Abstract
Background
This study aimed to use a portable ultrasound method to quantitatively measure skin thickness and to compare leg edema in obese and non-obese pregnant women.
Material/Methods
Thirty-six pregnant women (17 primiparas and 19 multiparas) at 27/28 and 37/38 weeks of pregnancy, with and without leg edema, had their lower leg skin thickness measured using a B-scan portable ultrasonography device (72 legs and maximum of 98 measurements). Measurements were compared between women who were obese prior to pregnancy, with a body mass index (BMI) ≥25 kg/m2 and non-obese with a BMI <25 kg/m2.
Results
Skin thickness of the legs in pregnant women with edema was significantly increased compared with that in pregnant women without edema (6.4±0.3 mm vs. 4.6±0.4 mm) (p=0.0001). There was a significant correlation between the degree of pitting edema and skin thickness in all edematous legs (ρ=0.56; n=98; p<0.0001). The cutoff level of edema measured by portable ultrasound in non-obese pregnant women was 4.7 mm (sensitivity 83.9%, specificity 66.7%) and was 7.5 mm in obese pregnant women. Obese pregnant women with edema had a significantly increased leg skin thickness compared with non-obese pregnant women with edema (11.3±1.3 mm vs. 5.7±0.2 mm) (p<0.0001).
Conclusions
Portable ultrasonography is a reliable method of quantitatively measuring skin thickness of the lower leg in edema associated with pregnancy. The thickness of the skin in obese pregnant women with edema can be expected to be significantly increased compared with non-obese pregnant women with edema.
MeSH Keywords: Edema, Leg, Subcutaneous Fat, Ultrasonography
Background
Leg and foot edema during pregnancy is very common, occurs in about 80% of all pregnancies, and is regarded as normal when it is not associated with pre-eclampsia [1]. Changes in the blood chemistry during pregnancy also cause some fluid to shift into the tissue, and lower limb edema can result as the growing uterus places pressure on the pelvic veins and vena cava, which slows the return of blood from the legs and feet, causing it to pool into the subcutaneous tissues of the legs and feet [2]. For these reasons, edema is most likely to occur in women during the third trimester of pregnancy and is known as physiologic edema. Lower limb edema can cause pain and difficulty in walking, or ankle stiffness [3]. Less commonly, leg swelling during pregnancy results from pre-eclampsia, deep vein thrombosis (DVT), and cellulitis, which are serious medical conditions [4]. Therefore, a reliable and objective method is required for the early diagnosis of leg edema during pregnancy to allow for early treatment and to distinguish physiological edema from more serious conditions.
Pitting edema is a characteristic of edema in pregnancy, and is detected when pressure that is applied to the skin leaves a depression when removed. This method of detection of lower limb edema is a qualitative diagnostic method performed during pregnancy. There are also quantitative techniques that may also be used to assess leg edema, including measurement of leg circumference, which can be assessed easily by using a tape measure, or with an improved form of tape measure, the Leg-O-Meter [5]. However, the leg circumference is not always directly correlated with the leg volume, which can be most easily assessed by water displacement leg volumetry [6]. Also, these methods for assessing leg edema lack sensitivity and are of most value in the assessment of relative changes in leg edema. Other approaches, such as rheoplethysmography, strain gauge plethysmography, and air plethysmography, can be used to assess changes associated with limb edema, but these methods measure the venomuscular pump or venous outflow rather than the volume [6]. Other approaches to the measurement of leg edema include optoelectronic assessments, computed tomography (CT) imaging, magnetic resonance imaging (MRI), dual X-ray absorptiometry, and measurement of electric and electromagnetic waves [7] and bioelectrical impedance [8]. However, these methods are expensive and many of them have not been validated.
Recently, a three-dimensional system for measuring the volume and circumference using a halogen light grid projection pattern method (GRASP) (Techno Arts Laboratory, Tokyo, Japan) has been developed and the images are integrated to calculate the coordinates [9,10]. In this technique, multiple grid patterns of halogen light are projected onto the leg from two directions and require a large device that is usually sited at a specific location. There remains a need for doctors or midwives to examine pregnant women for leg and foot edema easily and quickly in the outpatient clinic so that the effects of treatment for edema can be assessed easily.
This study aimed to use a portable ultrasound method to quantitatively measure skin thickness and to compare leg edema in obese and non-obese pregnant women. The skin thickness was the distance between the epidermis, dermis, and subcutaneous layers.
