Abstract
The present study aimed to estimate the differences in rates of prehypertension and hypertension in children and adolescents among three regions with different socioeconomic status in China, and explore the corresponding risk factors associated with prehypertension and hypertension to guide the prevention. Blood pressure measurements of 13 762 children and adolescents aged 6–17 years were obtained from a prospective national survey (the China Health and Nutrition Survey, 1991–2011). Prehypertension and hypertension were defined by age and gender, according to China’s standard criteria. Chi-square tests were used to compare the differences in the prevalence of prehypertension and hypertension among three regions. Trend chi-square tests were used to detect the trends in rates of prehypertension and hypertension over survey years. Logistic regression models were used to detect the potential risk factors of prehypertension and hypertension in children and adolescents. During the survey years, the overall prevalence of prehypertension and hypertension were 6.0% and 10.6%. The corresponding rates in the western region were lowest, but increased rapidly over the two decades (84.0% and 122.6% increases respectively, P<0.001). The overall hypertension rate remained high in the eastern region, despite the slower increase (24.2% increase). In the central region, although the prehypertension rate remained stable, the rate of hypertension had a 94.8% increase these years (P<0.0001). According to the results of logistic regression, age, body mass index (BMI) and waist/height ratio (WHtR) were associated with prehypertension and hypertension. Children and adolescents in the eastern region had the highest level of prehypertension and hypertension, while the rapid increase of blood pressure in the western and central regions were also supposed to concern. Improvement of the healthy lifestyle is urgent for prehypertension and hypertension prevention in children and adolescents.
Introduction
Adult hypertension has been epidemic worldwide and considered as an important risk factor for chronic diseases, such as cardiovascular disease [1]. As a systematic analysis showed, 31.3% of adults in the world had hypertension in 2010 [2]. In China, 27.8% of adults were hypertensive in 2013–2014 [3]. It has been found that the origin of hypertension in adulthood extends back to childhood [4]. Levels of blood pressure have been observed to track over time, and children with elevated blood pressure are more likely to become hypertensive adults [5–6]. Therefore, hypertension among children has become a significant public health issue in the last decades [7–10].
In China, there are various researches concerned on blood pressure in children and adolescents [11–15]. However, a majority of these studies are with limited time and geographic coverage. Socioeconomic status is associated with hypertension [16–18], although the results were ambivalent. Given the marked diversity of economy throughout China, it is necessary to estimate differences of prehypertension and hypertension in areas with varied economic development level. What’s more, the population pattern of hypertension is not static, since it rises and falls over time. A prior survey showed that the prevalence of hypertension in Chinese children and adolescents increased in the recent two decades [19], whereas the trends in the three regions in China remains unclear and they are worthy of exploring, considering the increasingly rapid economic growth and the uneven urbanization in China in recent decades.
Additionally, although a few studies have been conducted to evaluate the risk factors of prehypertension and hypertension in children and adolescents of China [7, 11], few studies were trying to explore the risk factors in different regions, given the different geography, economy and life circumstances.
This study aimed to estimate the differences in the prevalence of prehypertension and hypertension in children and adolescents among the eastern, central and western regions with different socioeconomic status in China, and explore risk factors associated with prehypertension and hypertension by three regions to guide the prevention and control of prehypertension and hypertension. Our data were extracted from the China Health and Nutrition Surveys (CHNSs) conducted during 1991–2011.
Methods
Study population
Data from CHNSs, conducted in 1991, 1993, 1997, 2000, 2004, 2006, 2009 and 2011, were extracted for nine provinces (i.e. Heilongjiang, Liaoning, Shandong, Jiangsu, Henan, Hubei, Hunan, Guangxi and Guizhou). The design and method of this survey were described in detail at the CHNSs website [20, 21]. In brief, those surveys used a stratified multistage random-cluster sampling method to select the sample surveyed in each of the provinces.
Data collection were reviewed and approved by the University of North Carolina and the China Centre for Disease Control and Prevention. The current study was approved by the Ethics Committee of Capital Institute of Paediatrics. All the data were collected from public online sources. All data were fully anonymized and no identifiable information was collected.
Measurements and definitions
The measurements were same with a prior study [7]. Blood pressure was measured by trained examiners using a mercury sphygmomanometer according to a standard protocol [22], and was measured three times on one visit. The three measurements were separated by at least a 1 to 2-min interval, during which the right arm was raised up for 5–6 s. Korotkoff phase 1 and Korotkoff phase 5 were used for defining systolic blood pressure (SBP) and diastolic blood pressure (DBP) respectively. The average of blood pressure values of three times was reported.
The criteria for pre-hypertension and hypertension were according to the age- and gender-specific blood pressure reference standard for Chinese children and adolescents [23]. Hypertension was defined as average SBP and/or DBP that is ≥95th percentile for gender and age, and pre-hypertension in children was defined as average SBP or DBP levels that are ≥90th percentile but <95th percentile.
Participants’ age was dichotomised into 6–12 year (children) and 13–17 year (adolescents) [24], and both genders (boy and girl) were recruited. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. The criteria to define overweight and obesity was proposed by the IOTF using age- and gender-specific BMI reference standard [25]. Abdominal obesity was defined as WHtR (waist/height ratio, calculated as waist circumferences divided height) ≥0.5 [26]. The regions of surveyed provinces were divided into three parts (eastern, central and western regions), as defined by the National Bureau of Statistics of China according to sociodemographic status, in which the eastern region included Liaoning, Jiangsu and Shandong, the central region included Heilongjiang, Henan, Hubei, and Hunan, and the western region included Guizhou and Gansu [27]. Location was divided into urban and rural areas. The urbanization index was collected and divided into quartiles, which consists of 12 components [28]. Information of 3-day average energy, carbohydrate, fat and protein were collected and divided into quartiles.
