Abstract
Objectives
We examine gender differences in the experienced burden of partner caregivers using the stress-appraisal model. Gender differences can be explained by differences in conditions of burden (primary stressors, help from others, hours of caregiving, and secondary stressors) and how strong their effects are.
Method
The data are from the Netherlands’ Older Persons and Informal Caregivers Survey—Minimum Data Set (N = 1,611 caregivers). We examine mediation and moderation effects using structural equation modeling.
Results
Women experience greater partner caregiver burden than men, which is related to women experiencing more secondary stressors (relational and financial problems, problems combining different tasks). For women and men alike, there is a positive association between burden and more primary stressors (partner’s care need indicated by health impairment), help from other caregivers, and secondary stressors. For male caregivers, caregiving intensity also contributes to a greater burden.
Discussion
This study corroborates the structural impact of gender on the conditions of as well as their effects on the partner caregiver burden. Reducing the hours of caregiving for male caregivers in severe care situations and helping female and male caregivers deal emotionally with the caregiving situation can reduce the partner caregiver burden.
Keywords: Burden, Caregiving, Gender differences, Secondary stressors, Spousal caregiving
Since population aging and public policy limit the accessible formal care services, informal caregivers provide a great deal of the long-term care services for frail older adults. Older people’s partners are the first in line to provide informal care. Compared to other types of caregivers, partners spend many more hours providing care in multiple fields for a longer period of time and are less frequently assisted by other informal caregivers (Jacobs, Broese van Groenou, Aartsen, & Deeg, 2016). The chronic and progressive impairment of a partner may contribute to an involuntary transformation of a relationship that can reduce its quality (Pearlin, Mullan, Semple, & Skaff, 1990). As a result, partner caregivers run a higher risk of being overburdened than other types of caregivers (Pearlin et al., 1990; Pinquart & Sörensen, 2003; Wolff & Kasper, 2006). This risk may be intensified in the increased need for informal care in the future.
Caregiver literature has consistently shown that female caregivers are more burdened than male caregivers (Marks, Lambert, & Choi, 2002; Mc Donnell & Ryan, 2013; Penning & Wu, 2016; Pinquart & Sörensen, 2006; Yee & Schulz, 2000). Explanations of gender differences in caregiver burden may follow two lines of reasoning. The first argues that women and men live in different structural contexts and the unequal distributions of rewards, privileges, opportunities, and responsibilities leads to different kinds and intensities of stressors to which people are exposed (Pearlin et al., 1990, p. 585). The unequal distribution of opportunities and responsibilities may push women into the caregiver role more often than men and thus hamper their functioning in other fields (work, health). The fact that women provide more hours of care and experience more negative effects of caregiving may explain why they experience a higher caregiver burden (Pinquart & Sörensen, 2006; Yee & Schulz, 2000). The empirical test here involves a mediation model showing the degree to which gender differences in burden are explained by gender differences in the conditions of burden. The second line of reasoning notes that, in addition to differences in the burden conditions, women and men experience caregiving differently (Calasanti, 2010; Mc Donnell & Ryan, 2013). It is argued that if women feel more responsible and obliged to care and men are more apt to step away from the care work (Hong & Coogle, 2016; Kramer 1997), the conditions of burden (e.g., intensity of caregiving) may play out differently for women and men. The empirical test in line with this argument involves a moderation model showing whether the conditions affect burden differently for women and men. This study aims to contribute to an understanding of the gender gap in the caregiver burden of partners by examining both lines of reasoning in a mediation and a moderation model.
Theoretical Model
Following Chappell and Reid (2002) and Yates, Tennstedt, and Chang (1999), we apply a stress-appraisal approach defining burden as the subjective evaluation of the care situation, that is, the overall stress when caring for or accompanying a care recipient. We separate this overall burden from the secondary stressors, that is, problems resulting from the caregiving situation. The stress-appraisal model integrates the notion of appraisal (Lawton, Moss, Kleban, Glicksman, & Rovine, 1991) into the stress process model of Pearlin et al. (1990). In the appraisal model, the experienced burden is considered an outcome of being a caregiver and can be distinguished from the caregiver’s well-being, which is a more general outcome of the caregiving process (Chappell & Reid, 2002; Yates et al., 1999).
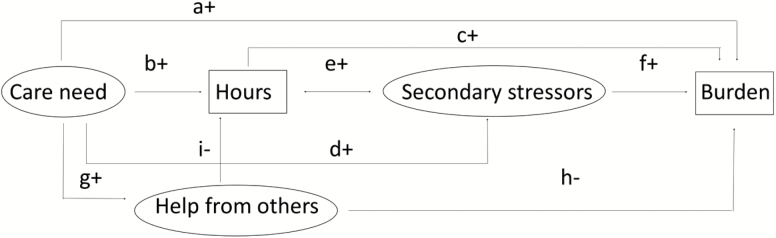
In line with the stress-appraisal model, the caregiver’s burden depends directly or indirectly on multiple conditions (Figure 1). The process starts with the primary caregiver stressors, the level and type of health impairment leading to the need for care, that is, the care recipient’s physical incapacity, cognitive dysfunction, mental health problems and co-morbidity. This may directly affect the level of burden (Arrow a), but the model assumes several indirect pathways between the need for care and burden. First, the caregiver makes the primary appraisal, a behavioral response to the need for care expressed during the informal caregiving (Yates et al., 1999). The greater the need for care, the more hours of care are provided (Arrow b) and the greater the caregiver burden (Arrow c). As a result of the primary stressors and the hours spent on caregiving, secondary stressors arise in other fields of functioning (Arrows d and e), which in turn increase the caregiver burden (Arrow f). Typical secondary stressors are relational problems with the care recipient, financial problems and problems combining the caregiving with social or work activities (Chappell & Reid, 2002; Savundranayagam, Montgomery, & Kosloski, 2010b). Another pathway to burden runs via the help provided by other formal and informal caregivers, which is also triggered by the need for care (Arrow g). The help provided by others may be experienced as emotionally supportive and directly lower the level of burden (Arrow h). Help from others might decrease burden indirectly by lowering the number of hours of care provided (Arrow i). For the mediation as well as the moderation model, we use the same conditions of burden (Figure 1). We add gender as an additional variable in the mediation model and stratify analyses for male and female caregivers in the moderation model.
