Abstract
Introduction:
It is widely known that the mind and the body, although described medically almost as separate entities, are in fact highly interrelated. This is not, however, always reflected within medical settings where physical interventions are often favoured over more holistic management, even in the case of long-term symptoms and/or pain where there is a strong evidence to favour the use of the latter. Mindfulness is an established and evidence-based intervention which can help people living with pain and physical symptoms. Interventions based on Compassion and Loving-kindness have also shown early promise but have not been fully explored. This study proposes a compassion-focused conceptualisation of persistent pain and reports on an intervention based upon this formulation.
Methods:
The study took place within a routine clinical setting. Standardised outcome measures were collected pre- and post-intervention and effect sizes calculated for mean differences on each measure. Written qualitative comments that participants attributed to the group were also collected post-intervention and analysed with a thematic analysis. This was an uncontrolled, unpowered study conducted within a clinical setting which aimed to examine the intervention for any initial evidence of promise and to explore how it would be received by patients.
Results:
The results of the study indicated that engagement of patients in the intervention was reasonable. Improvements were recorded in pain distress (effect size (ES), 0.47) and intensity (ES, 0.23), anxiety (ES, 0.72), depression (ES, 0.46) and self-efficacy (ES, 0.36). Following the intervention, patients described changes that were grouped into the categories of feeling different, doing things differently and changed attitude.
Conclusion:
This exploratory study has demonstrated that a group-based intervention based on a model of compassion and including mindfulness and loving-kindness exercise has potential as an intervention to be used within routine pain management settings.
Keywords: Pain management, pain clinics, pain, musculoskeletal pain, fibromyalgia, chronic pain, back pain
Introduction
It has been known for some time that physiological processes, influenced by the mind, exert more influence over pain intensity than the degree of structural damage to the body.1–3 In keeping with this knowledge, it has been shown that psychological treatments in general,4 and specifically interventions based on mindfulness,5 cognitive behaviour therapy (CBT)6 and acceptance and commitment therapy (ACT),7 are beneficial for people with long-term (persistent) pain. All of these interventions are grounded in various theoretical models/frameworks, but to date there has been very limited published interest in group-based pain management interventions explicitly grounded in a compassion-based model of persistent pain. There are, however, limited data with a high degree of attrition bias8,9 that suggest a compassion-focused intervention may have promise in helping in the management of persistent pain, especially in reducing pain intensity, anger and or psychological distress.
The compassion-focused therapy model described by Gilbert10 may be well placed to provide a framework for understanding persistent pain as it is grounded within a neurobiological understanding of the three systems within which our emotions are organised. These three systems guide our response to internal and external cues:
The first system, ‘the threat system’, becomes active in response to internal (e.g. fear generated from our memory) or external (e.g. visually identifying an assailant approaching) stimuli and helps us in fight or flight being regulated by hormones including serotonin.11 It serves a useful function, but can also become damaging if activated in the long term causing increased inflammation thereby predisposing to other health problems.12 Of the three systems, it is the most easily activated and will suppress the other systems when active.
The second emotional system, ‘the drive system’, becomes active in response to the need to seek resources and compete for status and is regulated by hormones including dopamine.11
The third and final system, ‘the affiliative or soothing system’, helps us to seek closeness and to forge and maintain affiliative and safe nurturing relationships with others. It is regulated by hormones which include opiates and oxytocin.11 This system is linked to the attachment system and so likely to be under-developed in people who have encountered difficulties during their early years, such as experiencing more threats than caring behaviours from caregivers.10 When activated this system can reduce sensitivity to various threatening situations which may include pain as a threat.13
Compassion-focused therapy was conceptualised around the need for development of the soothing system in order to allow people to build a tolerance to distressing emotional states.10 The individual’s ability to activate the soothing system may also be equally relevant to the ability to hold and relate to physical pain without becoming overwhelmed and responding in unhelpful ways. This premise would seem to be supported by data14 that indicate that heightened anxiety and long-term stress are associated with higher levels of pain, while positive emotions are associated with lower pain intensity.
