Abstract
Objective
To evaluate the rate of neointimal development and thrombus formation of surface-modified flow diverters in single antiplatelet therapy (SAPT) using optical coherence tomography (OCT) in a porcine model.
Methods
We divided 10 experimental pigs into two groups. One group (n=6) received dual antiplatelet therapy (DAPT) and the other group (n=4) received SAPT. Four stents (two per carotid artery) were implanted in both groups. The stents used were the Pipeline Flex embolization device (PED Flex), Pipeline Flex with Shield technology (PED Shield), and the Solitaire AB stent. All animals underwent weekly angiography and OCT. The OCT data were analyzed using the following measurements: neointimal ratio ((stent – lumen area)/stent area), stent-coverage ratio (number of stent struts covered by neointima/total stent struts), and the presence or absence of thrombus formation per 1 mm cross-section.
Results
PED Flex and Shield in the SAPT group had higher neointimal ratios than in the DAPT group (P<0.001, respectively). In the DAPT group, the speed of endothelial growth on day 7 in the PED Shield group was higher than that in the PED Flex group (P<0.001). In the SAPT group, PED Flex demonstrated significantly more thrombus formation on day 7 than PED Shield (P<0.001).
Conclusions
The PED Shield stent showed faster endothelial growth than the other devices and comparable neointimal volume. There was significantly less thrombus formation on PED Shield than PED Flex when using SAPT in a porcine model.
Keywords: flow diverter, optical coherence tomography, neointimal formation, antiplatelet therapy, surface modification, phosphorylcholine
Introduction
While flow diverters can introduce thromboembolic complications when used to treat intracranial aneurysms,1–3 a phosphorylcholine (PC) surface-modified flow diverter can be introduced to decrease thrombogenicity. PC is present on the surface of red blood cells. Recently, Medtronic (Irvine, Calfornia, USA) developed a version of its popular Pipeline Flex embolization device (PED Flex) that is modified with PC (PED Shield), with the intent of decreasing platelet adhesion to the implant by mimicking the surface of red blood cells.4 Indeed, platelet adherence and thrombosis have been shown to be inhibited on such PC-coated stents when placed in the peripheral arteries of rabbits, pigs, dogs, and baboons.5–9 Moreover, PC-coated stents have demonstrated no adverse effect on endothelialization.5–7
Dual antiplatelet therapy (DAPT) prior to implanting flow diverters is recommended to prevent thrombotic complications. However, delayed hemorrhagic complication still remains a concern with this modality. Although Hagen et al reported that the PED Shield with acetylsalicylic acid (ASA) alone exhibited similar platelet deposition to the PED Flex with DAPT ex vivo,10 it is unclear whether PC surface-modified stents require less antiplatelet therapy than currently recommended in vivo.10 11
Optical coherence tomography (OCT) is an intravascular high-definition imaging method that allows for in vivo tracking of neointima and thrombus development on the surface of an implanted device. A number of reports have validated the correlation of OCT imaging and histology of the coronary arteries.12 13 Furthermore, we reported a correlation for the development of neointima between OCT images and the histology of the carotid artery in a porcine model.14
We hypothesized that single antiplatelet therapy (SAPT) might be safely applied to PC surface-modified flow diverters. We evaluated and compared the rate of neointimal development and thrombus formation between standard and surface-modified flow diverters receiving SAPT and DAPT.
Methods
The study protocol was approved by the local institutional Animal Care and Use Committee. All animals received humane care in compliance with the Animal Welfare Act and the ‘Guide for the Care and Use of Laboratory Animals’ formulated by the Institute of Laboratory Animal Research (National Research Press, 1996).
