Abstract
Background:
A clinical study was undertaken on the management of zygomatic complex fractures using various surgical approaches in the Department of Oral and Maxillofacial surgery during the past 3 years.
Aims:
The aim of this study is to evaluate the versatility of various surgical approaches.
Materials and Methods:
A total of 15 cases were selected following a clinical and radiological examination of fractures of the zygomatic complex. A standard pro forma was used to record the case history and findings. These cases were treated by mini plate or micro plate osteosynthesis. Reduction techniques used were Gillie's temporal approach, Dingman's lateral eyebrow approach, upper buccal sulcus approach, and inferior orbital approach. Fixations were done either by mini plate or micro plate osteosynthesis. To compare the effectiveness of the reduction and fixation techniques the following parameters were assessed: facial symmetry-corrected/unaltered, wound healing-good/impaired, mouth opening good/restricted, diplopia-present/absent, infraorbital nerve – present/absent.
Results and Conclusion:
Successful surgical treatment of the zygomatic complex fracture is influenced by its geometry. Whether the alignment may be successfully achieved or not by open reduction at single or multiple locations, can vary with the individual surgeon's experience.
Keywords: Fixation, reduction, zygomatic fractures
INTRODUCTION
Orofacial injuries produce psychological, physical and economic consequences of great importance to the patient. Because of these considerations, the surgeon must direct his efforts toward the restoration of esthetic and function as expeditiously as possible.
The zygomatic bone/zygoma/malar bone is frequently involved in midfacial trauma because of its prominence and location. Any disruption of zygomatic position has great functional significance on the contour of the face. For both cosmetic and functional reasons, it is important that zygomatic injuries must be accurately diagnosed and properly treated.
Various methods for the repair of zygomatico complex fracture have been advocated by many surgeons with emphasis on the type of incision, methods of fixation and at times even reconstruction. The treatment of fractured zygomatic complex is carried out by various intraoral and extraoral methods. Among the various treatment options available, the extraoral approaches provide access for direct fixation at frontozygomatic, zygomatic maxillary sutures and intraoral approach provide access to zygomatic buttress.
The recent application of the rigid internal fixation by miniplates or microplates has outdated all other fixation techniques as it provides stabilization in all three planes of space.
Aim and objectives
-
To evaluate the versatility of various surgical approaches such as:
- Gillie's temporal approach
- Dingmans lateral eyebrow approach
- Upper buccal sulcus approach and
- Inferior orbital rim approach
For reduction and fixation of zygomatic complex fractures based on ease of accessibility, amount of exposure obtained, and post-operative esthetics.
MATERIALS AND METHODS
The material for this study consisted of cases with zygomatic complex fractures that were admitted and treated as in patients in the Department of Oral and Maxillofacial surgery at Sree Balaji Dental College and Hospital, Chennai. Those who required closed reduction, open reduction, and fixation to manage the fractures were candidates for this study. A total of 15 cases were selected following a clinical and radiological examination of fractures of the zygomatic complex. A prospective study was conducted.
After accessing the general condition of the patients, all the cases were performed under general anesthesia. After reduction, fixations were done either by mini plate or micro plate osteosynthesis. Postoperatively, all the patients were administered antibiotics which were continued for 7 days.
The following parameters were assessed to compare the effectiveness of the reduction and fixation techniques:
Facial symmetry-corrected/unaltered
Wound healing-good/impaired
Mouth opening-good/restricted
Diplopia-present/absent
Infraorbital nerve – present/absent.
Armamentarium
The armamentarium is illustrated in Figure 1.
Figure 1.

Armamentarium
Method
Closed reduction techniques
Gillie's temporal approach
In this approach, a 2 cm incision is made approximately 45° to the upper limit of the attachment of the external ear.[1] The incision is made through the skin and subcutaneous tissue at an angle running from anterosuperior to the posteroinferior area and carried down until the white glistening surface of the temporal fascia is visualized [Figure 2]. Blunt dissection is then done through the subcutaneous tissue. A second deeper incision is carefully placed to the full length of the skin incision until the temporalis bulge is seen.
Figure 2.