This study aimed to (1) explore the engagement of patients attending a routine NHS Pain Clinic with an intervention based on the principles of compassion-focused therapy and (2) report group outcomes on self-reported pain intensity, pain distress, anxiety, depression and pain-related self-efficacy and describe patient-reported changes following the intervention.
Methods
Ethical approval for this exploratory study was granted by the hosting university ethics committee as part of a Master’s dissertation. The local NHS ethics committee advised that the project fell under the remit of service development and did not require additional ethical approval. All participants were fully informed of the study and had opportunity to ask questions of the researcher. All provided written informed consent in order to take part. This was a mixed-methods uncontrolled, unpowered observational study to look for any evidence of promise in the intervention and explore how it would be received by patients.
Conceptual model underpinning intervention
A conceptual Compassion-focused model was empirically developed to inform the intervention15 and is shown in Figure 1. The model proposes that pain can be initially triggered by a range of different factors. If this pain is evaluated as manageable, the individual is likely to have the ability to respond to their own needs. Consistent with the psychological flexibility model described by McCracken and Morley16 in this instance an individual would be likely to continue to engage fully in life while experiencing pain. Alternatively, however, the pain may be evaluated by the individual as potentially overwhelming and met with resistance and attempts at experiential avoidance. In this case it is proposed that the pain, coupled with the response of experiential avoidance, would trigger the threat-based emotional system to become active. The model (Figure 1) allows for various cycles of reinforcement which are described with reference to the three emotional systems and which can potentially be targeted by the practice of mindfulness, loving-kindness exercises and group discussion.
Figure 1.
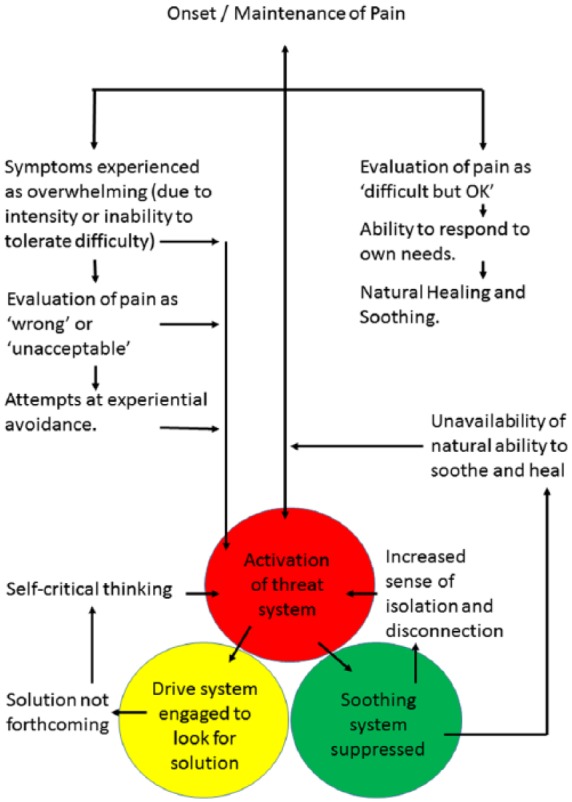
Proposed model of onset and maintenance of persistent pain.
It is proposed that the interactions of the three systems can act as strong maintaining factors for pain which is experienced as overwhelming. The interplay between the three systems may lead to physiological responses that lead to increased symptoms. If this increase is attributed to medical factors, it could further heighten any sense of being ignored by health care professionals who are unable to identify any ongoing physical targets for treatment.
Description of the intervention
The intervention is described in full in the supplemental appendix, but briefly the ResilientMind course is an 8-week group-based course consisting of weekly sessions of 2 hours. The course introduces participants to mindfulness and loving-kindness practices and to discussions of how these can be relevant to the management of long-term pain.
Each session of the ResilientMind course aims to weaken the cycles proposed to maintain pain, through meditation exercises, discussion and psychoeducation. Mindfulness is presented as a method of staying with present moment experience without being pulled into a cycle of resistance that would trigger many of the above patterns.17 Loving-kindness is presented as an accessible way of developing the soothing system which may be relatively under-developed due to the pressures of everyday life or past difficulties.18 Discussions bring to light the shared human experience of some of these patterns, many of which group participants have previously believed to be failings unique to themselves. The compassion-focused principles help guide discussions and help participants to look out for instances of the patterns playing out in their own experience within a safe space. It is emphasised that the patterns described are common human experiences caused by our basic anatomy, not weaknesses, mistakes or examples of personal failure. The framework supports a regular practice, at whatever level is manageable for each individual, of mindfulness and loving-kindness exercises.