We divided the 10 animals into two groups based on the antiplatelet protocol—namely, DAPT (n=6) and SAPT (n=4). The animals were Yorkshire pigs ranging in size from 10 to 35 kg. Both groups started antiplatelet therapy 3 days prior to stenting. The DAPT group received ASA (10 mg/kg) and clopidogrel (10 mg/kg). The SAPT group received only ASA (10 mg/kg), as in a previously reported trial.14 The implanted device sizes were 5×20 mm and 5×12 mm for PEDs and 4×20 mm and 5×20 mm for Solitaire AB, with two of the same kind of device implanted in each carotid artery. All interventions were performed under general anesthesia. Induction of anesthesia was achieved with subcutaneous tiletamine (4.4 mg/kg), xylazine (2.2 mg/kg), and atropine (0.4/mg/kg). After intubation we maintained isoflurane inhalation anesthesia (1.5–3%). The procedure started with a sterile cut-down to the femoral artery and placement of a 6F femoral sheath or percutaneously placed sheath. After sheath insertion, heparin (3000–8000 U) was administered. A 6F guide catheter was navigated to obtain baseline angiography and measurements. We used a 0.027 inch microcatheter to deploy the devices. PED Flex, PED Shield, and Solitaire AB were randomized for implantation into the bilateral carotid arteries with four stents in each experimental pig, with one exception with two stents because of anatomical difficulty. After the procedure the animals stayed under observation until fully recovered. All animals from both groups underwent follow-up angiograms and intravascular imaging with optical coherence tomography (OCT) at three time points (days 7, 14, and 21). During the study we lost one animal from the DAPT group due to an anesthesia complication; follow-up was not possible for this subject.
OCT imaging and analysis
OCT images were obtained using the Dragonfly Optis imaging system (LightLab Imaging, St Jude Medical, Minnesota, USA). In this procedure the OCT catheter is introduced into the 6F guide catheter and advanced over a 0.014 inch microguidewire distal to the implanted stents. A motorized OCT catheter pull-back at a rate of 18.0 mm/s and a simultaneous intra-arterial iodine contrast injection at rates of 4–6 mL/s for a total volume of 16–24 mL to clear the blood from the vessel were used to obtain all OCT images at 180 frames/s.
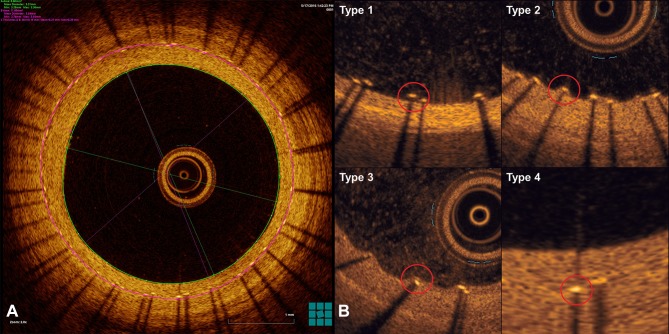
Follow-up digital subtraction angiography and OCT imaging were performed at three time points (days 7, 14, and 21). OCT image analysis was performed with Light Lab post-processing software. Every 1 mm of the OCT image dataset was analyzed. The measurements involved an automated device contour detection algorithm and endoluminal surface detection. Stent struts were manually traced and regions of interest were positioned in the center of the stent struts that showed a bright ’blooming' appearance (figure 1A).3 The following parameters were measured (figure 1A)14: lumen area (defined as contours of the vessel lumen), stent area (identified by circumferential area limited by the contours of the struts), neointimal area (stent area – lumen area), and neointimal ratio ((mean stent – mean lumen area)/mean stent area). OCT imaging was used to classify stent struts as types 1–4, with types 1 and 2 defined as uncovered struts (no neointima) and types 3 and 4 as covered struts (figure 1B).15 The stent-coverage ratio was measured as the number of stent struts covered by neointima/total stent struts. The neointimal ratio was a marker for neointimal volume, with a higher neointimal ratio indicating more neointimal formation. Change in the stent-coverage ratio over time showed the speed of endothelialization of the stent struts.
Figure 1.
Optical coherence tomography imaging. (A) Green and purple circles show the lumen area and stent area, respectively. (B) Stent strut classification is defined from types 1–4 by OCT imaging. Types 1 and 2 are uncovered struts and types 3 and 4 are covered struts (red circle).14
Red thrombus was defined by images showing protrusions into the lumen with high OCT backscattering and attenuation while white thrombus was defined by homogeneous backscattering and low attenuation.16 Thrombus formation was defined as present or absent in every 1 mm cross-section. OCT images were excluded from the analysis if stent struts and lumen contour were not visible in more than 45 degrees.