Statistical analysis
Mean (SD) or median [interquartile ranges (IQR)] was used to present continuous variable and frequencies (%) to present categorical variable. Significant differences among the variables are determined by analysis of variance (ANOVA) for normally distributed variables, Kruskal-Wallis tests for skewed distributed variables, and chi-square tests for categorical data accordingly. Additionally, the differences across the three regions were following tested by Bonferroni adjustments for multiple comparisons. For each of the 3 comparisons, a significance level of P = 0.0167 (0.05/3) provided an overall type I error rate of 0.05. Trend chi-square test was used to detect the trends in rates of prehypertension and hypertension over survey years. Logistic regression models were used to detect the associations between the prevalence of prehypertension and hypertension and potential risk factors, including year (1991–1997, 2000–2006 and 2009–2011), location (urban and rural areas), urbanization index [Q1 (the lowest quartile), Q2, Q3 and Q4 (the highest quartile)], age (6–12, 13–17 years), sex (male, female), BMI (thin and normal, overweight and obesity), abdominal obesity (no, yes), tobacco consumption (no, yes), alcohol consumption (no, yes), 3-day average energy (Q1, Q2, Q3 and Q4), 3-day average carbohydrate (Q1, Q2, Q3 and Q4), 3-day average fat (Q1, Q2, Q3 and Q4), 3-day average protein (Q1, Q2, Q3 and Q4).
Results
Characteristics of participants
From 1991 to 2011, 16 181 children and adolescents were recruited for surveys, among whom 13 762 (85.1%) participants were included with blood pressure values were available. The population characteristics were comparable between children and adolescents included in our study and those excluded (P>0.05), except those excluded from this analysis were older (P<0.001). Among the 13 762 children and adolescents, 4030 (29.3%), 5476 (39.8%) and 4256 (30.9%) were respectively from the eastern, central and western regions. 3899 (28.3%) were in urban areas, while 9863 (71.7%) were in rural areas. The mean age was 11.7 (3.1) years, with 8052 (58.5%) and 5710 (41.5%) were respectively children and adolescents. 7205 (52.4%) were male, and 6557 (47.7%) were female. Those overweight accounted for 6.7% (902), and 251 (1.9%) were obesity. The characteristics of participants according to the three regions are shown in Table 1. The mean age and proportion of male were similar among the three regions (P>0.05), while the distributions of obesity status, urban residence, urbanisation index and the life risk factors differed significantly by region (P<0.0001). The eastern region, as the most developed area in China, was with the highest urbanisation index, the largest proportions of urban residents as well as children and adolescents who were overweight or obesity. The children and adolescents in the western region were with higher tobacco and alcohol consumption, and lower energy, carbohydrate, fat and protein intake, compared with those in the eastern and central regions.
Table 1. Characteristics of participants stratified by region.
| Characteristics | Region | P | ||
|---|---|---|---|---|
| Eastern | Central | Western | ||
| Year | <0.0001 | |||
| 1991 | 777 (19.3) | 841 (15.4) | 746 (17.5) | |
| 1993 | 745 (18.5) | 867 (15.8) | 654 (15.4) | |
| 1997 | 451 (11.2) | 1145 (20.9) | 669 (15.7) | |
| 2000 | 656 (16.3) | 1001 (18.3) | 544 (12.8) | |
| 2004 | 385 (9.6) | 550 (10.0) | 364 (8.6) | |
| 2006 | 268 (6.7) | 480 (8.8) | 373 (8.8) | |
| 2009 | 246 (6.1) | 278 (5.1) | 366 (8.6) | |
| 2011 | 502 (12.5) | 314 (5.7) | 540 (12.7) | |
| Location | <0.0001 | |||
| Urban | 1063 (26.4) | 1538 (28.1) | 1298 (30.5) | |
| Rural | 2967 (73.6) | 3938 (71.9) | 2958 (69.5) | |
| Urbanisation index | <0.0001 | |||
| Q1 (the lowest quartile) | 795 (19.7) | 1503 (27.5) | 1142 (26.8) | |
| Q2 | 861 (21.4) | 1538 (28.1) | 1036 (24.3) | |
| Q3 | 1161 (28.8) | 1293 (23.6) | 994 (23.4) | |
| Q4 (the highest quartile) | 1213 (30.1) | 1142 (20.9) | 1084 (25.5) | |
| Age, y | 0.037 | |||
| Children (6~12) | 2295 (57.0) | 3262 (59.6) | 2495 (58.6) | |