Sample selection
Patients were recruited from a single Pain Clinic in the North East of England. Criteria for attending this clinic is the presence of non-malignant pain which has lasted for at least 3 months and for which medical causes either have not been identified or have been previously treated. The study therefore included participants with a range of long-term pain conditions; however, data on these were not recorded for the purpose of this study.
Patients who attended a Consultant appointment within the Pain Clinic and who were assessed as being potentially suitable for multidisciplinary intervention were invited to an education group session. At this point, patients were offered the opportunity to opt in to a standard CBT-based Pain Management Programme, the ResilientMind course (this course) or individual physiotherapy. The sample for this study consisted of all patients who opted to attend the ResilientMind course during the study period and attended at least six out of the eight course sessions. No restriction was placed on patients regarding ongoing routine treatment within the Pain Clinic. Most patients had completed treatment or were on a stabilised regime of medication prior to starting the ResilientMind course.
Study procedures
Completed questionnaires were collected from 58 individuals who attended the ResilientMind course over a period of 12 months. This consisted of a combination of standardised outcome measures and a free-text description of any changes noticed. A control group was unfortunately not feasible within the busy clinical setting within which the project took place. However, baseline data for some of the measures were available from questionnaires that patients had filled in prior to their initial consultation at the pain clinic to provide some level of comparison.
Design
A mixed-methods design was chosen to test for potential improvements on key measures routinely used within Pain Management settings while also exploring participants’ views about changes that they may have experienced as a result of the intervention. It was felt that the qualitative responses would add to the results of the standardised outcome measures by providing a description of participants’ lived experience of this novel intervention and its impact. Qualitative data from the study were analysed in iterative fashion: familiarisation with the data by reading and re-reading it; followed by coding the data into recurrent themes; and then examining the data in theme-by-theme frameworks for the purposes of analysis.
Standardised outcome measures
Outcome measures were completed during the first and last sessions of the group intervention. The majority of patients filled in these questionnaires independently, with a few requesting and receiving help from the clinician delivering the intervention which mainly related to difficulties in manual dexterity or eyesight.
All outcome measures were routinely used within the hosting pain service and have been selected for relevance and ease of administration. The primary outcomes of interest were pain distress and pain intensity which we hypothesised would improve with the intervention. Each of these was measured by a single question using a 0–10 numerical rating scale anchored appropriately at either end. Other validated outcome measures used included the following:
The Patient Health Questionnaire-4 (PHQ-4)19 ultra-short screening instrument for anxiety and depression. It consists of four questions which are scored on a 4-point ordinal scale. The scale is an amalgamation of two screening instruments, the General Health Questionnaire-2 (GHQ-2) for anxiety20 and the Patient Health Questionnaire-2 (PHQ-2) for depression,21 each of which was scored separately. Each scale scores from a minimum of 0 to a maximum of 6, with 6 being the worst.
The Pain Self-Efficacy Scale (PSEQ)22 which consists of 10 questions about how confident people are that they can perform certain activities despite their pain. Each question is rated on a 7-point numerical rating scale from 0 (not at all confident) to 6 (completely confident). Its scores range from a minimum of 0 to maximum of 60, with 0/60 being the worst.
Data processing and analysis
All data were collected by a singular researcher, cross-checked and entered into Excel (version 14). Inputted data were then cross-checked against the original questionnaire responses. Missing data were identified at questionnaire completion stage and in a very small number of cases where this did not occur, the figure from the previous questionnaire that the patient had completed at their initial consultation was used to provide a conservative and straightforward method of data imputation. Social Science Statistics (http://www.socscistatistics.com) was used for all analysis and simple descriptive statistics were used to look at the mean difference pre- and post-intervention. A Cohen’s d effect size23 was calculated to examine the magnitude of change between pre- and post-intervention scores on all outcome measures.