All pigs were euthanized under deep anesthesia with a lethal dose of potassium chloride on day 21 after the procedure. The vessels with stents were submitted for histology.
OCT data were analyzed by YM, DKJ, and JC.
Statistical analysis
All data are presented as mean±SD. Differences in parametric data were evaluated using a one-way analysis of variance. The Tukey test was used as a post hoc analysis. Non-parametric data between two groups were evaluated by the Mann–Whitney U test, and those among three groups by the Kruskal–Wallis test. The Bonferroni correction for multiple comparisons was performed. SPSS Version 23 (IBM, Armonk, New York, USA) was used for statistical analysis.
Results
The first angiographic follow-up demonstrated a high rate of stent thrombosis for the SAPT group; 6/6 of the PED Flex and 2/6 of PED Shield were occluded. All thrombosed devices underwent successful recanalization after mechanical thrombectomy with aspiration and angioplasty using a non-compliant balloon.14 We decided to amend the protocol and start DAPT for all experimental pigs after the eighth day follow-up results. Thereafter, ASA was administered daily throughout the study in all animals, and 10 mg/kg of clopidogrel was administered after the initial follow-up demonstrating 100% thrombosis of the SAPT group of PED Flex. Subsequent follow-up angiography showed no further implant thrombosis. The number of stents obtained by OCT images were seven PED Flex, seven PED Shield, and four Solitaire AB in the DAPT group, and six PED Flex, six PED Shield, and four Solitaire AB in the SAPT group. A total of 2348 slices on OCT images were evaluated.
Neointimal ratio
The results for the neointimal ratio on day 21 are shown in table 1 and figure 2. The neointimal ratios for the PED Shield and Flex were significantly different from that for Solitaire in both antiplatelet groups (neointimal ratio±SD: PED Flex and Shield vs Solitaire in SAPT and DAPT group, P<0.001, respectively; in total group, P<0.05). The neointimal ratio for PED Shield and Flex was similar in the combined groups. PED Flex and Shield stents showed a significantly higher neointimal ratio in the SAPT group than in the DAPT group (P<0.001, respectively). We found no difference in the neointimal ratio for the Solitaire stent between the SAPT and DAPT groups (P=0.126).
Table 1.
Comparison of neointimal ratio, stent-coverage ratio, and thrombus formation among stents
| Flex | Shield | Solitaire | P value Flex vs Shield |
P value Shield vs Solitaire |
P value Flex vs Solitaire |
|
| Neointimal ratio on day 21 | ||||||
| SAPT | 0.21±0.16* | 0.22±0.11* | 0.044±0.12 | NS | <0.001 | <0.001 |
| DAPT | 0.087±0.10 | 0.095±0.063 | 0.023±0.012 | NS | <0.001 | <0.001 |
| Total | 0.12±0.13 | 0.13±0.098 | 0.032±0.081 | NS | <0.05 | <0.05 |
| Stent-coverage ratio on day 7 | ||||||
| SAPT | 0.82±0.24* | 0.79±0.24* | 0.78±0.22 | NS | NS | NS |
| DAPT | 0.32±0.28 | 0.59±0.36 | 0.81±0.22 | <0.001 | <0.001 | <0.001 |
| Stent-coverage ratio on day 14 | ||||||
| SAPT | 0.93±0.096 | 0.92±0.13 | 0.81±0.28 | NS | NS | NS |
| DAPT | 0.92±0.093 | 0.93±0.13 | 0.90±0.16 | <0.001 | NS | 0.031 |
| Stent-coverage ratio on day 21 | ||||||
| SAPT | 0.96±0.10* | 0.98±0.059* | 0.85±0.27 | NS | 0.011 | NS |
| DAPT | 0.88±0.15 | 0.93±0.12 | 0.86±0.18 | 0.002 | NS | NS |
| %Thrombus formation on day 7 | ||||||
| SAPT | 100±0.00* | 36.36±48.38* | 43.08±49.90 | <0.001 | NS | <0.001 |
| DAPT | 9.42±29.32 | 9.40±29.28 | 33.33±47.35 | ns | <0.001 | <0.001 |
| Total | 39.02±48.90 | 19.41±39.63 | 36.93±48.40 | <0.001 | <0.001 | NS |
*P<0.001 compared with DAPT.