Figure 1.
Baseline theoretical model.
Gender Differences in the Conditions Associated With Burden
Due to an unequal distribution of opportunities and socialization of gender roles, there can be gender differences in all the burden-related conditions, that is, primary stressors, hours of caregiving, help from others and secondary stressors. Primary stressors are expected to be stronger for female than male caregivers. As women are often younger than their husbands and age is an important predictor of the level of impairment, women are more likely to have a partner with more of a care need than men. Women are also expected to devote more time to partner care than men. According to social role theory, women are viewed as being responsible for caregiving tasks. Especially women born in the first half of the 20th century have learned to nurture and care from childhood on (Stoller, 1992). Women and men internalize gender norms and come to view caring as women’s work (Glauber, 2016). Men are less socialized into the caregiving role than women (Allen, Goldscheider, & Ciambrone, 1999; Miller, 1990). Partner caregiving in old age is thus likely to be an extension of women’s social role earlier in life, whereas for men it is a new, unfamiliar role. Because of their greater commitment to the caregiving role, women spend more time on caregiving and often have less time for other activities. So women can experience more problems than men combining caregiving with other activities and tasks (Pavalko & Woodbury, 2000; Savundranayagam & Montgomery, 2010a). Because of these gender roles, men may more often be offered and accept help from others than women. Thus, Hypothesis 1 states that the lower burden of male caregiving is related to objective conditions (a) the more limited care needs of the care recipient wives, (b) fewer hours of caregiving by men and (c) more help received by men from others, as well as to a subjective condition (d) less secondary stressors experienced by men.
Gender Differences in Effects of the Conditions on Burden
The gender gap in the caregiver burden can also result from women and men dealing differently with the caregiving process even if the conditions are similar (Hong & Coogle, 2016). This assumption is derived from the masculinity theory of Calasanti (2010). Structural inequality over the life course influences how men and women approach care work, the stresses they encounter and how they cope with these stressors (Calasanti 2010, p. 726). As the life course of men evolves around their tasks in paid employment, men tend to approach caregiving as tasks to master and problems to solve (Russell, 2007). This reinforces the notion that men may feel less responsible for care work (Calasanti, 2010). During their life course, women put more emphasis on caring and nurturing, which may explain why they approach caring for their spouses with greater concern for the care recipient as a whole and for the mutuality of the emotional dynamics of the relationship (Calasanti, 2010). It is argued that men’s problem-focused strategy alleviates strain. Their managerial approach allows them to take control and introduce positive changes as caregivers, giving them a stronger sense of control and an opportunity to choose to act or not to act (Calasanti & King, 2007; Kramer, 1997). This may explain why male caregivers provide fewer hours of care than female caregivers, as is noted above, but it could also imply different effects of hours of caregiving on secondary stressors or on the caregiver burden of female and male caregivers. In addition, women are less likely than men to put their own interests or needs above those of their partners and as a result, are more dedicated to emotionally and physically caring for them (Impett & Peplau, 2006), whereas men focus on the practical issues and minimize their emotional responses to caregiving (McFarland & Sanders, 1999). So burden is greater for female than male caregivers under conditions that are objectively similar, such as care needs and hours of care provision. Receiving help from others may also be experienced differently, male caregivers may feel more relieved when others provide care whereas female caregivers may feel a loss of autonomy in their caregiver role. Hypothesis 2 states that pathways from the care recipient’s care need to the caregiver burden differ for female and male caregivers. The same level of care need, hours of caregiving and secondary stressors leads to a greater burden for female than male caregivers and the same level of help from others leads to a smaller burden for male than female caregivers.
Method
Data
The data are derived from the Older Persons and Informal Caregivers Survey—Minimum Data Set (TOPICS-MDS; www.topics-mds.eu), which is a public-access data repository designed to capture essential information on the physical and mental well-being of older persons and informal caregivers in the Netherlands (Lutomski et al., 2013). The Dutch National Care for the Elderly Program, commissioned by the Dutch Ministry of Health, Welfare and Sports, was established in 2008 to promote proactive, integrated health care for older persons with complex care needs. As part of this agenda, TOPICS-MDS was developed to collect uniform information from research projects funded under the program and to pool data. Thirty-one projects collected data in the Netherlands from 2008 to 2015 among care recipients as well as their informal caregivers. The projects differ in study design (see Supplementary Data I).
