Abstract
Very few cases of parotid oncocytoma have been reported in literature. Because of its rarity (<1% of salivary gland tumors) and clinical presentation of the tumor, there is a tendency among the clinicians to misdiagnose it as pleomorphic adenoma, hemangioma, or other forms of oncocytosis. Only a histopathological examination can confirm it. We evaluate here a case of swelling of the parotid gland in a 70-year-old male who had the tumor for over 9 years to reach a diagnosis. Furthermore, our aim is to bring to the forefront how these lesions require a comprehensive workup and how to choose the best treatment strategy.
Keywords: Fine-needle aspiration cytology, oncocytoma, parotid
INTRODUCTION
Salivary gland neoplasm represents the most complex and diverse group of tumors encountered by head-and-neck surgeons. Their diagnosis and management is complicated by their relative infrequency (1% of head-and-neck tumors), the limited amount of pretreatment information available, and wide range of biological behavior seen.[1] Oncocytoma are rare tumors. They are predominantly tumors that occur in those who are middle aged and above. Women, usually in the seventh or eighth decade, are likely to be affected. The parotid gland is the most frequent site (80%) for all salivary gland tumours. These tumors are slow growing and may rarely be bilateral.[2]
We present here a case of oncocytoma in a 70-year-old male who has had a lemon-sized swelling in the left parotid for about 9 years without undergoing any significant change in its size and character. The patient reported only for its unsightly appearance and had no other complaints. It is important to note that even though oncocytoma of the parotid is the most common of salivary gland tumours, is is only 1-2% of head and neck tumours, and with the associated vague complaints by patients and ambiguous fine needle aspiration cytology (FNAC), there is a tendency to either entirely miss it or diagnose it wrongly.
CASE REPORT
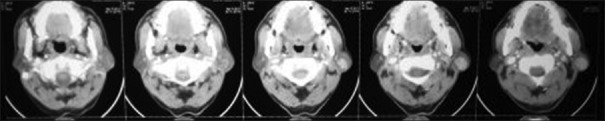
A 70-year-old male reported to the Ear, Nose and Throat Outpatient Department with a mass near the angle of the mandible on the left side for 9 years. It was a painless swelling which had an insidious onset but not increasing in size for the last many years. The patient had no other significant complaints. On examination, a solitary 3 cm × 2 cm-sized left parotid mass, posterior to the angle of the mandible, was present [Figure 1] (clinical photograph showing tumor in the left parotid). It was a nontender, nonfluctuant, nonpulsatile swelling with regular margins. It was not adherent to overlying skin or underlying structures. No signs of facial palsy were seen. FNAC report was suggestive of oncocytic neoplasm. On contrast-enhanced computerized tomography (CECT), a rounded hyperdense lesion in the superficial lobe of the left parotid was seen which according to radiologist could be benign parotid neoplasm, hemangioma, or enlarged lymph node [Figure 2] (CECT scan showing tumor in the left parotid gland). Ultrasonography identified a 2.5 cm × 1.7 cm-sized lobulated solid mass in the left parotid region which was closely abutting left parotid gland and was very vascular. Based on the above-mentioned findings, a provisional diagnosis of oncocytoma in the left parotid was made with differential diagnosis of hemangioma, and the patient was worked up for superficial parotidectomy. Superficial parotidectomy was done with preservation of the facial nerve [Figure 3] (identification and preservation of the facial nerve). Excised mass was sent for histopathological examination, which confirmed it as oncocytoma. Grossly, the resected specimen measured 5 cm × 4 cm × 2 cm in size. Macroscopically, the tumor was a nodular, circumscribed lesion measuring 2 cm × 1.5 cm × 2 cm in size and brown homogeneous in color. Microscopic findings show capsulated tumor composed of lobules of oncocytic cells [Figure 4]. The cells were large and round with abundant granular cytoplasm [Figure 5]. No mitotic figures were noted. These features are consistent with oncocytoma. The patient has been on follow-up for 2 years and has remained disease free with no local or remote recurrence of the disease.
Figure 1.

Solitary 3 cm × 2 cm-sized mass left parotid, posterior to the angle of the mandible
Figure 2.
Contrast-enhanced computerized tomography of the head and neck showing a rounded hyperdense lesion in the superficial lobe of the left parotid
Figure 3.

Identification and preservation of the facial nerve
Figure 4.
