Abstract
ABO incompatibility and other alloantibodies have emerged as a significant cause of hemolytic disease of fetus and newborn (HDFN), leading to neonatal morbidity and mortality. We report three cases of severe ABO-HDFN where blood exchange transfusions (ETs) were required in neonates with hyperbilirubinemia. Blood grouping (ABO/RhD) was performed using conventional tube technique. The antibody screen was done using commercial three-cell panel (Bio-Rad ID-Diacell-I-II-III, Switzerland) by gel technique. Direct antiglobulin test (DAT) on neonatal sample and compatibility testing were also done by gel technique. Elution on DAT-positive sample was performed using “heat elution” method. All the three neonates were A RhD positive and were born to O RhD-positive mothers who were negative for antibody screen. Their DAT was positive (2+) and the elution of neonatal red cells yielded a positive reaction with A cells which was suggestive of anti-A antibody. The maternal anti-A (immunoglobulin G) antibody titers were high: 512 and 1024 (in two cases). The total serum bilirubin (mg/dl) of the three neonates was 22, 27, and 25 which came down significantly after they received ETs. Severe ABO-HDFN may occur in neonates born to mother with high titer ABO antibodies which can be effectively managed with ET.
Keywords: ABO hemolytic disease of fetus and newborn, exchange transfusion, hemolytic disease of fetus and newborn, neonatal jaundice
Introduction
Hemolytic disease of fetus and newborn (HDFN), a condition which involves transplacental passage of maternal antibodies leading to immune hemolysis of neonatal red cells, is an important cause of neonatal morbidity and mortality. In recent years, ABO incompatibility and other alloantibodies have emerged as a significant cause of HDFN.[1,2] Although quite common and frequently benign in its clinical course, delay in recognizing ABO incompatibility often leads to significant hyperbilirubinemia that may require intervention. Herein, we report three cases of severe HDFN due to ABO incompatibility where blood exchange transfusions (BETs) had to be undertaken, to decrease the high serum bilirubin levels.
Materials and Methods
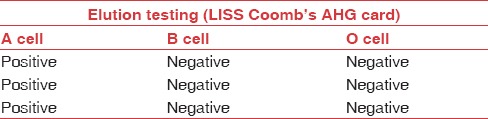
The ABO/RhD grouping was performed using conventional tube technique. The antibody screen was done using commercial three-cell panel (Bio-Rad ID-Diacell-I-II-III, Switzerland) by gel technique. Direct antiglobulin test (DAT) on neonatal sample was done by gel technique (LISS-Coombs AHG cards, Biorad, Switzerland). Elution on DAT-positive sample was performed using “heat elution” method.[3] The eluates were subsequently tested with A1 cell, B cell, and O cell by gel technique. The subclass characterization of immunoglobulin G (IgG) antibodies in DAT-positive samples was done using gel technique (ID-DAT IgG1-IgG3, Bio-Rad, Switzerland). Anti-A antibody titer in the mother's sample was done using tube technique by preparing serial doubling dilutions of serum. The room temperature (22°C) reading after centrifugation with A1 cells was taken as IgM titer and the results obtained after indirect antiglobulin test phase testing (at 37°C) were considered as IgG titer. The end point for titer was 1+ agglutination.[3] Compatibility testing between donor red blood cells (RBCs) and maternal serum was done by gel technique. All the packed RBC units used were reconstituted in AB plasma.
Results
Tables 1 and 2 summarize the detailed findings of the immunohematology workup of the three cases.
Table 1.
Clinical details and immunohematology findings of the neonates and their parents
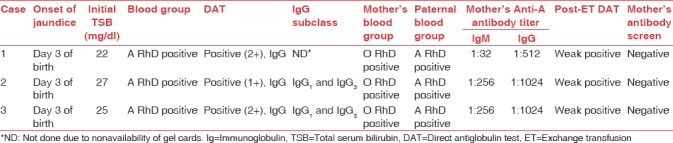
Table 2.