Analytical Sample
We used the dataset available in December 2015. We included thirty-one research projects with data on care recipients and their partners giving informal care (N = 2,662) and excluded one project with no data on the need for care of the care receiver (n = 246). From the thirty projects, we selected 1,611 couples and excluded couples where data on the caregiver was missing (n = 307) or zero hours of care was given, as a caregiver by definition should provide at least some care per week (n = 498). For more information on the projects, see Supplementary Data I.
Measurements Completed by Caregiver
We measured the experienced burden with a single question: On the scale below, 0 means you now feel that caring for or accompanying your partner is not hard at all and 100 means you now feel that caring for or accompanying your partner is much too hard. Please indicate with an x on the scale how much of a burden you feel caregiving is at the moment. This question is evaluated as a valid instrument to assess the burden of caregiving (among a sample of 148 caregivers of stroke patients; see Van Exel et al., 2004).
Hours of caregiving
We asked the caregivers whether they spent caregiving time in the past week on: (a) Activities such as preparing food and drinks, cleaning the house, washing, ironing and dusting, shopping, maintenance work, odd jobs or gardening, (b) Activities such as help with personal care, mobility or going to the toilet, (c) Mobility outside the home, taking trips or organizing help. For each activity, we asked the respondents: If you engaged in any of these activities, how many hours a week did you spend on them? We summarized the three reports on hours.
Other caregivers—Help from other informal caregivers
We asked the caregivers whether the care recipients receive care from informal caregivers other than the partner or from volunteers (0 = no, 1 = yes).
Secondary stressors
The caregivers responded to three statements: I have no/some/many relational problems with the care recipient, I have financial problems because of the caregiving situation, I have problems combining my care tasks with my daily activities because of the caregiving situation. The answers are coded as 0 = none, 1 = some or many.
Measurements Completed by Care Recipients
Primary stressors were related to four health characteristics.
Physical incapacity
The Katz-15 Index of Activities of Daily Living measures physical functioning in several fields such as bathing, dressing, transporting, and feeding (Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963). For each item, the respondents indicated whether the care recipient needs help (0 = no, 1 = yes). Physical incapacity represents the mean item score (reliability KR-20 = 0.86).
Cognitive dysfunction
We asked about the care recipients’ current situation: Do they have no/some/serious problems with memory, attention or thinking (0 = none, 1 = some or serious).
Mental health problems
We constructed a scale score as the mean score of five items (reliability alpha = 0.80): How much time in the past month have the care recipients been very nervous, felt calm and peaceful, felt downhearted and blue, been a happy person, felt so down in the dumps that nothing could cheer them up? Response categories range from all the time (1) to none of the time (6). We reversed code questions 2 and 6.
Comorbidity
We presented a list of twenty diseases and disorders and asked the care recipients whether they had them in the past 12 months (0 = no, 1 = yes). We counted the numbers.
Other caregivers—Home care
We asked the care recipients whether they had professional home care, for example nursing or domestic care (0 = no, 1= yes).
Day care
We asked the care recipients whether they go to a day care center (0 = no, 1 = yes).
Procedure
There were no missing data on the gender of the care recipients, but there were missing data on the gender of the caregivers (n = 353). Given the low number of registered same sex couples (1%; Statistics Netherlands, 2016), we assumed all the couples are heterosexual. In addition, data were missing for cognitive dysfunction (3%), mental health problems (10%) and co-morbidity (12%). We imputed the estimated probabilities on the basis of regressions among respondents with non-missing data on care need factors. We imputed the sample mean for the remaining missing data (1% missing all of the need factors, 4% of the help of other caregiver variables and 5% of secondary stressor variables). To test whether the imputations could bias our results, we performed correlations and multivariate regression analysis separately on the sample with no missing cases and the sample with imputations. Both analyses have comparable results, which shows that the imputation did not substantively impact the findings.
To create the best model fit and most parsimonious path model, we constructed latent variables for our theoretical concepts rather than use the indicators separately in the analysis. In particular, we constructed the latent variables from four care need factors, three secondary stressors and three variables on help from others.
We calculated the descriptive statistics using Chi-square and t tests to determine whether there is a gender difference in the conditions and burden. To estimate the gender difference in the means of the latent variables, we choose female caregivers as the reference group and fixed its mean on the construct at zero (CFA in Mplus, Muthén & Muthén 2012). The constructed mean of male caregivers represents its difference from females.
To test the conditions hypothesis (H1), we applied structural equation modeling (SEM in Mplus. Muthén & Muthén 2012) with gender as independent variable, burden as outcome and the other variables as mediating. To test the effects of conditions on burden hypothesis (H2), we applied SEM stratified by gender. We tested gender differences in the total set of estimates by a Wald test. If it was non-significant, we subsequently calculated one estimate in the pooled sample of female and male caregivers. In the final model, five coefficients differ in magnitude for female and male caregivers (Wald = 14.7, df = 5, p < .05), that is, the effects of the care need on the total hours of caregiving, on the help of others and on the secondary stressors and the effects of the total hours of caregiving on the secondary stressors and on the experienced burden (Supplementary Data II). However, the difference is only considered substantial as regards the effect of the hours of caregiving on burden (for females B = 0.06, SE = 0.03. for males B = 0.24, SE = 0.05). To check whether the models fit the data, we computed the root mean square error of approximation (RMSEA), the standardized root mean square residual (SRMR) and the comparative fit index (CFI), as they can deal with complex models. The RMSEA and SRMR are absolute fit indices; they do not rely on comparison with a reference model but depend only on how well the hypothesized model fits the sample. SRMR is a standardized summary of the average covariance residuals (Kline, 1998). These covariance residuals are the differences between the observed and the hypothesized co-variances. A value of less than 0.05 indicates a good fit for RMSEA and SRMR (Byrne, 2013). The CFI measures the proportionate improvement in model fit by comparing the hypothesized model, imposing structure with the less restricted nested baseline model. Good fit is indicated by CFI > 0.90 (Byrne, 2013).