Qualitative reports
In addition to the standardised outcome measures, participants were also asked to use free text to answer the question ‘What changes, if any, have you noticed in yourself as a result of attending this course?’ These data were collected at the final session of the course along with the standardised outcome measures. All 58 participants who attended the intervention provided a response to this free-text question. Analysis took place after all data were collected, thus thematic saturation was not considered in advance. However, no new themes were generated from the responses of the last 16 participants to be considered; therefore, it is likely that data saturation was achieved.
Responses were analysed using an inductive, data-driven thematic analysis as described by Braun and Clarke.24,25 First, the written descriptions from all participants who provided consent were read through twice in order to develop a familiarity with the data. Initial codes were then generated, marked on the text and listed. These codes were then grouped into themes, of which three were apparent within the data. These themes were discussed with a sample of the original study participants who attended a follow-up group session, who agreed that they were a good representation about how they felt they had changed since attending the course.
The qualitative and quantitative data were considered separately until the analysis was complete. At this stage, all data collected were considered as a whole, and efforts made to link participant descriptions of change with the results of the standardised outcome measures.
Results
The intervention was completed in full by 58 out of 83 participants enrolled. Table 1 outlines demographics of patients who were enrolled in the study.
Table 1.
Demographics of study participants.
| Female, n (%) |
Male, n (%) |
|||
|---|---|---|---|---|
| Enrolled | Completed | Enrolled | Completed | |
| 18–25 | 2 | 1 | 0 | 0 |
| 26–65 | 45 | 33 | 12 | 8 |
| 66+ | 16 | 11 | 8 | 5 |
Initially, 63 women and 20 men opted to attend the intervention. A similar proportion of men and women dropped out of the intervention. Of the 25 participants who did not complete the study, 24 stopped attending the course. Reasons given for this were as follows: moved house (1), were unable to continue because of returning to work (2), caring responsibilities (4), other commitments (1), missed final session (5), bereavement (2) and health problems (5). One person made contact to say that they did not wish to continue because the course was not what they had expected and three stopped attending and were lost to follow-up. The majority of those who did not complete the course (19) stopped within the first two sessions. One person declined to take part in the study but still completed the course and their decision did not impact on the intervention offered.
Standardised measures
Outcome measures are reported for each measure in Table 2. Scores at intake were collected on referral to the Pain Clinic and before any treatment. Baseline scores were collected at the first ResilientMind session by which time the medical interventions offered within the Pain Clinic were either completed or stabilised. These data are reported as a point of comparison and were not subject to further analysis. Improvements were seen on each measure with effect sizes which varied from 0.72 (large effect size) on the GHQ-2 to the much more modest effect size of 0.23 (small effect size) on self-reported pain intensity. All changes were in the expected direction.
Table 2.
Mean pre- and post-intervention summary scores of all outcome measures.
| Measure | Intake mean | Pre mean (SD) | Post mean (SD) | ES |
|---|---|---|---|---|
| Intensity | 7.6 | 7.17 (1.82) | 6.61 (2.13) | 0.23 |
| Pain distress | 7.6 | 7.13 (2.26) | 5.87 (2.42) | 0.47 |
| GHQ-2 | No data | 4.07 (1.74) | 2.67 (1.78) | 0.72 |
| PHQ-2 | 3.69 | 3.42 (1.92) | 2.53 (1.69) | 0.46 |
| SES | 23.3 | 21.3 (12.3) | 26.1 (14.46) | 0.36 |
SD: standard deviation; ES: effect size; GHQ-2: General Health Questionnaire-2; PHQ-2: Patient Health Questionnaire-2; SES: Self-Efficacy Scale.
Participants’ reports of pain intensity reduced slightly following the intervention. The effect size was 0.23, indicating a small change.23 Self-reported measures of pain distress showed a greater reduction with an effect size of 0.47. Self-reported anxiety, measured by the GHQ-2, reduced following group participation. Cohen’s effect size for this change was 0.72, indicating a moderate to large effect size. Reductions in self-reported depression were reported with a small to moderate effect size of 0.46. There was an increase in self-efficacy scores pre- to post-intervention (effect size, 0.36), indicating a slight improvement of self-efficacy.