DAPT, dual antiplatelet therapy; Flex, Pipeline Flex embolization device; SAPT, single antiplatelet therapy; Shield, Pipeline Flex embolization with Shield technology.
Figure 2.
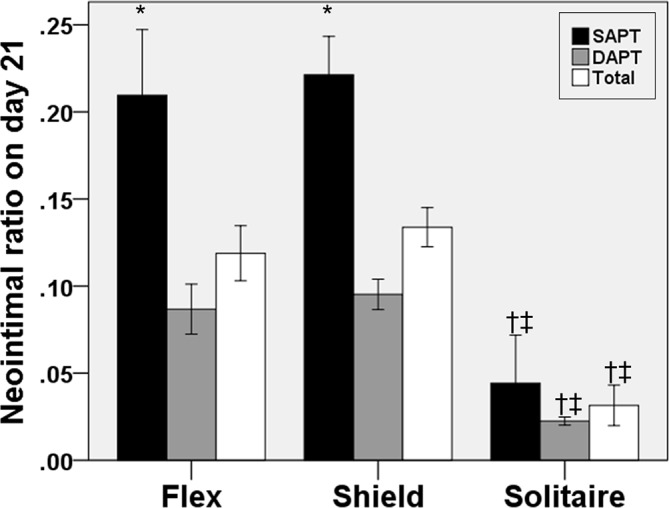
Neointimal ratios on day 21. The PED Flex and Shield showed a significant difference between the SAPT and DAPT protocols. For both protocols, Solitaire demonstrated significantly lower neointimal ratios than PED Flex and Shield. Bars are 95% CI. PED Flex, Pipeline Flex embolization device; PED Shield, Pipeline Flex embolization with Shield technology; SAPT, single antiplatelet therapy; DAPT, dual antiplatelet therapy; Flex, PED Flex; Shield, PED Shield; *P<0.001 compared with DAPT; †P<0.001 compared with PED Flex; ‡P< 0.001 compared with PED Shield.
Stent-coverage ratio
Results for the stent-coverage ratio are shown in table 1 and figure 3. In the DAPT group, PED Shield showed a greater stent-coverage ratio than Flex at every follow-up time point (table 1, figure 3: day 7, P<0.001; day 14, P<0.001; day 21, P=0.002). In the SAPT group we found no difference between the PED Flex and Solitaire group at any follow-up time point. Although there was no difference in the stent-coverage ratio on day 7 between the SAPT PED Shield and the Solitaire group, this ratio on day 21 was significantly increased in the PED Shield group compared with the Solitaire group (P=0.011).
Figure 3.

Stent-coverage ratio over time. For the DAPT protocol, PED Shield showed a significantly higher stent-coverage ratio than PED Flex. In the SAPT group there was no difference between PED Shield and PED Flex at any time point. PED Shield in the SAPT group showed significantly more endothelialization than Solitaire on day 21. PED Flex and Shield both showed higher stent-coverage ratios for the SAPT protocol than the DAPT protocol. PED Flex, Pipeline Flex embolization device; PED Shield, Pipeline Flex embolization with Shield technology; SAPT, single antiplatelet therapy; DAPT, dual antiplatelet therapy; Flex, PED Flex; Shield, PED Shield.
The stent-coverage ratio for PED Flex and Shield was significantly higher in the SAPT group than in the DAPT group on days 7 and 21 (day 7, P<0.001, respectively; day 21, P<0.001, respectively). There was no difference in the stent-coverage ratio between the DAPT and SAPT groups at any time in the follow-up period for the Solitaire stent (day 7, P=0.381; day 14, P=0.196; day 21, P=0.312). Regarding endothelial formation, all devices were almost completely covered by day 21.
