Abstract
Background:
Temporomandibular joint ankylosis is one of the most distressing clinical condition resulting in loss of jaw function and impairment of growth. Ankylosis is a greek word meaning “Stiff Joint”. It is observed that in humans the Sternoclavicular joint and Temporomandibular joint are similar morphologically and histologically as they are the only two synovial joints covered with fibrocartilage. This similarity of the joints have encouraged the surgeons to use SCG as an alternative to costochondral grafts.
Aims:
The purpose of this article was to evaluate the feasibility of using sternoclavicular graft for TMJ reconstruction in TMJ ankylosis patients and to also assess this technique in restoration of mandibular movement, function and growth of the mandible.
Settings and Design:
This retrospective study was conducted in 10 patients with unilateral TMJ ankylosiswho had undergone Interpositional arthroplasty with temporalis fascia and reconstruction of ramus condyle unit with sternoclavicular graft.
Methods and Material:
Ten patients(8 male and 2 female) with unilateral TMJ ankylosis within the growth period were included in the study. Clinical parameters assessed were maximal incisor opening, lateral excursion and protrusive movements.,ramus height,wound infection, donor sitemorbidity, evidence of neurological deficit in both donor and recipient site. Pre and post operative radiographic analysis of graft in relation to glenoid fossa and ramus of mandible was also done and donor site regeneration was also assessed.
Statistical Analysis Used:
The data were analysed using SPSS version 20 (IBM Corporation, SPPSInc; Chicago, IL, USA). Paired T test was used to compare the pre operative and post operativelaterotrusive, protrusive movements and the height of the ramus of the mandible. Repeated measures ANOVA was used to analyse the mouth opening pre operatively ,immediate post operatively and a after 5- year follow up.
Results:
The mean post operative mouth opening achieved was 28.9+_7.57mm with reankylosis in two patients. The mean laterotrusive and protrusive movements were 5.2 +_2.82mm and 2.2 +_.78 mm respectively postoperatively on a five year follow up. There was a 6.2 +_2.57mm increase in ramus height. The sternoclavicular graft had integrated and remodelled satisfactorily in eight patients. There was no change in the body length or midline deviation. Regarding the healing of the donor site there was a complete regeneration of clavicle within one year, however there was a incidence of clavicle fracture in one patient. The shoulder movements were normal in all patients.
Conclusions:
The reconstruction of TMJ with SCG has proved to be successful in this study. With an impressive success rate, the sternoclavicular graft could become a versatile and viable alternative to the surgeons in reconstruction of TMJ as it is relatively simple to carry out with minimal complications and good results.
Keywords: Ankylosis, sternoclavicular graft, temporomandibular joint
INTRODUCTION
Temporomandibular joint (TMJ) ankylosis is one of the most distressing clinical conditions resulting in loss of jaw function and impairment of growth. Ankylosis is a Greek word meaning “Stiff Joint.” It is defined as bony or fibrous adhesions between anatomical components of the TMJ.[1] The various techniques for surgical correction of TMJ ankylosis are gap arthroplasty, interpositional arthroplasty, and joint reconstruction.[2] The goals of TMJ reconstruction are restoration of the structure, form, function, and simultaneously allow an adaptive growth center in young patients.[3] Even though various alloplastic materials have been used for TMJ reconstruction, the inherent growth potential within the cartilaginous grafts makes them a first choice for TMJ reconstruction in young patients with growth potential.[4]
Conventionally, the costochondral grafts (CCGs) have been used for reconstruction of TMJ in ankylosis patients, but because of the unpredictable growth, warpage, and fracture of the CCGs, a need has emerged to search for an alternative.
It is observed that in humans, the Sternoclavicular joint and TMJ are similar morphologically and histologically as they are the only two synovial joints covered with fibrocartilage.[5] This similarity of the joints has encouraged the surgeons to use Sternoclavicular graft (SCG) as an alternative to CCGs.
The purpose of this retrospective study was to evaluate the feasibility of using sternoclavicular graft for TMJ reconstruction in TMJ ankylosis patients and to also assess this technique in restoration of mandibular movements and function and growth of the mandible.
SUBJECTS AND METHODS
This study was a retrospective analysis of patients with unilateral TMJ ankylosis in whom TMJ ankylosis release and TMJ reconstruction with sternoclavicular graft were carried out from April 2011 to November 2013 following approval from the institutional ethical committee and obtaining informed consent from each patient in the regional language (Tamil) explaining the nature of the surgical procedure and the outcome, potential risks, and benefits of participating in the study.