| Adolescents (13~17) | 1735 (43.1) | 2214 (40.4) | 1761 (41.4) | |
| Sex | 0.436 | |||
| Male | 2093 (51.9) | 2849 (52.0) | 2263 (53.2) | |
| Female | 1937 (48.1) | 2849 (48.0) | 1993 (46.8) | |
| Blood Pressure | <0.0001 | |||
| Normotension | 3199 (79.4) | 4503 (82.2) | 3770 (88.6) | |
| Prehypertension | 266 (6.6) | 365 (6.7) | 200 (4.7) | |
| Hypertension | 565 (14.0) | 608 (11.1) | 286 (6.7) | |
| Obesity status | <0.0001 | |||
| Thin and Normal | 3334 (85.3) | 4938 (92.3) | 4022 (96.1) | |
| Overweight | 449 (11.5) | 324 (6.1) | 129 (3.1) | |
| Obesity | 126 (3.2) | 89 (1.7) | 36 (0.9) | |
| Abdominal obesity | <0.0001 | |||
| No | 2477 (88.1) | 3715 (92.5) | 3042 (94.4) | |
| Yes | 334 (11.9) | 303 (7.5) | 179 (5.6) | |
| Tobacco consumption | <0.0001 | |||
| No | 4004 (99.4) | 5418 (98.9) | 4175 (98.1) | |
| Yes | 26 (0.7) | 58 (1.1) | 81 (1.9) | |
| Alcohol consumption | <0.001 | |||
| No | 3924 (97.4) | 5316 (97.1) | 4080 (95.9) | |
| Yes | 106 (2.6) | 160 (2.9) | 176 (4.1) | |
| 3-day average energy, kcal | <0.0001 | |||
| Q1 (the lowest quartile) | 989 (24.5) | 1263 (23.1) | 1188 (27.9) | |
| Q2 | 958 (23.8) | 1363 (24.9) | 1120 (26.3) | |
| Q3 | 1061 (26.3) | 1400 (25.6) | 980 (23.0) | |
| Q4 (the highest quartile) | 1022 (25.4) | 1450 (26.5) | 968 (22.7) | |
| 3-day average carbohydrate, g | <0.0001 | |||
| Q1 (the lowest quartile) | 1185 (29.4) | 1108 (20.2) | 1147 (27.0) | |
| Q2 | 961 (23.9) | 1426 (26.0) | 1054 (24.8) | |
| Q3 | 925 (23.0) | 1485 (27.1) | 1031 (24.2) | |
| Q4 (the highest quartile) | 959 (23.8) | 1457 (26.6) | 1024 (24.1) | |
| 3-day average fat, g | <0.0001 | |||
| Q1 (the lowest quartile) | 870 (21.6) | 1485 (27.1) | 1085 (25.5) | |
| Q2 | 1000 (24.8) | 1330 (24.3) | 1111 (26.1) | |
| Q3 | 1035 (25.7) | 1313 (24.0) | 1093 (25.7) | |
| Q4 (the highest quartile) | 1125 (27.9) | 1348 (24.6) | 967 (22.7) | |
| 3-day average protein, g | <0.0001 | |||
| Q1 (the lowest quartile) | 776 (19.3) | 1363 (24.9) | 1301 (30.6) | |
| Q2 | 881 (21.9) | 1437 (26.2) | 1123 (26.4) | |
| Q3 | 1093 (27.1) | 1369 (25.0) | 979 (23.0) | |
| Q4 (the highest quartile) | 1280 (31.8) | 1307 (23.9) | 853 (20.0) | |
| Urbanisation index, median (IQR) | 55.3 (41.3–73.5) | 47.9 (37.8–65.1) | 50.4 (38.0–68.8) | <0.0001 |
| Age, y, mean (SD) | 11.8 (3.1) | 11.7 (3.0) | 11.7 (3.1) | 0.080 |
| BMI, kg/m2, median (IQR) | 18.0 (16.0–20.3) | 17.1 (15.4–19.2) | 16.4 (15.0–18.5) | <0.0001 |
| SBP, mmHg, median (IQR) | 100.0 (90.0–110.0) | 99.3 (90.0–108.0) | 94.3 (88.7–102.7) | <0.0001 |
| DBP, mmHg, median (IQR) | 66.0 (60.0–70.7) | 64.0 (60.0–70.0) | 60.7 (58.0–69.3) | <0.0001 |
Values are shown as n (%), unless indicated otherwise. IQR, interquartile range; SD, standard deviation; Q, quartile.
Prevalence of prehypertension and hypertension
Children and adolescents were classified into three groups, which were normotensive, prehypertension and hypertension, according to the level of blood pressure. The overall prevalence of prehypertension and hypertension in children and adolescents was 6.0% and 10.6%, respectively. Across the study period, the overall prevalence of prehypertension and hypertension in children and adolescents was significantly different in the regions (P<0.0001). For the prehypertension of all survey years, the rates in the eastern, central and western regions were 6.6%, 6.7% and 4.7%. Under multiple comparisons, the overall prehypertension rates in the eastern and central regions were similar (P>0.0167), but significantly higher than that in the western region (P<0.0167). The hypertension rate was highest in the eastern region (14.0%), following by that in the central region (11.1%), and that in the western region was the lowest (6.7%). In 1991, the rates of prehypertension in the eastern, central and western regions were 4.3%, 6.1% and 2.8%, respectively (P = 0.007); the rates of hypertension in these corresponding regions were 11.1%, 7.9% and 4.2% (P<0.0001). In 2011, the rates of prehypertension in the corresponding regions were 10.8%, 4.8% and 5.2% (P<0.001); the hypertension rates were respectively 13.8%, 15.3% and 9.3% (P = 0.017).
