Abstract
Background
Continuous vector pathogen surveillance is essential for preventing outbreaks of mosquito-borne diseases. Several mosquito species acting as vectors of Japanese encephalitis virus (JEV), dengue virus, Zika virus, malaria parasites and other pathogens are primary mosquito species in Shanghai, China. However, few surveys of human pathogenic arboviruses in mosquitoes in Shanghai have been reported in the last ten years. Therefore, in this study, we evaluated mosquito activity in Shanghai, China during 2016 and tested for the presence of alphaviruses, flaviviruses, orthobunyaviruses and several parasitic pathogens.
Results
Five pooled samples were JEV-positive [4/255 pools of Culex tritaeniorhynchus and 1/256 pools of Cx. pipiens (s.l.)] based on analysis of the NS5 gene. Alphaviruses, orthobunyaviruses, Plasmodium and filariasis were not found in this study. Phylogenetic and molecular analyses revealed that the JEV strains belonged to genotype I. Moreover, newly detected Shanghai JEV strains were genetically close to previously isolated Shandong strains responsible for transmission during the 2013 Japanese encephalitis (JE) outbreak in Shandong Province, China but were more distantly related to other Shanghai strains detected in the early 2000s. The E proteins of the newly detected Shanghai JEV strains differed from that in the live attenuated vaccine SA14-14-2-derived strain at six amino residues: E130 (Ile→Val), E222 (Ala→Ser), E327 (Ser→Thr), E366 (Arg→Ser/Pro), E393 (Asn→Ser) and E433 (Val→Ile). However, no differences were observed in key amino acid sites related to antigenicity. Minimum JEV infection rates were 1.01 and 0.65 per 1000 Cx. tritaeniorhynchus and Cx. pipiens (s.l.), respectively.
Conclusions
Five new Shanghai JEV genotype I strains, detected after a ten-year hiatus in local mosquito surveillance, were genetically close to strains involved in the 2013 Shandong JE outbreak. Because JEV is still circulating, vaccination in children should be extensively and continuously promoted. Moreover, JEV mosquito surveillance programmes should document the genotype variation, intensity and distribution of circulating viruses for use in the development and implementation of disease prevention and control strategies.
Keywords: Japanese encephalitis, Mosquito-borne diseases, Culex tritaeniorhynchus, Culex pipiens, SA14-14-2
Background
Japanese encephalitis virus (JEV) is an arbovirus prevalent throughout Asia and in parts of the western and south Pacific [1, 2]. Similar to other members of the genus Flavivirus, JEV is a single-stranded positive-sense RNA virus with an 11-kb genome encoding three structural (capsid, C; pre-membrane, prM; and envelope, E) and seven nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B and NS5) [3, 4]. Rice paddy-breeding Culex tritaeniorhynchus is the primary JEV vector [1]. In addition, Cx. pipiens [5, 6], Cx. bitaeniorhynchus [5], Cx. modestus [7] and Anopheles sinensis [8] have been shown to transmit JEV in nature. Pigs, wading birds and bats are susceptible reservoirs and act as amplifiers of JEV [9]. Humans, cows and horses are dead-end hosts [10], as they fail to produce viremia at titers sufficient to infect mosquitoes [5]. In nature, JEV is transmitted from vectors to amplifying hosts and then back to vectors, and human outbreaks are the result of spillover effects into the human population [11]. Thus, evaluation of the infection prevalence of JEV in mosquitoes may be important for assessing the risk to public health [12].
An estimated three billion people live in JEV epidemic areas, including China, India and the Southeast Asian peninsula [11]. Approximately 67,900 cases of JEV infection are reported annually [1, 2, 9], although JEV epidemics are highly dynamic [11]. Approximately 50% of cases of JEV infection occur in China [1], potentially because Japanese encephalitis (JE) is a legally notifiable infectious disease in China, whereas effective reporting systems have not been established in most countries with high incidences of JE [6]. In China, JE cases are mainly concentrated in the eastern and southwestern regions, and no local cases have been reported in Xinjiang or Qinghai to date [6]. The principal JEV-susceptible population is children below 15 years of age, and the virus has an incubation period of 5–15 days [13]. Clinically, since the virus can cross the blood brain barrier, JE manifests as a high fever and generalized tonic spasms; thus, in severe cases, irreversible neurologic damage, resulting in consciousness disorders and serious dystonia, may be observed [14, 15].
There is no established treatment for JE [9]. Fortunately, JEV infection is symptomatic in less than 1% of cases [16], and for this reason, JE is often confused with other forms of encephalitis [11]. Thus, the morbidity of JEV is likely to be underestimated [17]. Vaccination programmes, improvements in living standards and sanitation, and the mechanization of agriculture, coincident with economic growth and development, influence the incidence of JE [11]. The most important strategy for preventing JE and reducing the disease burden is increased use of JEV vaccines [16]. In China, the disease burden of JE has declined sharply since the late 1970s, a decade after the introduction of the inactivated vaccine P3 began in economically developed cities, such as Beijing and Shanghai, in 1968 [6]. Subsequently, the vaccine virus strain SA14-14-2 was derived from a wild-type JEV isolated from Cx. p. pallens mosquito larvae in Xi’an, China and licensed in 1988 [18]. Owing to its advantages, such as increased efficacy at a lower dose, fewer side effects, and lower cost [13, 19, 20], the attenuated live vaccine SA14-14-2 is now the main vaccine used in China. Moreover, since 2008, the JEV vaccine has been available free of charge to children 0–15 years-old in China, significantly reducing the spread of JEV [21]. Indeed, only 2178 cases were reported in 2013 [22]. However, the proportion of adult JE cases has increased in Henan, Hebei, Shandong, Shanxi, Shaanxi and Gansu Provinces, located north of the Yangtze River in China [6, 21]. An outbreak of JE in 2013 in Shandong Province, China occurred mainly in adults (73% of 407 cases) [12]. Similar phenomena have been observed in other countries in eastern Asia, including Japan [23] and Korea [24].
Japanese encephalitis virus strains originating from the Indonesia-Malaysia region can be divided into five geographical and epidemiological genotypes based on the E gene, i.e. GV, GIV, GIII, GII and GI (evolutionary order) [25, 26]. The GI genotype can be further divided into two subgenotypes, i.e. GI-a and GI-b. The distribution of GI-a is restricted to Thailand and Cambodia, while GI-b has been the most commonly isolated JEV genotype this century [27]. The prototype JEV strain (known as Nakayama) was isolated in Japan in 1935 and was recognized to be a member of GIII [28]; this genotype was also identified in China (Beijing-1 virus) in 1949 [6]. GIII was the predominant genotype in temporal JEV epidemic regions from 1935 until the 1980s and was then gradually replaced by GI-b thereafter [6, 27, 29]. JEV GI has been isolated in China since 1979 and has expanded rapidly in endemic areas over the past 35 years, whereas JEV strains isolated before the 1970s generally belonged to GIII [26, 30]. The tendency for GI to gradually replace GIII, becoming the dominant JEV genotype, has been observed in many other regions in Asia and reflects its efficiency in replication [27, 31] and superior tolerance to temperature extremes [32]. However, the host range of GI is more restricted than that of GIII, reflected in the fact that there is greater genetic variation in the E gene of GIII than in that of GI [29, 31, 33]. An ancient GV strain was detected in Tibet, China in 2009 [34], 50 years after it was originally identified in a patient in Malaysia in 1952 [35]. Shortly thereafter, another GV isolate was detected in Cx. bitaeniorhynchus in Korea in 2010 [36]. Notably, currently available vaccines do not induce appropriate immune protection against GV [37]. The GIV genotype appears to be confined to the Indonesia-Malaysia region, and the latest isolate was collected in the early 1980s [38]. To date, three JEV genotypes, i.e. GI, GIII and GV, have been isolated in China. In contrast, GII was prevalent in Korea in the 1950s and was associated with a JE outbreak among American soldiers during the Korean War [39]. However, GII quickly died off in temperate Asia and is primary sampled from tropical and subtropical regions, such as Malaysia, Indonesia and north Australia [38, 40].
The spread of JEV in Asia originated from Thailand and the Shanghai, Shandong, Sichuan, Yunnan and Zhejiang Provinces of China [41]. In Shanghai, the first JE outbreak on record occurred in 1965 and speculating that the epidemic period was approximately 15 years in Shanghai prior to the implementation of a vaccine programme [42]. By the end of the last century, total positivity rates of the JE H1 antibody in urban and rural residents reached 88.15 and 87.46%, respectively [43]. In 2016, there were two clinical cases in Shanghai reported via personal communication with officials at the Shanghai City Disease Prevention and Control. This pattern was also observed in Taiwan Province, China, where routine use of the JEV vaccine began in 1968, and the annual JE incidence is currently between 20 and 40 cases [16]. Thus, JEV is expected to remain a public health issue. However, the most recent JEV genotype identified in Shanghai was available publicly in 2007 [30]. Few surveys of human pathogenic arboviruses in mosquitoes, such as JEV and dengue virus, have been reported in Shanghai in the last ten years.