Patients with unilateral TMJ ankylosis who were referred to the department of oral and maxillofacial surgery were included in the study. The inclusion criteria were patients within the age group of 10–20 years, with unilateral TMJ ankylosis presenting no systemic contraindication for the surgical procedure, and who had undergone TMJ ankylosis release and TMJ reconstruction with sternoclavicular graft. Inability in mouth opening or a limited mouth opening was the chief complaint in all patients. Patients with bilateral TMJ ankylosis or a history of clavicle fracture or any TMJ or clavicular pathology were excluded from the study.
Preoperative assessment of the patients included thorough history and clinical examination and extraoral and intraoral photographs. Clinical parameters assessed were Maximal incisal opening (MIO), lateral excursion, and protrusive movements. Radiographic analysis included orthopantomogram and posteroanterior (PA) view of the chest. Computed tomography (CT) scan was taken to assess the extension of ankylotic mass in all three planes. PA view of the chest was taken to assess the thickness of clavicle and to rule out any evidence of previous clavicular fracture or pathology. PA cephalograms were analyzed pre- and postoperatively to determine the ramus height. The patients were also assessed postoperatively for wound infection, donor-site morbidity, and evidence of neurological deficit in both donor and recipient site. Pre- and postoperative radiographic analysis of graft in relation to glenoid fossa and ramus of mandible was done. Regeneration of the donor site was assessed 6 months post operatively and on the subsequent yearly follow up visits using chest X-ray PA view.
Surgical technique
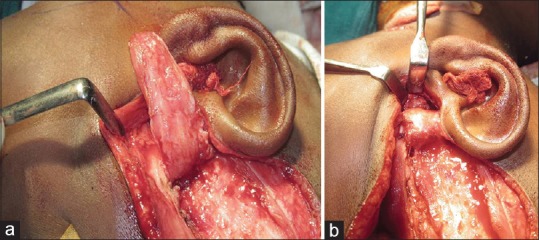
The surgical management of all the cases of TMJ ankylosis was done under general anesthesia with fiber-optic-assisted nasoendotracheal intubation (in six patients) and video laryngoscopy-assisted nasoendotracheal intubation in one patient and retrograde intubation in three patients. Al-Kayat and Bramley incision[6] was used to gain access to TMJ in all cases [Figure 1a and b], and the ankylotic mass was resected leaving a gap of 1–1.5 cm [Figure 2] and ipsilateral coronoidectomy was done. In three patients, since the mouth opening was <30 mm after ipsilateral coronoidectomy, a contralateral coronoidectomy was done.
Figure 1.
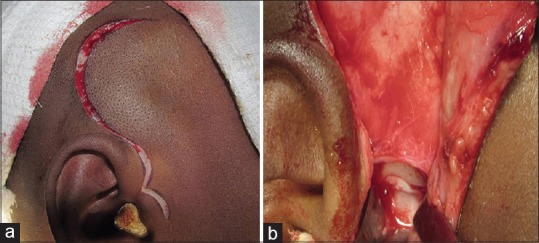
(a) Al-Kayat and Bramley incision. (b) Exposure of ankylotic mass
Figure 2.