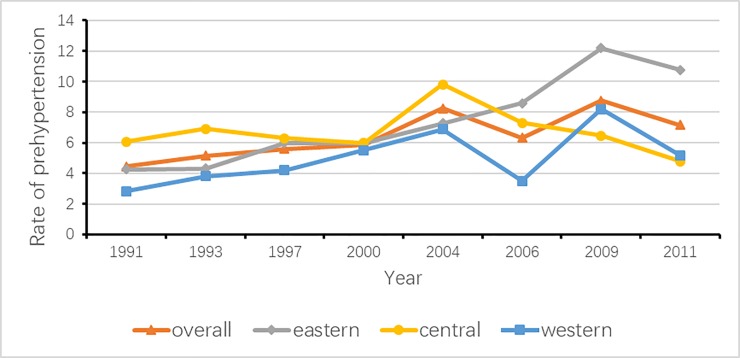
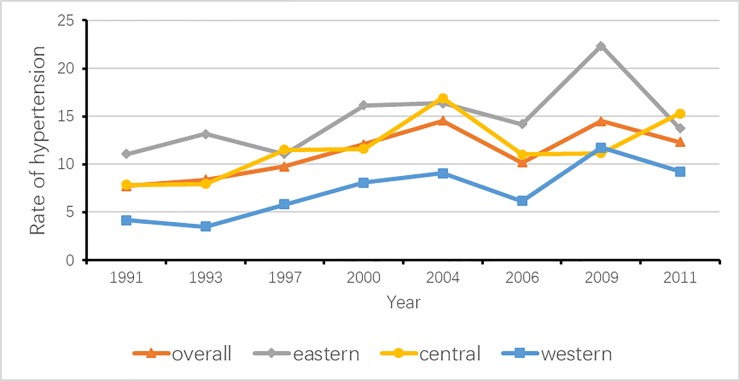
In addition, as Fig 1 and Fig 2 show, the yearly total prevalence of prehypertension and that of hypertension, as well as the corresponding prevalence according to the three regions, were compared to explore the variation tendency. From 1991 to 2011, the trajectories in the rates of prehypertension and hypertension were similar, except the trend of prehypertension in the central region. The total prevalence of prehypertension significantly increased from 4.4% to 7.2% (P<0.0001), and the prevalence of hypertension increased from 7.7% to 12.3% (P<0.0001). For children and adolescents in the eastern region, the prevalence of prehypertension increased from 4.3% in 1991 to 10.8% in 2011 (P<0.0001), and prevalence of hypertension increased from 11.1% in 1991 to 22.4% in 2009, and then decreased to 13.8% (P = 0.001). For those in the central region, the incidence of prehypertension remained stable from 6.1% in 1991 to 4.8% in 2011 (P = 0.589), while the rate of hypertension increased from 7.9% in 1991 to 15.3% in 2011 (P<0.0001). The prehypertension prevalence for those in the western region significantly rose from 2.8% in 1991 to 5.2% in 2011 (P = 0.001); in the meantime, the corresponding hypertension rate significantly increased from 4.2% in 1991 to 9.3% in 2011 (P<0.0001).
Fig 1. Trends of prehypertension by survey years.
Fig 2. Trends of hypertension by survey years.
Logistic regression analyses
The potential factors of prehypertension and hypertension versus normotension in children and adolescents were explored. Table 2 showed the general results of crude and adjusted ORs for these potential factors. A few associations were still significant after adjustments. After adjustments, we found that adolescents were at a higher risk of prehypertension and hypertension than children (adjusted OR: 2.483; 95%CI: 2.213, 2.786; P<0.0001). Overweight children and adolescents had nearly 2 fold increased risk of developing prehypertension and hypertension (adjusted OR: 1.954; 95%CI: 1.619, 2.357; P<0.0001) and obese children and adolescents had more than 2 fold increased risk of developing prehypertension and hypertension compared with those with healthy or low weight (adjusted OR: 2.427; 95%CI: 1.757, 3.354; P<0.0001); a similar pattern existed for abdominal obesity (adjusted OR: 1.706; 95%CI: 1.421, 2.049; P<0.0001).
Table 2. Factors associated with prehypertension and hypertension.
| Variables | Crude OR (95%CI) | P | Adjusted OR (95%CI) | P |
|---|---|---|---|---|
| Year | ||||
| 1991~1997 | Ref | |||
| 2000~2006 | 1.278 (1.165, 1.403) | <0.0001 | 1.271 (1.115, 1.447) | <0.001 |
| 2009~2011 | 1.415 (1.263, 1.585) | <0.0001 | 1.452 (1.234, 1.708) | <0.0001 |
| Location | ||||
| Urban | Ref | Ref | ||
| Rural | 0.816 (0.740, 0.899) | <0.0001 | 0.938 (0.827, 1.065) | 0.324 |
| Urbanization index | ||||
| Q1 (the lowest quartile) | Ref | Ref | ||
| Q2 | 1.047 (0.944, 1.160) | 0.385 | 1.041 (0.878, 1.233) | 0.645 |
| Q3 | 0.919 (0.828, 1.021) | 0.116 | 0.895 (0.752, 1.065) | 0.212 |
| Q4 (the highest quartile) | 1.422 (1.288, 1.569) | <0.0001 | 1.008 (0.837, 1.215) | 0.933 |
| Age, y | ||||
| Child (6~12) | Ref | Ref | ||
| Adolescent (13~17) | 2.518 (2.297, 2.760) | <0.0001 | 2.483 (2.213, 2.786) | <0.0001 |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 1.006 (0.920, 1.101) | 0.894 | 1.083 (0.970, 1.207) | 0.155 |
| BMI, kg/m2 | ||||
| Thin and Normal | Ref | Ref | ||
| Overweight | 2.135 (1.834, 2.485) | <0.0001 | 1.954 (1.619, 2.357) | <0.0001 |
| Obesity | 2.438 (1.864, 3.189) | <0.0001 | 2.427 (1.757, 3.354) | <0.0001 |
| Abdominal obesity | ||||
| No | Ref | Ref | ||
| Yes | 2.320 (1.983, 1.983) | <0.0001 | 1.706 (1.421, 2.049) | <0.0001 |
| Tobacco consumption | ||||
| No | Ref | Ref | ||
| Yes | 1.780 (1.254, 2.528) | 0.001 | 1.157 (0.740, 1.811) | 0.522 |
| Alcohol consumption | ||||
| No | Ref | Ref | ||
| Yes | 2.008 (1.624, 2.484) | 2.484 | 1.135 (0.854, 1.510) | 0.383 |
| 3-day average energy, kcal | ||||
| Q1 (the lowest quartile) | Ref | Ref | ||
| Q2 | 0.850 (0.764, 0.946) | 0.003 | 1.088 (0.888, 1.332) | 0.416 |
| Q3 | 1.067 (0.963, 1.182) | 0.216 | 1.158 (0.871, 1.541) | 0.313 |
| Q4 (the highest quartile) | 1.316 (1.192, 1.454) | <0.0001 | 1.110 (0.763, 1.613) | 0.586 |
| 3-day average carbohydrate, g | ||||
| Q1 (the lowest quartile) | Ref | Ref | ||
| Q2 | 0.891 (0.801, 0.990) | 0.032 | 0.927 (0.778, 1.103) | 0.392 |
| Q3 | 0.925 (0.833, 1.027) | 0.145 | 0.895 (0.711, 1.127) | 0.345 |
| Q4 (the highest quartile) | 1.227 (1.110, 1.357) | <0.0001 | 1.072 (0.792, 1.451) | 0.652 |
| 3-day average fat, g | ||||
| Q1 (the lowest quartile) | Ref | Ref | ||
| Q2 | 0.976 (0.880, 1.083) | 0.651 | 1.084 (0.920, 1.279) | 0.335 |
| Q3 | 1.035 (0.934, 1.148) | 0.509 | 1.108 (0.927, 1.326) | 0.261 |
| Q4 (the highest quartile) | 1.296 (1.173, 1.432) | 1.432 | 1.058 (0.845, 1.325) | 0.621 |
| 3-day average protein, g | ||||
| Q1 (the lowest quartile) | Ref | Ref | ||
| Q2 | 0.840 (0.755, 0.935) | 0.001 | 0.936 (0.788, 1.112) | 0.454 |
| Q3 | 0.990 (0.892, 1.098) | 0.850 | 0.948 (0.778, 1.155) | 0.594 |
| Q4 (the highest quartile) | 1.472 (1.335, 1.624) | <0.0001 | 1.067 (0.852, 1.335) | 0.575 |
OR, odds ratio; CI, confidence interval; Ref, reference; Q, quartile.