Shanghai is a high-risk area for arbovirus spread because of the abundance of migratory birds, human migration and international travel [11, 44]. Furthermore, Shanghai has a temperate climate, which may increase the JEV disease burden compared with that in tropical and subtropical regions [45]. Although the implementation of vaccination programmes has dramatically decreased the incidence of JE in Shanghai, epidemic outbreaks, such as incidental JE [5, 12, 29] and dengue [46, 47], have occurred in areas near Shanghai. Notably, the spread of arboviruses is accelerating faster than anticipated [48, 49]. In addition to JEV, imported cases or even local outbreaks of emerging mosquito-borne diseases such as Zika [50, 51], chikungunya [52] and West Nile virus (WNV) [53] have been reported successively in China. Moreover, both malaria and lymphatic filariasis were once prevalent in Shanghai [54, 55]. Although lymphatic filariasis has been eliminated [55] and the local transmission of malaria has been effectively controlled in China [56], the numbers and proportions of imported cases of malaria have continued to increase [57, 58]. Therefore, mosquito-borne pathogen surveillance programmes are urgently needed in Shanghai, an international metropolis with important commercial harbors and nature reserves hosting numerous migratory birds. The primary mosquito species in Shanghai are Cx. pipiens (s.l.), Cx. tritaeniorhynchus, Aedes albopictus and An. sinensis [59], which act as vectors for multiple human pathogens [60]. It should be mentioned that the Cx. pipiens complex encompasses three forms (pallens, molestus, quinquefasciatus) and hybrid forms of pallens and quinquefasciatus [61]. The complex is widely distributed in China, with intermediates of Cx. p. pallens and Cx. p. quinquefasciatus found in a zone approximately between 30–32°N [62], within which Shanghai is located. Therefore, Cx. pipiens (s.l.) here represents all forms of the Cx. pipiens complex in Shanghai. It is worth noting that insecticide resistance in mosquito vectors is high in several districts of Shanghai, as for some mosquito vectors that prefer manmade habitats, such as those in irrigated rice fields, larvae are often heavily exposed to pesticide selection pressure [63, 64]. Therefore, in this study, we conducted a survey to determine the presence, genetic variation, geographical distribution and infection rate of JEV and other arboviruses in the area.
Methods
Sampling
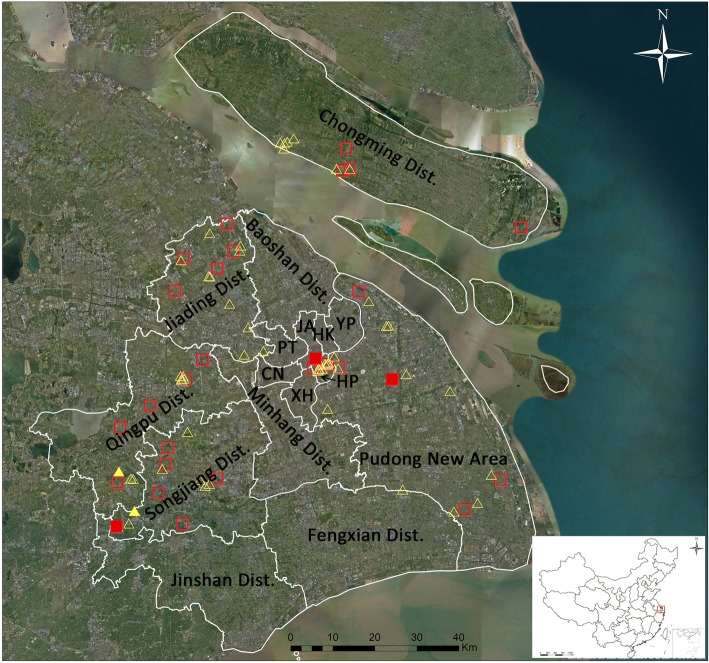
Shanghai is located in the alluvial plain of the Yangtze River Delta, at the mouth of the Changjiang River. In this region, the climate is temperate, which is suitable for mosquito breeding. Arboviral surveillance was carried out from May to November 2016 using CO2-baited traps and the labor hour method. CO2-baited traps were hung from sunset to sunrise for collecting mosquitoes overnight. The labor hour method was used to catch adult mosquitoes in indoor habitats by using a mosquito aspirator for 15 min within 1 h after sunset. Both methods were performed three times per month, i.e. in the first, second, or third week and in the last week of the month. A total of 94 survey sites covering multiple ecological areas from central, subrural, rural and island regions were examined, as shown in Fig. 1. The map was generated using ArcGIS 10.1 ArcMap software (ESRI, Redlands, CA, USA). Mosquitoes were identified using morphological characteristics according to the national key [61], and blood-containing and male mosquitoes were excluded. Mosquitoes containing blood were excluded to prevent contamination with virus contained in a blood meal. Some morphologically ambiguous specimens were evaluated by molecular methods [65]. Since the vector competence of Cx. tritaeniorhynchus, Cx. pipiens (s.l.), Ae. albopictus and An. sinensis in transmitting corresponding mosquito-borne pathogens in China has been confirmed [60, 66], we did not dissect each mosquito to separate the salivary gland from the other tissues, but we instead used the entire individual to analyze the presence of target pathogens. Groups of mosquitoes consisting of 1–50 individuals were pooled by species, collection date, method and location; preserved in 75% ethanol; and stored at -20 °C for further virus direct analysis without isolation.
Fig. 1.
Map of survey sites for the mosquito-borne pathogen surveillance programme in 2016 in Shanghai, China. Squares represent sites using the CO2-baited trap, triangles represent sites using the labor hour method and color-filled symbols represent Japanese encephalitis virus detection. Abbreviations: HP, Huangpu District; XH, Xuhui District; CN, Changning District; JA, Jing’an District; PT, Putuo District; HK, Hongkou District; YP, Yangpu District
Nucleic acid extraction and polymerase chain reaction (PCR)
RNA was extracted from pools of Cx. tritaeniorhynchus, Cx. pipiens (s.l.) and Ae. albopictus as previously described [67], yielding a final product of 50 μl/pool. First-strand cDNA was synthesized by reverse-transcription PCR (RT-PCR) using a Takara PrimeScript RT Reagent Kit with gDNA Eraser (Takara Bio, Shiga, Japan). To assess the integrity of RNA, the mosquito 18S gene was amplified using the RT-PCR products [68]. Flavivirus was amplified with the primer pair PF1S and PF2R-bis, targeting the partial NS5 gene (216 bp) [69]. Primer sets JEV-Ef/JEV-Er [70] and prMF/prMR [30] were used to amplify the 1581-nt E and 674-nt prM genes for further genotype identification. Alphavirus and orthobunyavirus in mosquito samples was amplified by primer sets α6533f/α6999c [71] and BCS82C/BCS332V [72], respectively. PCR products were visualized by 1 or 2% (depending on the length of the amplification fragments) agarose gels with Goldview in 0.5× Tris-acetate-EDTA buffer. Positive products were purified, cloned and sequenced by Sangon (Shanghai, China).
For DNA extraction, ATL (Qiagen, Hilden, Germany) was added to replace the 75% ethanol in pools of An. sinensis. Samples were homogenized in a mixer mill (Jingxin, Shanghai, China), with one 5-mm and one 3-mm steel ball added to each tube. The mixture was incubated at 56 °C overnight in an oscillation thermo-block. The samples were then centrifuged at 1000 rpm for 3 min at room temperature. Next, 200 μl of supernatant from each ground sample was added to the Roche® MagNA Pure 96 sample plate, which was placed into to the MagNA Pure 96 System (Roche, Basel, Switzerland) for automated DNA extraction (MagNA Pure 96 DNA and Viral NA Small Volume Kit) according to the manufacturer’s instructions. The extraction process, based on magnetic glass particles, can extract DNA from 96 pools simultaneously in approximately 1 h. After extraction, DNA was eluted in 50 μl of buffer solution. Nested PCR was carried out to detect the presence of five species of Plasmodium, including P. falciparum, P. vivax, P. malariae, P. ovale and P. knowlesi, as described by Yan et al. [73]. In addition, the SspI DNA repeat sequence of Wuchereria bancrofti [74] and HhaI repeat sequence of Brugia malayi [75] were detected in the DNA products obtained from pools of Cx. pipiens (s.l.)and An. sinensis, respectively.
Phylogenetic analysis
Sequences of PCR products were compared with those deposited in the GenBank database using the BLAST program. The obtained flavivirus sequences were aligned with available sequences of the flavivirus NS5, prM and E genes of JEV retrieved from the GenBank database using ClustalW2 [76] with default settings, which were manually adjusted if necessary. Neighbor-joining (NJ) trees were established following Kimura’s two-parameter (K2P) distance model [77] with 1000 bootstrap replicates using MEGA v.7.0 software [78]. Both intra- and inter-genotype E gene divergences were examined based on our original obtained sequences and those deposited in GenBank using the K2P distance model in MEGA v.7.0. Based on the Akaike information criterion, the best-fit model for the alignment was determined using Modeltest 3.7, in cooperation with PAUP* v.4.0b10 [79]. Consequently, calculation of the maximum likelihood (ML) and Bayesian likelihood trees was completed under the GTR + I + G model for both the NS5 and E genes, whereas the TrN+G model was used for the prM gene. The ML tree was constructed using MEGA v.7.0 software, with 1000 bootstrap replicates. The Bayesian tree was constructed with MrBayes v.3.2.1 [80], run for 10 million generations, with the first 25% of generations discarded as burn-in. The trees were unrooted to provide the least biased topology and visualized using Figtree v.1.4.2 (http://tree.bio.ed.ac.uk/software/figtree/).