Results of eluate testing
Case 1
Blood sample of a 3-day-old female neonate (birth weight 2.5 kg) with the diagnosis of neonatal jaundice (NNJ) with encephalopathy was received in immunohematology laboratory for blood group and DAT along with a requisition of 2 PRBC units for BET. History revealed that she was the first child in the family. Onset of jaundice was on the 3rd day of life. The total serum bilirubin (TSB) of the infant was 22 mg/dl. BET was done with two O RhD-positive PRBC units compatible with the mother's and baby's blood sample by gel technique. The TSB value decreased to 9.8 mg/dl by the next day.
Case 2
The second case was a 4-day-old male neonate (birth weight − 3.5 kg) with the diagnosis of NNJ and TSB value of 27 mg/dl. There was a history of jaundice in elder sibling (blood group not known) as well. Onset of jaundice was on day 3 of life for which phototherapy was given. For the index case, two BETs were done at the interval of 24 h with O RhD-negative PRBC unit, as O RhD-positive PRBC unit within 5 days of collection was not available at that time. Post-BET, the DAT was weak positive and the hyperbilirubinemia subsided in the next 24 h.
Case 3
The third patient was a 4-day-old female neonate (birth weight - 2.5 kg), with a TSB value of 25 mg/dl. The hemoglobin was 5 g/dl and the hematocrit was 15%. Peripheral blood film (PBF) showed microcytosis and spherocytosis. There was no history of jaundice in elder sibling (boy, 2 years of age, blood group O RhD positive) at birth. Post-BET, serial 8-hourly TSB values were – 20 mg/dl, 15 mg/dl, 11 mg/dl, and 10 mg/dl. Post-BET, the DAT was weak positive.
Discussion
HDFN due to non-anti-D antibodies is being increasingly diagnosed due to increasing awareness among the clinicians regarding the screening of RhD-negative antenatal women and use of anti-D prophylaxis.[1,2] ABO hemolytic disease is relatively lesser recognized entity as routine antenatal screening for high-titer anti-A and anti-B is not recommended due to poor reproducibility. In addition, HDFN due to ABO antibodies is rarely severe enough to warrant BET.[4] The reported incidence of ABO-incompatible pregnancies is 15%–25%.[5] In a study from southern India by Bhat and Kumar,[5] ABO incompatibility was seen in 17.3% (151/878) of pregnancies, out of which 50.4% were O-A- and 49.6% were O-B-incompatible pregnancies. Forty six (30.4%) required phototherapy, none required ET. In another study by Usha and Sulochana.[6] including 100 antenatal O group mothers, ABO-HDFN was encountered in three neonates with high titers of both IgG and IgM anti-A and anti-B antibodies. In our three cases of ABO-HDFN, BET was required due to severe hyperbilirubinemia (>20 mg/dl) in the first 72 h of life. All the three cases were of O-A incompatibility and had a positive DAT with IgG as the antibody specificity. IgG subclass was found to be IgG1 and IgG3 in two of the three cases. It is advocated that lysis of RBCs in ABO-incompatible HDFN is extravascular mediated by macrophages and complement is not activated.[7] It is due to low level of A and B antigenic expression on neonatal red cells and low complement levels in serum.[8] Antibody screen on maternal serum was negative, ruling out other irregular red cell alloantibodies. IgG anti-A titer in maternal serum was 512 in one and 1024 in the other two cases. Eluate prepared from neonatal samples by heat elution showed reactivity with A1 cells in the antihuman globulin phase.