Material and Methods
Study subjects and study approval
Thirty-six pregnant women (17 primiparas and 19 multiparas) who attended an outpatient clinic in the Department of Obstetrics and Gynecology, Nagahama City, Shiga, Japan were selected over a six-month period, between April 2017 and September 2017. The study protocol was approved by the Ethics Committee of the University of Shiga Prefecture (No 571), and all pregnant women provided their written informed consent prior to study entry.
Clinical characteristics of the study participants
The mean age of the women, ± standard error of the mean (SEM), was 30.2±4.87 years (range, 20–41 years). The body mass index (BMI) prior to pregnancy was calculated from the pre-pregnancy height (in metres) and weight (in kg). The study participants were divided into two groups, the non-obese group (BMI <25 kg/m2) and the obese group (BMI ≥25 kg/m2), and the mean BMI before pregnancy was 21±3.1 kg/m2. Weekly laboratory investigations included measurement of the blood hematocrit, hemoglobin, and albumin, and urine protein levels.
Measurements of the skin thickness
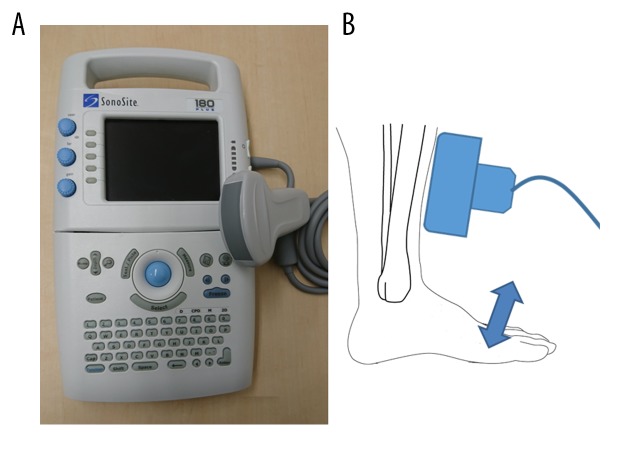
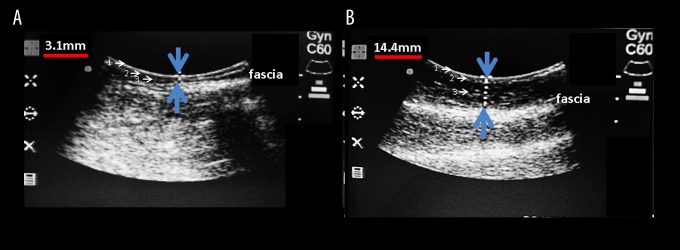
The thickness of the skin of the leg was measured using a B-scan portable ultrasonography device, the SonoSite 180 plus (SonoSite, Inc. WA, USA) (Figure 1A). The skin thickness measurements included the epidermis, dermis, and subcutaneous tissue above the fascia and muscle of both legs. Ultrasonography was performed at 27/28 (27 or 28) and/or 37/38 (37 or 38) weeks of pregnancy (once or twice). Fifty-two legs of 13 women were measured twice at both 27/28 and 37/38 weeks, six legs of three women were measured at 27/28 weeks, and 40 legs of 20 women were measured once at 37/38 weeks. An ultrasonography probe (5 MHz) was placed on the skin of the lower leg at the specific point, including at 6 cm from the upper part of the medial malleolus and 1 cm inside the anterior border of the tibia (Figure 1B). This point was chosen for their ease of use in the ultrasonography technique as at the specific measurement point, there were few other structures between the skin and bone with a thin portion of the soleus muscle. When the skin thickness was being measured, the women repeatedly performed anteflexion and retroflexion of the ankle (Figure 1B). Because the skin thickness measurements included the epidermis, dermis, and subcutaneous layers above the fascia and muscle, movements of the ankle resulted in the movement of the fascia and muscle layers, but not the skin, which allowed identification of the skin layer. Using ultrasonography, the distance between the skin surface and the upper part of the fascia was measured as the skin thickness, which included the epidermis, dermis, and subcutaneous tissue layer (Figure 2A, 2B).
Figure 1.
The portable ultrasonography device and its use in measuring skin thickness. (A) The portable ultrasonography device. (B) The lower edge of the probe was set at 6 cm from the upper part of the medial malleolus and 1 cm inside the anterior border of the tibia. During measurement of the skin thickness, the woman repeatedly performed anteflexion and retroflexion of the ankles.
Figure 2.