Infection rate calculation
Because the sizes of the pools of collected mosquitoes varied considerably, infection rates were calculated by bias-corrected maximum likelihood estimation (MLE) and minimum infection rate (MIR) using the Excel add-in PooledInfRate v.4 statistical software package [81] and expressed as the number of infected mosquitoes per 1000 individuals.
Results
Detection of mosquito-borne pathogens from samples
In total, 21,881 adult mosquitoes belonging to nine species from five genera of the family Culicidae (Culex, Aedes, Anopheles, Mansonia and Coquillettidia) were collected at 94 survey sites (Fig. 1) during the peak mosquito activity period from May to November 2016 in Shanghai. Among them, 10,004 (45.72%) were Cx. tritaeniorhynchus, 4813 (22.00%) were An. sinensis, 3385 (15.47%) were Cx. pipiens (s.l.), 3365 (15.38%) were Ae. albopictus, 150 (0.69%) were Cx. inatomii, 111 (0.51%) were Ae. dorsalis, 32 (0.15%) were Ae. vexans, 20 (0.09%) were Mansonia uniformis and one (0.01%) was Coquillettidia ochracea. The geographical distribution of the survey sites is shown in Fig. 1. Among the collected mosquitoes, sites located on Chongming Island had the highest diversity of mosquito species, particularly sites closest to the Chongming Dongtan National Nature Reserve. For arbovirus detection by RT-PCR, 255 of 655 pools of Cx. tritaeniorhynchus, 256 of 611 pools of Cx. pipiens (s.l.) and 257 of 456 pools of Ae. albopictus were randomly chosen. Moreover, 192 of 362 pools of An. sinensis were randomly chosen for DNA extraction for further parasitic pathogen detection. According to sequence identity and phylogenetic analysis (Fig. 2), five pools were positive for the JEV NS5 gene, including four pools of Cx. tritaeniorhynchus (two pools from Songjiang District, one pool from Huangpu District and one pool from the Pudong New Area) and one of Cx. pipiens (s.l.) (from Qingpu District). The prM and E genes were successfully amplified in three and two of the five JEV-positive pools, respectively. Phylogenetic analyses (Figs. 3, 4) indicated that GI was the only genotype detected among samples collected in Shanghai in 2016. Collection information, host species and GenBank accession numbers are shown in Table 1. No sequences ascribable to the PCR target were obtained using the screening PCR for alphaviral and orthobunyaviral genomes. Moreover, no parasites, including Plasmodium spp., W. bancrofti and B. malayi, were found in this study.
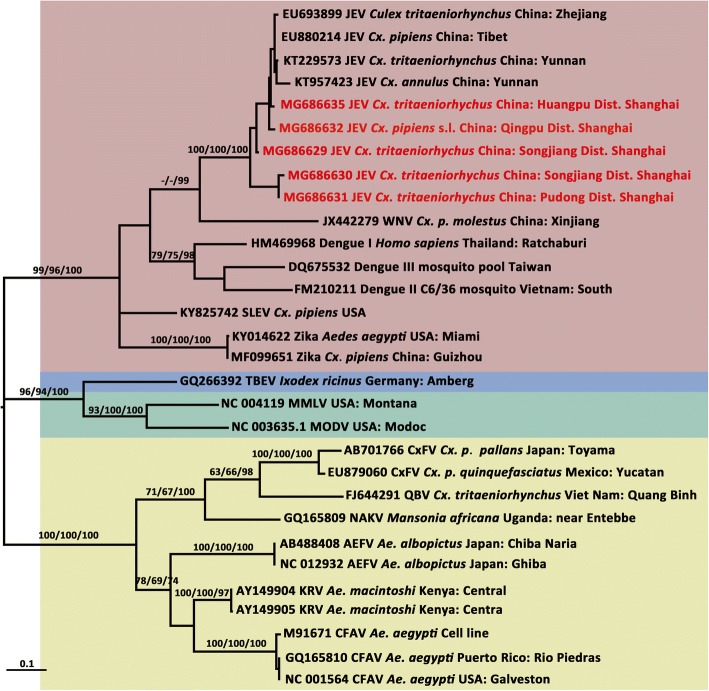
Fig. 2.
Maximum likelihood phylogenetic tree of partial NS5 gene sequences of flavivirus. The maximum likelihood tree was constructed by the GTR + I + G model. The GenBank accession number, virus name, origin, and country/province are noted. The JEV sequences obtained in this study are marked in red. The numbers above each branch represent the bootstrap support for the maximum likelihood, neighbor-joining, and Bayesian analyses, respectively, based on 1000 replicates. The scale-bar indicates 0.1 substitutions per site. Sequences shaded tan represent mosquito-borne flavivirus, those shaded sky blue represent tick-borne flavivirus, those shaded aquamarine represent no-known vector flavivirus, and those shaded khaki represent insect-specific flavivirus. Abbreviations: JEV, Japanese encephalitis virus; SLEV, Santa Louis encephalitis virus; TBEV, tick-borne encephalitis virus; MMLV, Montana myotis leukoencephalitis virus; MODV, Modoc virus; CxFV, Culex flavivirus; QBV, Quang Binh flavivirus; NAKV, Nakiwogo virus; AEFV, Aedes flavivirus; KRV, Kamiti River virus; CFAV, cell fusing agent virus
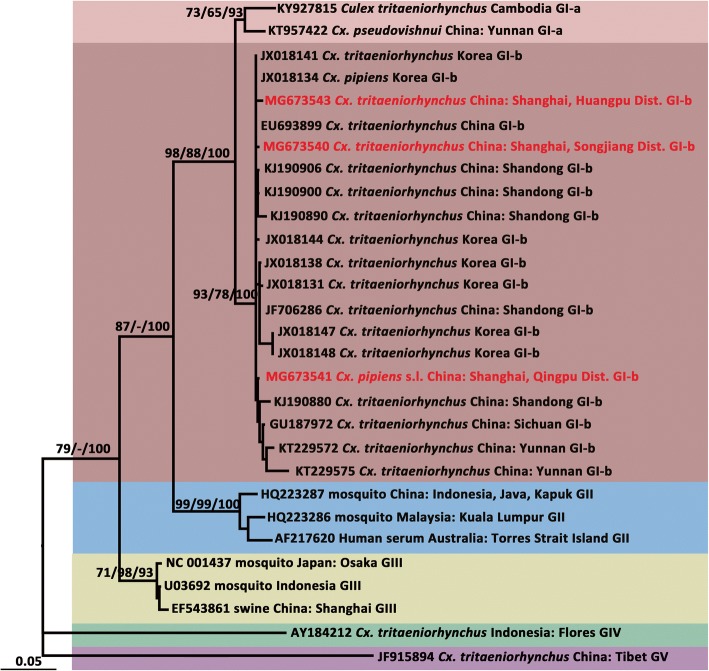
Fig. 3.
Maximum likelihood phylogenetic analysis of Japanese encephalitis virus pre-membrane gene sequences. The maximum likelihood tree was constructed under the TrN + G model. The GenBank accession number, origin, country/province and genotype of each strain are noted. The JEV sequences obtained in this study are marked in red. The numbers above each branch represent the bootstrap support of the maximum likelihood, neighbor-joining, and Bayesian analyses, respectively, based on 1000 replicates. The scale-bar indicates 0.05 substitutions per site. Sequences shaded tan represent the GI-a genotype, those shaded rose-brown represent the GI-b genotype, those shaded sky blue represent the GII genotype, those shaded khaki represent the GIII genotype, those shaded aquamarine represent the GIV genotype, and those shaded thistle represent the GV genotype
Fig. 4.
Maximum likelihood phylogenetic analysis of Japanese encephalitis virus envelope gene sequences. The maximum likelihood tree was constructed under the GTR + I + G model. The GenBank accession number, origin, country/province and genotype of each strain are noted. The JEV sequences obtained in this study are marked in red. The numbers above each branch represent the bootstrap support of the maximum likelihood, neighbor-joining, and Bayesian analyses, respectively, based on 1000 replicates. The scale-bar indicates 0.05 substitutions per site. Sequences shaded tan represent the GI-a genotype, those shaded rose-brown represent the GI-b genotype, those shaded sky blue represent the GII genotype, those shaded khaki represent the GIII genotype, those shaded aquamarine represent the GIV genotype, and those shaded thistle represent the GV genotype
Table 1.