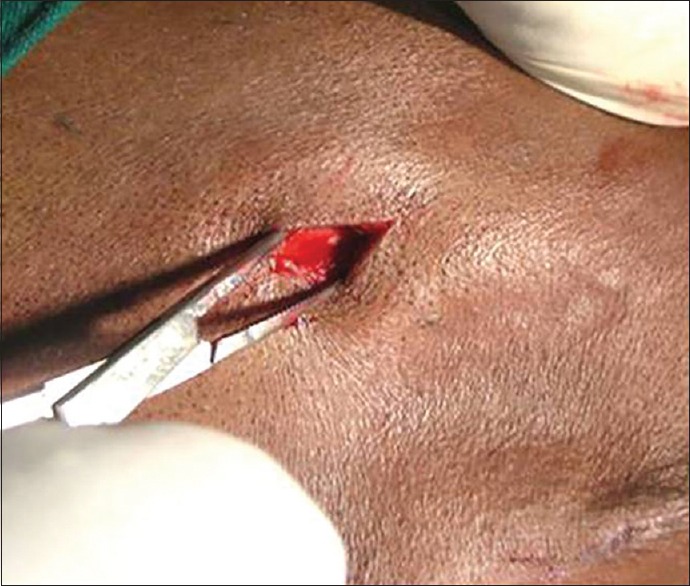
Gille's incision
A flat instrument such as a large Freer elevator or broad end of no 9 periosteal elevator is inserted between the temporalis muscle and temporalis fascia.
The instrument is swept back and forth while the tip is moved inferiorly to the medial aspect of the zygomatic arch and infratemporal surface of the body of the zygoma. In medially displaced fracture, it may be difficult to pass the instrument medial to the zygomatic arch. In this instance, the tip of the instrument must be placed medially until the medial aspect of the zygomatic arch is reduced.
The Rowe's zygomatic elevator is then passed beneath the periosteal elevator, as it is withdrawn. When stabilizing, the handle is kept in position and lifting handle is activated. Once Rowe's zygomatic elevator is in proper depth, the external handle is elevated while the other handle stabilizes the working blade position [Figure 3]. Firm anterior, superior, and lateral elevation is applied to the body of the zygoma and the arch. An audible crunch or crack sound usually accompanies the elevation; later, instrument working blade is swept posteriorly and laterally, reducing any zygomatic arch fracture. Once verification of adequate reduction and resistance to displacement has been accomplished the elevator is withdrawn and the incision is closed in one or two layer with vicryl or chromic catgut 9 [Figure 4].
Figure 3.

Fixation
Figure 4.

Wound closure
Dingmans lateral eyebrow approach
In this approach, before skin incision, the lateral orbital rim was palpated to confirm the location of the fracture site which is located at the frontozygomatic suture.[2] The skin is kept taut over the orbital rim using two fingers. A 1.5 cm long incision is made at the lateral portion of the eyebrow [Figure 5].
Figure 5.

Upper buccal sulcus incision and exposure at fracture site
The dissection is then carried out sharply and bluntly through the subcutaneous tissue down to the bone.
The periosteum is incised and reflected from the bone and the fracture is visualized at frontozygomatic suture line. A Rowe's zygomatic elevator is passed through the incision behind and lateral to orbital margin into temporal fossa. The elevator is passed behind the temporal aponeurosis. The elevator may either be passed under the zygomatic arch to lift it laterally or under the body of the zygoma to lift it upward, forward, laterally and outward movement. The displaced segment was then repositioned correctly. During respositioning, the zygoma was palpated through the skin along the infraorbital margin for checking continuity of the rim, in case of fracture involving the infraorbital rim and guided into position [Figure 6].
Figure 6.
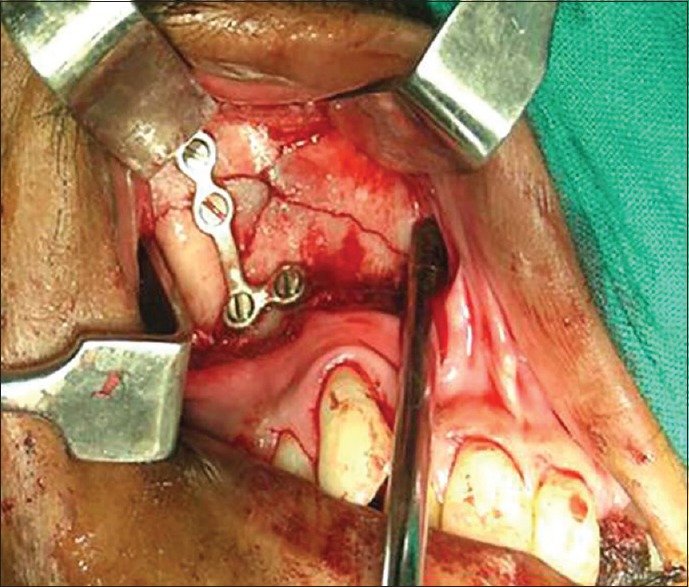
Miniplate fixation at zygomatic buttress
Drill holes were placed through the bone 5mm to each side of fracture sites after reduction at frontozygomatic suture using handpiece with bur and saline 26G stainless steel wires were passed through the holes and twisted to maintain the bony fragments in anatomical reduction [Figure 7].