Ultrasonography measurements of skin thickness in women with and without leg edema. (A) Using ultrasonography, the distance between the skin surface and the fascia was measured as the skin thickness (between the epidermis, dermis, and subcutaneous layers). The skin thickness was 3.1 mm in a pregnant woman without edema. (B) The skin thickness was 14.4 mm in a pregnant woman with edema. 1=the skin epidermal layer; 2=the skin dermal layer; 3=the subcutaneous layer.
Assessment and grading of edema of the lower leg
At the same time as the quantitative measurements of skin thickness were being performed, a qualitative evaluation of the degree of physiologic pitting edema of the skin of the lower leg was performed. Finger pressure was applied to the swollen area of skin to determine whether an indentation formed that persisted after removal of pressure. The grades of pitting edema were as follows: Grade 0, negative for edema, with no persisting indentation after release of finger pressure; Grade 1, mild pitting edema (slight indentation) that disappeared within 10 seconds; Grade 2, moderate pitting edema that disappeared after 10–15 seconds; Grade 3, severe pitting edema that lasted for more than 15 seconds, after release of finger pressure. Also, bilateral lower leg circumference was measured using a tape measure as a conventional method of assessment of lower leg edema, with measurements taken at the specific point described above.
Statistical analysis
Statistical analysis was performed using the JMP Pro statistical software program, version 12 (SAS Institute Japan, Tokyo, Japan). The results were presented as the mean ±SEM and compared using a one-way analysis of variance (ANOVA). The required sample size was calculated based on analysis of the mean ±SEM measurements of the thickness of the skin of the legs in 10 women with edema vs. 10 women without edema (α level, 5%; power, 90%). Receiver operating characteristic (ROC) curves were prepared using logistic regression analysis and cutoff levels were calculated using Youden’s index. Correlations between the measurement of skin thickness by ultrasonography and the degree of pitting edema were calculated using a rank correlation analysis and compared using Spearman’s rank correlation coefficient. The correlation between the difference in the bilateral lower leg circumference, the difference in the bilateral lower leg skin thickness and the hematocrit at 37/38 and 27/28 weeks of pregnancy was calculated by multivariate correlation analysis. The coefficient of each correlation was compared using Pearson’s correlation coefficient. P-values of <0.05 were considered to indicate statistical significance.
Results
The skin thickness of the leg in pregnant women with edema and pregnant women without edema
