Abstract
Cervicofacial actinomycosis is an invasive destructive infectious syndrome, caused by Gram-positive, branching filamentous bacteria, Actinomyces. Most of the cases are traced to an odontogenic source with periapical abscess and posttraumatic or surgical complications with poor hygiene and immunosuppression as contributing factors. Diagnosis is often delayed because of nonspecific and prolonged symptoms usually mimicking a malignant or a granulomatous lesion. Solitary or multiple abscesses and fistula formation across normal tissue planes accompany chronic draining lesions and may lead to invasion of viscera. Hence, early diagnosis and appropriate treatment is mandatory to reduce morbidity. In this paper, we report two cases of cervicofacial actinomycosis, one presented with intraoral granulomatous lesion treated with surgical curettage and intramuscular penicillin and another case with extraoral swelling and multiple draining sinuses treated with oral antibiotics.
Keywords: Actinomycosis, cervicofacial, granulomatous
INTRODUCTION
Actinomycotic infections of the cervicofacial region are uncommon. Presenting clinical manifestations is confusing because they often mimic a malignancy or a granulomatous lesion. Diagnosis may be difficult because of a general lack of familiarity with the disease and a low success rate in culturing the organism as a result of its fastidious nature. As the cervicofacial manifestations of actinomycosis are varied, a high index of suspicion is required to make an accurate and timely diagnosis.[1] Appropriate treatment is always demanding as the disease causes extensive tissue destruction. The traditional treatment is high-dose penicillin for a prolonged period (6 months to 1 year).[2] The duration of antibiotic therapy with 6–12 million IU penicillins can range from 4 weeks to 1 year based on the severity of the disease. Surgical management without antibiotic therapy is associated with recurrence. Although good responses were reported with combined surgical treatment and short-term antibiotic therapy for cervicofacial actinomycosis, surgical management is associated with morbidity especially with large extensive lesion. Hence, it is mandatory to customize the treatment based on the anatomical region involved, extension, and response to the antibiotic therapy.
CASE REPORTS
Case 1
A 48-year-male patient reported with growth in the upper left back tooth region for 3 months associated with intermittent, lancinating type of pain. There was no history of any discharge from the growth and paraesthesia. The patient underwent extraction of upper left molar along with excision of growth in the same region 2 years back. The biopsy report was suggestive of granulation tissue. On physical examination of the present lesion, the growth was of size 4 cm × 5 cm extending anteriorly to the distal surface of maxillary second premolar and posteriorly to the maxillary tuberosity region [Figure 1]. The lesion extended from the depth of the buccal vestibule to the vault of the hard palate, 0.5 cm away from the median palatine raphe. Margins were well defined and the surface was smooth with interspersed erythematous areas. Pathological migration of 26 was present associated with mobility. The lesion was tender on palpation and was soft in consistency. The computed tomography (CT) scan revealed a large expansile soft-tissue lesion involving the left maxillary sinus [Figure 2]. Incisional biopsy of the lesion suggested actinomycosis. Curettage of the lesion along with extraction of the maxillary upper left premolars and first molar was done under general anesthesia. The defect was initially packed with cuticell dressing supported with an obturator and allowed to heal by secondary intention. Histopathological examination of the excised specimen suggested soft-tissue fibroma secondarily infected with actinomycosis. Antibiotic therapy with intramuscular injection of benzylpenicillin 800,000 international units was continued for a period of 3 months. The patient remained asymptomatic with no recurrence for the past 2 years following the surgery [Figure 3].
Figure 1.

Preoperative image of the intraoral lesion
Figure 2.

Computed tomography scan image showing an expansile lesion involving the left maxillary sinus
Figure 3.

Two-year postoperative image with satisfactory healing and no residual defect
Case 2
A 60-year-old male patient reported with swelling with recurrent eruptions and pus discharge over the right side of the face in the middle third region for the past 2 years. The patient gave a history of trauma 2 years back and suturing was done for the laceration in the infraorbital region by a local registered medical practitioner. The patient also gave a history of wound infection with gaping following the treatment. Debridement of the wound was done, and oral antibiotic therapy was started to which the patient was noncompliant. The patient reports the exaggeration of the multiple sinus tract openings with pus discharge following fine-needle aspiration cytology. On physical examination, diffuse swelling was present on the right middle third region of the face extending superiorly to lower eyelid region and inferiorly to a line 2 cm above the lower border of the mandible [Figure 4]. Superior displacement of the right globe was present with normal visual acuity and no restricted eye movements. Obliteration of the nasolabial fold was present. The skin over the swelling had an orange peel appearance with interspersed multiple nodular eruptions. Swelling was firm to hard in consistency and nontender. CT scan revealed expansile soft-tissue lesion involving the right infraorbital and cheek region [Figures 5 and 6]. Incisional biopsy and histopathological examination of the lesion suggested actinomycosis. The swelling and the symptoms did not subside with the oral Augmentin (amoxycillin 500 mg and potassium clavulanate 125 mg) for 7 days following incisional biopsy. Hence, oral administration of Bactrim DS (combination of sulfamethoxazole 800 mg and trimethoprim 160 mg) twice daily is advised for a period of 1 year after obtaining opinion from the physician. The patient responded positively to the antibiotic therapy and there is regression of the lesion [Figures 7 and 8].
Figure 4.