In crude analyses, living in rural areas decreased the corresponding risk (crude OR: 0.816; 95%CI: 0.740, 0.899; P < .0001), while living in the area with high urbanization index increased the risk (crude OR: 1.422; 95%CI: 1.288, 1.569; P<0.0001). Superfluous energy, carbohydrate and protein intake (Q4) were risk factors (P<0.0001), while the corresponding medium intake (Q2) were protective factors (P<0.05). However, these associations mentioned above in crude analyses became non-significant after adjustments (P>0.05).
In the three regions, age and obesity were still associated with increased prehypertension and hypertension. (P<0.01, Table 3). Besides, after adjustments, superfluous carbohydrate intake was positively associated with prehypertension and hypertension in children and adolescents residing in the eastern region (OR: 1.733; 95%CI: 1.019, 2.948; P<0.0001), and alcohol consumption increased the corresponding risk (OR: 1.693; 95%CI: 1.089, 2.630; P<0.0001) in those living in the western region.
Table 3. Factors associated with prehypertension and hypertension in three regions.
| Variables | Eastern | Central | Western | |||
|---|---|---|---|---|---|---|
| Crude OR (95%CI) | Adjusted OR (95%CI) | Crude OR (95%CI) | Adjusted OR (95%CI) | Crude OR (95%CI) | Adjusted OR (95%CI) | |
| Year | ||||||
| 1991–1997 | Ref | |||||
| 2000–2006 | 1.202 (1.024, 1.411) | 1.508 (1.17, 1.943) | 1.301 (1.130, 1.499) | 0.994 (0.825, 1.197) | 1.261 (1.033, 1.033) | 1.596 (1.197, 2.129) |
| 2009–2011 | 1.644 (1.370, 1.973) | 1.892 (1.393, 2.568) | 1.090 (0.876, 1.356) | 0.954 (0.726, 1.254) | 1.800 (1.462, 2.216) | 2.277 (1.637, 3.165) |
| Location | ||||||
| Urban | Ref | |||||
| Rural | 0.690 (0.584, 0.814) | 0.822 (0.64, 1.055) | 0.861 (0.740, 1.001) | 1.062 (0.868, 1.298) | 0.854 (0.698, 1.043) | 0.903 (0.707, 1.152) |
| Urbanization index | ||||||
| Q1 (the lowest quartile) | Ref | |||||
| Q2 | 0.986 (0.818, 1.189) | 0.960 (0.668, 1.38) | 1.101 (0.945, 1.282) | 1.355 (1.065, 1.723) | 1.060 (0.853, 1.318) | 0.861 (0.612, 1.211) |
| Q3 | 0.891 (0.751, 1.057) | 0.791 (0.562, 1.113) | 0.882 (0.746, 1.042) | 1.073 (0.832, 1.384) | 0.930 (0.741, 1.167) | 0.792 (0.553, 1.135) |
| Q4 (the highest quartile) | 1.575 (1.342, 1.848) | 0.965 (0.654, 1.426) | 1.316 (1.118, 1.549) | 1.235 (0.934, 1.633) | 1.326 (1.078, 1.631) | 0.775 (0.537, 1.117) |
| Age, y | ||||||
| Child (6~12) | Ref | |||||
| Adolescent (13~17) | 2.186 (1.872, 2.552) | 2.047 (1.672, 2.506) | 2.422 (2.103, 2.789) | 2.346 (1.969, 2.796) | 3.494 (2.856, 4.276) | 3.456 (2.696, 4.431) |
| Sex | ||||||
| Male | Ref | |||||
| Female | 0.997 (0.856, 1.162) | 1.150 (0.947, 1.395) | 1.101 (0.958, 1.265) | 1.130 (0.955, 1.336) | 0.840 (0.694, 1.016) | 0.893 (0.711, 1.12) |
| BMI | ||||||
| Thin and Normal | Ref | |||||
| Overweight | 1.895 (1.526, 2.352) | 1.666 (1.262, 2.199) | 1.767 (1.368, 2.283) | 1.609 (1.176, 2.200) | 2.553 (1.685, 3.868) | 2.803 (1.708, 4.602) |
| Obesity | 1.830 (1.248, 2.685) | 1.578 (0.972, 2.562) | 2.522 (1.622, 3.923) | 2.372 (1.404, 4.007) | 3.026 (1.450, 6.314) | 4.580 (1.966, 10.668) |
| Abdominal obesity | ||||||
| No | Ref | |||||
| Yes | 2.987 (2.352, 3.793) | 2.430 (1.834, 3.219) | 1.850 (1.425, 2.401) | 1.539 (1.140, 2.078) | 1.447 (0.968, 2.161) | 0.887 (0.553, 1.424) |