Results
In 57% of the couples, the wife was the caregiver, in the other 43% the husband was. The average age of the caregivers was 73, and of the care recipients 77. We reported the means and percentages of the study variables in Table 1. The female caregivers were disadvantaged on all the conditions. They reported a higher burden, had partners with a greater care need, provided more hours of care a week, reported more secondary stressors and received less help from others than male caregivers. Husbands only used more day care than wives. There were no significant differences in the latent variables need factors or help from others.
Table 1.
Description of Study Variables (N = 1,611), Female Caregivers (n = 911), Male Caregivers (n = 700)
| All | Female | Male | |||
|---|---|---|---|---|---|
| %/M | SD | %/M | %/M | ||
| Gender (1 = male) (CG) (%) | 43 | ||||
| Age (CR) | 77.5 | (6.8) | 77.8 | 77.1 | |
| Age (CG) | 73.2 | (9.2) | 71.5 | 75.5 | *** |
| Burden (standardized coefficient) (CR) | 0.12 | −0.15 | *** | ||
| Burden (CG) | 46.1 | (24.5) | 48.9 | 42.4 | *** |
| Need factors (latent variable) (CR) | 0.0 | −0.06 | |||
| Physical incapacity (CR) (0–1) | 0.39 | (0.25) | 0.40 | 0.39 | |
| Cognitive dysfunction (CR) (0–1) (%) | 52 | 56 | 49 | *** | |
| Mental health problems (CR) (1.0–5.8) | 2.5 | (0.89) | 2.6 | 2.5 | |
| Co-morbidity (CR) (0–11) | 3.5 | (2.0) | 3.6 | 3.4 | |
| Hours (standardized coefficient) (CG) | 0.05 | −0.06 | * | ||
| Total hours of caregiving (week) (0.1–168) | 29.2 | (32.5) | 30.8 | 27.2 | * |
| Help from others (latent variable) | 0.0 | 0.05 | |||
| Help from other informal caregivers (CG) (%) | 29 | 28 | 31 | ||
| Home care (CR) (%) | 41 | 39 | 44 | * | |
| Day care (CR) (%) | 14 | 17 | 11 | *** | |
| Secondary stressors (latent variable) (CG) | 0.0 | −0.29 | *** | ||
| Relational problems (%) | 47 | 54 | 37 | *** | |
| Financial problems (%) | 14 | 15 | 12 | ||
| Problems combining tasks (%) | 0 50 | 59 | 40 | *** | |
Notes: CG = caregiver; CR = care recipient. Chi-square tests and t tests. In bold standardized values of the variables used in the SEM model in Mplus. Latent variable gender difference from the model “grouped by gender” (Figure 3).
*p < .05; **p < .01; ***p <.001.
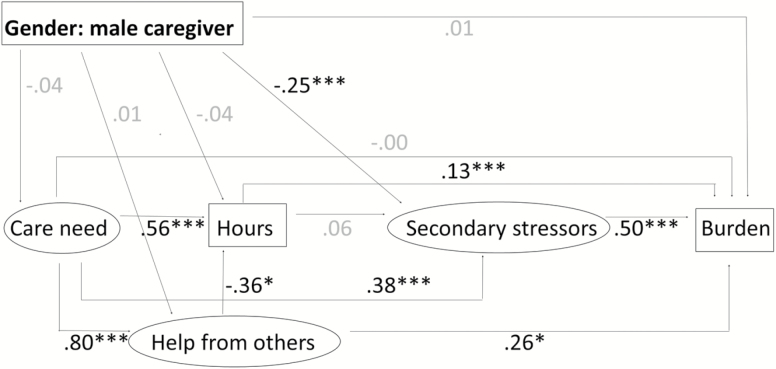
Figure 2 shows the standardized estimates of the mediating model and makes it possible to test Hypothesis 1. The model fitted the data well and explained 44% of the variance in the experienced burden. We present the loadings of the indicators for the latent variables in Supplementary Data III. The most important finding is that there was no significant direct effect of gender on burden. The lower burden of male than female caregivers (bivariate standardized B = −0.27, p < .001) was related to the weaker experienced secondary stressors among male caregivers. There was no evidence from this multivariate model that female caregivers bear a greater burden than male caregivers due to differences in care needs, hours of care, or help from others. The indirect path from gender to burden runs via secondary stressors (−0.25, p < .001) to burden (0.50, p < .001). We computed the strength of the indirect path as the product of the two direct effects (−0.25 × 0.50 = −0.13, p < .001).
Figure 2.
