconstruction using the 2 reconstruction techniques were found in the literature.
In our study, graft diameter was larger on average in the all-inside group versus the complete tibial tunnel group (9.0 vs 8.3 mm, respectively). Prior studies have reported that smaller graft diameter may play a role in worsening outcomes following ACLR.16,25,26 In our study, smaller graft diameter (≤9 mm) was not correlated with higher failure rates (P = .616). Although the graft diameter was larger in the all-inside group, this is consistent with the nature of the technique and should be viewed not as a confounder but rather as an inherent property of this surgical technique when compared with complete tibial tunnel reconstruction. Wernecke et al29 reported that increased hamstring autograft diameter did not significantly reduce the need for revision ACLR or improve clinical outcomes. However, prior studies have documented that hamstring grafts smaller than 8 mm are more vulnerable to failure.16
In the current study, the return-to-sport interval was significantly shorter and graft diameter was significantly smaller in the complete tibial tunnel group. However, it is not likely that earlier return to sport was a causative factor, as graft failure occurred at a mean of 21.44 months after surgery in the complete tibial tunnel group.
This study is limited by its retrospective nature. The 2 groups of patients differed in mean age (25.8 vs 21.1, P = .008) at the time of surgery; however, both ages fell within an accepted range of skeletal maturity.6,11,12 Preinjury Tegner activity scores were similar between the 2 groups, suggesting comparable preinjury activity levels. The patient groups had comparable body mass index, numbers of concomitant injuries and operations at the time of index surgery, duration from injury to surgery, and preoperative activity scores but were not explicitly matched by their comorbidities or demographic features. Four surgeons at a single institution performed the procedures, which could have led to slight variation in technique, graft selection, and fixation devices. In addition, 30% of eligible patients were lost to follow-up. Finally, use of the Tegner activity score and return to sport as outcome measures has inherent limitations, given that these parameters fail to incorporate how psychological factors or life events may prevent patients from participating in their highest level of activity or desired sport over the course of their rehabilitation. Despite the above limitations, our large sample of compatible patient cohorts, thorough analysis of preoperative patient and injury characteristics, and duration of clinical examination and patient-reported follow-up have provided the means for valuable information to guide ACLR practices.
Conclusion
All-inside and complete tibial tunnel hamstring autograft ACLR resulted in excellent physical examination findings and patient-reported outcomes at minimum 2-year follow-up. Both techniques successfully restored knee stability and patient function.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.A.L. receives royalties from Arthrex; is a paid consultant for Arthrex and Smith & Nephew; and receives research support from Arthrex, Biomet, Smith & Nephew, and Stryker. D.L.D. receives research support from Arthrex and is a member of the NBA/GE Strategic Advisory Board, and her spouse has stock/stock options in and receives royalties from Tenex Health and Sonex Health. C.L.C. has received educational support from Arthrex and Zimmer Biomet and hospitality payments from Arthrex. A.J.K. receives research support from Aesculap/B. Braun and the Arthritis Foundation; receives royalties from Arthrex; and is a paid consultant for Arthrex, Vericel, DePuy Orthopaedics, and the Musculoskeletal Transplant Foundation. M.J.S. receives royalties from Arthrex, is a paid consultant for Arthrex, receives research support from Stryker, and has received hospitality payments from Gemini Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic (IRB No. 15-000601).