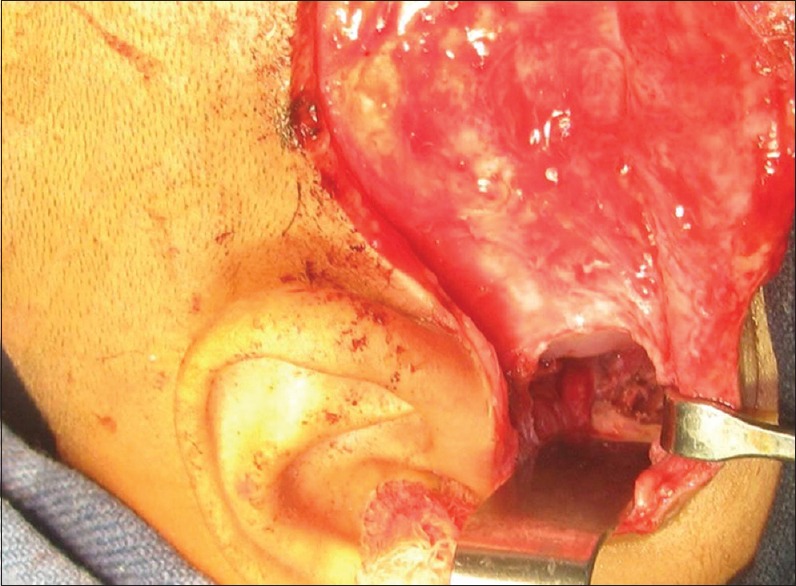
Gap arthroplasty
The sternoclavicular graft was procured through an infraclavicular incision made 2–3 cm lateral from the condylar head of the sternoclavicular joint. The initial incision was made through the skin, subcutaneous tissues, and platysma. The overlying fascia and periosteum were next incised. Muscle attachment and periosteum were dissected from superior and medial aspects of the clavicle, maintaining the integrity of attachment of the ligaments of the articular disc to the clavicular head and avoiding injury to the pleura. In all cases, a split-thickness graft was used leaving the inferior part intact [Figure 3a and b]. The articulating end of the graft was shaped to simulate the head of the condyle for a better fit into the glenoid fossa. Moreover, the graft was fixed on the lateral aspect of the ramus using 1.5 mm × 10 mm screws through a submandibular incision [Figure 4]. Finally, after the graft placement, interpositioning of temporalis fascia and muscle was done in all cases [Figure 5] and the wounds were closed layer wise.
Figure 3.
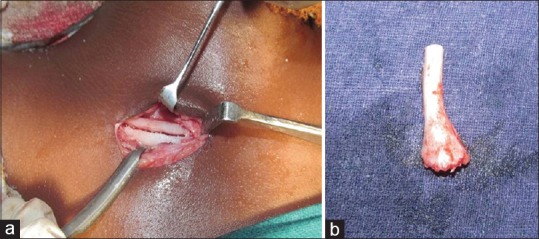
(a) Harvesting of sternoclavicular graft. (b) Harvested sternoclavicular graft
Figure 4.
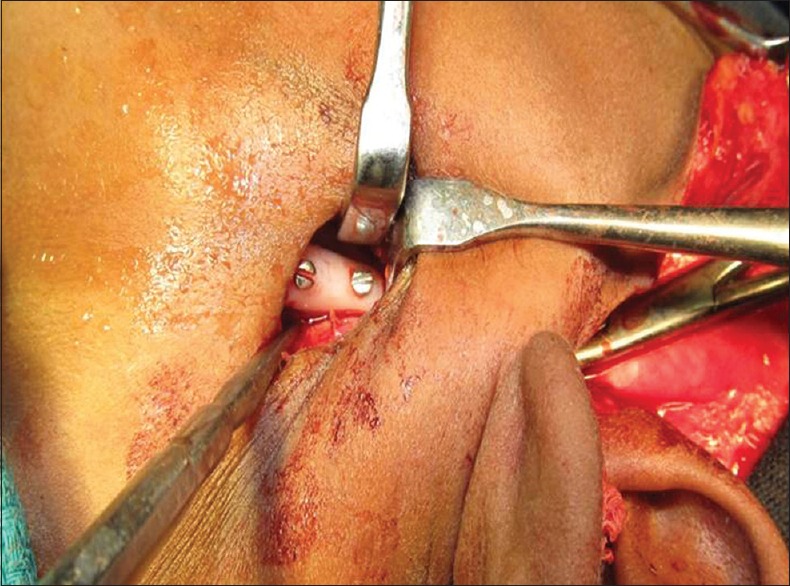
Fixation of graft on the lateral aspect of the ramus through submandibular incision
Figure 5.
(a and b) Interpositioning of temporalis muscle and fascia
Postoperatively, all patients were placed in intermaxillary fixation (IMF) for 1 week for stabilization of the graft, and physiotherapy was commenced on the 7th day after IMF release using “Heister jaw opener” for 6 months to maintain and improve the intraoperative mouth opening. The patients were advised arm sling for 1 month to minimize chances of clavicular fracture and were instructed not to lift anything heavy for 3 months. Regular follow-up was carried out and once in a year for 1 year after the surgery.