Figure 7.

Wound closure
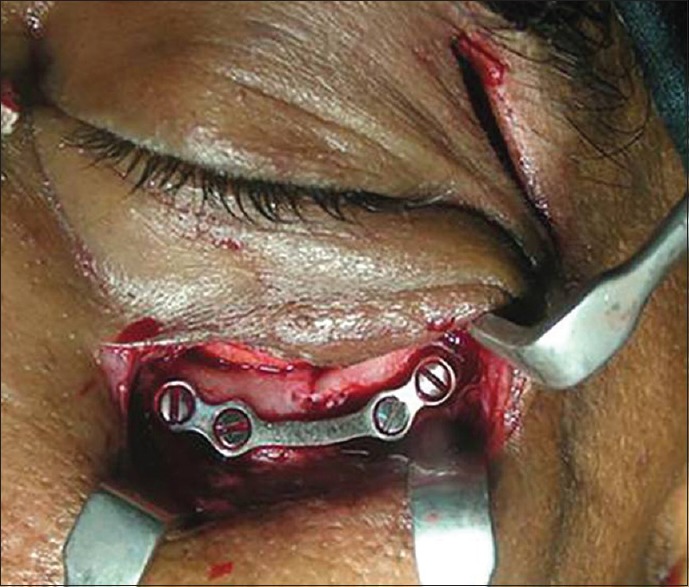
Low infraorbital approach
The infraorbital rim incision is made in the eyelid skin several millimeter above the inferior orbital rim [Figure 8]. Blunt dissection of the orbicularis muscle is carried out until the periosteum of the inferior orbital rim is reached. Another incision is made through the periosteum which was reflected. The rim is reduced either through Dingman's lateral eyebrow approach or Gillie's temporal approach or intraoral buccal sulcus approach.[3] After reduction and obtaining the continuity of the inferior orbital rim, the fragment is stabilized with miniplate osteosynthesis [Figure 9].
Figure 8.
Dingman's lateral eye brow approach incision
Figure 9.
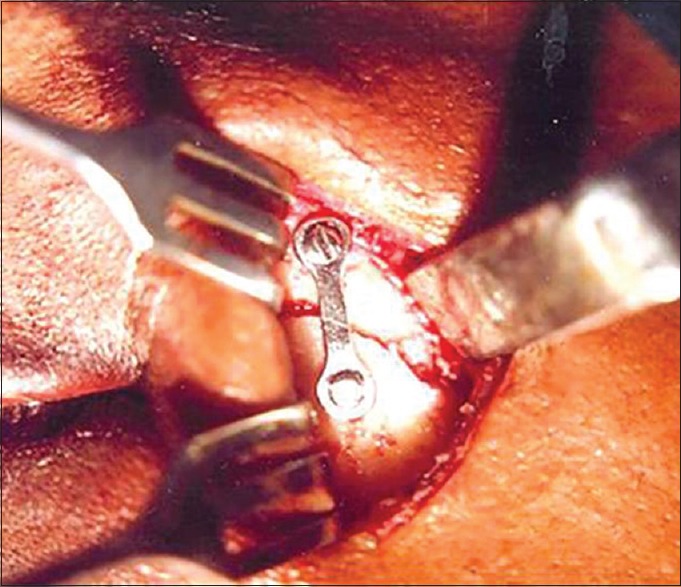
Miniplate fixation at frontozygomatic suture
The wound is well irrigated with saline and closed by two layers-the muscle layer with vicryl and skin by mersilk suture material.