Profile picture of the patient showing diffuse swelling with multiple nodular projections
Figure 5.
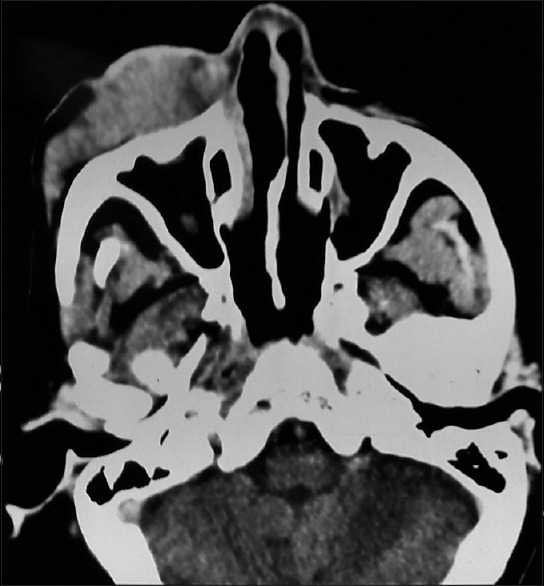
Axial computed tomography scan section showing soft-tissue lesion not involving the maxillary sinus
Figure 6.

Coronal computed tomography section showing diffuse soft tissue involving the right infraorbital and cheek region
Figure 7.

Photograph of the patient 5 months following antibiotic therapy showing regression of the swelling and the eruptions
Figure 8.