| Tobacco consumption | ||||||
| No | Ref | |||||
| Yes | 1.156 (0.463, 0.463) | 0.854 (0.272, 2.681) | 2.103 (1.2, 3.684) | 1.409 (0.692, 2.868) | 2.434 (1.443, 4.105) | 1.096 (0.556, 2.16) |
| Alcohol consumption | ||||||
| No | Ref | |||||
| Yes | 1.540 (1.002, 2.366) | 1.003 (0.528, 1.902) | 2.098 (1.488, 2.959) | 0.881 (0.545, 1.425) | 2.835 (1.992, 4.034) | 1.693 (1.089, 2.630) |
| 3-day average energy, kcal | ||||||
| Q1 (the lowest quartile) | Ref | |||||
| Q2 | 0.868 (0.722, 1.043) | 0.992 (0.689, 1.427) | 0.946 (0.805, 1.112) | 1.260 (0.919, 1.728) | 0.708 (0.563, 0.892) | 1.039 (0.689, 1.567) |
| Q3 | 1.010 (0.849, 1.200) | 1.000 (0.602, 1.659) | 1.090 (0.932, 1.275) | 1.368 (0.878, 2.132) | 1.028 (0.822, 1.285) | 1.162 (0.644, 2.095) |
| Q4 (the highest quartile) | 1.383 (1.169, 1.637) | 0.998 (0.513, 1.945) | 1.116 (0.956, 1.302) | 1.184 (0.661, 2.120) | 1.558 (1.265, 1.919) | 1.383(0.647, 2.955) |
| 3-day average carbohydrate, g | ||||||
| Q1 | Ref | |||||
| Q2 | 0.902 (0.752, 1.082) | 1.103 (0.809, 1.503) | 0.940 (0.802, 1.103) | 0.960 (0.732, 1.259) | 0.786 (0.625, 0.99) | 0.779 (0.540, 1.126) |
| Q3 | 0.911 (0.757, 1.095) | 1.244 (0.828, 1.868) | 0.945 (0.808, 1.106) | 0.872 (0.607, 1.253) | 0.905 (0.905, 1.133) | 0.691 (0.425, 1.125) |
| Q4 | 1.277 (1.073, 1.518) | 1.733 (1.019, 2.948) | 1.156 (0.991, 1.348) | 1.034 (0.644, 1.661) | 1.291 (1.045, 1.594) | 0.765 (0.408, 1.433) |
| 3-day average fat, g | ||||||
| Q1 (the lowest quartile) | Ref | |||||
| Q2 | 1.006 (0.844, 1.201) | 1.285 (0.934, 1.767) | 1.011 (0.861, 1.189) | 1.007 (0.789, 1.286) | 0.908 (0.729, 1.13) | 1.036 (0.74, 1.451) |
| Q3 | 0.989 (0.83, 1.178) | 1.339 (0.952, 1.885) | 1.068 (0.910, 1.254) | 1.020 (0.779, 1.335) | 1.064 (0.86, 1.318) | 1.099 (0.765, 1.579) |
| Q4 (the highest quartile) | 1.357 (1.151, 1.600) | 1.447 (0.960, 2.181) | 1.101 (0.940, 1.29) | 0.899 (0.634, 1.274) | 1.457 (1.181, 1.799) | 0.936 (0.596, 1.471) |
| 3-day average protein, g | ||||||
| Q1 (the lowest quartile) | Ref | |||||
| Q2 | 0.835 (0.690, 1.011) | 0.793 (0.568, 1.107) | 0.910 (0.776, 1.068) | 0.851 (0.654, 1.107) | 0.001 (0.628, 0.984) | 1.039 (0.735, 1.468) |
| Q3 | 0.908 (0.763, 1.081) | 0.760 (0.525, 1.101) | 1.005 (0.857, 1.179) | 0.856 (0.628, 1.167) | 1.003 (0.801, 1.255) | 0.971 (0.647, 1.457) |
| Q4 (the highest quartile) | 1.461 (1.246, 1.712) | 0.790 (0.52, 1.201) | 1.219 (1.042, 1.428) | 0.919 (0.645, 1.31) | 1.674 (1.352, 2.073) | 1.267 (0.794, 2.023) |
OR, odds ratio; CI, confidence interval; ref, reference; Q, quartile.
Discussion
We examined the differences in prehypertension and hypertension rates in children and adolescents according to the eastern, central and western regions in China. For the whole study period, the rates of prehypertension and hypertension were 6.0% and 10.6%, respectively; the prevalence of prehypertension in the eastern and central regions was significantly higher than that in the western region; and the hypertension rate was highest in the eastern region, followed by central region, and that in the western region was lowest. From 1991 to 2011, there were increasing trajectories in the rates of prehypertension and hypertension in the three regions, except the trend of prehypertension rate in the central region.