RESULTS
The data were analyzed using SPSS version 20 (IBM Corporation, SPPS Inc., Chicago, IL, USA). Paired t-test was used to compare the pre- and post-operative laterotrusive, protrusive movements and the height of the ramus of the mandible. Repeated measures ANOVA was used to analyze the mouth opening preoperatively, immediate postoperatively, and after a 4-year follow-up.
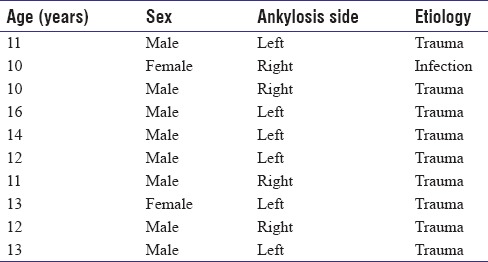
Ten patients with unilateral TMJ ankylosis were included in this study. The mean age of the patients was 12.2 years. Nearly 80% were male patients and left side was involved in 60% of patients. Trauma was the cause of ankylosis in nine patients and infection in one patient. The mean duration of the ankylosis was 4 years [Table 1]. The mean follow-up period was 4 years.
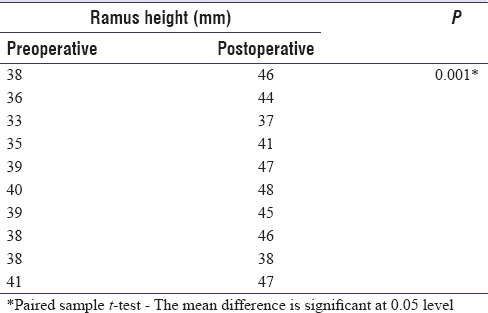
Table 1.
Demographic data of the patient
The range of preoperative mouth opening was 0–10 mm (mean: 5.7 mm) [Figure 6]. The mean mouth opening achieved in the immediate postoperative period was 32.5 mm (range: 26–37 mm); postoperatively after 4 years, there was a comparative decrease in mouth opening in all patients with a mean mouth opening of 26.7 mm ± 7.57 mm (range: 10–36 mm) [Figure 7] and two patients had reankylosis with a mouth opening of 10 mm [Table 2]. There were no protrusive or laterotrusive movements preoperatively. There was an improvement in translatory movements of the jaws with a mean protrusive movement of 2.2 mm ± 0.78 mm and laterotrusive movement of 5.2 mm ± 2.82 mm [Table 3]. There was no change in body length pre- and postoperatively, and a mean increase of 6.2 mm ± 2.57 mm in the ramal height was observed postoperatively [Table 4].
Figure 6.

Preoperative frontal view showing reduced mouth opening
Figure 7.

(a) Postoperative frontal view showing increased mouth opening. (b) Postoperative frontal view showing mouth opening after 4-year follow-up
Table 2.
Mouth opening in mm
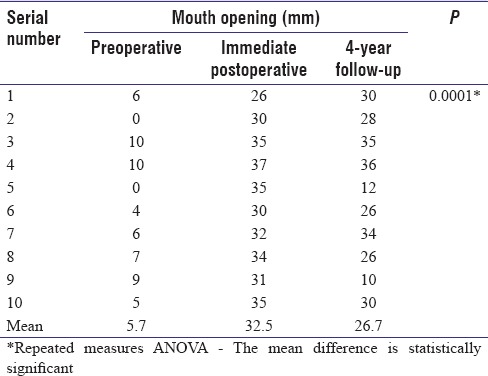
Table 3.
Temporomandibular joint movements
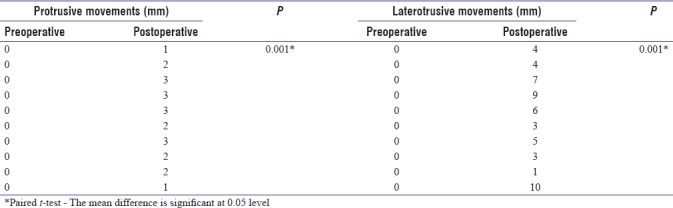
Table 4.