Upper buccal sulcus approach
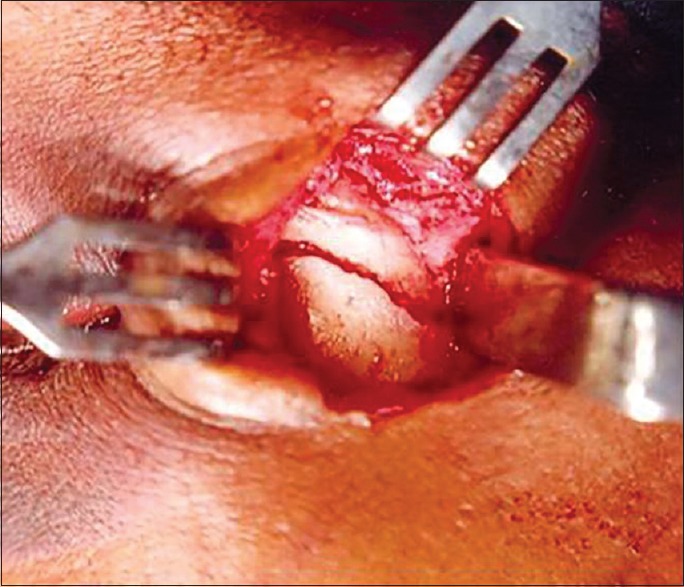
In this approach, a small incision approximately 1cm is made in the mucobuccal fold, just beneath the zygomatic buttress of the maxilla [Figure 10]. The sharp end of no. 9 periosteal elevator or curved freer elevator or Taylor monk's elevator is inserted into the incision and using a side-to-side sweeping motion, the surgeon makes contact with the infratemporal surface of maxilla, zygoma and zygomatic arch and dissects the tissue in a supra periosteal manner.[4] A heavier instrument such as Rowe's zygomatic elevator can then be inserted behind the infratemporal surface of the zygoma and using superior, lateral and anterior force [Figure 11]. The surgeon reduces the bone. In cases of zygomatic buttress fracture, the fragments can be aligned and fixed with four hole miniplate after reduction and stabilized with screws, wound well irrigated with saline [Figure 12]. The incision in the mucobuccal fold is sutured with silk.
Figure 10.

Low infraorbital approach incision placed over existing wound
Figure 11.

Exposed fracture site
Figure 12.
Miniplate fixation at infraorbital margin
RESULTS
A total of 15 patients with fractures of the zygomatic complex were treated in this study. Nine cases had isolated fractures of the zygomatic complex with displacement.
Six cases had mandibular fractures in addition to the displaced zygomatic fracture and one case of fracture involving zygomatic arch alone. The various aspects evaluated in this study are recorded in Tables 1–4.
Table 1.
Preoperative evaluation
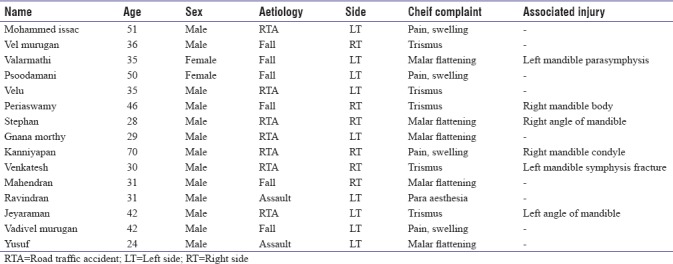
Table 4.
Postoperative evaluation
Out of 15 patients, 10 (70%) patients had functional complaints; 5 patients (30%) had a cosmetic complaint of flattening of the malar prominence[Table 1].
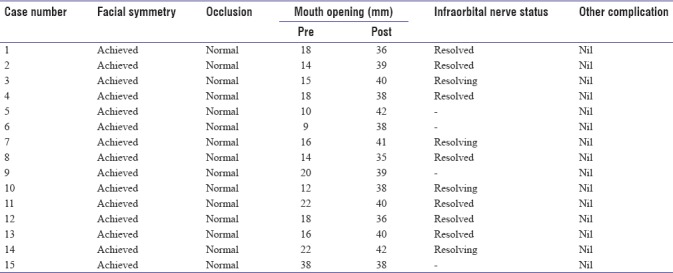
11 (70%) patients had a sensory disturbance of the infraorbital nerve following trauma. Among five patients who complained of trismus their interincisal opening ranged from 8 mm to 20 mm. Flattening of malar prominence was marked in five cases and to varying degree in rest of the cases. Step defects were palpable at frontozygomatic suture region in twelve cases, at the infraorbital margin in six cases, zygomatic buttress in five cases [Table 2].