Children and adolescents in the eastern region had the highest prevalence of pre-hypertension and hypertension over the two decades. According to the Chinese government, the eastern region has been the most developed and has the highest socioeconomic status, maybe leading to the children and adolescents’ intake of more modern convenient diets that are high in sodium and saturated fats and low in vegetables [29], which is an essential factor of blood pressure elevation [30]. In the present study, the rate of prehypertension in the eastern region was 4.3% in 1991 and 10.8% in 2011 respectively, with a 153% increase, while the rate of hypertension in the eastern region increased 24% from 11.1% in 1991 to 13.8% in 2011. The relatively less increase of hypertension rate might result from rising attention toward blood pressure and the implement of lifestyle interventions [31, 32]. What’s more, in the eastern region, although the prehypertension rate was not higher than the hypertension rate, the rate of prehypertension increased rapidly in recent decades. Prehypertension has accounted in no small degree as a precursor of hypertension and has been associated with excess morbidity and mortality from cardiovascular diseases [33]. This rapid increase suggests that much more attention should be given to prehypertension control, such as the lifestyle and frequent blood pressure monitoring necessary to treat prehypertension [34]. In the central region, the prevalence of prehypertension remained stable; on the contrary, its hypertension rate increased from 7.9% to 15.3%, with nearly twice in two decades. Besides, in the western region, the rates of prehypertension and hypertension increased rapidly as well, with 84.0% and 122.6% increase respectively, despite the remaining lowest prevalence of prehypertension and hypertension among the three regions. These variations were in accordance with the development of the economy [35], and the trends in overall blood pressure indicated that controlling blood pressure in relatively less developed areas became a public concern as well. Consistent with the increasing upward trends of prevalence of prehypertension and hypertension reported by other studies [7, 8, 36], the nearly twice rates of prehypertension in the eastern and western regions, as well as hypertension in the central and western regions in our study, indicated the urgency of the high blood pressure prevention in children and adolescents after twenty years urbanization development in China.
We observed overweight and obese children and adolescents respectively had higher possibilities in developing prehypertension and hypertension, consistent with other studies that blood pressure or hypertension were positively correlated with BMI and obesity [11, 14]. The prevalence of overweight and obesity in children and adolescents increased across the latest decades [36, 37], with the enrichment of material consumption. The levels of blood pressure increased in parallel with the increasing BMI among Chinese boys and girls, possibly since some adipocyte-derived factors are linked to blood pressure control, and aberrant production and release of those factors may contribute to the high prevalence of hypertension in the obese population [36, 38, 39]. In this study, we also found the higher risk for adolescents to have prehypertension and hypertension than children, inconsistent with the previous report [7]. The possible reasons for our finding may be due to the complex physiological and hormonal changes during puberty, and sexual maturation during adolescence [40]. It is worth mentioning that the urban location was not significant after adjustments, which might be because the lifestyle, such as the consumption of energy-rich foods, expenditure of energy and social support, was the more important reason. Additionally, alcohol consumption was found to be associated with prehypertension and hypertension in children and adolescents in the western regions, in which the rate of alcohol consumption was higher than that in the eastern and central areas, indicating the need to intervene in the unhealthy lifestyle in these target population, especially in adolescents.
There are some strengths in our study. First, we stratified and analysed the data from three regions with different sociodemographic statuses, which enabled us to estimate the blood pressure situation in regions with different socioeconomic developmental levels. Second, we used China’s standard criteria to identify children and adolescents with prehypertension and hypertension, which made our results comparable with other studies in China. Several limitations also existed in this study. First was that three measurements performed in one visit were used to calculate the mean SBP and DBP and judge the presence of prehypertension and hypertension, which might make the prevalence overrated. Second, causal links could not be evaluated, and some confounding factors could not be avoided since data came from the cross-sectional survey. Furthermore, we only looked at the factors with available data, so other important factors such as the family history of hypertension need to be investigated in future studies.
Conclusions
Children and adolescents in the eastern region had the highest level of prehypertension and hypertension, while the rapid increase of blood pressure in the western and central regions were also supposed to concern. Improvement of the healthy lifestyle is urgent for prehypertension and hypertension prevention in children and adolescents.
Acknowledgments
We warmly thank the participants of the China Health and Nutrition Survey.
Data Availability
The dataset analyzed during this study is available on https://www.cpc.unc.edu/projects/china/data/datasets.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Archives of internal medicine. 1993;153(5):598–615. 10.1001/archinte.1993.00410050036006 [DOI] [PubMed] [Google Scholar]
- 2.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441–50. 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y, Yang L, Wang L, Zhang M, Huang Z, Deng Q, et al. Burden of hypertension in China: A nationally representative survey of 174,621 adults. International journal of cardiology. 2017;227:516–23. 10.1016/j.ijcard.2016.10.110 [DOI] [PubMed] [Google Scholar]
- 4.Berenson GS, Wattigney WA, Bao W, Srinivasan SR, Radhakrishnamurthy B. Rationale to study the early natural history of heart disease: the Bogalusa Heart Study. The American journal of the medical sciences. 1995;310 Suppl 1:S22–8. 10.1097/00000441-199512000-00005 [DOI] [PubMed] [Google Scholar]