Thirty-six pregnant women (17 primiparas and 19 multiparas) at 27/28 and 37/38 weeks of pregnancy, with and without leg edema, had their lower leg skin thickness measured using a B-scan portable ultrasonography device (72 legs and maximum of 98 measurements). Qualitative evaluation of pitting edema of the skin of the lower leg used the pressure method (positive: Grade ≥1). Using ultrasonography, the distance between the skin surface and the fascia, between the epidermis, dermis, and subcutaneous layers, was used as the measurement of skin thickness in the legs of pregnant women without edema (Figure 2A) and in legs with edema (Figure 2B). Skin thickness of the legs in pregnant women with edema was significantly increased compared with that in pregnant women without edema (6.4±0.3 mm vs. 4.6±0.4 mm) (p=0.0001). (Figure 3).
Figure 3.
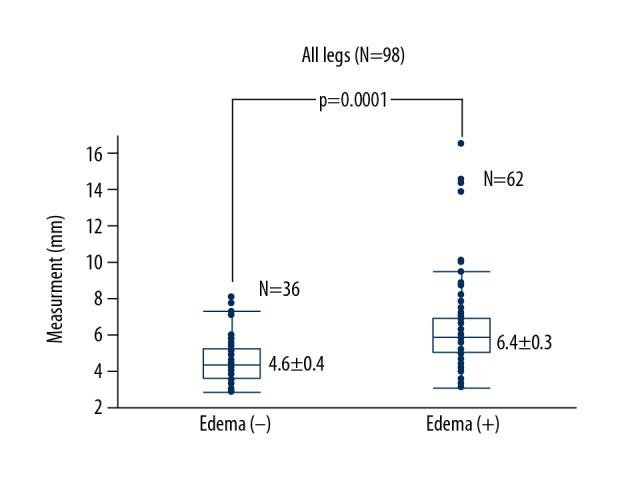
Comparison of the thickness of the skin of the leg with and without edema. The thickness of the skin of the leg with edema was significantly increased compared with the skin of the leg without edema (6.4±0.3 mm vs. 4.6±0.4 mm) (p=0.0001)
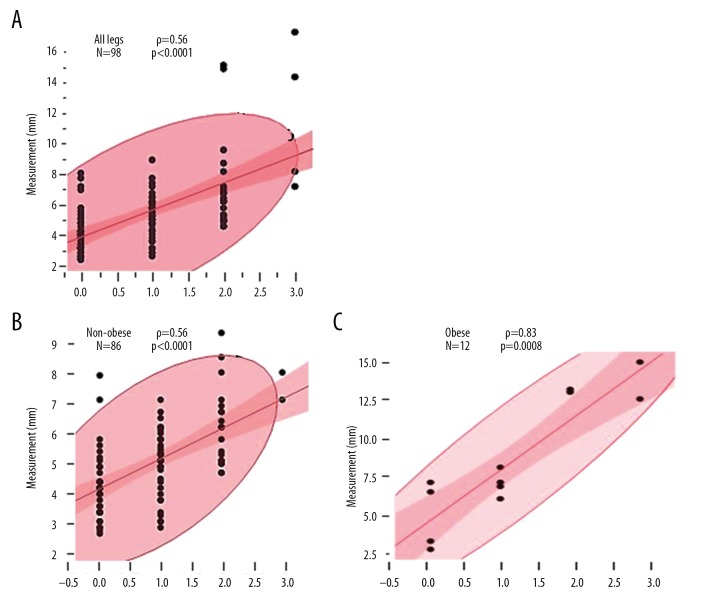
The relationship between the skin thickness on B-scan ultrasonography and the degree of pitting edema in non-obese and obese pregnant women
The degree of pitting edema was graded qualitatively (Grade 0, 1, 2, and 3) and compared with the quantitative skin thickness measurements from ultrasonography. Using Spearman’s correlation on the ranked values of the data, there was a significant correlation between the degree of pitting edema and the skin thickness of all legs (ρ=0.56, n=98) (p<0.0001) (Figure 4A). There was a significant correlation between the degree of pitting edema on skin pressure and the skin thickness measured on ultrasonography in the non-obese group (ρ=0.56, n=86) (p<0.0001) (Figure 4B) and in the obese group (ρ=0.83, n=12) (p=0.0008) (Figure 4C).
Figure 4.
Correlation between the degree of pitting edema and the skin thickness in the legs of obese and non-obese pregnant women. (A) There was a significant correlation between the degree of pitting edema and the skin thickness on ultrasonography in all legs (ρ=0.56; n=98; p<0.0001). (B) There was a significant correlation between the degree of pitting edema and the skin thickness in the legs of non-obese women (ρ=0.56; n=86; p<0.0001). (C) There was a significant correlation between the degree of pitting edema and the skin thickness in the legs of obese women (ρ=0.83; n=12; p=0.0008).
The thickness of the skin of the leg in non-obese and obese pregnant women
There was no significant difference in the thickness of the skin of the leg between non-obese and obese pregnant women in the non-edematous group (4.5±0.2 mm vs. 5.3±1.8 mm) (Figure 5). However, the thickness of the skin of the leg was significantly increased in obese pregnant women when compared with non-obese pregnant women in the edematous group (5.7±0.2 mm vs. 11.3±1.3 mm; 1.97-fold) (p<0.0001).
Figure 5.
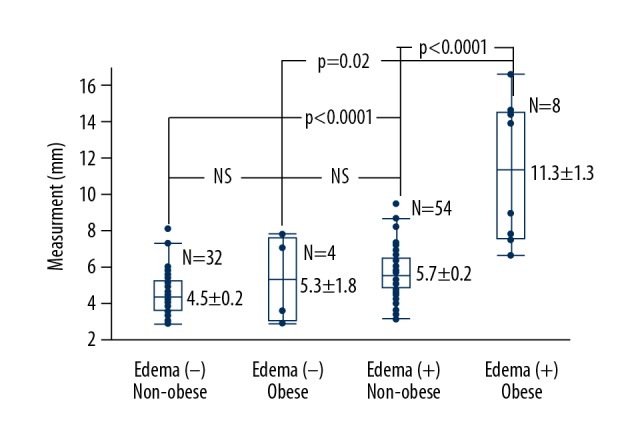
The thickness of the skin of the leg between non-obese and obese women with and without leg edema. No significant difference was found in the thickness of the skin of the leg between non-obese and obese women without leg edema (4.5±0.2 mm vs., 5.3±1.8 mm, NS). However, the thickness of the skin of the leg was significantly increased in obese women compared with non-obese women in the edematous group (5.7±0.2 mm vs. 11.3±1.3 mm; 1.97-fold; p<0.0001).