Qualitative reports
After familiarisation with the data, 28 codes were initially defined. The analysis was iterative and led by the data, and no attempt was made to impose a theoretical model on the data. The codes were categorised into three themes, each of which incorporated three subthemes (Figure 2). The first theme was ‘feeling different’. One group participant commented that ‘I don’t feel so guilty about the things I can’t do anymore when my pain is bad. I am starting to realise that it is not just me who experiences these issues, which means that it’s not about me being weak’. The second theme identified was about doing things differently. Most of the participants commented about something that they had started to do differently since attending the course. One person wrote, ‘I always do breathing now to help me through the day, which helps to keep me calm with my day to day anxiety and emotions I’m going through, as I find it hard but this has helped me no end’. The third category was ‘Changed attitude’ with many comments made about becoming kinder and more accepting towards difficulties experienced including pain while acknowledging that they are not to blame for their symptoms. Two out of the 58 participants commented that they were not aware of any changes.
Figure 2.
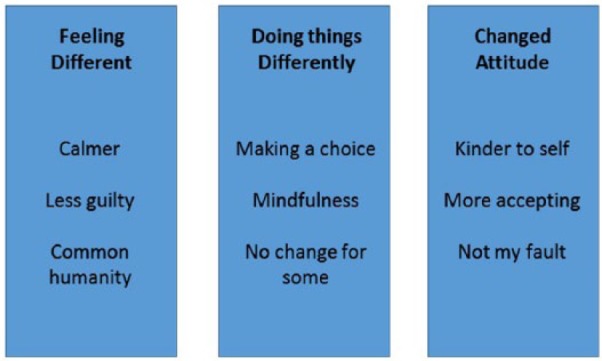
Thematic analysis of free-text responses.
Discussion
This was an exploratory study, which aimed to describe the engagement, outcomes and self-reported changes of patients attending The ResilientMind intervention in order to explore whether the intervention had any promise in the short term and, if so, to establish an effect size which could be used to plan a fully powered trial if appropriate.
This study demonstrated that the intervention has potential for use within a routine Pain Clinic, with reasonable patient engagement and some improvements on measures of pain distress, pain intensity, anxiety and depression which are largely consistent with other reported psychological interventions.4
A sufficient number of patients attended and completed the group to suggest that the intervention is worthy of further study. It is to be noted that patients self-selected into the intervention, as they do with all biopsychosocial interventions within our setting. We feel that this is an important part of collaborative care and that this was an important factor in supporting engagement with the intervention. Within this context, our findings indicate that sufficient patients chose to engage with the intervention to suggest that it is feasible within this setting.
Most participants identified positive changes which they felt had arisen as a result of their attending the intervention. Patients reported changes in the way they did things, and many reported making a positive effort to incorporate some form of the group exercises into daily life. Perhaps because of an increased awareness, many also said that they were choosing to do things in a different way than they would have done before, making choices in a way that could accommodate their actual current needs, rather than being caught up in trying to do what they thought they should be able to do. This is interesting, as activity-based pain management strategies were not covered on the group. It would be helpful in future research to explore how changes in self-efficacy, pain interference and psychological distress might link with behavioural changes such as return to valued activity.
Participants also reported a changed attitude, including a tendency to be more accepting of their pain and limitations and to approach their experiences with a kinder attitude. There was a burgeoning awareness that some of the responses to pain and other difficulties which people had tended to label as ‘just me’ or ‘stupid’ were in fact readily understood in terms of the tricky human brain and shared human experience. Feelings of increased calm and reduced guilt, a willingness to modify expectations in order to accommodate pain and a kinder attitude were reported by many people who attended these sessions.