Thrombus formation
The results of thrombus formation on the surface of the stent on day 7 are shown in table 1 and figure 4. In the SAPT group, PED Flex showed thrombus for all frames on day 7. In addition, PED Flex showed more thrombus formation than PED Shield or Solitaire (P<0.001, P<0.001). On the other hand, we found no difference for thrombus formation between the PED Shield and Solitaire stents in the SAPT group. In the DAPT group, Solitaire showed significantly more thrombus formation than PED Flex or Shield (P<0.001, P<0.001). When considering both DAPT and SAPT, the percentage of thrombus formation on the surface of the PED Shield was lower than for the other devices (P<0.001, P<0.001).
Figure 4.
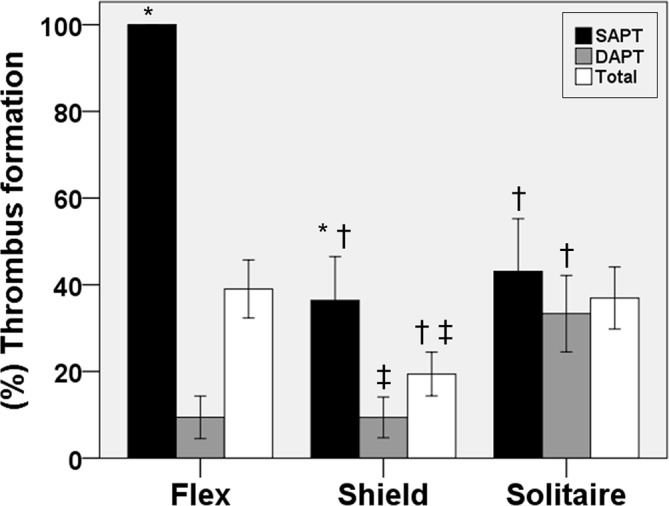
Thrombus formation percentage on day 7. In the SAPT protocol, PED Flex showed thrombus for all frames on day 7. In addition, PED Flex showed more thrombus formation than PED Shield and Solitaire. On the other hand, we found no difference in thrombus formation between PED Shield and the Solitaire stent in the SAPT protocol. In the DAPT protocol, Solitaire showed significantly more thrombus formation than PED Flex or Shield. Bars are 95% CI. PED Flex, Pipeline Flex embolization device; PED Shield, Pipeline Flex embolization with Shield technology; SAPT, single antiplatelet therapy; DAPT, dual antiplatelet therapy; Flex, PED Flex; Shield, PED Shield. *P<0.05 compared with DAPT; †P<0.05 compared with PED Flex; ‡P<0.05 compared with Solitaire.
Discussion
Our study showed that the PED Shield stent had faster endothelial growth and less thrombus formation than PED Flex and Solitaire.
Speed of stent-coverage
In the literature there are reports proposing that coronary PC-coated stents might reduce the rate of re-endothelialization because of inhibition of the deposition of plasma protein onto the stent strut.8 17 However, in the DAPT group we found a significant difference in the stent-coverage ratio for PED Shield compared with PED Flex at each time point of our follow-up until the device was fully covered with neointima. These results could support the notion that the PC effect induces faster endothelialization. On the other hand, in the SAPT group there was no difference in the stent-coverage ratio on day 7 between the PED Shield and the Flex and Solitaire groups. In fact, on day 21 the PED Shield showed more endothelial coverage than Solitaire. These results also suggest that the PED Shield, which has PC surface modification, accelerated the endothelialization process compared with the other devices studied in this porcine model. This result must be further investigated since surface modification could be less thrombogenic immediately after implantation and may also shorten the duration of antiplatelet therapy needed, since complete endothelialization of the device is seen at a significantly earlier time than with the other devices tested. As a result, the PED Shield stent may allow us to discontinue antiplatelet therapy sooner than the current practice and decrease the impact of antiplatelet therapy complications. Additionally, our study also supports previous reports that early endothelialization of the PED Shield reduces the risk of thrombus formation after implantation.18
Neointimal volume
In coronary lesions, excessive neointimal hyperplasia leads to in-stent restenosis.19 We used the neointimal ratio as the index of neointimal volume.14 PED Shield demonstrated no difference for neointimal volume compared with PED Flex in the DAPT and SAPT groups. This finding suggests that PC surface modification results in similar rates of in-stent stenosis or late loss between PED Flex and Shield. However, Caroff et al reported that a surface-modified flow diverter had significantly less in-stent neointimal hyperplasia in a rabbit model.20 The difference in animal model might cause the difference between their result and ours.