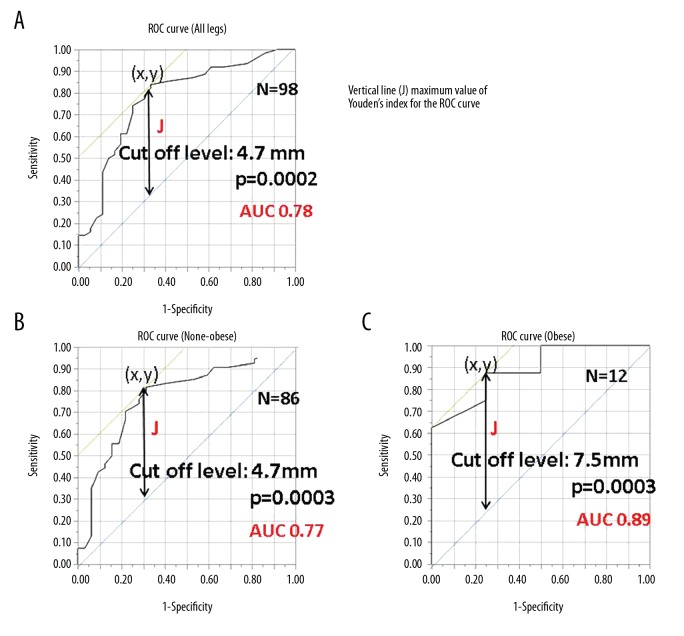
Receiver operating characteristic (ROC) curves and cutoff levels of the skin measurements, sensitivity, and specificity of the ultrasound method
The plot of the ROC curve was used to determine the sensitivity (the true positive rate, on the Y-axis) and 1 – the specificity (the false-positive rate, on the X-axis) across a series of cutoff points (Figure 6A–6C). Data from the use of the Youden index of the maximal vertical distances from the line of equality to the point (x, y) are shown in Figure 6A–6C. The farthest distance between two points in each ROC curve was calculated as the cutoff level. Using ultrasonography, the cutoff level for the measurement of skin edema compared with non-edema in all legs was 4.7 mm, with a sensitivity of 83.9% (52/62), a specificity of 66.7% (24/36), and an accuracy of 77.6% (76/98) (Figure 6A). The cutoff level in non-obese pregnant women was 4.7 mm, with a sensitivity of 81.5% (44/54), a specificity of 71.9% (23/32), and an accuracy of 77.9% (67/86) (Figure 6B). The cutoff level in obese pregnant women was 7.5 mm, with a sensitivity of 87.5% (7/8), a specificity of 75.0% (3/4), and an accuracy of 83.3% (10/12) (Figure 6C).
Figure 6.
Receiver operating characteristic (ROC) curves and cutoff measurements of edema and non-edema in obese and non-obese women. (A) The receiver operating characteristic (ROC) curve was drawn by logistic analysis. The cutoff level of edema and non-edema measurements using ultrasonography in all legs was 4.7 mm. (B) The cutoff level of edema and non-edema measurements using ultrasonography in non-obese women was 4.7 mm. (C) The cutoff level of edema and non-edema measurements using ultrasonography in obese women was 7.5 mm.
Comparison of the measurement values obtained at 37/38 and 27/28 weeks of pregnancy from multivariate analysis
The differences of five measurements were compared, including the bilateral leg skin thickness, the bilateral leg circumferences, and the hematocrit level, using multivariate analysis (Figure 7). The differences between the left and right circumference measurements at 37/38 and 27/28 weeks were positively correlated (r=0.60, p=0.03), and the differences between the left and right leg skin thickness measured using ultrasonography at 37/38 and 27/28 weeks were positively correlated (r=0.61, p=0.03). Other measurements showed no significant correlation.
Figure 7.