Standardized path coefficients of the gender-mediation model. *p < .05; **p < .01; ***p < .001. RMSEA = 0.049 (90% CI = 0.043–0.055); CFI = 0.91; SRMR = 0.034; R2 (burden) = 44%; N = 1,611.
Gender Differences in Magnitude of Effects
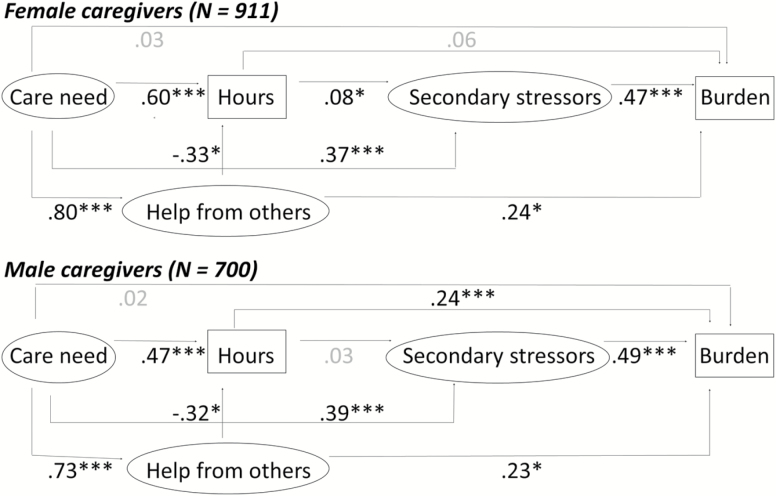
In Figure 3 we examine the results of the moderation effects of Hypothesis 2. The model fitted the data well and explained 42% and 44% of the variance in the experienced burden of female and male partner caregivers. We considered one standardized coefficient as different in magnitude for female and male caregivers, that is, the effect of the total hours of caregiving on the experienced burden.
Figure 3.
Standardized path coefficients for female caregivers (above) and male caregivers (below). *p < .05; **p < .01; ***p < .001; RMSEA = 0.048 (90% CI: 0.041–0.054); CFI = 0.91; Wald(df = 5) = 14.7; p < .05; SRMR = 0.041; R2 (burden) female caregivers = 42%; male caregivers = 44%; N = 1,611.
For female caregivers, there were two significant indirect paths from the care need to burden. A greater care need on the part of the recipient husband contributed to a higher level of secondary stressors (0.37, Figure 3), increasing the female caregivers’ burden (0.47) and resulting in an indirect path of 0.17 (Table 2). A greater care need increased the hours of caregiving (0.60) but for women this condition was not directly associated with the caregiver burden. A greater care need on the part of the recipient contributed to more help from other caregivers (0.80) and (contrary to our hypothesized model) increased burden (0.24), resulting in an indirect path of 0.20. So for female caregivers, burden was directly and positively associated with the secondary stressors, negatively with help from other caregivers, and indirectly (via secondary stressors or help from other caregivers) with the husband’s need for care.
Table 2.
Structural Equation Model Estimates of Indirect and Total Effects of Care Need on Burden
| Female caregivers | Male caregivers | |
|---|---|---|
| Indirect via | ||
| Secondary stressors | 0.17*** | 0.19*** |
| Hours of caregiving | 0.04 | 0.11* |
| Help from other caregivers | 0.20* | 0.17 |
| Total | 0.43*** | 0.42*** |
Notes. The path is only shown if significant for female or male caregivers. Estimates are from Figure 3.
*p < .05, **p < .01, ***p < .001.
For male caregivers, one path was similar to that of female caregivers, that is, a greater care need of the recipient wife contributed to a higher level of secondary stressors (0.39), increasing the male caregivers’ burden (0.49) and resulting in an indirect path of 0.19. A greater care need on the part of the recipient wife contributed to more hours of caregiving (0.47) and increased burden (0.24), resulting in an indirect path of 0.11; we did not find this path among female caregivers. The greater the care need of the recipient wife, the more help the male caregiver received from others (0.73), but this was not significantly associated with a greater experienced burden (the indirect effect is 0.17, p = .06). So for male caregivers the experienced burden was directly and positively associated with the secondary stressors and hours of caregiving and only indirectly (via secondary stressors and hours of caregiving) with his wife’s need for care.
Discussion
This study assessed the explanations of the gender gap in burden experienced by partner caregivers. Guided by the stress-appraisal model (Yates et al. 1999), we argue that a gender gap in this burden can be explained by gender differences in the conditions of burden (H1), and in the magnitude of the effects of these conditions on burden (H2). There are four major findings. First, female caregivers reported a greater experienced burden than male caregivers and our mediation model showed that secondary stressors—relational and financial problems and problems combining different tasks—are the major explanations for this gender gap. So it were not the objective factors but the subjective factors, the secondary stressors that explained the gender gap, partly supporting Hypothesis 1. Second, the moderation model showed that only one pathway to burden differs. More hours of care given by female caregivers did not increase their burden, though it did so for male caregivers. This refutes Hypothesis 2, that is, that the effects of the care need on secondary stressors are stronger for male than female caregivers and the effects of secondary stressors on burden are similar. In line with Lin, Fee, and Wu (2012) and Penning and Wu ( 2016), we observe that the act of caregiving differs for females and males.