Darsaut et al reported that aneurysm occlusion was associated with neointimal closure of the flow diverter pores and the amount of metal surface coverage over the aneurysm ostium.21 We found a significant difference in the neointimal volume between the flow diverter and Solitaire stent in both the SAPT and DAPT groups. The more significant neointimal volume seen in flow diverters during this study may be one of the reasons we see more durable aneurysm occlusion rates with PED Flex and Shield than with Solitaire (lower coverage devices).
Thrombus formation
Some previous studies have reported that platelet adhesion and thrombus are reduced in PC-coated devices.5–8 Our study demonstrated that PED Shield was less thrombogenic than PED Flex in the SAPT group. In addition, in the SAPT group, PED Shield was similar to Solitaire in terms of thrombogenicity, as reported previously.22 Hagen et al reported that PED Shield with aspirin showed similar thrombogenicity to PED Flex under DAPT.10 In a rabbit model, Marosfoi et al reported that PED Shield was associated with less thrombus formation regardless of antiplatelet therapy.9 Our protocol was changed mid-experiment because of the high rate of thrombosis in PED Flex in the SAPT group. We therefore evaluated thrombus formation on day 7 before switching to the DAPT protocol. In our study, PED Shield demonstrated a higher rate of thrombus in the SAPT group compared with PED Flex under DAPT (36.36% vs 9.42%). Based on this animal study, the use of PED Shield with SAPT should still be carefully considered. However, in ruptured cases in whom DAPT or additional surgery such as external ventricular drainage is difficult to administer and shunt placement is necessary, PED Shield could be more feasible than PED Flex.
There are some reports describing an association of thrombus and neointima. The intimal thickening consisted of organizing thrombus.8 Moreover, early thrombus formation and acute inflammation was followed by neointimal growth after bare metal stent implantation.23 24 Our histology showed thrombus covered by neointima in figure 5. In this study, the neointimal volume of the flow diverter was greater in the SAPT group than in the DAPT group. Furthermore, both flow diverters in our results showed a greater stent-coverage ratio at day 7 in the SAPT protocol than in the DAPT protocol. Thrombus could result in more endothelialization. Therefore, these results indicate that thrombus could induce the development of neointimal formation.
Figure 5.
Representative OCT image (left) and histopathological findings (right) in Pipeline Flex embolization device demonstrating the correlation between the two techniques. Left: OCT image shows thrombus on the surface of the stent (red square). Right: Thrombus covered by neointima was shown on magnification (black arrows) in histopathological finding. OCT, optical coherence tomography.
Study limitations
We recognize that this study and its conclusions may have limitations and the translation to clinical practice needs to be carefully considered.
The high rate of thrombosis in the SAPT group caused changes in the antiplatelet therapy protocol and mechanical thrombectomy for recanalization of thrombosed stents. Mechanical thrombectomy for thrombosed PED Flex and Shield could influence endothelialization. Steele et al reported that percutaneous transluminal angioplasty (PTA) could result in endothelial denudation in vessels, followed by complete endothelial regrowth 7 days after PTA.25 Considering this report, the effect of PTA could hardly impact our stent-coverage ratio on day 7 because the measurement for OCT images was performed just after PTA. Therefore, this result may support the notion that thrombus induces more endothelialization.