Height of the ramus
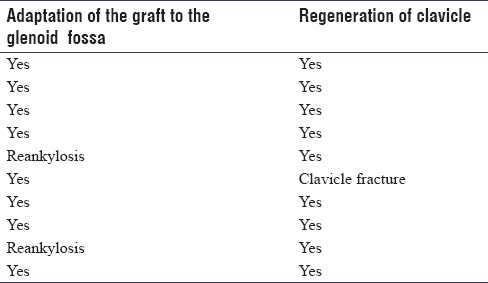
There was no change in the midline deviation. There was no evidence of facial nerve paresis, wound infection, or dehiscence or donor-site morbidity or pain in the clavicle. The shoulder movements were normal after 3 months. However, the presence of unsightly scar was evident in the clavicular region in all the patients and scar was hypertrophic in five patients. No signs of graft rejection were seen in all patients. Radiographic analysis and CT scan showed that the graft had integrated and remodeled satisfactorily in eight patients [Figures 8a, b and 9a, b] and reankylosis in two patients. Regarding the healing of the donor site, there was a complete regeneration of clavicle within 1 year [Figure 10a] and [Figure 10b]; however, there was an incidence of clavicle fracture in one patient [Table 5].
Figure 8.
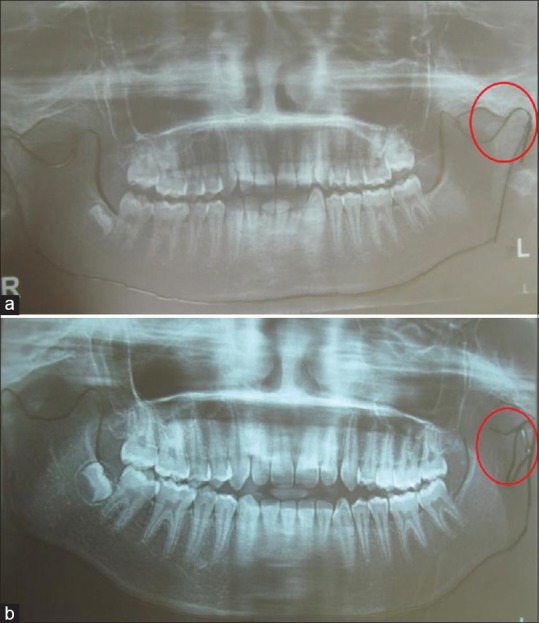
(a) Preoperative orthopantomogram showing ankylosis. (b) Immediate postoperative orthopantomogram showing reconstructed joint with sternoclavicular graft
Figure 9.
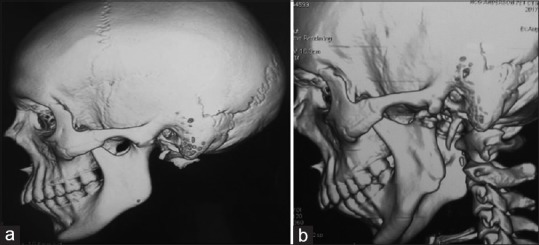
(a) Preoperative computed tomography scan showing ankylosis of temporomandibular joint. (b) Postoperative computed tomography scan showing remodeling and adaptation of the sternoclavicular graft
Figure 10.
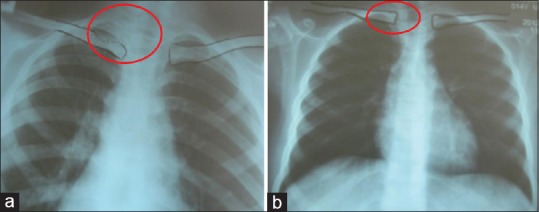
(a) Posteroanterior view chest showing clavicle after harvesting the graft. (b) Posteroanterior view chest showing complete regeneration of the clavicle at 6-month follow-up
Table 5.
Assessment of morbidity in the donor site and reconstructed temporomandibular joint to the glenoid fossa
DISCUSSION
TMJ ankylosis is one of the most physically and psychologically distressing conditions to the patients. The surgical procedure for TMJ ankylosis can be either a condylectomy alone or a gap arthroplasty or interpositional arthroplasty. The rationale behind the placement of an interpositional material was that it forms a partition between bony compartments, similar to an articular disc.[7] However, the recurrence rate was high in the study by Topazian (53%) using interpositional arthroplasty.[8] Moreover, the interpositional material failed to restore adequate ramal height.