The finding that providing more hours of care means a greater burden for men but not for women seems to contradict the general finding (also in our study) that women report a greater caregiver burden than men. Perhaps women experience a greater burden regardless of the hours of care provided. It is possible that gender differences in the experienced burden change over the course of the care process. If the care need is limited and care provision is not intense, women may experience more of a care burden than men because of their emotional and nurturing approach. Men’s problem-focused strategy may make it easier for them to handle the caregiving situation (Calasanti, 2010; Hong & Coogle, 2016; Kramer, 1997). However, if the care is more intense and requires more problem-solving skills, this may increase the experienced burden more for men than for women, who might have experienced a greater burden from the start. The findings imply that male caregivers need help to change the subjective perception of care; they may be less used to providing care and therefore may experience the time they spend on caregiving as more burdensome than women. For women it is mainly the consequences of care in other areas that require additional attention. Yet, for men and women alike, it is useful to recognize the stress of the caregiving situation.
Third, the role of help from others is not what we expected. It impacts the caregiving intensity but not the secondary stressors, and it increases rather than reduces burden for caregivers. If the help of others increases burden, this might mean partner caregivers only request or accept help if burden is extremely or excessively high (Verbakel, Metzelthin, & Kempen, 2016). This is supported by the strong positive association between the care need and help from other caregivers for women and men alike. Another interpretation is that some partners may perceive accepting help from others as a failure, that is, they were unable to fulfill their duty as a partner (Stoller, 1992). Research supports the idea that a partner is more committed than other caregivers to providing all the forms of care themselves (Marks et al., 2002). Earlier research reveals that interventions focused on increasing the caregiver’s satisfaction with the network support can alleviate a caregiver’s emotional distress (Roth, Mittelman, Clay, Madan, & Haley, 2005). Other studies corroborate that the quality of support is important for reducing the strain of a partner caregiver (Savundranayagam, 2014). So partner interventions should include apprehending skills that enable them to mobilize help from others, as well as a cognitive reframing of accepting help as a positive act and not as a personal shortcoming.
Fourth, many pathways in the stress-appraisal model proved to be similar for female and male partner caregivers. This may not be the case with gender differences in other types of care relationships, for example, between parents and children. The partner relationship is a caregiving situation and especially sensitive to an imbalance if one partner becomes a dependent care recipient and the other a caregiver. The role change may be less detrimental in other types of relationships, for example, a child caregiver is more likely to have alternative roles and social activities outside the home that serve as a buffer against severe and long-lasting caregiving stress (Pinquart & Sörensen, 2003). So secondary stressors may play out differently in the stress-appraisal model for adult child caregivers. Recent research suggests that the needs of a partner caregiver differ from those of an adult child caregiver (Savundranayagam, 2014). We cannot generalize our findings on gender-related burden differences to other caregiver types. Future research should be conducted on the differences in the stress-appraisal model between partner caregivers and other types of caregivers.
This study has several strengths, particularly the large sample with dyadic information on the caregivers and care recipients and the models used. However, data limitations should be acknowledged as well. The findings show a strong association between secondary stressors and the caregiver burden. In part, this may be due to the measurements, since they both concern evaluations of the caregiving situation. Our outcome measurement is a one-item measurement of experienced burden, which requires an emotional evaluation of the caregiving situation. The three aspects of secondary stressors require an evaluation of the effects of the caregiving situation in other fields of functioning. The subjective and evaluative nature of these measurements may contribute to the strong correlation. Zarit, Reever, and Bach-Peterson (1980) included these aspects in a multidimensional burden scale, and Savundranayagam and Montgomery (2010a) composed a scale involving stress, relationship, and objective burden. Our study shows the merits of separating the evaluation of the caregiving itself from evaluations in other fields. Our results suggest that understanding gender differences in the partner caregiving burden requires separate research on the various fields of the Zarit burden scale for female and male partner caregivers. Savundranayagam and Colleagues (2010b) arrived at the same conclusion and discussed the importance of measuring specific burden dimensions. A second data limitation is perhaps that the thirty projects vary in their sampling frame and mode of data collection. Although all the samples report a greater female than male caregiving burden, the extent differs across the sampling frame and mode of data collection so we should be cautious about generalizing the results. We also checked whether the exclusion of cases with zero hours of caregiving was gender specific and may have impacted our results. Additional analyses showed that excluded caregivers were somewhat more often female, reported low care burden and concerned cases with low care need. Multivariate analyses conducted with a sample including those with zero hours of caregiving showed the comparable gender-specific effect of hours of caregiving on burden. This corroborates our conclusion that for male caregivers only, hours of caregiving increase burden.
Despite the theoretical model depicting a dynamic process, we did not implement a longitudinal design. Future studies need to examine whether gender differences in burden do indeed vary over time or care intensity. In addition, running structural equating modeling required the use of latent variables to test our models. This means we lost the nuances of, for example, a more detailed description of help from others as is presented by Verbakel and Colleagues (2016), who analyzed data from the same projects and studied a sample of various caregiver types. Lastly, the utilization of help from others depends in part on the allocation of professional home care and community services like day care, which varies across countries (Suanet, Broese van Groenou, & Van Tilburg, 2012). This means the positive association between help from others, care need, care intensity and burden is different in other societies. It would be useful to conduct further research on gender differences in burden in a cross-national perspective.