Intraoral examination of the patient did not reveal any apparent traces of the lesion
DISCUSSION
Actinomyces are nonspore-forming, filamentous, and facultative anaerobes. They are normal constituents of the oral flora within gingival crevices and tonsillar crypts and are particularly prevalent in periodontal pockets, dental plaques, and on carious teeth.[3] A retrospective study done in the University of Cologne reported the incidence of actinomycotic infection affecting the mandible (53.6%), cheek (16.4%), chin (13.3%), submaxillary ramus and angle (10.7%), maxilla (5.7%), and temporomandibular joints (0.3%).[4,5] About half of the patients diagnosed with actinomycosis have a history of local trauma resulting in mucosal breakdown.[1] Actinomyces bacteria cannot penetrate healthy tissue, and mucosal breakdown is a prerequisite for infection. Poor dental hygiene, caries, oral trauma, dental extraction, and an immunocompromised status are considered to be important antecedents.[1] Moreover, as reported in the present case reports, the first patient had a history of dental extraction supporting the prerequisite, mucosal breakdown for the infection and the second patient had a history of local trauma followed by infection of the wound. A hallmark of cervicofacial actinomycosis is the tendency to spread without regard for anatomical barriers, including fascial planes or lymphatic drainage, and the development of multiple sinus tracts.[2] A malignant neoplasm may also result in an enhancing solid mass, but the lesion usually has a relatively well-defined margin, without substantial inflammatory change in the adjacent soft tissue unless it is complicated by infection.[4] The lack of lymphadenopathy despite a large, aggressive-appearing mass with an inflammatory change may be a helpful clue in differentiating cervicofacial actinomycosis from a malignancy.[4]
Diagnostic imaging technologies such as CT and magnetic resonance imaging usually yield nonspecific findings, contributing only to define radiological features of the mass and its involvement in adjacent soft tissues.[5] Culture and isolation of the bacteria make the definitive diagnosis of the disease. However, Actinomyces growth is very difficult even on appropriate anaerobic media with the recovery from culture being <50%.[6] Possible suppressive effect of prior antibiotic therapy could also be attributed to the negative culture of the bacteria. Several authors agree that incisional biopsy can be of great help in the diagnosis of actinomycosis. The typical microscopic finding always consistent with diagnosis of actinomycosis is an outer zone of granulation and a central zone of necrosis containing multiple basophilic granules that represent lobulated microcolonies of Actinomyces.[5] In both the cases reported in the present article, though the organism could not be cultured, the histopathological examination of the incisional biopsy specimens was suggestive of actinomycosis. Final diagnosis should be made based on clinical findings in combination with bacteriological and/or histopathological findings.[7]
Antibiotics, especially penicillins, form the cornerstone for treatment of actinomycosis.[8] The organism is readily susceptible to the β-lactam antibiotics. Harvey, Cantrell and Fischer were the first to routinely use prolonged high-dose penicillin therapy for actinomycosis, advocating “initial massive penicillin therapy, wide surgical excision of infected tissue, and long-continued penicillin therapy in a dosage of 2–5 million IU per day for 12–18 months after excision.”[9] Long-term antibiotic therapy eradicates all signs of activity of the disease and precludes the reactivation. In recent series, 3–6 weeks of oral antibiotic therapy, combined with surgical drainage, has been curative for cervicofacial actinomycosis.[10] For patients who had more advanced disease and for those who did not respond to penicillins, penicillin therapy is often alternated with sulfa drugs such as sulfamethoxazole. Since the patient in the second case report was unresponsive to the previous antibiotic therapy and the lesion being aggressive involving the orbital region, antibiotic Bactrim Ds was advised.
Surgical therapy is often indicated for curettage of bone, resection of necrotic tissue, excision of sinus tracts, and drainage of soft-tissue abscesses.[11] Surgical excision remains the fundamental therapy for soft-tissue tumors secondarily infected with actinomycosis as reported in the first case and the last resolutive approach for the infections that are unresponsive to antimicrobial therapy.
CONCLUSION
Appropriate diagnosis greatly influences the prognosis of cervicofacial actinomycosis, the great masquerade of head-and-neck disease. A negative culture of the bacteria does not exclude the diagnosis of the disease. Even though surgery plays an important role in the diagnosis and treatment of actinomycosis, recurrence following surgery alone is very common and wide excision of the lesion results in morbidity. A multidisciplinary approach with antibiotic therapy and surgical management is advised for lesions unresponsive to antimicrobial therapy.
Declaration of patient consent
The authors certify that they have obtained appropriate consent from both the patients to publish images and clinical information to be reported in the journal. The patients understand that due efforts will be made to conceal their identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck. 1999;21:264–8. doi: 10.1002/(sici)1097-0347(199905)21:3<264::aid-hed12>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 2.Pradhan S, Datta NR, Prasad KN, Ayyagari S, Pandey R. Actinomycosis mimicking carcinoma of the maxillary sinus. Indian J Cancer. 1993;30:1–4. [PubMed] [Google Scholar]
- 3.Lerner PI. The lumpy jaw. Cervicofacial actinomycosis. Infect Dis Clin North Am. 1988;2:203–20. [PubMed] [Google Scholar]
- 4.Bochev V, Angelova I, Tsankov N. Cervicofacial actinomycosis – Report of two cases. Acta Dermatovenerol APA. 2003;12:105–8. [Google Scholar]
- 5.Vorasubin N, Wu AW, Day C, Suh JD. Invasive sinonasal actinomycosis: Case report and literature review. Laryngoscope. 2013;123:334–8. doi: 10.1002/lary.23477. [DOI] [PubMed] [Google Scholar]
- 6.Yadav SP, Chanda R, Gathwala G, Yadav RK. Actinomycosis of tonsil masquerading as tumor in a 12-year old child. Int J Pediatr Otorhinolaryngol. 2002;63:73–5. doi: 10.1016/s0165-5876(01)00647-4. [DOI] [PubMed] [Google Scholar]
- 7.Park JK, Lee HK, Ha HK, Choi HY, Choi CG. Cervicofacial actinomycosis: CT and MR imaging findings in seven patients. AJNR Am J Neuroradiol. 2003;24:331–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Martin MV. The use of oral amoxycillin for the treatment of actinomycosis. A clinical and in vitro study. Br Dent J. 1984;156:252–4. doi: 10.1038/sj.bdj.4805331. [DOI] [PubMed] [Google Scholar]
- 9.Harvey JC, Cantrell JR, Fisher AM. Actinomycosis: Its recognition and treatment. Ann Intern Med. 1957;46:868–85. doi: 10.7326/0003-4819-46-5-868. [DOI] [PubMed] [Google Scholar]
- 10.Moghimi M, Salentijn E, Debets-Ossenkop Y, Karagozoglu KH, Forouzanfar T. Treatment of cervicofacial actinomycosis: A report of 19 cases and review of literature. Med Oral Patol Oral Cir Bucal. 2013;18:e627–32. doi: 10.4317/medoral.19124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oostman O, Smego RA. Cervicofacial actinomycosis: Diagnosis and management. Curr Infect Dis Rep. 2005;7:170–4. doi: 10.1007/s11908-005-0030-0. [DOI] [PubMed] [Google Scholar]