Details of Japanese encephalitis virus strains detected from culicines, captured in Shanghai during May to November 2016
| Strain | Host | Collection date | Geographical location | Habitat | GenBank ID | ||
|---|---|---|---|---|---|---|---|
| NS5 | E | prM | |||||
| PD3G_16-9-S-Cut-R-10-3 | Culex tritaeniorhynchus | 23-Sep-16 | Songjiang District | Livestock farm | MG686629 | MG673540 | |
| PD3H_16-9-S-Cut-C-4-1 | Cx. tritaeniorhynchus | 2-Sep-16 | Songjiang District | Suburb residential area | MG686630 | ||
| PD8F_16-9E-P-Cut-C-2-21 | Cx. tritaeniorhynchus | 2-Sep-16 | Pudong New Area | Suburb residential area | MG686631 | ||
| QP5E_16-7L-Q-Cup-R-4-1 | Cx. pipiens (s.l.) | 24-Jul-16 | Qingpu District | Suburb residential area | MG686632 | MG673536 | MG673541 |
| HP4A_16-7-H-Cut-C-5-2 | Cx. tritaeniorhynchus | 22-Jul-16 | Huangpu District | Urban residential area | MG686635 | MG673537 | MG673543 |
Abbreviations: NS5 non-structural 5 gene, E envelope gene, prM pre-membrane gene
Molecular characterization and phylogenetic analysis based on the prM and E genes of JEV
The phylogenetic tree based on the NS5 gene (Fig. 2) showed that the genus of Flavivirus contains four distinguishable clusters, including mosquito-borne flavivirus, tick-borne flavivirus, no-known vector flavivirus and insect-specific flavivirus. All five JEV-positive sequences (MG686629, MG686630, MG686631, MG686632 and MG686635) clustered within the JEV clade. WNV, spread by Culex, was found to be genetically close to JEV.
The topologies of the trees produced from the JEV prM (Fig. 3) and E genes (Fig. 4) identified five major clades, including genotypes I, II, III, IV and V. Moreover, GI was composed of two distinct clades, representing the two sub-genotypes, GI-a and GI-b. Based on the supporting values of the three phylogenetic trees (Figs. 3, 4), for the majority of lineages, the Bayesian method returned relatively higher bootstrap values than the ML and NJ methods. The prM (650 nt) tree showed some lower bootstrap values but displayed a topology consistent with that obtained with the E gene sequence (1500 nt).
The sequences of the JEV prM gene from the Songjiang (PD3G_16-9-S-Cut-R-10-3, MG673540), Qingpu (QP5E_16-7L-Q-Cup-R-4-1, MG673541) and Huangpu (HP4A_16-7-H-Cut-C-5-2, MG673543) strains showed high levels of identity with each other at the nucleotide (range: 99.08–99.38%) and amino acid (range: 99.34–100%) levels, but lower homology to the SA14-14-2 strain (89.09–89.40% at the nucleotide level and 96.05–97.71% at the amino acid level). In the phylogenetic tree based on the prM gene (Fig. 3), the Qingpu, Huangpu and Songjiang strains formed a cluster with other GI-b sequences. The Huangpu and Songjiang strains were genetically similar but were relative more distantly related to the Qingpu strain, which was detected in Cx. pipiens (s.l.).
According to sequence homology analyses based on the E gene, the Qingpu strain (MG673536) shared 87.99% nucleotide identity and 97.00% amino acid identity with that of the live attenuated vaccine SA14-14-2, while the Huangpu strain (MG673537) shared 87.58% nucleotide and 96.60% amino acid identity with SA14-14-2. As expected, 99.00% similarity was observed between the Qingpu and Huangpu strains, both at the nucleotide and amino acid levels. In the phylogenetic tree based on the E gene (Fig. 4), these strains fell into the GI-b cluster and were most closely related to the Shandong strains, which were suspected to have contributed to the JE outbreak in Shandong Province, China in 2013 [12]; however, they were more distantly related to previously detected local strains, including the SH101 (AY555761, in 2001) and SH05-24 strains (DQ404108, in 2005), both isolated from Cx. tritaeniorhynchus.
Deduced amino acid differences in E protein sequences were aligned for comparison among Huangpu and Qingpu strains, strains involved in JE outbreaks, and SA and vaccine strains currently used in China (Fig. 5). Six amino acid residues in the newly detected Shanghai JEV strains differed from those in the live attenuated vaccine SA14-14-2-derived strain (SA14): E130 (Ile→Val), E222 (Ala→Ser), E327 (Gly→Glu), E366 (Arg→Ser/Pro), E393 (Asn→Ser) and E433 (Val→Ile).
Fig. 5.
Sequence comparison of amino acid differences in the envelope protein of Japanese encephalitis virus (JEV). Sequence comparisons were performed among the live attenuated vaccine SA14-14-2, SA14, and newly detected Shanghai JEV strains (marked in red), as well as strains suspected to have contributed to prior Japanese encephalitis outbreaks (2013 in Shandong Province, China; 2010 in Korea; and 2006 in Wuhan Province, China) near Shanghai. Dots indicate consensus. The GenBank accession numbers and countries/provinces are noted. Triangles represent eight amino acids (F107L, K138E, V176I, A177T, H264Q, M279K, V315A, and R439K) related to virus attenuation; circles represent two pairs of co-evolving sites (residues S89N to F360Y and M129T to I141V) observed in GI; squares represent four sites (E123, E209, E327, and E408) in the E protein used for haplotype definitions; stars represent the amino acids (I130V, A222S, S327T, R366S/P, N393S, and V433I) of newly detected Shanghai JEV strains that were not consistent with those in the SA14 strain
Genetic distance analyses of the E gene based on 69 sequences from GenBank and the two obtained here (GenBank accession numbers available in Fig. 4) showed that the average K2P distances within and between JEV genotypes were 0.032 (range: 0.018–0.039) and 0.202 (range: 0.109–0.272), respectively (Fig. 6). On average, the differences between genotypes were 6-fold higher than those within genotypes. The maximum K2P distance within genotypes was observed in GIII (0.039), and the minimum K2P distance between JEV genotypes was 0.109. Thus, the genetic distances among JEV genotypes ranged from 0.039 to 0.109.
Fig. 6.
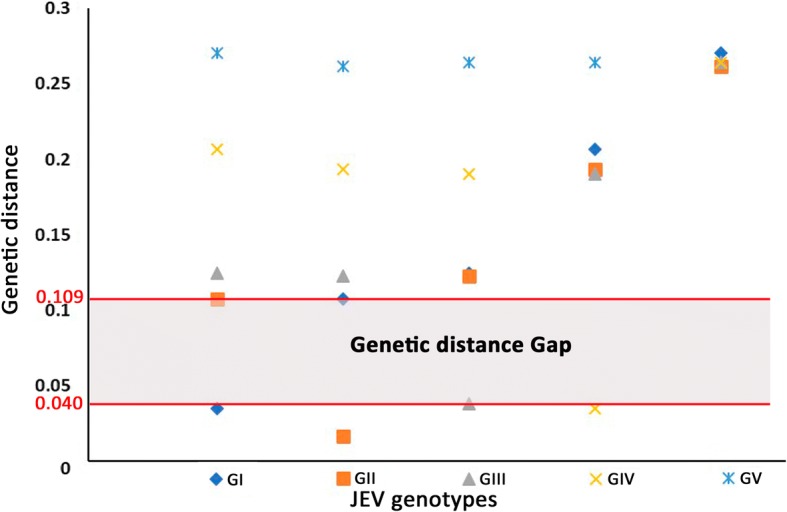
Genetic distances of the envelope genes from five genotypes of Japanese encephalitis virus (JEV). Genetic distance analyses were performed using Kimura’s two-parameter model based on 69 JEV envelope sequences from GenBank and two sequences obtained in this study. The GenBank accession numbers of involved sequences are available in Fig. 4. Y-axis, genetic divergence; X-axis, JEV genotypes
Infection rate of JEV in culicines
The infection rate (Table 2) according to bias-corrected MLE and MIR of JEV in Cx. tritaeniorhynchus, both with 95% confidence intervals (CI), were 1.01 (0.33–2.42) and 1.01 (0.02–2.01) per 1000, respectively. Those of JEV in Cx. pipiens (s.l.) were 1.01 (0.00–1.92) and 0.65 (0.04–3.14) per 1000, respectively. The overall bias-corrected MLE infection rates and MIR of JEV in culicines were 0.91 (0.34–2.01) and 0.91 (0.11–1.71) per 1000 vectors, respectively. Four out of five positive pools originated from residential areas; three were collected in suburbs, whereas one was collected in the central city region (Huangpu District). The remaining pool was collected from a livestock farm.
Table 2.
