Abstract
Lesions in multiple sclerosis can involve brain, optic nerve and spinal cord. We here report a patient of multiple sclerosis, who had unilateral vertical pendular nystagmus, because of simultaneous involvement of optic nerve and asymmetric brain stem lesions. This specific combination is rarely seen in other disorders, therefore can be considered as a distinctive neuro-opthalmoloical sign of multiple sclerosis.
Keywords: Brain-stem. multiple sclerosis, nystagmus, optic nerve
Eye movement's abnormalities are very common in multiple sclerosis (MS). MS has few characteristic neuro-ophthalmological signs like “internuclear ophthalmoplegia” and “one-and-a-half syndrome.” These specific signs are due to characteristic and discrete brainstem structures involved and propensity to have multiple lesions at a single time in MS. We have encountered a case of left eye vertical pendular nystagmus in MS, where the possible cause of this rare presentation was simultaneous involvement of left optic nerve and asymmetric brainstem lesions.
A 31-year-old male, with history of numbness in both upper limbs with complete recovery over 4–5 days 2 years back, presented now with unsteadiness of gait for 3 months and painless mild diminution of vision in the left eye for 15 days. Clinical examination revealed left eye diminished vision (6/12 by Snellen's chart) with relative afferent pupillary defect with partial optic disc atrophy. The right eye was normal. He had dysarthria with gait ataxia, with swaying toward the left side. Eye examination also showed isolated, unilateral pendular vertical nystagmus (UVPN) in primary gaze in the left eye [Video 1]. All deep tendon reflexes were brisk with bilateral planter response extensor. Visual evoked potential showed mildly reduced amplitudes in the left eye. Contrast-enhanced magnetic resonance imaging of brain and spine showed multiple ovoid T-2 and FLAIR hyperintense lesions in bilateral periventricular and juxtacortical white matter, thalamus, centrum semiovale, gangliocapsular region, and brainstem. Many of these lesions showed postcontrast peripheral open-ring enhancement. Cervical spine showed similar intramedullary lesions from C-3 to C-5 levels [Figure 1].
Figure 1.
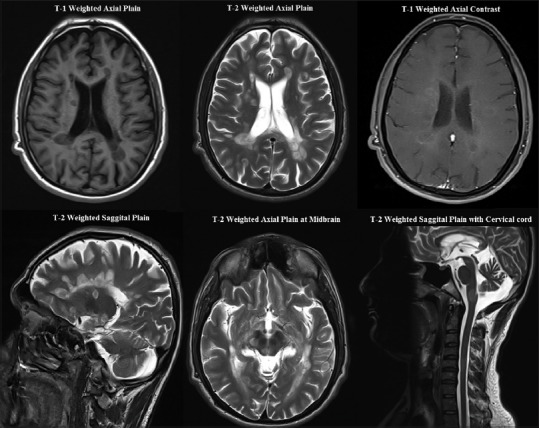
Magnetic resonance imaging of brain and cervical spine showing multiple ovoid lesions in bilateral periventricular and juxtacortical white matter, brainstem, and spinal cord, with few of these lesions showing postcontrast peripheral open-ring enhancement. These imaging findings are suggestive of multiple sclerosis
These findings were suggestive of relapsing-remitting MS. Workup for other demyelinating disorders and infective disorders were negative. The patient was started on intravenous methylprednisolone 1 g daily for 5 days. The vision of the patient improved to 6/9 and nystagmus disappeared gradually. Speech and gait also got better. The patient was started on interferon beta-1a 30 μg once weekly and asked to follow-up regularly.
DISCUSSION
Nystagmus is to-and-fro biphasic ocular oscillations. It can be jerk nystagmus where there is a slow drift of eyes and a quick corrective component, or pendular nystagmus, where eyes move with the same speed in both directions. Nystagmus is mostly a symmetric binocular disorder, but monocular eye oscillations and asymmetric binocular eye oscillations are also rarely seen. UVPN is a rare type of acquired monocular eye oscillations where only one eye moves to-and-fro with same speed in vertical direction.
UVPN has been earlier described in profound visual loss (Heimann-Bielschowsky [HB] phenomenon), MS, syphilis, optic chaisamal tumors, and brainstem infarction (midbrain or thalamic).[1,2,3] Patients with profound visual loss may have monocular vertical nystagmus characterized by slow, coarse, pendular, and variable amplitude movements known as HB phenomenon. Disruption of the fusional vergence mechanism or the monocular visual stabilization system is probable cause in this condition.[3] As this patient did not have profound visual loss, HB phenomenon can be ruled out. UVPN may also be caused by asymmetric brainstem disease as described by few studies.[4] However, it may be related to optic nerve dysfunction since it is found that larger oscillations correlate with greater optic neuropathy. Studies suggested that asymmetric signs of optic neuropathy were more common in patients with dissociated pendular nystagmus than in those with symmetric nystagmus. Role of asymmetric brainstem lesions, especially midbrain and thalamus, has been also evident in different case studies.[5] Although the cause of UVPN is still debatable, it has been postulated that UVPN is most likely caused by abnormal brainstem feedback circuits for eye position, which is calibrated by visual factors. This implies that any condition where both abnormal brainstem lesions and unilateral optic nerve lesions are temporally associated can result in UVPN. In our patient, unilateral lesions of midbrain affecting the rostral interstitial nucleus of the MLF in midbrain (which integrates the neural input into a final command for vertical gaze), along with unilateral optic neuropathy, may have culminated in vertical rather than horizontal or torsional nystagmus.
Therefore, in our patient, UVPN was seen as both optic neuropathy and asymmetric brainstem lesions were present. This combination of unilateral optic neuropathy and asymmetric brainstem lesions occurring simultaneously at a time is rare, that is why UVPN is a rare entity but is possible in MS. Other diseases where optic nerve and brainstem lesions can be seen are syphilis, Wernicke's encephalopathy, few vasculitis syndromes, and neuromylitis optica, but cooccurrence of both the lesions at a time together is very uncommon.
Hence, UVPN can be considered as distinguishing ophthalmological sign of MS as “internuclear ophthalmoplegia” or “one-and-a-half syndrome.” However, still, other more specific and targeted studies are required to support the above-mentioned proposition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.annalsofian.org
REFERENCES
- 1.Dehaene I, Van Zandycke M, Appel B. Acquired pendular nystagmus. Neuro Ophthalmol. 1987;7:297–300. [Google Scholar]
- 2.Schulman JA, Shults WT, Jones JM., Jr Monocular vertical nystagmus as an initial sign of chiasmal glioma. Am J Ophthalmol. 1979;87:87–90. doi: 10.1016/0002-9394(79)90197-1. [DOI] [PubMed] [Google Scholar]
- 3.Davey K, Kowal L, Friling R, Georgievski Z, Sandbach J. The heimann-bielscholwsky phenomenon: Dissociated vertical nystagmus. Aust N Z J Ophthalmol. 1998;26:237–40. doi: 10.1111/j.1442-9071.1998.tb01318.x. [DOI] [PubMed] [Google Scholar]
- 4.Barton JJ, Cox TA. Acquired pendular nystagmus in multiple sclerosis: Clinical observations and the role of optic neuropathy. J Neurol Neurosurg Psychiatry. 1993;56:262–7. doi: 10.1136/jnnp.56.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall RS, Sacco RL, Kreuger R, Odel JG, Mohr JP. Dissociated vertical nystagmus and internuclear ophthalmoplegia from a midbrain infarction. Arch Neurol. 1991;48:1304–5. doi: 10.1001/archneur.1991.00530240110032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