The clinical severity in ABO-HDFN varies from mild to moderate hyperbilirubinemia that can be managed by phototherapy in most of the cases. Rarely, BET may be required. The extent of involvement depends on the amount of antibody that crosses the placenta. Deng et al.[9] reported an unusual case of significant ABO-HDFN presenting with severe anemia in a neonate with a cis-AB phenotype born to a group O mother. The baby was treated with phototherapy, intravenous Ig (IVIg), and recombinant human erythropoietin (rhEPO). Haque and Rahman[10] reported that severe HDFN in a neonate with A1B blood group (mother's blood group B RhD positive) requiring two BETs. ABO-HDFN leading to hydrops has been reported in two case reports.[11,12]
A high index of suspicion is required for early diagnosis of ABO-HDFN. According to Procianoy et al., DAT in cord blood, elution test, and evidence of hemolysis (rise in bilirubin concentration, anemia, reticulocytosis, and spherocytosis on PBF) may help in early diagnosis.[13] Sarici et al. prospectively determined the critical TSB level to predict significant hyperbilirubinemia and severe hemolytic disease in healthy term newborns with ABO incompatibility. They concluded that TSB levels of 4 mg/dL and 6 mg/dL at the sixth hour of life predicted the development of significant hyperbilirubinemia and severe hemolytic disease of the newborn, respectively.[14]
Other treatment modalities include IVIg and rhEPO. The efficacy of IVIg in ABO-HDFN has been found to be variable.[1,15] Its potential benefits should be weighed against the potential risks, especially necrotizing enterocolitis, thrombosis, and IVIg-mediated hemolysis from anti-A and anti-B antibodies found in IVIg. With the advent of modern highly effective light emitting diode (LED) phototherapy systems and potential adverse effects of IVIg, its role has become questionable.
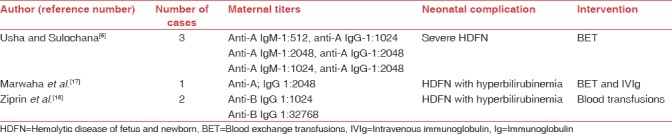
Ziprin et al. while reporting severe anemia secondary to ABO incompatibility due to IgG anti-B antibodies found high titers in both their cases.[16] Interestingly, the first patient had a twin pregnancy and a high titer of IgG anti-B antibodies (1024). Both the twins were managed with phototherapy, folic acid supplementation and blood transfusions. The second patient, who presented with sickle cell crisis requiring BET and a very high IgG anti-B antibody titer of 32728, delivered a baby who developed hemolytic anemia in the neonatal period which was successfully managed with blood transfusions. Similarly, Marwaha et al.[17] reported a case of severe hemolytic anemia in a neonate due to high titers of IgG anti-A antibodies (2048), who responded favorably to BET and IVIg. None of the authors reported the subclass of IgG antibodies. Table 3 describes the cases of severe ABO-HDFN requiring significant medical intervention, as reported in literature.
Table 3.
Cases of severe ABO hemolytic disease of fetus and newborn reported by other authors
ABO-HDFN, usually a mild condition, has been implicated in complications such as neonatal cholestasis if not diagnosed appropriately.[18] If maternal and neonatal ABO incompatibility is present, red cell transfusions should be compatible with both maternal and neonatal serum. Transfusion of red cells identical only to neonate can lead to hemolysis due to stronger ABO antigen expression on adult donor cells. Thus, there is a need to increase awareness towards ABO-HDFN for optimizing care in terms of early diagnosis and adequate monitoring. Larger case series are required to determine the true prevalence of ABO-HDFN as these reported cases may only be the tip of the iceberg. In addition, determination of IgG subclass is equally important as only IgG1 and G3, as seen in the present cases, appear to be pathogenic. Thus, a high-risk approach should be adopted if there is a history of ABO-HDFN in previous pregnancies or if there is ABO incompatibility between the partners.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nasseri F, Mamouri GA, Babaei H. Intravenous immunoglobulin in ABO and rh hemolytic diseases of newborn. Saudi Med J. 2006;27:1827–30. [PubMed] [Google Scholar]