Table 2.
Clinical features
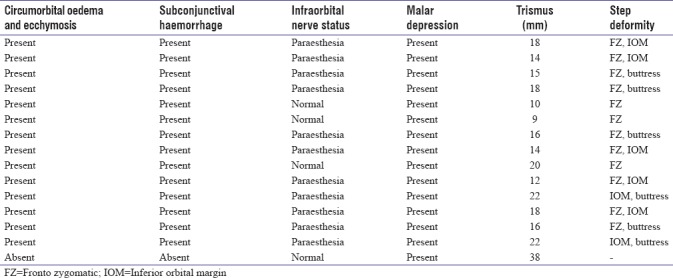
Table 3 shows the operative procedures performed. The earliest intervention was done after 4 days and the latest after 10 days.
Table 3.
Operative procedure
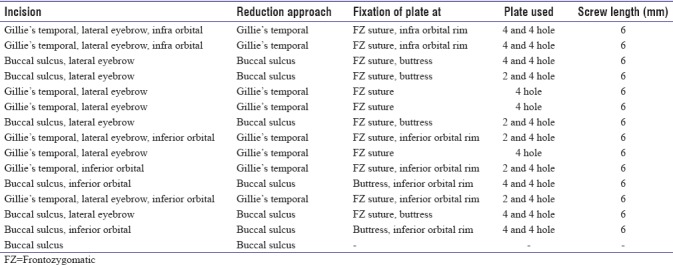
Table 4 shows the post-operative evaluation of the patients. Postoperatively, jaw opening had improved in those cases with limitation in mouth opening up to 35 mm to 40 mm of inter incisial opening. Post-operative infection was treated with thorough debridement and a course of proper antibiotic therapy. Miniplates or microplates fixation were done in all cases.
DISCUSSION
The zygomatico maxillary complex (ZMC) is an essential element of the facial configuration.
Because of its location, it is subjected to trauma more often than any other element of the face. The consequences of such injuries may involve ocular function, facial esthetics, and mandibular mobility.
The susceptibility of zygomatic bone fracture is explained by Markus zing et al. due to its prominent location in the face.[5] It is the most commonly fractured bone after the nasal bone as stated by Vernard et al.[6]
The major cause of zygomatic complex fractures in the present study was road traffic accidents which accounted for 75% of the entire sample, as stated by Marciani.[7] The second most common cause was accidental fall (15%), followed by assault (10%).
The incidence of zygomatic complex fractures peak around the second and third decades in males and fourth and fifth decades in females with fractures being common in males in a ratio of approximately 4:1 (Edward Ellis).[8] In our study, the age of the patient ranged from 24 to 70 years with peak age group of 24 to 42 years.
Fractures of the zygomatic complex comprises about 60% of all facial bones requiring treatment. Some form of fixation may be required following reduction although the incidence of fractures needing stabilization has been variably reported as 100% (matsunga), 40% (Knight and north), and 25% (jayhoyt). Fractures without displacement do not require surgery (kruger). In fact, Ellis et al. in his study reported that 23% of their 2067 cases did not receive surgical intervention. Important factor to be remembered in the reduction of zygomatic fracture is the time element, the earliest permissible time after the accident is considered ideal.
ZMC fracture, may at times present challenging diagnostic and reconstruction problems for the surgeon.
The method of treatment varies depending on the type of fracture, the delay in treatment, the general condition of the patient, the surgeon's armamentarium and experience.
Various methods for the repair of ZMC fractures has been advocated by many surgeons with emphasis on the types of incisions, methods of fixation, and at times even reconstruction.[9] In order to obtain standardization of treatment, several classifications of ZMC fractures have evolved, based on clinical and radiological examination.
The principle management of ZMC fractures are similar to the principles of management of fractures elsewhere in skeletal system.[10]
The principle management involves the reduction of the fractured fragments to their normal anatomical relationship to provide bony contact and alignment. Excessive muscular force and motion at the site of fracture stimulate non osteogenic cells to invade the area which results in fibrous union. Therefore accurate anatomic reduction, fixation is a must to achieve the healing of fractured bone.