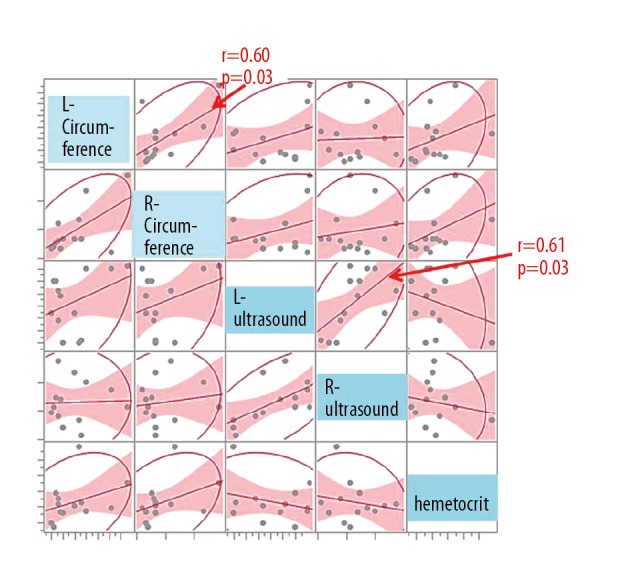
Left and right leg thickness measurements using ultrasonography at 37/38 and 27/28 weeks of pregnancy. The differences of five measurements between 37/38 and 27/28 weeks of pregnancy were compared using multivariate correlation analysis, in all combinations. The differences between the left and right leg circumference measurements at 37/38 and 27/28 weeks were positively correlated (r=0.60, p=0.03) and the differences between the left and right leg skin thickness measured using ultrasonography at 37/38 and 27/28 weeks were positively correlated (r=0.61, p=0.03).
Discussion
Previously published studies on the measurement of the thickness of the skin of the leg using ultrasonography have been reported in patients with chronic venous disease [11], lymphedema [12,13], synovitis with pitting edema syndrome (RS3PE) [14], and age-related diurnal changes of dermal edema [15]. Most of these previous studies have shown varied ultrasound patterns of subcutaneous edema. There have been previously published studies that have used ultrasound to measure dermal thickness [16–18]. One previously published report described the use of ultrasonography in the measurement of the dermal and subcutaneous skin thickness of the forehead and tibia in the evaluation of thigh pressure cuffs [19]. Another study described an increase in subepidermal edema in people with diabetic neuropathy and ulceration using an ultrasound scanner [20]. To our knowledge, the present study was the first to use portable ultrasonography to measure and compare the thickness of the skin of the leg, including the epidermis, dermis, and subcutaneous tissue, of pregnant women with and without edema. Also, the method used described how to identify the skin layers by the use of anteflexion and retroflexion ankle movements, as the fascia and muscle layers moved, while the skin layer did not.
Edema affects about three-quarters of pregnant women, usually from weeks 22–27 of pregnancy. Leg and foot edema occurs when circulating blood volume increases to provide oxygen and nutrients to the mother and growing fetus, and due to the increase in intrapelvic pressure, from the gravid uterus, on the pelvic veins and vena cava, which returns blood from the lower limbs to the heart [2,21]. The pressure slows the return of blood from the legs and feet, causing it to pool, which forces fluid from the veins into the tissues of the legs and feet. Therefore, edema is most likely to affect women during the third trimester of pregnancy.
Leg and foot edema is a frequent and unpleasant accompaniment to pregnancy, causing pain on walking in severe cases [22]. Therefore, this study focused on the measurement of the thickness of the skin of the leg using ultrasonography to diagnose leg edema easily and accurately at an early stage. In the present study, the skin thickness was measured between the epidermis, dermis, and subcutaneous tissue, which can be difficult to distinguish on ultrasound. However, the identification of the subcutaneous fascia at the selected points of measurement provided a high-echo landmark that could be and is easily identified, particularly when the use of ankle movement distinguished between the mobile muscular fascia and the immobile skin tissue layer.
The anterior border of the tibia was determined to be the most easily detected point when the women performed anteflexion and retroflexion of their ankles. Edematous skin of the leg during pregnancy thickens uniformly and it was possible to obtain precise measurements using ultrasound. This ultrasound method showed that the skin thickness of edematous legs was significantly increased when compared with non-edematous legs (p=0.0001). Also, the skin thickness measured by ultrasonography and the degree of pitting edema were significantly correlated. The results of the pitting edema method, using finger pressure and a grading system, showed some variation between the method of measurement and the operator interpretation of the grades, which might be expected in a qualitative and subjective method of evaluating leg edema. In contrast, the advantage of measurements using ultrasonography was that this was an objective method and different operators reported consistent results.
The findings of this study also showed that the use of B-scan ultrasound to measure skin thickness was a reliable approach for the identification of cases of edema, supported by the positive correlation observed between the differences in the bilateral leg skin thickness as determined by multivariate correlations analysis, as edema during pregnancy occurs bilaterally and equally in the legs and feet. Calculation of the cutoff level for the presence of edema, when compared with no edema, was 4.7 mm, although this was only a guide and some exceptions were noted. However, when all legs included in the study were evaluated, this cutoff level showed a high degree of diagnostic sensitivity (83.9%), specificity (66.7%) and accuracy (77.6%). After dividing the pregnant women in the study into a non-obese and obese group, the specificity (formerly 66.7%) rose to 71.9% and 75.0%, respectively. Although these sensitivity, specificity, and accuracy rates might limit the utility of skin thickness measurement using portable ultrasonography, it is possible that these rates could be improved by combining this approach with the pitting edema method. While measurements using ultrasonography were not performed after treatment in this study, it is possible that this approach will also prove useful for the assessment of the effects of treatments for leg and foot edema. The future development of methods for measuring the volume of fluid that accumulates in the skin layer might also lead to more accurate diagnosis and monitoring of lower limb skin edema.