Despite these limitations, the strength of our contribution to the field is that our study shows that gender is a structurally varying element for outcomes of caregiving. As we can see in the mediation model (Figure 2), just adding gender as an extra variable does not shed light on the different underlying processes, which only emerge in the moderation model (Figure 3). To a certain degree, female and male caregivers deal differently with caregiving. Men seem to respond more strongly to the severity of the caregiving situation and for women the caregiving situation itself seems to be what causes the strain (burden as well as secondary stressors). This study supports the work of Savundranayagam and Montgomery (2010a), who conclude that it is the subjective evaluation of the workload as well as the subjective evaluation of its effects that cause caregiver burden. In view of the explanations in this study for gender differences in partner caregivers, it is not the objective conditions (need factors, hours of caregiving) that explain the gender difference, it is the subjective evaluation of the caregiving situation. This can be structural and thus not easy to resolve. However, recognizing the difficult situation partner caregivers are in and devoting more effort to emotional support may well relieve burden experienced for both males and females.
Funding
The work was supported by the National Care for the Elderly Program on behalf of the Netherlands Organisation for Health Research and Development (ZonMw, Grant reference 310300002). This study makes use of data generated by the Older Persons and Caregivers Survey Minimum Dataset (TOPICS-MDS). A list of the investigators is available at www.topics-mds.eu.
Conflict of Interest
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Supplementary Material
Acknowledgment
Author Contributions: Joukje Swinkels planned the study, performed all statistical analyses, wrote and revised the paper. Theo van Tilburg helped to plan the study, supervised the data analysis, and contributed to writing and revising the paper. Ellen Verbakel helped to plan the study and contributed to writing and revising the paper. Marjolein Broese van Groenou, helped to plan the study, supervised the data analysis, and contributed to writing and revising the paper.
References
- Allen S. M., Goldscheider F., Ciambrone D. A. (1999). Gender roles, marital intimacy, and nomination of spouse as primary caregiver. The Gerontologist, 39, 150–158. doi:10.1093/geront/39.2.150 [DOI] [PubMed] [Google Scholar]
- Byrne B. M. (2013). Structural equation modeling with Mplus: Basic concepts, applications, and programming. New York: Routledge [Google Scholar]
- Calasanti T. (2010). Gender relations and applied research on aging. The Gerontologist, 50, 720–734. doi:10.1093/geront/gnq085 [DOI] [PubMed] [Google Scholar]
- Calasanti T., King N. (2007). Taking ‘women’s work’ ‘like a man’: Husbands’ experiences of care work. The Gerontologist, 47, 516–527. doi:10.1093/geront/47.4.516 [DOI] [PubMed] [Google Scholar]
- Chappell N. L., Reid R. C. (2002). Burden and well-being among caregivers: Examining the distinction. The Gerontologist, 42, 772–780. doi:10.1093/geront/42.6.772 [DOI] [PubMed] [Google Scholar]
- Glauber R. (2016). Gender differences in spousal care across the later life course. Research on Aging. doi:10.1177/0164027516644503 [DOI] [PubMed] [Google Scholar]
- Hong S. C., Coogle C. L. (2016). Spousal caregiving for partners with dementia: A deductive literature review testing calasanti’s gendered view of care work. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 35, 759–787. doi:10.1177/0733464814542246 [DOI] [PubMed] [Google Scholar]
- Impett E. A., & Peplau L. A (2006). “His” and “her” relationships? A review of the empirical evidence. In A. L., Vangelisti, D., Perlman (Eds.), The Cambridge handbook of personal relationships (pp. 273–292). Cambridge, UK: Cambridge University. [Google Scholar]
- Jacobs M. T. Broese van Groenou M. I. Aartsen M. J., & Deeg D. J. H (2016). Diversity in older adults’ care networks: The added value of individual beliefs and social network proximity. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbw012 [DOI] [PubMed] [Google Scholar]
- Katz S., Ford A. B., Moskowitz R. W., Jackson B. A., Jaffe M. W. (1963). Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA, 185, 914–919. doi:10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kline R. B. (1998). Principles and practice of structural equation modeling. New York: The Guilford Press. [Google Scholar]
- Kramer B. J. (1997). Differential predictors of strain and gain among husbands caring for wives with dementia. The Gerontologist, 37, 239–249. doi:10.1093/geront/37.2.239 [DOI] [PubMed] [Google Scholar]
- Lawton M. P., Moss M., Kleban M. H., Glicksman A., Rovine M. (1991). A two-factor model of caregiving appraisal and psychological well-being. Journal of gerontology, 46, 181–189. doi:10.1093/geronj/46.4.P181 [DOI] [PubMed] [Google Scholar]