The condyle is just an adaptive center whereby the secondary cartilage responds to the enlargement of the surrounding functional matrix.[9] Hence, in ankylosis, the absence of translational movements leads to failure of condylar and ramal growth, and therefore, early release of ankylosis and reconstruction with an autogenous graft is necessary to permit an adaptive growth center and the other reason for reconstructing a condyle with autogenous grafts is that a normal mandible is basically a Class 3 lever with condyle as the fulcrum of rotation, so in case of a condylectomy or gap arthroplasty with or without interpositional material, this third-class lever is converted to a first-class lever. The most posterior tooth which occludes with the upper jaw then becomes the fulcrum which means that the fulcrum is now anterior to the working force and the mandible in turn tends to rotate clockwise resulting in an anterior open bite, and moreover, there is a shortening of muscles leading to misdirected growth. Hence, there is a need to provide a graft with growth capacities similar to normal condyle in patients in the growth period,[10] and in accordance with this principle, a treatment plan of early ankylosis release and joint reconstruction with a cartilaginous graft was devised in the present study as all the patients were in the growth period.
In spite of having drawbacks such as donor-site morbidity, infection, and failure of uptakes, autogenous grafts have been still widely used for TMJ reconstruction. The various autogenous grafts used are costochondral,[11] sternoclavicular,[12,13,14] metatarsal,[15] iliac crest,[16] fibula,[17] and coronoid.[18]
The most widely used autogenous graft, the CCG was first described by Gillies;[19] however, the current technique was popularized by Poswillo.[11] CCG is a biologically compatible, easily workable graft which adapts into the new environment even sometimes with a potential for the donor site to grow or regenerate.[19] CCGs too have many drawbacks such as unpredictable growth, flexibility and elasticity of bone, warpage with continuous loading, poor quality of medullary and cortical bone, possibility of resorption and infection, possible separation of cartilage from the bone, and the donor-site complications such as pleural tear, pneumothorax, and pleural effusion,[10,12,20] and this has made to search for an alternative, and the sternoclavicular graft which resembles the TMJ morphologically and histologically could be a viable option.
Wolford et al.[20] reported a success rate of 93% in TMJ reconstruction using sternoclavicular grafts in patients with existing non-Proplast-Teflon prosthesis or noninflammatory pathology. Singh et al.[21] had also reported similar success rates with 2 failures out of 15 patients; similar success rate of 80% was observed in the present study. In the current study, MIO at 4-year follow-up was 26.7 mm which was lesser than the results achieved by Singh et al.[21] in which MIO was 32.9 mm and Wolford et al.[20] 34.8 mm and Kaban et al.[22] 31 mm where CCG was used. The decrease in mouth opening could be attributed to the failure by some patients to aggressively follow the physiotherapy regime. A gap arthroplasty was done for the reankylosis patients and the graft was removed, and the patients were advised to follow vigorous mouth opening exercises.
There was no change in midline deviation in our study consistent with the study by Singh et al. The increase in ramus height achieved in the present study was only 6.2 mm contrary to Wolford et al.[20] study which suggests that large advancements of the mandible and vertical lengthening of the ramus can be achieved. There was an improvement in facial symmetry to a certain extent, but residual deformity persisted requiring additional orthognathic surgeries after the completion of growth period.
Regarding donor-site morbidity, Siemssen[12] reported no functional deformity of the shoulder and arm even after using a full-thickness SCG. Wolford et al.[20] reported clavicle fracture in four patients, Singh et al.[21,23] in two patients out of 15 cases, and in this study in one patient supporting the evidence of very minimal donor-site morbidity compared to the CCG. There was a complete regeneration of clavicle in all patients similar to Singh et al.[21] studies.
Literature suggests that maintaining the articular disc and resuturing of the lateral pterygoid muscle to the graft results in better translational movements than placing the graft in the eroded fossa. In this study, however, articular disc could not be maintained in any of the cases; hence, temporalis fascia and muscle was used as an interposing material. It not only improved the translatory movements but also had an added advantage of reducing the chance of reankylosis as it minimizes bone to bone contact. Singh et al.[23] used buccal fat pad as an interpositioning material in their study.
It was found in the present study that the sternoclavicular graft had a anatomic resemblance to the condyle and very minimal shaping was needed as published by Ellis and Carlson.[4,5] They reported that the SCJ contains layers of cartilage similar to the TMJ such as the articular, prechondroblastic, chondroblastic, hypertrophic, and endochondral ossification layers at each age during the growth unlike the CCG which appears to resemble the growth plate of long bone epiphysis during growth. The overgrowth of the CCG could be due to this histological variation from the TMJ.