The follow-up period of our study was just 1 month. Late in-stent restenosis might show different results in long-term follow-up. However, our previous report demonstrated that the concentric neointima in the PED Shield might reduce late in-stent restenosis.14 In addition, this study had few subjects; a larger and longer cohort study is necessary to prove the effect of PC-coated flow diverters. Another limitation is the potential biases of OCT image evaluation of different observers.
Conclusions
This study used OCT to compare endothelial development in different neurovascular implants in vivo. The PED Shield stent showed faster endothelial growth than the other devices and comparable neointimal volume. We observed no difference in thrombus formation on the surface of flow diverters when using DAPT. On the other hand, there was significantly less thrombus formation for the surface-modified flow diverter (PED Shield) compared with PED Flex when using SAPT in a porcine model.
Acknowledgments
The authors thank St Jude Medical for lending them the IlumienOptis analysis system for use in the study, and specifically Michael Chapman and Paul Sahagian for their assistance in troubleshooting the OCT system and creating the pictures. The authors thank Luiza de Lima e Silva Bagno and the Rush University animal laboratory for assistance with this experiment.
Footnotes
Contributors: DL conceived the study. YM, D-KJ and JC executed the study. YM and D-K J performed acquisition of data and YM conducted analysis of data for the work and drafted it. All authors reviewed the final version of the submitted manuscript. DL revised it critically and approved the final version of the manuscript.
Funding: This work was supported by Medtronic and Cure4Stroke Foundation. Material support: PED and PED Shield was given by Medtronic.
Competing interests: JMW is an employee of Medtronic.
Patient consent: Not required.
Ethics approval: Local Institutional Animal Care and Use Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Kallmes DF, Hanel R, Lopes D, et al. . International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol 2015;36:108–15. 10.3174/ajnr.A4111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Murayama Y, Nien YL, Duckwiler G, et al. . Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg 2003;98:959–66. 10.3171/jns.2003.98.5.0959 [DOI] [PubMed] [Google Scholar]
- 3. Shapiro M, Becske T, Sahlein D, et al. . Stent-supported aneurysm coiling: a literature survey of treatment and follow-up. AJNR Am J Neuroradiol 2012;33:159–63. 10.3174/ajnr.A2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Campbell EJ, O’Byrne V, Stratford PW, et al. . Biocompatible surfaces using methacryloylphosphorylcholine laurylmethacrylate copolymer. Asaio J 1994;40:M853–7. 10.1097/00002480-199407000-00118 [DOI] [PubMed] [Google Scholar]
- 5. Chen C, Lumsden AB, Ofenloch JC, et al. . Phosphorylcholine coating of ePTFE grafts reduces neointimal hyperplasia in canine model. Ann Vasc Surg 1997;11:74–9. 10.1007/s100169900013 [DOI] [PubMed] [Google Scholar]
- 6. Kuiper KK, Robinson KA, Chronos NA, et al. . Phosphorylcholine-coated metallic stents in rabbit iliac and porcine coronary arteries. Scand Cardiovasc J 1998;32:261–8. [DOI] [PubMed] [Google Scholar]
- 7. Lewis AL, Stratford PW. Phosphorylcholine-coated stents. J Long Term Eff Med Implants 2002;12:20–50. 10.1615/JLongTermEffMedImplants.v12.i4.20 [DOI] [PubMed] [Google Scholar]