The results of the standardised outcome measures collected backed up the reports of increased calm, with a significant reduction in anxiety scores on the PHQ-4 and a large effect size. Smaller improvements in depression (0.46), self-efficacy (0.36), pain intensity (0.23) and pain distress (0.47) were recorded, all of which are below Cohen’s description of a medium effect size of 0.5.23 These figures are largely consistent with post-treatment effect sizes reported in a meta-analysis of psychology and multidisciplinary team (MDT)-based group interventions for back pain of 0.35 for depression and 0.50 for pain intensity4 and with reported effect sizes of 0.15 for depression and 0.32 for pain intensity reported in a meta-analysis of mindfulness for pain management intervention.26 It may be helpful for clinicians using compassion-focused interventions within pain management contexts in the future to consider including a measure of anxiety, as this changed the most in this study with a moderate to large effect size of 0.72.
It is interesting that more women than men opted to attend the intervention at a ratio of more than 3:1, with 63 women and only 20 men opting to attend. Possibly an intervention of this nature may appeal more to women than men. In a recent review of mindfulness for pain management,26 the mode percentage of male participants was 15%. No differences were reported in how beneficial the interventions were between female and male participants. A review of psychological and multidisciplinary pain management treatments4 reported that 34% participants were male. Further exploration of gender differences within groups of this nature would be an interesting avenue for further research.
The study demonstrates that a compassion-based conceptualisation may have promise in a pain management context. A major strength of the study is that, having taken place within a routine clinical context, the results have been shown to be achievable in such a context. There were few exclusion criteria, and therefore, unlike research with highly selected populations, the results may be more generalisable to many patients who routinely attend pain management clinics, the majority of whom do have comorbidities. Another strength is that the intervention was based on a theoretical model, an application of compassion-focused therapy, and has provided some initial support for this model within a pain management setting.
Limitations of the study are also related to the clinical context in which it took place. The study was not randomised or controlled and patients were permitted to continue with routine treatments from the Pain Clinic while taking part in this intervention. There is thus no way of knowing which improvements reported were the result of the intervention as opposed to placebo or alternative treatments which may have been ongoing in a few cases. The strategy of replacing missing data with the last available figure is also a weakness which could have had an impact on the outcomes reported. A further weakness was the failure of the intervention to consider in advance the issue of thematic saturation from the qualitative findings.
In addition, the project did not take a long-term view and was therefore unable to determine whether early improvements might be built on and increase with time and continued practice of the exercises or whether they turn out to be short lived. However, the study has reported effect sizes which may be helpful in planning a fully powered study into the intervention including a control group and follow-up data collection.
Limited information was available from participants who started but did not complete the intervention. This would be an important avenue for future research, given both the reported effectiveness4,6 and high attrition rates27 of psychological or multidisciplinary interventions within pain management settings. This intervention had an attrition rate of 30%, which is consistent with the range of attrition rates from pain management programmes reported in the literature.28,29 This potentially weakens confidence in the outcomes reported as analysis on an intention-to-treat basis may yield very different results. There is clearly a lot of scope for improvement in these figures. Further work exploring and addressing the reasons why some people drop out of group-based pain management interventions would be helpful, as would an exploration of different models of service delivery to minimise dropout.
The study supports previous research that suggests that loving-kindness may be a helpful intervention for people with persistent pain.8,9 It builds on this research by conceptualising the intervention within a compassion-focused model which describes potential interactions between the three systems and how these may impact pain.
Conclusion
This study reported on the outcomes of participants of an 8-week course using Mindfulness and Loving-kindness exercises within a routine pain clinic setting and based on a compassion-focused conceptualisation of long-term pain. Early results are promising and indicate that compassion-focused interventions deserve further exploration within the field of pain management. While the study was limited by lack of randomisation and a control group, it seems that a compassion-focused understanding of persistent pain has the potential to add to the current treatment methods available.