References
- 1. Astur DC, Cachoeira CM, da Silva Vieira T, Debieux P, Kaleka CC, Cohen M. Increased incidence of anterior cruciate ligament revision surgery in paediatric versus adult population. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1362–1366. [DOI] [PubMed] [Google Scholar]
- 2. Benea H, d’Astorg H, Klouche S, Bauer T, Tomoaia G, Hardy P. Pain evaluation after all-inside anterior cruciate ligament reconstruction and short term functional results of a prospective randomized study. Knee. 2014;21(1):102–106. [DOI] [PubMed] [Google Scholar]
- 3. Blackman AJ, Stuart MJ. All-inside anterior cruciate ligament reconstruction. J Knee Surg. 2014;27(5):347–352. [DOI] [PubMed] [Google Scholar]
- 4. Briggs KK, Steadman JR, Hay CJ, Hines SL. Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37(5):898–901. [DOI] [PubMed] [Google Scholar]
- 5. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3(1):2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Calfee RP, Sutter M, Steffen JA, Goldfarb CA. Skeletal and chronological ages in American adolescents: current findings in skeletal maturation. J Child Orthop. 2010;4(5):467–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee injury and Osteoarthritis Outcome Score (KOOS), Knee injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63(suppl 11):S208–S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Connaughton AJ, Geeslin AG, Uggen CW. All-inside ACL reconstruction: how does it compare to standard ACL reconstruction techniques? J Orthop. 2017;14(2):241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Csintalan RP, Inacio MCS, Funahashi TT. Incidence rate of anterior cruciate ligament reconstructions. Perm J. 2008;12(3):17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. [PubMed] [Google Scholar]
- 11. Groell R, Lindbichler F, Riepl T, Gherra L, Roposch A, Fotter R. The reliability of bone age determination in central European children using the Greulich and Pyle method. Br J Radiol. 1999;72(857):461–464. [DOI] [PubMed] [Google Scholar]
- 12. Hansman CF, Maresh MM. A longitudinal study of skeletal maturation. Am J Dis Child. 1961;101:305–321. [DOI] [PubMed] [Google Scholar]
- 13. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171(8):808–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lubowitz JH, Schwartzberg R, Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29(7):1195–1200. [DOI] [PubMed] [Google Scholar]
- 16. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 17. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 18. Mitsou A, Vallianatos P, Piskopakis N, Maheras S. Anterior cruciate ligament reconstruction by over-the-top repair combined with popliteus tendon plasty. J Bone Joint Surg Br. 1990;72(3):398–404. [DOI] [PubMed] [Google Scholar]
- 19. Pallis M, Svoboda SJ, Cameron KL, Owens BD. Survival comparison of allograft and autograft anterior cruciate ligament reconstruction at the United States Military Academy. Am J Sports Med. 2012;40(6):1242–1246. [DOI] [PubMed] [Google Scholar]
- 20. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325. [DOI] [PubMed] [Google Scholar]
- 21. Sanders TL, Pareek A, Hewett TE, et al. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):222–228. [DOI] [PubMed] [Google Scholar]
- 22. Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schurz M, Tiefenboeck TM, Winnisch M, et al. Clinical and functional outcome of all-inside anterior cruciate ligament reconstruction at a minimum of 2 years’ follow-up. Arthroscopy. 2016;32(2):332–337. [DOI] [PubMed] [Google Scholar]
- 24. Spindler KP, Wright RW. Anterior cruciate ligament (ACL) tear. N Engl J Med. 2008;359(20):2135–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Spragg L, Chen J, Mirzayan R, Love R, Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(6):1475–1481. [DOI] [PubMed] [Google Scholar]
- 26. Steiner M. Editorial commentary: size does matter—anterior cruciate ligament graft diameter affects biomechanical and clinical outcomes. Arthroscopy. 2017;33(5):1014–1015. [DOI] [PubMed] [Google Scholar]
- 27. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 28. Volpi P, Bait C, Cervellin M, et al. No difference at two years between all inside transtibial technique and traditional transtibial technique in anterior cruciate ligament reconstruction. Muscles Ligaments Tendons J. 2014;4(1):95–99. [PMC free article] [PubMed] [Google Scholar]
- 29. Wernecke GC, Constantinidis A, Harris IA, Seeto BG, Chen DB, MacDessi SJ. The diameter of single bundle, hamstring autograft does not significantly influence revision rate or clinical outcomes after anterior cruciate ligament reconstruction. Knee. 2017;24(5):1033–1038. [DOI] [PubMed] [Google Scholar]
- 30. Wilson AJ, Yasen SK, Nancoo T, Stannard R, Smith JO, Logan JS. Anatomic all-inside anterior cruciate ligament reconstruction using the translateral technique. Arthrosc Tech. 2013;2(2):e99–e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yasen SK, Borton ZM, Eyre-Brook AI, et al. Clinical outcomes of anatomic, all-inside, anterior cruciate ligament (ACL) reconstruction. Knee. 2017;24(1):55–62. [DOI] [PubMed] [Google Scholar]