The SCG underwent remodeling and resembled the native condyle in the current study as reported by Daniels et al.[5,24] who reported that when implanted in the TMJ area, SCG graft undergoes remodeling and resembles the native condyle unlike CCG which does not.
Snyder et al.[13] as early as in 1971 reported doing a sternoclavicular whole joint graft on a 70-year-old man. In 1982, Siemssen[12] described a muscle pedicle SCG for TMJ reconstruction. Reid et al.[25] reported a free flap technique that included the clavicular head of the pectoralis major muscle and the overlying skin. They suggested splitting the clavicle longitudinally and repositioning it with the attached flap. The technique suggested by Wolford et al.[20] was used in the reported study for harvesting the sternoclavicular graft. The sternoclavicular graft can be placed in three positions, namely on the lateral aspect of the ramus or on the medial side or along the posterior border. Placing the graft on the medial side is suitable for patients with hemifacial microsomia, and when placing the graft on the posterior border, a vertical ramus osteotomy is needed to provide adequate space for the graft and a contralateral clavicular graft needs to be harvested. Since none of the patients had hemifacial microsomia, graft was placed on the lateral aspect rather than on the medial side, or since the graft was not placed on the posterior border of the mandible, the ipsilateral clavicle was harvested in all cases as suggested by Wolford et al.[20]
In this study, patients above 10 years were chosen as the clavicular thickness below 10 years precludes the use of split-thickness graft, wherein a full-thickness graft would be the option. It was also noted that the split-thickness graft comprising the superior half of the clavicle fitted better into the newly created glenoid fossa similar to Wolford et al.'s study.[20] The advantages of using a split-thickness graft are a good fit, minimal donor-site morbidity, faster regeneration of bone in the donor site, and better graft uptake as revascularization is easier because of direct exposure of the medullary bone to the adjacent soft tissues.
The graft was fixed to the ramus using screws in the same way as Wolford et al.[20] and Siemsen et al.,[12] but Singh et al.[23] used lag screws; however, there were no evidence of screw loosening or any graft rejection in the current study.
CONCLUSION
The reconstruction of TMJ with SCG has been proved to be successful in this study, as it has been mentioned in various literature, by many authors. The results of the present study reveal that there was an anatomic resemblance of the SCG to the TMJ and there was no donor-site morbidity as there was a regeneration of clavicle at the donor site, and the operative complications in harvesting the graft were minimal. With an impressive success rate, the sternoclavicular graft could become a versatile and viable alternative to the surgeons in reconstruction of TMJ as it is relatively simple to carry out with minimal complications and good results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Valentini V, Vetrano S, Agrillo A, Torroni A, Fabiani F, Iannetti G, et al. Surgical treatment of TMJ ankylosis: Our experience (60 cases) J Craniofac Surg. 2002;13:59–67. doi: 10.1097/00001665-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Katsnelson A, Markiewicz MR, Keith DA, Dodson TB. Operative management of temporomandibular joint ankylosis: A systematic review and meta-analysis. J Oral Maxillofac Surg. 2012;70:531–6. doi: 10.1016/j.joms.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Vasconcelos BC, Porto GG, Bessa-Nogueira RV, Nascimento MM. Surgical treatment of temporomandibular joint ankylosis: Follow-up of 15 cases and literature review. Med Oral Patol Oral Cir Bucal. 2009;14:E34–8. [PubMed] [Google Scholar]
- 4.Ellis E, 3rd, Carlson DS. Histologic comparison of the costochondral, sternoclavicular, and temporomandibular joints during growth in Macaca mulatta. J Oral Maxillofac Surg. 1986;44:312–21. doi: 10.1016/0278-2391(86)90082-0. [DOI] [PubMed] [Google Scholar]