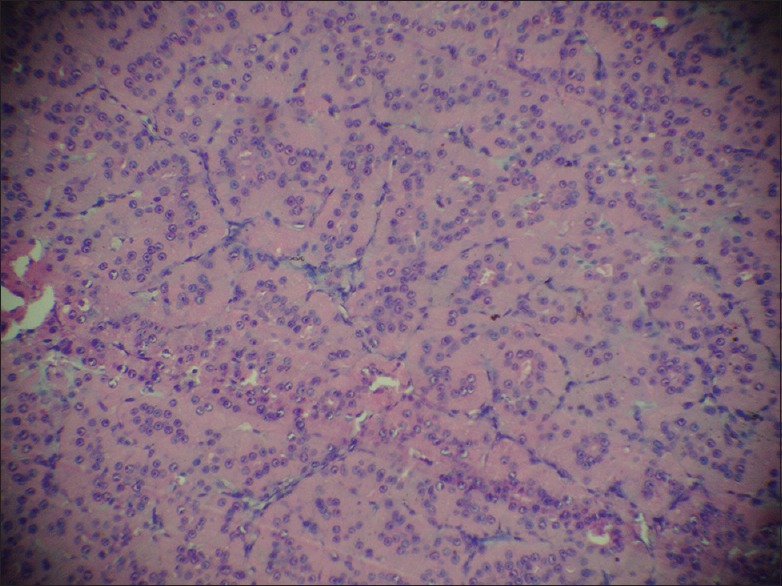
Capsulated tumor composed of lobules of oncocytic cells
Figure 5.
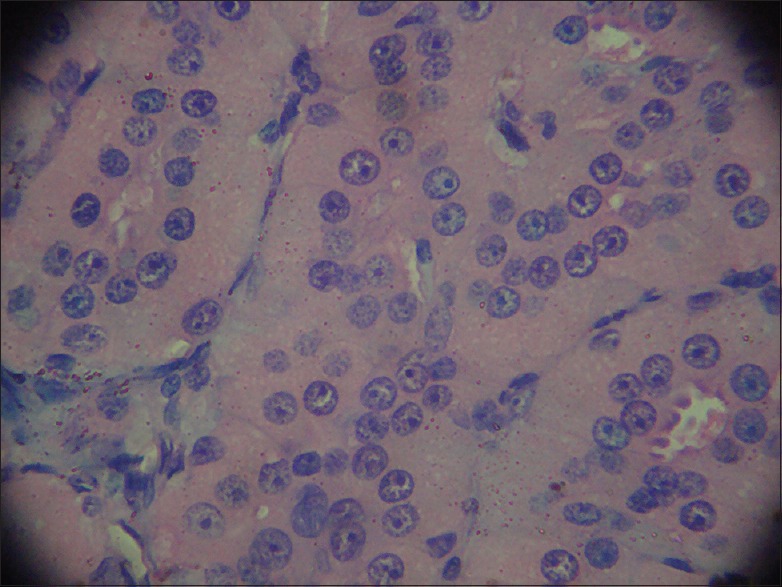
Large round oncocytes with abundant granular eosinophilic cytoplasm
DISCUSSION
Oncocytes are epithelial cells which appear as cells with abundant granular, eosinophilic cytoplasm, a centrally pyknotic nucleus, and ultrastructurally are crammed with numerous mitochondria of various sizes. Oncocytes are seen in various organs such as salivary glands, thyroid, parathyroid, pituitary, nasal cavity, sinuses, ocular carbuncle, lacrimal glands, buccal mucosa, eustachian tube, larynx, esophagus, liver, pancreas, and kidney.[3] The World Health Organization classification of salivary gland neoplasms recognizes three oncocytic entities: oncocytosis, oncocytoma, and oncocytic carcinoma. Oncocytoma is more common than oncocytic carcinomas.
Oncocytoma usually occurs in the elderly and affects the parotid glands in 80%. Pathologically, oncocytoma is described as a well-circumscribed mass, composed of layers of oncocytes (small round nucleus and microgranular, eosinophilic cytoplasm). Pathogenesis is quite obscure although mitochondrial functional defects are believed to mediate the progressive degeneration of the salivary epithelial cells.[4] Of note, only one mitochondrial DNA rearrangement (among 200 described) has been linked to parotid tumorigenesis.[5] Tandler revealed by electron microscopy that the oncocytes contained unusually large number of mitochondria.[6] Oncocytic cells are thought of as metaplastic cells formed in response to adverse changes, with the normal cells losing their original specialization. Aging is also thought to cause a functional exhaustion of mitochondrial enzymes, and a compensatory hyperplasia of mitochondria can occur, which, in turn, is responsible for the oncocytic change. Indeed, solitary oncocytes appear most often as incidental findings in aging salivary tissue, with studies showing up to 80% presence in persons older than 70 years of age.[3] In our case also, the age of patient was 70 years which points toward the progressive degeneration of salivary epithelial cells which lead to oncocytic changes.
The correlation of certain viruses, such as Epstein–Barr virus, HIV, human herpesvirus-8, human T-lymphotropic virus-1, and human papillomavirus with parotid neoplasia has been documented. Vlachaki et al. described the case of a 74-year-old female patient with left parotid oncocytoma and a previous history of immune thrombocytopenia and chronic HBV infection.[7] In our case, there was no history of viral infection or thrombocytopenia in the patient.