Bias-corrected maximum likelihood estimation (MLE) and minimum infection rate (MIR) of Japanese encephalitis virus in Shanghai, China from May to November 2016
| Host | No. of individuals | No. of PP | No. of pools | Positive pool rate (%) | MLE (95% CI) | MIR (95% CI) |
|---|---|---|---|---|---|---|
| Culex tritaeniorhynchus | 3945 | 4 | 255 | 1.57 | 1.01 (0.33–2.42) | 1.01 (0.02–2.01) |
| Cx. pipiens (s.l.) | 1540 | 1 | 256 | 0.39 | 1.01 (0.00–1.92) | 0.65 (0.04–3.14) |
| Overall | 5485 | 5 | 511 | 0.98 | 0.91 (0.34–2.01) | 0.91 (0.11–1.71) |
Abbreviations: PP positive pool, CI confidence interval
Discussion
Historical co-circulation of JEV GI and GIII strains in Shanghai
The first JEV strain found in Shanghai was isolated from a human brain in 1987 and classified as the GIII genotype [30]. In contrast, GI was first detected from Cx. tritaeniorhynchus in Shanghai in 2001 [82]. GI and GIII were found alternately between 2003 and 2008, suggesting that these two genotypes co-circulated in this area, although they were never identified in the same year [30]. Thereafter, JEV mosquito surveillance and arbovirus detection in mosquitoes have seldom been carried out in Shanghai. To the best of our knowledge, no data on JEV genotypes has been reported within the last ten years. However, although the implementation of vaccination programmes has dramatically decreased the incidence of JE in Shanghai, JEV will probably continue to circulate in nature based on the existence of annual JE cases.
A single genotype (GI) has been detected in Shanghai after a ten-year hiatus in JEV mosquito surveillance
In this study, we carried out mosquito-borne surveillance from May to November 2016. The predominant species of mosquitoes collected were Cx. tritaeniorhynchus, Cx. pipiens (s.l.), Ae. albopictus and An. sinensis. Here, Cx. tritaeniorhynchus yielded the majority of JEV-positive pools, indicating that Cx. tritaeniorhynchus is the primary vector of JEV, whereas Cx. pipiens (s.l.) may play some role in JEV circulation in Shanghai. GI was previously thought to be almost exclusively restricted to Cx. tritaeniorhynchus [33]. However, in this study, this genotype was also detected in Cx. pipiens (s.l.). This is the first record of JEV being detected in Cx. pipiens (s.l.) in Shanghai. Cx. pipiens (s.l.) and is found mostly in small waste water reservoirs surrounding houses in urban areas in which drainage and sanitation are inadequate, whereas Cx. tritaeniorhynchus is mainly distributed in rural and sub-rural areas. Thus, the JEV transmitted by Cx. pipiens (s.l.) may be more harmful to public health.
In this study, a single genotype of JEV (GI) was detected in Shanghai, which is not surprising given that GIII has not been detected in some areas of Asia for several years. In Korea, GIII was not isolated from 1995 to 2010, although both GI and GIII were detected in Korea in 1994 [5]. Additionally, mosquito pathogen detection results have suggested that only JEV GI strains were involved in the 2010 outbreak [5]. Even in Vietnam, GI was the only JEV genotype detected after 2004 [83, 84]. Furthermore, a low genetic diversity (99.00% identity at both the nucleotide and amino acid levels) of the E gene was observed between newly detected Shanghai JEV strains, suggesting that frequent JEV transmission occurs in local areas. However, these strains are genetically distant from a previously detected Shanghai strain (SH101 strain in 2001, AY555761) according to E gene sequences, sharing only 87.3% and 96.6% identity at the nucleotide and amino acid levels, respectively. These findings suggest that the haplotype of GI circulating in local areas has changed, likely via mutation or introduction from northeastern areas of Asia, such as Shandong Province or Korea, as implied by the close genetic relationships among these strains.
Sequence comparison with strains involved in JE outbreaks and vaccine strain currently used in China
Both the inactivated P3 vaccine and the live attenuated SA14-14-2 vaccine are derived from GIII strains [6]. The vaccines appear to be effective against four genotypes (GI–GIV) of the virus [9, 16, 19]. In case-control studies in Sichuan Province, China, a single dose of the live attenuated SA14-14-2 vaccine was found to be 80% effective (95% CI: 44–93%), whereas administration of two doses increased the efficacy to 97.5% (95% CI: 86–99.6%) [85]. The effectiveness of a single dose of the SA14-14-2 vaccine varied with regard to the duration of protection, the chance of exposure to wild JEV, and sampling bias [86, 87].
In contrast, a recent study showed that the vaccine SA14-14-2 failed to induce appropriate immune protection against GV [37]. According to sequence homology analyses of the E protein, the recurrent genotype GV (JF915894) was found to have a significantly low identity (79.30%) with the live attenuated vaccine SA14-14-2 at the amino acid level. The E protein is the major constituent of the mature virion surface and is under continuous selection pressure owing to its roles in infectivity and immunity processes, including hemagglutination, virus neutralization and viral particle assembly [6, 27]. The E gene has been shown to provide reliable information reflecting the broad geographical and temporal relationships of JEV [32]. Additionally, a small number of mutations in the E amino acid sequence have been shown to be associated with host adaptation and influence the efficiency of mosquito oral infectivity [25]. Eight amino acids (F107L, K138E, V176I, A177T, H264Q, M279K, V315A and R439K) are related to virus attenuation, and residue E138 is particularly important in this process [18]. The co-evolution of two pairs of sites (residues S89N to F360Y and M129T to I141V) was observed in GI, in which these residues functionally interact with each other to maintain a functional E protein [27]. Moreover, 12 haplotypes were defined based on the four sites in the E protein (E123, E209, E227 and E408) predicted to be under positive selection, with SKSS as the predominant haplotype [33]. Thus, we compared the amino acid residues of the live attenuated vaccine SA14-14-2 with the SA14, Qingpu and Huangpu strains, as well as strains involved in recent JE outbreaks [5, 12, 88] near Shanghai. However, there were no corresponding mutations at the E107, E138, E176, E177, E264, E279, E315 or E439 loci. Although mutations in residue 129 occurred in wild JEV strains compared with the SA14 strain sequence, no corresponding paired mutations were identified in E141. All of the observed JEV strains carried the dominant haplotype, SKSS. Notably however, six amino acid residues (I130V, A222S, S327T, R366S/P, N393S and V433I) in the newly detected Shanghai JEV strains differed from the vaccine-derived strain. Thus, continuous surveillance of JEV should be sustained to better understand the genetic characteristics of circulating JEV and to avoid potential breakthrough infection (after vaccination), caused by amino acid mutation at key loci related to antigenicity. Additionally, it has been reported that GI has rarely been isolated from human serum and replicates much more effectively in mosquito and porcine cell lines than in human cell lines, as compared with the performance of GIII [31]. However, all cases of JEV in the last ten years in most parts of Asia have been due to GI [5, 12, 29, 88, 89]. This indicates that GI strains may have evolved to be more effective at infecting humans or are the result of genotype shift in vectors and amplifying hosts. These findings raise concerns regarding potential changes in the epidemiological characteristics of the virus and the effectiveness of vaccines [29]. In addition, the development of novel vaccines is necessary to prevent the recurrence of GV in Asia.
Extensive promotion of vaccinations and sustained JEV mosquito surveillance are crucial for JE prevention and control in China
Since 2010, the annual number of JEV cases in China has decreased to approximately 2000 [22]. However, JE is still prevalent in Yunnan, Guizhou and Guangxi Provinces, particularly in very remote areas where the administration of JEV vaccinations is not as common [6]. Moreover, in these rural areas, livestock may shed viruses near humans, and breeding habitats, such as paddy fields, may be nearby. These conditions facilitate JEV circulation and amplification, resulting in spillover of the virus into the human population and triggering epidemics. Accordingly, these findings suggest that all domestic pigs should be moved to communal piggeries several kilometers away from the homes of humans in order to reduce the risk of JEV transmission to humans [10]. However, the most effective approach for controlling JEV is thought to be full coverage vaccination of susceptible populations (i.e. children ages 0–15 years) [9]. It is also possible that JE outbreaks may occur in some areas of eastern and middle Asia, where the incidence of JE has been reduced to low levels for several years while JEV continues to circulate in the field, as has been observed for the recurrence of JEV epidemics in Wuhan Province [88]. Thus, areas with a few or no reported JE cases but historical epidemics should be subjected to periodic vector surveillance to monitor the dynamics of JEV prevalence in local areas. More importantly, it is necessary to implement immunization programmes for children in these areas. Additionally, emergency vaccination should be conducted in adults with no history of JEV vaccination during JE outbreaks or when the local JEV infection rate in vectors reaches the level of an epidemic [21].
The infection rate of JEV in Shanghai was found to be 1.01 per 1000 Cx. tritaeniorhynchus. The actual infection rate in the field is probably underestimated because samples in the present study were directly tested by RT-PCR, without virus amplification or isolation, since the mosquitoes were preserved in 75% ethanol. Compared with those during JE outbreaks in Shandong Province, China [12] and Korea [5], which averaged 9.1 and 11.8 per 1000 vectors, respectively, the infection rate of JEV in Shanghai in 2016 was ten times lower. However, the infectious prevalence of flavivirus, e.g. WNV (data unavailable for JEV), that represents an “epidemic risk” is more than 5 per 1000 mosquitoes [12]. Thus, the infection rate of JEV in Shanghai derived here is on the same order of magnitude as the epidemic risk of WNV, indicating that it is crucial to promote continuous mosquito-borne virus surveillance in Shanghai.