- Lin I. F., Fee H. R., Wu H. S. (2012). Negative and positive caregiving experiences: A closer look at the intersection of gender and relatioships. Family Relations, 61, 343–358. doi:10.1111/j.1741-3729.2011.00692.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutomski J. E. Baars M. E. Schalk B. W. M. Boter H. Buurman B. M. Den Elzen W. P. J., & Melis R. J. F (2013). The development of the older persons and informal caregivers survey minimum data set (TOPICS-MDS): A large-scale data sharing initiative. PloS One, 8, e81673. doi:10.1371/journal.pone.0081673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks N. F. Lambert J. D., & Choi H (2002). Transitions to caregiving, gender, and psychological well-being: A prospective U.S. national study. Journal of Marriage and Family, 64, 657–667. doi: 10.1111/j.1741-3737.2002.00657.x [Google Scholar]
- Mc Donnell E., Ryan A. (2013). Male caregiving in dementia: A review and commentary. Dementia (London, England), 12, 238–250. doi:10.1177/1471301211421235 [DOI] [PubMed] [Google Scholar]
- McFarland P. L., & Sanders S (1999). Male caregivers: Preparing men for nurturing roles. American Journal of Alzheimer’s Disease, 14, 278–282. doi:10.1177/153331759901400504 [Google Scholar]
- Miller B. (1990). Gender differences in spouse caregiver strain: Socialization and role explanations. Journal of Marriage and Family, 52, 311–321. doi:10.2307/353028 [Google Scholar]
- Muthén L. K., & Muthén B. O (2012). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pavalko E. K., Woodbury S. (2000). Social roles as process: Caregiving careers and women’s health. Journal of Health and Social Behavior, 41, 91–105. [PubMed] [Google Scholar]
- Pearlin L. I., Mullan J. T., Semple S. J., Skaff M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist, 30, 583–594. doi:10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Penning M. J., Wu Z. (2016). Caregiver stress and mental health: Impact of caregiving relationship and gender. The Gerontologist, 56, 1102–1113. doi:10.1093/geront/gnv038 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58, P112–P128. doi:10.1093/geronb/58.2.P112 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2006). Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 61, P33–P45. doi:org/10.1093/geronb/61.1.P33 [DOI] [PubMed] [Google Scholar]
- Roth D. L., Mittelman M. S., Clay O. J., Madan A., Haley W. E. (2005). Changes in social support as mediators of the impact of a psychosocial intervention for spouse caregivers of persons with Alzheimer’s disease. Psychology and Aging, 20, 634–644. doi:10.1037/0882-7974.20.4.634 [DOI] [PubMed] [Google Scholar]
- Russell R. (2007). The work of elderly men caregivers: From public careers to an unseen world. Men and Masculinities, 9, 298–331. doi: 10.1177/1097184X05277712 [Google Scholar]
- Savundranayagam M. Y. (2014). Receiving while giving: the differential roles of receiving help and satisfaction with help on caregiver rewards among spouses and adult-children. International Journal of Geriatric Psychiatry, 29, 41–48. doi:10.1002/gps.3967 [DOI] [PubMed] [Google Scholar]
- Savundranayagam M. Y., & Montgomery R. J. V (2010a). Impact of role discrepancies on caregiver burden among spouses. Research on Aging, 32, 175–199. doi:10.1177/0164027509351473 [Google Scholar]
- Savundranayagam M. Y., Montgomery R. J., Kosloski K. (2010b). A dimensional analysis of caregiver burden among spouses and adult children. The Gerontologist, 51, 321–331. doi:10.1093/geront/gnq102 [DOI] [PubMed] [Google Scholar]
- Statistics Netherlands (2016). Marriages and partnership registrations Retrieved on October 24, 2016, from http://statline.cbs.nl/Statweb/publication/?DM=SLEN&PA=37772eng&D1=0–53&D2=0,10,20,30,40,50,64-65&LA=EN&VW=T
- Stoller E. P. (1992). Gender differences in the experiences of caregiving spouses. In J. W., Dwyer, R. T., Coward (Eds.), Gender, families, and elder care (pp. 49–64). Thousand Oaks, CA: Sage. [Google Scholar]
- Suanet B. A. Broese van Groenou M. I., & Van Tilburg T. G (2012). Informal and formal home-care use among older adults in Europe: Can cross national differences be explained by societal context and composition?Ageing and Society, 32, 491–515. doi:10.1017/S0144686X11000390 [Google Scholar]
- van Exel N. J., Scholte op Reimer W. J., Brouwer W. B., van den Berg B., Koopmanschap M. A., van den Bos G. A. (2004). Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: A comparison of CSI, CRA, SCQ and self-rated burden. Clinical Rehabilitation, 18, 203–214. doi:10.1191/0269215504cr723oa [DOI] [PubMed] [Google Scholar]
- Verbakel E. Metzelthin S. F., & Kempen G. I. J. M (2016). Caregiving to older adults: Determinants of informal caregivers’ subjective well-being and formal and informal support as alleviating conditions. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbw047 [DOI] [PubMed] [Google Scholar]
- Wolff J. L., Kasper J. D. (2006). Caregivers of frail elders: updating a national profile. The Gerontologist, 46, 344–356. doi:10.1093/geront/46.3.344 [DOI] [PubMed] [Google Scholar]
- Yates M. E., Tennstedt S., Chang B. H. (1999). Contributors to and mediators of psychological well-being for informal caregivers. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 54, P12–P22. doi:10.1093/geronb/54B.1.P12 [DOI] [PubMed] [Google Scholar]
- Yee J. L., Schulz R. (2000). Gender differences in psychiatric morbidity among family caregivers: A review and analysis. The Gerontologist, 40, 147–164. doi:10.1093/geront/40.2.147 [DOI] [PubMed] [Google Scholar]
- Zarit S. H., Reever K. E., Bach-Peterson J. (1980). Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist, 20, 649–655. doi:org/10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.