In our study out of fifteen cases of ZMC fractures, in eight cases fracture reduction was done by Gillie's temporal approach. This method of reduction was simple and quite effective with no visible scar as noted by James Hoyt and Ogden. In seven cases, Upper Buccal Sulcus approach was used for reduction of the fracture satisfactorily.
Its advantages are no skin scar, closer and more precise application of force by the operator, placement of bone plates at the buttress possible through the same incision, minimal bleeding, simplified antral bone harvest if required, and simple mucosal closure.
In four out of the seven cases, fixation at the zygomatic buttress was done through the same incision by miniplate or microplate osteosynthesis.
Reduction and fixation of the zygomatic complex fracture was satisfactorily achieved in eleven cases through Dingman's lateral eyebrow approach in the present study which correlates the same as that of Pozatek et al.
The lateral eyebrow incision resulted in cosmetically acceptable scar in all the cases of present study. We were able to reduce all the fractures easily through the incision.
Open reduction and internal fixation by mini plate was done in relation to Frontozygomatic suture via Dingman's lateral eyebrow approach. In five cases with communited fracture of ZMC, reduction and fixation was done by two hole mini plate at Frontozygomatic suture and one four holed Miniplate was fixed at the infraorbital rim via a infraorbital approach and one four holed Miniplate at the Zygomatico maxillary suture.
The low infraorbital approach have the following advantages
Simple incision
Avoidance of the orbital septum and periorbital fat
Nonexistent postoperative ectropion.
In six cases reduction at the infraorbital margin was achieved through this method and fixation done by Miniplate osteosynthesis.
The recent application of rigid fixation techniques for zygomatic complex fracture has outdated all the older technique of fixation.
There is no better method of providing stabilization to the unstable zygomatic fractures than to rigidly secure it internally.
The obvious advantage to bone plate is that it provides stabilization in three planes. The technique of mini plate osteo synthesis for stable fixation of zygomatic bone fracture was first described by Michelet, Ian Jackson, Fain et al. who used Champy mini plates in the treatment of midface and zygomatic bone fractures.
In our study there was no displacement of the zygomatic fracture after fixation by mini plate or micro plate as it gives stability in three planes and facial symmetry was corrected.
With regard to healing of fractured fragments and occurrence of ophthalmic signs like diplopia, our results were in accordance with the results of Cassini. No neurological deficits were found in this study which correlates with the studies by Ian Jackson, who reported that after mini plate osteo synthesis, neurological complications were about 50% lower than those treated by wire osteo synthesis.
On all the above cases, bradycardia was produced during reduction of zygomatic arch fractures which correlates with that of study conducted by J Loewinger.
The possible mechanism is occulo cardiac reflux; where the afferent pathway is through the short cilliary nerves and the ophthalmic division of trigeminal nerve through the Gasserian ganglion and hence to the main sensory nucleus of the trigeminal nerve. The efferent pathway is via the vagus nerve which release acetylcholine that produces bradycardia by increasing the parasympathetic tone; furthermore, the bradycardia disappeared promptly once the stimulus is ceased. This reflex is known to be a potential hazard of ophthalmic surgery. This reflex should be recognized as a potential hazard.
It is not always necessary to explore the orbital floor in such fractures. Fractures involving >50% of the orbital floor or defects measuring 1 to 2 cm[2] should be explored and repaired.[11,12,13,14,15] The usual shape of this muscle is elliptical. Rounding of the inferior rectus muscle and lying mainly within the maxillary sinus on coronal CT view indicate an increase in orbital volume, resulting in symptomatic enophthalmos.[16,17] In our study, the orbital floor was explored in a displaced fracture, with increasing rates of exploration seen if the patient has symptomatic diplopia.
CONCLUSION
It can be concluded from the study that:
Zygomatic complex fractures are the most common facial injuries of the midfacial skeleton
Dingman's lateral eyebrow incision gives excellent direct access and visibility to frontozygomatic suture for reduction and fixation with minimal scar
Infraorbital incision used to expose infra orbital rim gives excellent exposure of infraorbital rim from medial to the lateral end. However, it has disadvantage of producing visible scar
Upper buccal sulcus which can be used for both reduction and placement of bone plates at the zygomatic buttress through the same incision with the advantages of no skin scar.