Conclusions
In summary, our findings showed that four out of five JEV-positive pools were collected from residential areas, suggesting an increased risk of human infection in Shanghai. Thus, it is necessary to promote continuous, full coverage vaccination in children, supplemented with surveillance of the virus carrier rate of mosquito vectors. Our results also highlight the importance of documenting the genotype distributions and genetic variations in JEV over time in order to establish strategies for the control of mosquitoes and mosquito-borne diseases. Further studies are also needed to evaluate the potential of pigs to act as reservoirs and to determine the role of bird migration in JEV spread.
Acknowledgements
The authors thank the staff of the Centers for Disease Control and Prevention of Songjiang District, Chongming District, Qingpu District, Huangpu District, Jiading District, and Pudong New Area, Shanghai, China for their assistance in carrying out field work.
Funding
This work was supported by the National Key Research and Development Programme of China (grant nos. 2016YFC1202000, 2016YFC1202002, 2016YFC1202003).
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The newly generated sequences were submitted to the GenBank database under the accession numbers MG686629-MG686637, MG686640, MG686641 and MG686643.
Abbreviations
- CI
Confidence interval
- E gene
Envelope gene
- JE
Japanese encephalitis
- JEV
Japanese encephalitis virus
- K2P
Kimura’s 2-parameter
- MIR
Minimum infection rate
- ML
Maximum likelihood
- MLE
Maximal likelihood estimation
- NJ
Neighbor-joining
- NS5 gene
Nonstructural5 gene
- prM gene
Pre-membrane gene
- WNV
West Nile virus
Authors’ contributions
YF, YZ, ZZ, SX, WS, JX, YL and JW designed the study. YF, ZZ, WS and JW conducted the field collections. YF, ZZ, SX, JX, YL and JW carried out laboratory experiments and performed phylogenetic analyses. YF wrote the original manuscript and SX, JX, YL and YZ revised the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Mosquito surveillance was conducted within the jurisdictions of the Centers for Disease Control and Prevention of Songjiang District, Chongming District, Qingpu District, Huangpu District, Jiading District, and Pudong New Area, Shanghai, China respective governance domain by routine mosquito surveillance. Sample collections made on private land or in private residences were conducted after acquisition of permission from the landowners or residents. The study did not involve endangered or protected species.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yuan Fang, Email: fangyuan@nipd.chinacdc.cn.
Yi Zhang, Email: zhang1972003@163.com.
Zheng-Bin Zhou, Email: zhouzb@nipd.chinacdc.cn.
Shang Xia, Email: xiashang@nipd.chinacdc.cn.
Wen-Qi Shi, Email: shiwq@nipd.chinacdc.cn.
Jing-Bo Xue, Email: xuejb@nipd.chinacdc.cn.
Yuan-Yuan Li, Email: liyy@nipd.chinacdc.cn.
Jia-Tong Wu, Email: wujt@nipd.chinacdc.cn.
References
- 1.Campbell GL, Hills SL, Fischer M, Jacobson J, Hoke CH, Hombach J, et al. Estimated global incidence of Japanese encephalitis: a systematic review. B World Health Organ. 2011;89:766–774. doi: 10.2471/BLT.10.085233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Centers for Disease Control and Prevention Japanese encephalitis surveillance and immunization - Asia and the Western Pacific, 2012. Morb Mortal Wkly Rep. 2013;62:658–662. [PMC free article] [PubMed] [Google Scholar]
- 3.Lindenbach BD, Rice CM. Molecular biology of flaviviruses. Adv Virus Res. 2003;59:23–61. doi: 10.1016/S0065-3527(03)59002-9. [DOI] [PubMed] [Google Scholar]
- 4.Kuno G, Chang GJ, Tsuchiya KR, Karabatsos N, Cropp CB. Phylogeny of the genus Flavivirus. J Virol. 1998;72:73–83. doi: 10.1128/jvi.72.1.73-83.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seo HJ, Kim HC, Klein TA, Ramey AM, Lee JH, Kyung SG, et al. Molecular detection and genotyping of Japanese encephalitis virus in mosquitoes during a 2010 outbreak in the Republic of Korea. PLoS One. 2013;8:e55165. doi: 10.1371/journal.pone.0055165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng Y, Li M, Wang H, Liang G. Japanese encephalitis and Japanese encephalitis virus in mainland China. Rev Med Virol. 2012;22:301–322. doi: 10.1002/rmv.1710. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Fu S, Wang H, Mao X, Liu W, He Y, et al. Isolation and identification of Japanese encephalitis virus in Liaoning Province. Chin J Exp Clin Virol. 2006;20:61–65. [PubMed] [Google Scholar]
- 8.Gong D, Guo X, Zhou H, Wang P. Investigation of the prevalence of Japanese encephalitis in Jingdong County. Yunnan. Chin J Pathol Bio. 2010;5:57–58. [Google Scholar]
- 9.Solomon T. Control of Japanese encephalitis - within our grasp? N Engl J Med. 2006;355:869–871. doi: 10.1056/NEJMp058263. [DOI] [PubMed] [Google Scholar]
- 10.Johansen CA, van den Hurk AF, Pyke AT, Zborowski P, Phillips DA, Mackenzie JS, et al. Entomological investigations of an outbreak of Japanese encephalitis virus in the Torres Strait, Australia, in 1998. J Med Entomol. 2001;38:581–588. doi: 10.1603/0022-2585-38.4.581. [DOI] [PubMed] [Google Scholar]
- 11.Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emerg Infect Dis. 2009;15:1–7. doi: 10.3201/eid1501.080311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tao Z, Liu G, Wang M, Wang H, Lin X, Song L, et al. Molecular epidemiology of Japanese encephalitis virus in mosquitoes during an outbreak in China, 2013. Sci Rep. 2014;4:4908. doi: 10.1038/srep04908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar R. Prevention, diagnosis, and management of Japanese encephalitis in children. Pediatric Health Med Ther. 2014;5:99–110. doi: 10.2147/PHMT.S49049. [DOI] [Google Scholar]
- 14.Kumar R, Tripathi P, Singh S, Bannerji G. Clinical features in children hospitalized during the 2005 epidemic of Japanese encephalitis in Uttar Pradesh, India. Clin Infect Dis. 2006;43:123–131. doi: 10.1086/505121. [DOI] [PubMed] [Google Scholar]
- 15.Yin Z, Wang H, Yang J, Luo H, Li Y, Hadler SC, et al. Japanese encephalitis disease burden and clinical features of Japanese encephalitis in four cities in the People’s Republic of China. Am J Trop Med Hyg. 2010;83:766–73. [DOI] [PMC free article] [PubMed]
- 16.Chen H, Chang J, Tang R. Current recommendations for the Japanese encephalitis vaccine. J Chin Med Assoc. 2015;78:271–275. doi: 10.1016/j.jcma.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Batchelor P, Petersen K. Japanese encephalitis: a review of clinical guidelines and vaccine availability in Asia. Trop Dis Travel Med Vaccines. 2015;1:11. doi: 10.1186/s40794-015-0013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu Y. Phenotypic and genotypic characteristics of Japanese encephalitis attenuated live vaccine virus SA14-14-2 and their stabilities. Vaccine. 2010;28:3635–3641. doi: 10.1016/j.vaccine.2010.02.105. [DOI] [PubMed] [Google Scholar]
- 19.Liu X, Yu Y, Li M, Liang G, Wang H, Jia L, et al. Study on the protective efficacy of SA14-14-2 attenuated Japanese encephalitis against different JE virus isolates circulating in China. Vaccine. 2011;29:2127–2130. doi: 10.1016/j.vaccine.2010.12.108. [DOI] [PubMed] [Google Scholar]
- 20.McArthur MA, Holbrook MR. Japanese encephalitis vaccines. J Bioterror Biodef. 2011;S1:2. doi: 10.4172/2157-2526.S1-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X, Cui S, Gao X, Wang H, Song M, Li M, et al. The spatio-temporal distribution of Japanese encephalitis cases in different age groups in mainland China, 2004–2014. PLoS Negl Trop Dis. 2016;10:e0004611. doi: 10.1371/journal.pntd.0004611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu D, Ning G, Yin Z, Li J, Li Y. Epidemiological characteristics of Japanese encephalitis in China, 2011–2013. Chin J Vaccines Immun. 2015;21:486–490. [Google Scholar]