Areas of oncocytic metaplasia can be seen in a host of salivary gland tumors such as basal cell adenoma, pleomorphic adenoma, myoepithelioma, cystadenoma, canalicular adenoma, polymorphous low-grade adenocarcinoma, Warthin's tumor, acinic cell carcinoma, and mucoepidermoid carcinoma.[4] However, oncocytes also give rise to neoplasms such as oncocytoma and its malignant counterpart, the oncocytic carcinoma. Histopathological findings in our case are typical of a benign oncocytic neoplasm which points toward the fact that prolonged follow-up may not be necessary.
Fine-needle aspiration is the procedure of choice for making a diagnosis in the majority of cases although its sensitivity is reported to be only 29%.[4] FNAC has increasingly been used as a primary screening tool for salivary gland lesions with high levels of sensitivity and specificity. However, as salivary glands are notorious for having overlapping morphological features, diagnosis by cytology alone often becomes difficult.[2] The situation may slightly improve using multiple passes from the swelling.
Diouf et al. reported a case of oncocytoma of the left parotid gland in a 69-year-old woman in whom FNAC was for a pleomorphic adenoma. Through this case, they highlighted the importance of histopathology in the positive diagnosis of parotid oncocytoma as well as in its differential diagnosis and also the place of FNAC.[8]
In salivary glands, oncocytes may be present in a plethora of conditions ranging from hyperplasia to overtly malignant lesions. Diagnosis by FNAC may be very difficult due to focal sampling of the lesion as oncocytic change can occur in a large variety of neoplastic as well as nonneoplastic conditions. Histopathology remains the gold standard to clinch the precise diagnosis. Chakrabarti et al. presented a case of a cytologically diagnosed oncocytic lesion with a possibility of oncocytoma. However, on subsequent histopathology, the lesion was diagnosed as diffuse hyperplastic oncocytosis. In our case, the FNAC was clearly suggestive of oncocytic features of the tumor, and after histopathological examination, oncocytoma was confirmed.[9]
Surgical management with radical or superficial parotidectomy represents the cornerstone of therapy.[4] In our case also, we removed the tumor by superficial parotidectomy and preserving the facial nerve. Postoperative period was uneventful.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nagarkar NM, Bansal S, Dass A, Singhal SK, Mohan H. Salivary gland tumors – Our experience. Indian J Otolaryngol Head Neck Surg. 2004;56:31–4. doi: 10.1007/BF02968769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palmer TJ, Gleeson MJ, Eveson JW, Cawson RA. Oncocytic adenomas and oncocytic hyperplasia of salivary glands: A clinicopathological study of 26 cases. Histopathology. 1990;16:487–93. doi: 10.1111/j.1365-2559.1990.tb01549.x. [DOI] [PubMed] [Google Scholar]
- 3.Kontaxis A, Zanarotti U, Kainz J, Beham A. Diffuse hyperplastic oncocytosis of the parotid gland. Laryngorhinootologie. 2004;83:185–8. doi: 10.1055/s-2004-814267. [DOI] [PubMed] [Google Scholar]
- 4.Capone RB, Ha PK, Westra WH, Pilkington TM, Sciubba JJ, Koch WM, et al. Oncocytic neoplasms of the parotid gland: A 16-year institutional review. Otolaryngol Head Neck Surg. 2002;126:657–62. doi: 10.1067/mhn.2002.124437. [DOI] [PubMed] [Google Scholar]
- 5.Lewis PD, Baxter P, Paul Griffiths A, Parry JM, Skibinski DO. Detection of damage to the mitochondrial genome in the oncocytic cells of warthin's tumour. J Pathol. 2000;191:274–81. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH634>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 6.Tandler B. Fine structure of oncocytes in human salivary glands. Virchows Arch Pathol Anat Physiol Klin Med. 1966;341:317–26. doi: 10.1007/BF00956872. [DOI] [PubMed] [Google Scholar]
- 7.Vlachaki E, Tsapas A, Dimitrakopoulos K, Kontzoglou G, Klonizakis I. Parotid gland oncocytoma: A case report. Cases J. 2009;2:6423. doi: 10.1186/1757-1626-2-6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diouf MS, Claros P, Claros A. Oncocytoma of the parotid gland: A case report. Rev Laryngol Otol Rhinol (Bord) 2012;133:109–12. [PubMed] [Google Scholar]
- 9.Chakrabarti I, Basu A, Ghosh N. Oncocytic lesion of parotid gland: A dilemma for cytopathologists. J Cytol. 2012;29:80–2. doi: 10.4103/0970-9371.93236. [DOI] [PMC free article] [PubMed] [Google Scholar]