In the present study, the evaluation of edema of the skin of the lower leg included the epidermis, dermis, and subcutaneous layers using ultrasonography. In edematous legs, the subcutaneous layer was found to be particularly thickened with a hypo-echoic pattern (Figure 2B). This finding is supported by a previous ultrasound study of the skin of C3 class leg edema that used the clinical etiology anatomy pathophysiology (CEAP) classification of venous disease, which also showed thickening of the subcutaneous layer [11].
In this study, in women with edema, the thickness of the skin of the legs in pregnant obese women was more significantly increased compared with that in pregnant non-obese women. The subcutaneous layer, or subdermal layer, consists mainly of adipose tissue and collagen and contains abundant lymphatic and blood vessels, making it a suitable environment for the accumulation of extracellular fluid, much of which is found in the collagen network that surrounds the adipocytes [23]. Zaleska et al. showed that the increase in limb volume in cases of lymphedema was partially caused by the expansion of adipose tissue [24]. Because the subcutaneous layer of the leg in obese pregnant women is composed of adipose-rich tissue, a greater amount of fluid may collect in the subcutaneous layer when compared with the epidermis and dermis. This phenomenon explains the findings in the subcutaneous layer of pregnant obese women with edema when compared with pregnant non-obese women with leg edema, which was clearly demonstrated by the use of portable ultrasound.
Conclusions
The findings of this study have shown that portable B-scan ultrasonography was able to quantitatively measure the increased thickness of the skin of the leg in pregnant women. Portable ultrasonography was a reliable, objective, and quantitative method for identifying legs with and without edema and was without operator variability. The ultrasound device is portable, the imaging method is easy to use and produces consistent results between operators. A doctor or midwife would be able to perform this imaging method easily in an outpatient setting. An important finding of this study has shown that the subcutaneous layer of the skin of obese women who have leg edema during pregnancy shows significantly greater thickening when compared with pregnant non-obese women who have leg edema during pregnancy.
Acknowledgments
The authors would like to thank Dr. Brian Quinn for proofreading assistance.
Footnotes
Conflict of interest
None.
Source of support: Departmental sources
References
- 1.Cunningham FG, Gant NF, Leveno KJ, et al. Williams obstetrics. 21st edition. McGraw-Hill; New York, USA: 2001. [Google Scholar]
- 2.Reynolds D. Severe gestational edema. J Midwifery Womens Health. 2003;48:146–48. doi: 10.1016/s1526-9523(02)00419-1. [DOI] [PubMed] [Google Scholar]
- 3.Hartmann S, Huch R. Response of pregnancy leg edema to a single immersion exercise session. Acta Obstet Gynecol Scand. 2005;84:1150–53. doi: 10.1111/j.0001-6349.2005.00829.x. [DOI] [PubMed] [Google Scholar]
- 4.Bamigboye AA, Hofmeyr GJ. Interventions for leg edema and varicosities in pregnancy. What evidence? Eur J Obstet Gynecol Reprod Biol. 2006;129:3–8. doi: 10.1016/j.ejogrb.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Berard A, Kurz X, Zuccarelli F, et al. Reliability study of the Leg-O-Meter, an improved tape measure device, in patients with chronic venous insufficiency of the leg. Angiology. 1998;49:169–73. doi: 10.1177/000331979804900301. [DOI] [PubMed] [Google Scholar]
- 6.Perrin M. Edema and leg volume: Methods of assessment. Angiology. 2000;51:9–12. doi: 10.1177/000331970005100103. [DOI] [PubMed] [Google Scholar]
- 7.Mittinen M, Monkkonen J, Lahtinen MR, et al. Measurement of oedema in irritant-exposed skin by a dielectric technique. Skin Res Technol. 2006;12:235–40. doi: 10.1111/j.0909-752X.2006.00162.x. [DOI] [PubMed] [Google Scholar]