Successful surgical treatment of the zygomatic complex fracture is influenced by its geometry. Whether the alignment may be successfully achieved or not by open reduction at single or multiple locations, can vary with the individual surgeon's experience.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Snehalata P, Ravi SP. Zygomatic arch fracture reduction via Gillie's (Temporal) approach: Report of 3 cases. Indian J Mednodent Allied Sci. 2014;2:126–9. [Google Scholar]
- 2.Dingman RO, Natvig P. Surgery of Facial Fractures. Philadelphia: W.B. Saunders Co; 1964. pp. 212–3. [Google Scholar]
- 3.Juliana DM, Everton LS, Micena RM. Comparison of cutaneous incisions to approach the infraorbital rim and orbital floor. Braz J Oral Sci. 2009;8:88–91. [Google Scholar]
- 4.Chuong R, Kaban LB. Fractures of the zygomatic complex. J Oral Maxillofac Surg. 1986;44:283–8. doi: 10.1016/0278-2391(86)90079-0. [DOI] [PubMed] [Google Scholar]
- 5.Zingg M, Laedrach K, Chen J, Chowdhury K, Vuillemin T, Sutter F, et al. Classification and treatment of zygomatic fractures: A review of 1,025 cases. J Oral Maxillofac Surg. 1992;50:778–90. doi: 10.1016/0278-2391(92)90266-3. [DOI] [PubMed] [Google Scholar]
- 6.Vernard RJ, Joseph AA, Sanford G, Corpus C. Balloon technique for treatment of fractures of the zygomatic bone. J Oral Surg. 1956;14:14–9. [Google Scholar]
- 7.Marciani RD. Management of midface fractures: Fifty years later. J Oral Maxillofac Surg. 1993;51:960–8. doi: 10.1016/s0278-2391(10)80035-7. [DOI] [PubMed] [Google Scholar]
- 8.Ellis E, 3rd, Kittidumkerng W. Analysis of treatment for isolated zygomaticomaxillary complex fractures. J Oral Maxillofac Surg. 1996;54:386–400. doi: 10.1016/s0278-2391(96)90107-x. [DOI] [PubMed] [Google Scholar]
- 9.Esben K. Zygomatico-maxillary fractures. J Cranio Maxillofac Surg. 1989;17:210–4. doi: 10.1016/s1010-5182(89)80070-8. [DOI] [PubMed] [Google Scholar]
- 10.Pozatek ZW, Kaban LB, Guralnick WC. Fractures of the zygomatic complex: An evaluation of surgical management with special emphasis on the eyebrow approach. J Oral Surg. 1973;31:141–8. [PubMed] [Google Scholar]
- 11.Yab K, Tajima S, Ohba S. Displacements of eyeball in orbital blowout fractures. Plast Reconstr Surg. 1997;100:1409–17. doi: 10.1097/00006534-199711000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Tahernia A, Erdmann D, Follmar K, Mukundan S, Grimes J, Marcus JR, et al. Clinical implications of orbital volume change in the management of isolated and zygomaticomaxillary complex-associated orbital floor injuries. Plast Reconstr Surg. 2009;123:968–75. doi: 10.1097/PRS.0b013e318199f486. [DOI] [PubMed] [Google Scholar]
- 13.Hawes MJ, Dortzbach RK. Surgery on orbital floor fractures. Influence of time of repair and fracture size. Ophthalmology. 1983;90:1066–70. doi: 10.1016/s0161-6420(83)80049-9. [DOI] [PubMed] [Google Scholar]
- 14.Gart MS, Gosain AK. Evidence-based medicine: Orbital floor fractures. Plast Reconstr Surg. 2014;134:1345–55. doi: 10.1097/PRS.0000000000000719. [DOI] [PubMed] [Google Scholar]
- 15.Christensen BJ, Zaid W. Inaugural survey on practice patterns of orbital floor fractures for American oral and maxillofacial surgeons. J Oral Maxillofac Surg. 2016;74:105–22. doi: 10.1016/j.joms.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 16.Chiasson G, Matic DB. Muscle shape as a predictor of traumatic enophthalmos. Craniomaxillofac Trauma Reconstr. 2010;3:125–30. doi: 10.1055/s-0030-1262954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banerjee A, Moore CC, Tse R, Matic D. Rounding of the inferior rectus muscle as an indication of orbital floor fracture with periorbital disruption. J Otolaryngol. 2007;36:175–80. [PubMed] [Google Scholar]