- 23.Konishi E, Kitai Y, Tabei Y, Nishimura K, Harada S. Natural Japanese encephalitis virus infection among humans in west and east Japan shows the need to continue a vaccination program. Vaccine. 2010;28:2664–2670. doi: 10.1016/j.vaccine.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 24.Lee D-W, Choe YJ, Kim JH, Song KM, Cho H, Bae G-R, et al. Epidemiology of Japanese encephalitis in South Korea, 2007–2010. Int J Infect Dis. 2012;16:e448–e452. doi: 10.1016/j.ijid.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Solomon T, Ni H, Beasley DWC, Ekkelenkamp M, Cardosa M, Barrett AD. Origin and evolution of Japanese encephalitis virus in southeast Asia. J Virol. 2003;77:3091–3098. doi: 10.1128/JVI.77.5.3091-3098.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan X, Liu H, Wang H, Fu S, Liu H, Zhang H, et al. Emergence of genotype I of Japanese encephalitis virus as the dominant genotype in Asia. J Virol. 2011;85:9847–9853. doi: 10.1128/JVI.00825-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schuh AJ, Ward MJ, Brown AJL, Barrett ADT. Dynamics of the emergence and establishment of a newly dominant genotype of Japanese encephalitis virus throughout Asia. J Virol. 2014;88:4522–4532. doi: 10.1128/JVI.02686-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewis L, Taylor HG, Sorem MB, Norcross JW, Kindsvatter VH. Japanese B encephalitis: clinical observations in an outbreak on okinawa shima. Arch Neurol Psychiatry. 1947;57:430–463. doi: 10.1001/archneurpsyc.1947.02300270048004. [DOI] [PubMed] [Google Scholar]
- 29.Pan J, Yan J, Zhou J, Tang X, He H, Xie R, et al. Sero-molecular epidemiology of Japanese encephalitis in Zhejiang, an eastern province of China. PLoS Negl Trop Dis. 2016;10:e0004936. doi: 10.1371/journal.pntd.0004936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang H, Takasaki T, Fu S, Sun X, Zhang H, Wang Z, et al. Molecular epidemiological analysis of Japanese encephalitis virus in China. J Gen Virol. 2007;88:885–894. doi: 10.1099/vir.0.82185-0. [DOI] [PubMed] [Google Scholar]
- 31.Do LP, Bui TM, Phan NT. Mechanism of Japanese encephalitis virus genotypes replacement based on human, porcine and mosquito-originated cell lines model. Asian Pac J Trop Med. 2016;9:333–336. doi: 10.1016/j.apjtm.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 32.Schuh AJ, Ward MJ, Brown AJ, Barrett AD. Phylogeography of Japanese encephalitis virus: genotype is associated with climate. PLoS Negl Trop Dis. 2013;7:e2411. doi: 10.1371/journal.pntd.0002411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Han N, Adams J, Chen P, Guo Z, Zhong X, Fang W, et al. Comparison of genotypes I and III in Japanese encephalitis virus reveals distinct differences in their genetic and host diversity. J Virol. 2014;88:11469–11479. doi: 10.1128/JVI.02050-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li M, Fu S, Chen W, Wang H, Guo Y, Liu Q, et al. Genotype V Japanese encephalitis virus is emerging. PLoS Negl Trop Dis. 2011;5:e1231. doi: 10.1371/journal.pntd.0001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hale JH, Lim KA, Chee PH. Japanese type B encephalitis in Malaya. Ann Trop Med Parasit. 1952;46:220–226. doi: 10.1080/00034983.1952.11685526. [DOI] [PubMed] [Google Scholar]
- 36.Takhampunya R, Kim HC, Tippayachai B, Kengluecha A, Klein TA, Lee WJ, et al. Emergence of Japanese encephalitis virus genotype V in the Republic of Korea. Virol J. 2011;8:449. doi: 10.1186/1743-422X-8-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cao L, Fu S, Gao X, Li M, Cui S, Li X, et al. Low protective efficacy of the current Japanese encephalitis vaccine against the emerging genotype 5 Japanese encephalitis virus. PLoS Negl Trop Dis. 2016;10:e0004686. doi: 10.1371/journal.pntd.0004686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schuh AJ, Guzman H, Tesh RB, Barrett ADT. Genetic diversity of Japanese encephalitis virus isolates obtained from the Indonesian archipelago between 1974 and 1987. Vector Borne Zoonotic Dis. 2013;13:479–488. doi: 10.1089/vbz.2011.0870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schuh AJ, Li L, Tesh RB, Innis BL, Barrett ADT. Genetic characterization of early isolates of Japanese encephalitis virus: genotype II has been circulating since at least 1951. J Gen Virol. 2010;91:95–102. doi: 10.1099/vir.0.013631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams DT, Wang LF, Daniels PW, Mackenzie JS. Molecular characterization of the first Australian isolate of Japanese encephalitis virus, the FU strain. J Gen Virol. 2000;81:2471–2480. doi: 10.1099/0022-1317-81-10-2471. [DOI] [PubMed] [Google Scholar]
- 41.Gao X, Zhou H, Liu H, Fu S, Wang H, Guo Z, et al. Study on spatial dispersal and migration events of Japanese encephalitis virus. Chin J Virol. 2015;31:264–268. [PubMed] [Google Scholar]
- 42.Ding D, Kilgore PE, Clemens JD, Liu W, Xu Z. Cost-effectiveness of routine immunization to control Japanese encephalitis in Shanghai, China. B World Health Organ. 2003;81:334–342. [PMC free article] [PubMed] [Google Scholar]
- 43.Shen B, Ding D, Xu R-F, Shen B-H, Liu Y, Xu D-L, et al. Sero-epidemiological survey of Japanese encephalitis in residents of Shanghai. Chin J Vaccines Immun. 2001;8:215–217. [Google Scholar]
- 44.Benedict MQ, Levine RS, Hawley WA, Lounibos LP. Spread of the tiger: global risk of invasion by the mosquito Aedes albopictus. Vector Borne Zoonotic Dis. 2007;7:76–85. doi: 10.1089/vbz.2006.0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu W, Ding D, Clemens JD, Yen NT, Porpit V, Xu Z. Measuring Japanese encephalitis (JE) disease burden in Asia. In: Victor RP, Ronald RW, editors. Handbook of Disease Burdens and Quality of Life Measures. Seattle: Springer; 2010. pp. 1391–1399. [Google Scholar]
- 46.Sun J, Lin J, Yan J, Fan W, Lu L, Lv H, et al. Dengue virus serotype 3 subtype III, Zhejiang Province, China. Emerg Infect Dis. 2011;17:321. [DOI] [PMC free article] [PubMed]
- 47.Wu Y, Ling F, Gong Z, Guo S, Ren J, Chen E. An analysis on the reasons for the delay in discovering dengue fever outbreak in Zhejiang Province. Chin Prev Med. 2017;29:113–116. [Google Scholar]
- 48.Enserink M. An obscure mosquito-borne disease goes global. Science. 2015;350:1012–1013. doi: 10.1126/science.350.6264.1012. [DOI] [PubMed] [Google Scholar]
- 49.Wang S, Yang M, Zhu G, Sun L, Geng H, Cao J, et al. Control of imported mosquito-borne diseases under the Belt and Road Intiative. Chin J Schisto Control. 2018;30:9–13. doi: 10.16250/j.32.1374.2017208. [DOI] [PubMed] [Google Scholar]
- 50.Li J, Xiong Y, Wu W, Liu X, Qu J, Zhao X, et al. Zika virus in a traveler returning to China from Caracas, Venezuela, February 2016. Emerg Infect Dis. 2016;22:1133–1136. doi: 10.3201/eid2206.160273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hu J, Guo X, Li Z, Ma P, Tan Z, Zhang G, et al. First imported case of Zika virus infection into Jiangsu Province, China, returning from Ecuador. J Public Health Emerg. 2017;1:77. doi: 10.21037/jphe.2017.09.01. [DOI] [Google Scholar]
- 52.De W, Jie W, Qiaoli Z, Haojie Z, Changwen K, Xiaoling D, et al. Chikungunya outbreak in Guangdong Province, China, 2010. Emerg Infect Dis. 2012;18:493. [DOI] [PMC free article] [PubMed]
- 53.Lu Z, Fu S, Cao L, Tang C, Zhang S, Li Z, et al. Human infection with West Nile virus, Xinjiang, China, 2011. Emerg Infect Dis. 2014;20:1421. doi: 10.3201/eid2008.131433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu M, Jiang X-J, Shen L, Hong M, Wang Z-Y, Cai L. Epidemiological analysis on malaria prevalence in Shanghai from 2003 to 2012. Chin J Epidemiol. 2014;35:817–820. [PubMed] [Google Scholar]
- 55.Sun D-J, Deng X-L, Duan J-H. The history of the elimination of lymphatic filariasis in China. Infect Dis Poverty. 2013;2:30. doi: 10.1186/2049-9957-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feng J, Tu H, Zhang L, Zhang S, Jiang S, Xia Z, et al. Mapping transmission foci to eliminate malaria in the People’s Republic of China, 2010-2015: a retrospective analysis. BMC Infect Dis. 2018;18:115. doi: 10.1186/s12879-018-3018-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang L, Feng J, Zhang S, Jiang S, Xia Z, Zhou S. Malaria situation in the People’s Republic of China in 2016. Chin J Parasiol Parasit Dis. 2017;35:515–9. (In Chinese).