Supplemental Material
Supplemental material, Outline_for_ResilientMind_8_week_course_revised_(2) for Exploring a compassion-focused intervention for persistent pain in a group setting by Chris Penlington in British Journal of Pain
Acknowledgments
The author thanks Dr David McMurtry (University of Aberdeen) who supervised this project and Prof. Justin Durham (Newcastle University) for assistance in preparation of the manuscript.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Melzack R, Wall PD. Pain mechanisms: a new theory. Surv Anesthesiol 1967; 11(2): 89–90. [Google Scholar]
- 2. Melzack R. From the gate to the neuromatrix. Pain 1999; 82: S121–S126. [DOI] [PubMed] [Google Scholar]
- 3. Melzack R. Gate control theory: on the evolution of pain concepts. Pain Forum 1996; 5: 128–138. [Google Scholar]
- 4. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007; 26(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 5. Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J Altern Complem Med 2011; 17(1): 83–93. [DOI] [PubMed] [Google Scholar]
- 6. Dixon KE, Keefe FJ, Scipio CD, et al. Psychological interventions for arthritis pain management in adults: a meta-analysis. Health Psychol 2007; 26(3): 241–250. [DOI] [PubMed] [Google Scholar]
- 7. McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. Am Psychol 2014; 69(2): 178. [DOI] [PubMed] [Google Scholar]
- 8. Carson J, Keefe F, Lynch T, et al. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs 2005; 23(3): 287–304. [DOI] [PubMed] [Google Scholar]
- 9. Chapin HL, Darnall BD, Seppala EM, et al. Pilot study of a compassion meditation intervention in chronic pain. J Compassionate Healthc 2014; 1(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gilbert P. Introducing compassion-focused therapy. Adv Psychiat Treat 2009; 15(3): 199–208. [Google Scholar]
- 11. Gilbert P. The compassionate mind. London: Constable & Robinson, 2009. [Google Scholar]
- 12. McEwen BS. Central effects of stress hormones in health and disease: understanding the protective and damaging effects of stress and stress mediators. Eur J Pharmacol 2008; 583(2): 174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Craig A. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol 2003; 13(4): 500–505. [DOI] [PubMed] [Google Scholar]
- 14. Lumley MA, Cohen JL, Borszcz GS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol 2011; 67(9): 942–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Penlington C. An evaluation of the ResilientMind course within a routine pain management setting. MSc Thesis, University of Aberdeen, Aberdeen, 2017. [Google Scholar]
- 16. McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain 2014; 15(3): 221–234. [DOI] [PubMed] [Google Scholar]
- 17. Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985; 8(2): 163–190. [DOI] [PubMed] [Google Scholar]
- 18. Irons C. The science of compassion: evolutionary, neurophysiological and psychological perspectives. J Holist Healthc 2013; 10(3): 10–15. [Google Scholar]
- 19. Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics 2009; 50(6): 613–621. [DOI] [PubMed] [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JB, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007; 146(5): 317–325. [DOI] [PubMed] [Google Scholar]
- 21. Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res 2005; 58(2): 163–171. [DOI] [PubMed] [Google Scholar]
- 22. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain 2007; 11(2): 153–163. [DOI] [PubMed] [Google Scholar]
- 23. Cohen J. A power primer. Psychol Bull 1992; 112(1): 155–159. [DOI] [PubMed] [Google Scholar]
- 24. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3(2): 77–101. [Google Scholar]
- 25. Braun V, Clarke V. What can ‘thematic analysis’ offer health and wellbeing researchers? Int J Qual Stud Health Well-being. Epub ahead of print 16 October 2014. DOI: 10.3402/qhw.v9.26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hilton L, Hempel S, Ewing BA, et al. Systematic review and meta-analysis. Ann Behav Med 2016; 51(2): 199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Turk DC, Rudy TE. Neglected factors in chronic pain treatment outcome studies – referral patterns, failure to enter treatment, and attrition. Pain 1990; 43(1): 7–25. [DOI] [PubMed] [Google Scholar]
- 28. Morley S, Williams A, Hussain S. Estimating the clinical effectiveness of cognitive behavioural therapy in the clinic: evaluation of a CBT informed pain management programme. Pain 2008; 137(3): 670–680. [DOI] [PubMed] [Google Scholar]
- 29. Biller N, Arnstein P, Caudill MA, et al. Predicting completion of a cognitive-behavioral pain management program by initial measures of a chronic pain patient’s readiness for change. Clin J Pain 2000; 16(4): 352–359. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Outline_for_ResilientMind_8_week_course_revised_(2) for Exploring a compassion-focused intervention for persistent pain in a group setting by Chris Penlington in British Journal of Pain