- 8.Berlit S, Tuschy B, Stojakowits M, et al. Bioelectrical impedance analysis in pregnancy: reference range. In Vivo. 2013;27:851–54. [PubMed] [Google Scholar]
- 9.Hirai M, Nukumizu Y, Kidokoro H, et al. Effect of elastic compression stockings on oedema prevention in healthy controls evaluated by a three-dimensional measurement system. Skin Res Technol. 2006;12:32–35. doi: 10.1111/j.0909-725X.2006.00129.x. [DOI] [PubMed] [Google Scholar]
- 10.Hirai M, Iwata H, Niimi K, et al. Improvement of a three-dimensional measurement system for the evaluation of foot edema. Skin Res Technol. 2012;18:120–24. doi: 10.1111/j.1600-0846.2011.00527.x. [DOI] [PubMed] [Google Scholar]
- 11.Caggiati A. Ultrasonography of skin changes in legs with chronic venous disease. Eur J Vasc Endovasc Surg. 2016;52:534–42. doi: 10.1016/j.ejvs.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 12.Suehiro K, Morikage N, Murakami M, et al. Significance of ultrasound examination of skin and subcutaneous tissue in secondary lower extremity lymphedema. Ann Vasc Dis. 2013;6:180–88. doi: 10.3400/avd.oa.12.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suehiro K, Morikage N, Murakami M, et al. Subcutaneous tissue ultrasonography in legs with dependent edema and secondary lymphedema. Ann Vasc Dis. 2014;7:21–27. doi: 10.3400/avd.oa.13-00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal V, Dabra AK, Kaur R, et al. Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome: Ultrasonography as a diagnostic tool. Clin Rheumatol. 2005;24:476–79. doi: 10.1007/s10067-004-1061-x. [DOI] [PubMed] [Google Scholar]
- 15.Gniadecka M, Serup J, Søndergaard J. Age-related diurnal changes of dermal oedema: evaluation by high-frequency ultrasound. Br J Dermatol. 1994;131:849–55. doi: 10.1111/j.1365-2133.1994.tb08588.x. [DOI] [PubMed] [Google Scholar]
- 16.Volikova AI, Edwards J, Stacey MC, Wallace HJ. High-frequency ultrasound measurement for assessing post-thrombotic syndrome and monitoring compression therapy in chronic venous disease. J Vasc Surg. 2009;50(4):820–25. doi: 10.1016/j.jvs.2009.05.060. [DOI] [PubMed] [Google Scholar]
- 17.Eisenbeiss C, Welzel J, Eichler W, Klotz K. Influence of body water distribution on skin thickness: Measurements using high-frequency ultrasound. Br J Dermatol. 2001;144:947–51. doi: 10.1046/j.1365-2133.2001.04180.x. [DOI] [PubMed] [Google Scholar]
- 18.Tsukahara K, Takema Y, Moriwaki S, et al. Dermal fluid translocation is an important determinant of the diurnal variation in human skin thickness. Br J Dermatol. 2001;145:590–96. doi: 10.1046/j.1365-2133.2001.04430.x. [DOI] [PubMed] [Google Scholar]
- 19.Diridollou S, Maillet A, Pavy-Le Traon A, et al. Use of thigh pressure cuffs to modulate simulated microgravity-induced changes in the skin measured with high-resolution B-scan ultrasound. Eur J Ultrasound. 2001;13:215–26. doi: 10.1016/s0929-8266(01)00135-5. [DOI] [PubMed] [Google Scholar]
- 20.Chao CYL, Zheng YP, Cheing GLY. The association between skin blood flow and edema on epidermal thickness in the diabetic foot. Diabetes Technol Ther. 2012;14:602–9. doi: 10.1089/dia.2011.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mollart L. Single-blind trial addressing the differential effects of two reflexology techniques versus rest, on ankle and foot oedema in late pregnancy. Complement Ther Nurs Midwifery. 2003;9:203–8. doi: 10.1016/S1353-6117(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe Y, Koshiyama M, Yanagisawa N. Treatment of leg and foot edema in women. Women Health Open J. 2017;3(2):69–74. [Google Scholar]
- 23.Comley K, Fleck NA. A micromechanical model for the Young’s modulus of adipose tissue. Int J Solids Struct. 2010;47:2982–90. [Google Scholar]
- 24.Zaleska M, Olszewski WL, Durlik M. The effectiveness of intermittent pneumatic compression in long-term therapy of lymphedema of lower limbs. Lymphat Res Biol. 2014;12(2):103–9. doi: 10.1089/lrb.2013.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]