- 58.Song LG, Zeng XD, Li YX, Zhang BB, Wu XY, Yuan DJ, et al. Imported parasitic diseases in mainland China: current status and perspectives for better control and prevention. Infect Dis Poverty. 2018;7:78. doi: 10.1186/s40249-018-0454-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou Z, Lv S, Zhang Y, Gu W, Guo Y, Jiang M, et al. Mosquito species, distribution and their pathogens in Shanghai, China. Chin J Vector Biol Control. 2015;26:28–32. [Google Scholar]
- 60.Liang G, Li X, Gao X, Fu S, Wang H, Li M, et al. Arboviruses and their related infections in China: a comprehensive field and laboratory investigation over the last 3 decades. Rev Med Virol. 2018;28:e1959. [DOI] [PubMed]
- 61.Lu B, Xu J, Yu Y, Zhang B, Dong X. Fauna Sinica, Insecta, vol. 8. Diptera: Culicidae I. 1st ed. Beijing: Science Press; 1997. (In Chinese).
- 62.Gao Q, Xiong C, Su F, Cao H, Zhou J, Jiang Q. Structure, spatial and temporal distribution of the Culex pipiens complex in Shanghai, China. Inter J Env Res Pub Heal. 2016;13:1150. doi: 10.3390/ijerph13111150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu H, Leng P, Xu R, Wang S. A study on resistance of vector for Japanese encephalitis to insecticides in Shanghai. Shanghai J Prev Med. 2008;20:209–211. [Google Scholar]
- 64.Liu H, Zhu J, Liu Y, Xu J, Leng P. Study on the seasonal dynamics and insecticides resistence of Aedes albopicuts larvae, in Shanghai, 2015–2016. Chin J Vector Biol Control. 2017;28:305–307. [Google Scholar]
- 65.Fang Y, Shi W, Zhang Y. Molecular phylogeny of Anopheles hyrcanus group members based on ITS2 rDNA. Parasit Vectors. 2017;10:417. doi: 10.1186/s13071-017-2351-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lu G, Zhou S, Horstick O, Wang X, Liu Y, Müller O. Malaria outbreaks in China (1990–2013): a systematic review. Malar J. 2014;13:269. doi: 10.1186/1475-2875-13-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fang Y, Zhang Y, Zhou Z, Shi W, Xia S, Li Y, et al. Co-circulation of Aedes flavivirus, Culex flavivirus, and Quang Binh virus, in Shanghai, China. Infect Dis Poverty. 2018;7:75. doi: 10.1186/s40249-018-0457-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoffmann PR, Woodrow RJ, Calimlim PS, Sciulli RH, Effler PV, Miyamoto V, et al. West Nile virus surveillance: a simple method for verifying the integrity of RNA in mosquito (Diptera: Culicidae) pools. J Med Entomol. 2004;41:731–735. doi: 10.1603/0022-2585-41.4.731. [DOI] [PubMed] [Google Scholar]
- 69.Cook S, Moureau G, Harbach RE, Mukwaya L, Goodger K, Ssenfuka F, et al. Isolation of a novel species of flavivirus and a new strain of Culex flavivirus (Flaviviridae) from a natural mosquito population in Uganda. J Gen Virol. 2009;90:2669–2678. doi: 10.1099/vir.0.014183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gao X, Liu H, Wang H, Fu S, Guo Z, Liang G. Southernmost Asia is the source of Japanese encephalitis virus (genotype 1) diversity from which the viruses disperse and evolve throughout Asia. PLoS Negl Trop Dis. 2013;7:e2459. doi: 10.1371/journal.pntd.0002459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bryant JE, Crabtree MB, Nam VS, Yen NT, Duc HM, Miller BR. Isolation of arboviruses from mosquitoes collected in northern Vietnam. Am J Trop Med Hyg. 2005;73:470–473. doi: 10.4269/ajtmh.2005.73.470. [DOI] [PubMed] [Google Scholar]
- 72.Kuno G, Mitchell CJ, Chang GJ, Smith GC. Detecting bunyaviruses of the Bunyamwera and California serogroups by a PCR technique. J Clin Microbiol. 1996;34:1184–1188. doi: 10.1128/jcm.34.5.1184-1188.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yan J, Li N, Xu W, Li P, Zhao Z, Wang L, et al. Performance of two rapid diagnostic tests for malaria diagnosis at the China-Myanmar border area. Malaria J. 2013;12:73. doi: 10.1186/1475-2875-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vasuki V, Hoti SL, Sadanandane C, Jambulingam P. A simple and rapid DNA extraction method for the detection of Wuchereria bancrofti infection in the vector mosquito, Culex quinquefasciatus by Ssp I PCR assay. Acta Tropica. 2003;86:109–114. doi: 10.1016/S0001-706X(02)00267-X. [DOI] [PubMed] [Google Scholar]
- 75.Xie H, Bain O, Williams SA. Molecular phylogenetic studies on Brugia filariasis using HHA I repeat sequences. Parasite. 1994;1:255–260. doi: 10.1051/parasite/1994013255. [DOI] [PubMed] [Google Scholar]
- 76.Larkin MA, Blackshields G, Brown NP, Chenna R, McGettigan PA, McWilliam H, et al. Clustal W and Clustal X version 2.0. Bioinformatics. 2007;23:2947–2948. doi: 10.1093/bioinformatics/btm404. [DOI] [PubMed] [Google Scholar]
- 77.Kimura M. A simple method for estimating evolutionary rates of base substitutions through comparative studies of nucleotide sequences. J Mol Evol. 1980;16:111–120. doi: 10.1007/BF01731581. [DOI] [PubMed] [Google Scholar]
- 78.Kumar S, Stecher G, Tamura K. MEGA7: Molecular Evolutionary Genetics Analysis version 7.0 for bigger datasets. Mol Biol Evol. 2016;33:1870–1874. doi: 10.1093/molbev/msw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wilgenbusch JC, Swofford D. Inferring evolutionary trees with PAUP*. Curr Protoc Bioinformatics. 2003;6:6.4. doi: 10.1002/0471250953.bi0604s00. [DOI] [PubMed] [Google Scholar]
- 80.Ronquist F, Teslenko M, van der Mark P, Ayres DL, Darling A, Hohna S, et al. MrBayes 3.2: efficient Bayesian phylogenetic inference and model choice across a large model space. Syst Biol. 2012;61:539–542. doi: 10.1093/sysbio/sys029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Biggerstaff BJ. PooledInfRate, version 3.0: a Microsoft® Excel® add-in to compute prevalence estimates from pooled samples. Fort Collins, CO: CDC; 2006. [Google Scholar]
- 82.Wang H, Fu S, Li X, Song H, Min J, Deng J, et al. Isolation and identification of genotype I Japanese encephalitis virus in China. Chin J Microbiol Immunol. 2004;24:843–849. [Google Scholar]
- 83.Do LP, Bui TM, Hasebe F, Morita K, Phan NT. Molecular epidemiology of Japanese encephalitis in northern Vietnam, 1964–2011: genotype replacement. Virol J. 2015;12:51. doi: 10.1186/s12985-015-0278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nga PT. Shift in Japanese encephalitis virus (JEV) genotype circulating in northern Vietnam: implications for frequent introductions of JEV from Southeast Asia to East Asia. J Gen Virol. 2004;85:1625–1631. doi: 10.1099/vir.0.79797-0. [DOI] [PubMed] [Google Scholar]
- 85.Hennessy S, Liu Z, Tsai TF, Strom BL, Wan CM, Liu HL, et al. Effectiveness of live-attenuated Japanese encephalitis vaccine (SA14-14-2): a case-control study. Lancet. 1996;347:1583–1586. doi: 10.1016/S0140-6736(96)91075-2. [DOI] [PubMed] [Google Scholar]
- 86.Bista MB, Banerjee MK, Shin SH, Tandan JB, Kim M, Sohn YM, et al. Efficacy of single-dose SA 14-14-2 vaccine against Japanese encephalitis: a case control study. Lancet. 2001;358:791–795. doi: 10.1016/S0140-6736(01)05967-0. [DOI] [PubMed] [Google Scholar]
- 87.Kumar R, Tripathi P, Rizvi A. Effectiveness of one dose of SA 14-14-2 vaccine against Japanese encephalitis. N Engl J Med. 2009;360:1465–1466. doi: 10.1056/NEJMc0808664. [DOI] [PubMed] [Google Scholar]
- 88.Hu Q, Chen B, Zhu Z, Tian J, Zhou Y, Zhang X, et al. Recurrence of Japanese encephalitis epidemic in Wuhan, China, 2009–2010. PLoS One. 2013;8:e52687. doi: 10.1371/journal.pone.0052687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang L, Fu S, Wang H, Liang X, Cheng J, Jing H, et al. Japanese encephalitis outbreak, Yuncheng, China, 2006. Emerg Infect Dis. 2007;13:1123–1125. doi: 10.3201/eid1307.070010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article. The newly generated sequences were submitted to the GenBank database under the accession numbers MG686629-MG686637, MG686640, MG686641 and MG686643.