- 5.Daniels S, Ellis E, 3rd, Carlson DS. Histologic analysis of costochondral and sternoclavicular grafts in the TMJ of the juvenile monkey. J Oral Maxillofac Surg. 1987;45:675–83. doi: 10.1016/0278-2391(87)90306-5. [DOI] [PubMed] [Google Scholar]
- 6.Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg. 1979;17:91–103. doi: 10.1016/s0007-117x(79)80036-0. [DOI] [PubMed] [Google Scholar]
- 7.Topazian RG. Etiology of ankylosis of temporomandibular joint: Analysis of 44 cases. J Oral Surg Anesth Hosp Dent Serv. 1964;22:227–33. [PubMed] [Google Scholar]
- 8.Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;24:405–9. [PubMed] [Google Scholar]
- 9.Moss ML. Functional cranial analysis and the functional matrix. Int J Orthod. 1979;17:21–31. [PubMed] [Google Scholar]
- 10.Politis C, Fossion E, Bossuyt M. The use of costochondral grafts in arthroplasty of the temporomandibular joint. J Craniomaxillofac Surg. 1987;15:345–54. doi: 10.1016/s1010-5182(87)80081-1. [DOI] [PubMed] [Google Scholar]
- 11.Poswillo DE. Biological reconstruction of the mandibular condyle. Br J Oral Maxillofac Surg. 1987;25:100–4. doi: 10.1016/0266-4356(87)90003-9. [DOI] [PubMed] [Google Scholar]
- 12.Siemssen SO. Temporomandibular arthroplasty by transfer of the sterno-clavicular joint on a muscle pedicle. Br J Plast Surg. 1982;35:225–38. doi: 10.1016/s0007-1226(82)90107-2. [DOI] [PubMed] [Google Scholar]
- 13.Snyder CC, Benson AK, Slater PV. Construction of the temporomandibular joint by transplanting the autogenous sternoclavicular joint. South Med J. 1971;64:807–14. doi: 10.1097/00007611-197107000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Snyder CC, Levine GA, Dingman DL. Trial of a sternoclavicular whole joint graft as a substitute for the temporomandibular joint. Plast Reconstr Surg. 1971;48:447–52. doi: 10.1097/00006534-197111000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Lexer E. Joint transplantations and arthroplasty. Surg Gynecol Obstet. 1925;40:782–809. [Google Scholar]
- 16.Matukas VJ, Szymela VF, Schmidt JF. Surgical treatment of bony ankylosis in a child using a composite cartilage-bone iliac crest graft. J Oral Surg. 1980;38:903–5. [PubMed] [Google Scholar]
- 17.Wax MK, Winslow CP, Hansen J, MacKenzie D, Cohen J, Andersen P, et al. A retrospective analysis of temporomandibular joint reconstruction with free fibula microvascular flap. Laryngoscope. 2000;110:977–81. doi: 10.1097/00005537-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Hong Y, Gu X, Feng X, Wang Y. Modified coronoid process grafts combined with sagittal split osteotomy for treatment of bilateral temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2002;60:11–8. doi: 10.1053/joms.2002.29050. [DOI] [PubMed] [Google Scholar]
- 19.Gillies H. London: Oxford University Press; 1920. Plastic Surgery of the Face. [Google Scholar]
- 20.Wolford LM, Cottrell DA, Henry C. Sternoclavicular grafts for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1994;52:119–28. doi: 10.1016/0278-2391(94)90391-3. [DOI] [PubMed] [Google Scholar]
- 21.Singh V, Verma A, Kumar I, Bhagol A. Reconstruction of ankylosed temporomandibular joint: Sternoclavicular grafting as an approach to management. Int J Oral Maxillofac Surg. 2011;40:260–5. doi: 10.1016/j.ijom.2010.09.023. [DOI] [PubMed] [Google Scholar]
- 22.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–51. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- 23.Singh V, Dhingra R, Bhagol A. Prospective analysis of temporomandibular joint reconstruction in ankylosis with sternoclavicular graft and buccal fat pad lining. J Oral Maxillofac Surg. 2012;70:997–1006. doi: 10.1016/j.joms.2011.02.129. [DOI] [PubMed] [Google Scholar]
- 24.Henning TB, Ellis E, 3rd, Carlson DS. Growth of the mandible following replacement of the mandibular condyle with the sternal end of the clavicle: An experimental investigation in Macaca mulatta. J Oral Maxillofac Surg. 1992;50:1196–206. doi: 10.1016/0278-2391(92)90154-r. [DOI] [PubMed] [Google Scholar]
- 25.Reid CD, Taylor GI, Waterhouse N. The clavicular head of pectoralis major musculocutaneous free flap. Br J Plast Surg. 1986;39:57–65. doi: 10.1016/0007-1226(86)90005-6. [DOI] [PubMed] [Google Scholar]