- 2.Basu S, Kaur R, Kaur G. Hemolytic disease of the fetus and newborn: Current trends and perspectives. Asian J Transfus Sci. 2011;5:3–7. doi: 10.4103/0973-6247.75963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saran RK, editor. Transfusion Medicine Technical Manual. 2nd ed. New Delhi: Mehta Offset Pvt. Ltd; 2003. Preparation of Solution and Methods; pp. 305–40. [Google Scholar]
- 4.White J, Qureshi H, Massey E, Needs M, Byrne G, Daniels G, et al. Guideline for blood grouping and red cell antibody testing in pregnancy. Transfus Med. 2016;26:246–63. doi: 10.1111/tme.12299. [DOI] [PubMed] [Google Scholar]
- 5.Bhat YR, Kumar CG. Morbidity of ABO haemolytic disease in the newborn. Paediatr Int Child Health. 2012;32:93–6. doi: 10.1179/2046905512Y.0000000002. [DOI] [PubMed] [Google Scholar]
- 6.Usha KK, Sulochana PV. Detection of high risk pregnancies with relation to ABO haemolytic disease of newborn. Indian J Pediatr. 1998;65:863–5. doi: 10.1007/BF02831348. [DOI] [PubMed] [Google Scholar]
- 7.Brouwersm HA, Overbeeke MA, Huiskes E. Complement is not activated in ABO-haemolytic disease of the newborn. Br J Haernatol. 1988;68:363–6. doi: 10.1111/j.1365-2141.1988.tb04215.x. [DOI] [PubMed] [Google Scholar]
- 8.Klein HG, Anstee DJ, editors. Mollison's Blood Transfusion in Clinical Medicine. 11th ed. Oxford: Hemolytic Disease of Fetus and Newborn; 2002. Hemolytic Disease of Fetus and Newborn; pp. 496–545. [Google Scholar]
- 9.Deng ZH, Seltsam A, Ye YW, Yu Q, Li Q, Su YQ, et al. Haemolytic disease of fetus and newborn caused by ABO antibodies in a cis-AB offspring. Transfus Apher Sci. 2008;39:123–8. doi: 10.1016/j.transci.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Haque KM, Rahman M. An unusual case of ABO-haemolytic disease of the newborn. Bangladesh Med Res Counc Bull. 2000;26:61–4. [PubMed] [Google Scholar]
- 11.McDonnell M, Hannam S, Devane SP. Hydrops fetalis due to ABO incompatibility. Arch Dis Child Fetal Neonatal Ed. 1998;78:220–1. doi: 10.1136/fn.78.3.f220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goraya J, Basu S, Sodhi P, Mehta S. Unusually severe ABO hemolytic disease of newborn. Indian J Pediatr. 2001;68:285–6. doi: 10.1007/BF02723208. [DOI] [PubMed] [Google Scholar]
- 13.Procianoy RS, Giacomini CB, Farina DM, Mollin GA, Winckler MI, Silveira MB, et al. Early diagnosis of ABO haemolytic disease of the newborn. Eur J Pediatr. 1987;146:390–3. doi: 10.1007/BF00444945. [DOI] [PubMed] [Google Scholar]
- 14.Sarici SU, Yurdakök M, Serdar MA, Oran O, Erdem G, Tekinalp G, et al. An early (sixth-hour) serum bilirubin measurement is useful in predicting the development of significant hyperbilirubinemia and severe ABO hemolytic disease in a selective high-risk population of newborns with ABO incompatibility. Pediatrics. 2002;109:e53. doi: 10.1542/peds.109.4.e53. [DOI] [PubMed] [Google Scholar]
- 15.Keir AK, Dunn M, Callum J. Should intravenous immunoglobulin be used in infants with isoimmune haemolytic disease due to ABO incompatibility? J Paediatr Child Health. 2013;49:1072–8. doi: 10.1111/jpc.12440. [DOI] [PubMed] [Google Scholar]
- 16.Ziprin JH, Payne E, Hamidi L, Roberts I, Regan F. ABO incompatibility due to immunoglobulin G anti-B antibodies presenting with severe fetal anaemia. Transfus Med. 2005;15:57–60. doi: 10.1111/j.1365-3148.2005.00549.x. [DOI] [PubMed] [Google Scholar]
- 17.Marwaha N, Dhawan HK, Thakral B, Kaur R, Basu S, Parmar V, et al. Severe ABO hemolytic disease of newborn with a positive direct antiglobulin test. Indian J Pathol Microbiol. 2009;52:292. doi: 10.4103/0377-4929.48958. [DOI] [PubMed] [Google Scholar]
- 18.Jain A, Poddar U, Elhence P, Tripathi A, Shava U, Yachha SK, et al. Cholestasis in a neonate with ABO haemolytic disease of newborn following transfusion of ABO group-specific red cells compatible with neonatal serum: Inspissated bile syndrome. Blood Transfus. 2014;12:621–3. doi: 10.2450/2014.0099-14. [DOI] [PMC free article] [PubMed] [Google Scholar]