- 8. Whelan DM, van der Giessen WJ, Krabbendam SC, et al. . Biocompatibility of phosphorylcholine coated stents in normal porcine coronary arteries. Heart 2000;83:338–45. 10.1136/heart.83.3.338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marosfoi M, Clarencon F, Langan ET, et al. . Acute thrombus formation on phosphorilcholine surface modified flow diverters. J Neurointerv Surg 2018;10:406–11. 10.1136/neurintsurg-2017-013175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hagen MW, Girdhar G, Wainwright J, et al. . Thrombogenicity of flow diverters in an ex vivo shunt model: effect of phosphorylcholine surface modification. J Neurointerv Surg 2017;9:1006–11. 10.1136/neurintsurg-2016-012612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chiu AHY, Ramesh R, Wenderoth J, et al. . Use of aspirin as sole oral antiplatelet therapy in acute flow diversion for ruptured dissecting aneurysms. BMJ Case Rep 2016:bcr2016012657–3. 10.1136/bcr-2016-012657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fu Q, Hu H, Chen W, et al. . Histological validation of frequency domain optical coherence tomography for the evaluation of neointimal formation after a novel polymer-free sirolimus-eluting stent implantation. Int J Clin Exp Pathol 2015;8:11068–75. [PMC free article] [PubMed] [Google Scholar]
- 13. Lemos PA, Takimura CK, Laurindo FR, et al. . A histopathological comparison of different definitions for quantifying in-stent neointimal tissue: implications for the validity of intracoronary ultrasound and optical coherence tomography measurements. Cardiovasc Diagn Ther 2011;1:3–10. 10.3978/j.issn.2223-3652.2011.10.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Matsuda Y, Chung J, Lopes DK. Analysis of neointima development in flow diverters using optical coherence tomography imaging. J Neurointerv Surg 2018;10:162–7. 10.1136/neurintsurg-2016-012969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murase S, Suzuki Y, Yamaguchi T, et al. . The relationship between re-endothelialization and endothelial function after DES implantation: comparison between paclitaxcel eluting stent and zotarolims eluting stent. Catheter Cardiovasc Interv 2014;83:412–7. 10.1002/ccd.25140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tearney GJ, Regar E, Akasaka T, et al. . Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol 2012;59:1058–72. 10.1016/j.jacc.2011.09.079 [DOI] [PubMed] [Google Scholar]
- 17. Ikada Y. Surface modification of polymers for medical applications. Biomaterials 1994;15:725–36. 10.1016/0142-9612(94)90025-6 [DOI] [PubMed] [Google Scholar]
- 18. Finn AV, Nakazawa G, Joner M, et al. . Vascular responses to drug eluting stents: importance of delayed healing. Arterioscler Thromb Vasc Biol 2007;27:1500–10. 10.1161/ATVBAHA.107.144220 [DOI] [PubMed] [Google Scholar]
- 19. Tahir H, Hoekstra AG, Lorenz E, et al. . Multi-scale simulations of the dynamics of in-stent restenosis: impact of stent deployment and design. Interface Focus 2011;1:365–73. 10.1098/rsfs.2010.0024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Caroff J, Tamura T, King RM, et al. . Phosphorylcholine surface modified flow diverter associated with reduced intimal hyperplasia. J Neurointerv Surg 2018:neurintsurg-2018-013776 10.1136/neurintsurg-2018-013776 [DOI] [PubMed] [Google Scholar]
- 21. Darsaut TE, Bing F, Salazkin I, et al. . Flow diverters can occlude aneurysms and preserve arterial branches: a new experimental model. AJNR Am J Neuroradiol 2012;33:2004–9. 10.3174/ajnr.A3075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Girdhar G, Li J, Kostousov L, et al. . In-vitro thrombogenicity assessment of flow diversion and aneurysm bridging devices. J Thromb Thrombolysis 2015;40:437–43. 10.1007/s11239-015-1228-0 [DOI] [PubMed] [Google Scholar]
- 23. Farb A, Sangiorgi G, Carter AJ, et al. . Pathology of acute and chronic coronary stenting in humans. Circulation 1999;99:44–52. 10.1161/01.CIR.99.1.44 [DOI] [PubMed] [Google Scholar]
- 24. Komatsu R, Ueda M, Naruko T, et al. . Neointimal tissue response at sites of coronary stenting in humans: macroscopic, histological, and immunohistochemical analyses. Circulation 1998;98:224–33. 10.1161/01.CIR.98.3.224 [DOI] [PubMed] [Google Scholar]
- 25. Steele PM, Chesebro JH, Stanson AW, et al. . Balloon angioplasty. Natural history of the pathophysiological response to injury in a pig model. Circ Res 1985;57:105–12. 10.1161/01.RES.57.1.105 [DOI] [PubMed] [Google Scholar]