- 5.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171–80. 10.1161/CIRCULATIONAHA.107.730366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119(2):237–46. 10.1542/peds.2006-2543 [DOI] [PubMed] [Google Scholar]
- 7.Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, et al. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991–2004. Blood pressure. 2011;20(1):45–53. 10.3109/08037051.2010.524085 [DOI] [PubMed] [Google Scholar]
- 8.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116(13):1488–96. 10.1161/CIRCULATIONAHA.106.683243 [DOI] [PubMed] [Google Scholar]
- 9.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. Jama. 2007;298(8):874–9. 10.1001/jama.298.8.874 [DOI] [PubMed] [Google Scholar]
- 10.Yan W, Liu F, Li X, Wu L, Zhang Y, Cheng Y, et al. Blood pressure percentiles by age and height for non-overweight Chinese children and adolescents: analysis of the China Health and Nutrition Surveys 1991–2009. BMC pediatrics. 2013;13:195 10.1186/1471-2431-13-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung LC, Sung RY, So HK, Wong SN, Lee KW, Lee KP, et al. Prevalence and risk factors for hypertension in Hong Kong Chinese adolescents: waist circumference predicts hypertension, exercise decreases risk. Archives of disease in childhood. 2011;96(9):804–9. 10.1136/adc.2010.202770 [DOI] [PubMed] [Google Scholar]
- 12.Yan WL, Li XS, Wang Q, Huang YD, Zhang WG, Zhai XH, et al. Overweight, high blood pressure and impaired fasting glucose in Uyghur, Han, and Kazakh Chinese children and adolescents. Ethnicity & health. 2015;20(4):365–75. 10.1080/13557858.2014.921894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu X, Shi P, Luo CY, Zhou YF, Yu HT, Guo CY, et al. Prevalence of hypertension in overweight and obese children from a large school-based population in Shanghai, China. BMC public health. 2013;13:24 10.1186/1471-2458-13-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu H, Hu X, Zhang Q, Du S, Fang H, Li Y, et al. The Association of Hypertension with Obesity and Metabolic Abnormalities among Chinese Children. International journal of hypertension. 2011;2011:987159 10.4061/2011/987159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu YH, Reilly KH, Liang YJ, Xi B, Liu JT, Xu DJ, et al. Increase in body mass index, waist circumference and waist-to-height ratio is associated with high blood pressure in children and adolescents in China. The Journal of international medical research. 2011;39(1):23–32. 10.1177/147323001103900103 [DOI] [PubMed] [Google Scholar]
- 16.Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Current opinion in cardiology. 2008;23(4):335–9. 10.1097/HCO.0b013e3283021c70 [DOI] [PubMed] [Google Scholar]
- 17.Tareque MI, Koshio A, Tiedt AD, Hasegawa T. Are the rates of hypertension and diabetes higher in people from lower socioeconomic status in Bangladesh? Results from a nationally representative survey. PloS one. 2015;10(5):e0127954 10.1371/journal.pone.0127954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levine DA, Morgenstern LB, Langa KM, Skolarus LE, Smith MA, Lisabeth LD. Does socioeconomic status or acculturation modify the association between ethnicity and hypertension treatment before stroke? Stroke. 2013;44(11):3243–5. 10.1161/STROKEAHA.113.003051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yan W, Li X, Zhang Y, Niu D, Mu K, Ye Y, et al. Reevaluate secular trends of body size measurements and prevalence of hypertension among Chinese children and adolescents in past two decades. Journal of hypertension. 2016;34(12):2337–43. 10.1097/HJH.0000000000001114 [DOI] [PubMed] [Google Scholar]
- 20.Popkin BM, Paeratakul S, Zhai F, Ge K. Dietary and environmental correlates of obesity in a population study in China. Obesity research. 1995;3 Suppl 2:135s–43s. [DOI] [PubMed] [Google Scholar]
- 21.CHNSs. China Health and Nutrition Survey: Design and Methods. Available from: http://www.cpc.unc.edu/projects/china/about/design.
- 22.Blumenthal S, Epps RP, Heavenrich R, Lauer RM, Lieberman E, Mirkin B, et al. Report of the task force on blood pressure control in children. Pediatrics. 1977;59(5 2 suppl):I-ii, 797–820. [PubMed] [Google Scholar]
- 23.Jie MI, Wang TY, Meng LH, Zhu GJ, Han SM, Zhong Y, et al. Development of blood pressure reference standards for Chinese children and adolescents. Chinese Journal of Evidence-Based Pediatrics. 2010;5(1):4–14. 10.1161/CIRCULATIONAHA.115.017936 PMID: 26671979 [DOI] [Google Scholar]
- 24.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. Jama. 2004;291(17):2107–13. 10.1001/jama.291.17.2107 [DOI] [PubMed] [Google Scholar]
- 25.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ (Clinical research ed). 2000;320(7244):1240–3. 10.1136/bmj.320.7244.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message—'keep your waist circumference to less than half your height'. International journal of obesity (2005). 2006;30(6):988–92. 10.1038/sj.ijo.0803226 [DOI] [PubMed] [Google Scholar]
- 27.National Bureau of Statistics of China. National Real Estate Development and Sales in 2016. Available from: http://www.stats.gov.cn/english/PressRelease/201701/t20170122_1456808.html.
- 28.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Social science & medicine (1982). 2010;71(8):1436–46. 10.1016/j.socscimed.2010.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mittal BV, Singh AK. Hypertension in the developing world: challenges and opportunities. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2010;55(3):590–8. 10.1053/j.ajkd.2009.06.044 [DOI] [PubMed] [Google Scholar]
- 30.Wen M, Li K. PARENTAL AND SIBLING MIGRATION AND HIGH BLOOD PRESSURE AMONG RURAL CHILDREN IN CHINA. Journal of biosocial science, 2016. 48(1): 129–42. 10.1017/S002193201500005X [DOI] [PubMed] [Google Scholar]
- 31.Wan YP, Xu RY, Wu YJ, Chen ZQ, Cai W. Diet intervention on obese children with hypertension in China. World journal of pediatrics: WJP. 2009;5(4):269–74. 10.1007/s12519-009-0051-0 [DOI] [PubMed] [Google Scholar]
- 32.Fu JF, Liang L, Zou CC, Hong F, Wang CL, Wang XM, et al. Prevalence of the metabolic syndrome in Zhejiang Chinese obese children and adolescents and the effect of metformin combined with lifestyle intervention. International journal of obesity (2005). 2007;31(1):15–22. 10.1038/sj.ijo.0803453 [DOI] [PubMed] [Google Scholar]
- 33.Sun Z, Zheng L, Wei Y, Li J, Zhang X, Zhang X, et al. The prevalence of prehypertension and hypertension among rural adults in Liaoning province of China. Clinical cardiology. 2007;30(4):183–7. 10.1002/clc.20073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen C, Yuan Z. Prevalence and risk factors for prehypertension and hypertension among adults in Central China from 2000–2011. Clinical and Experimental Hypertension. 2018:1–10. 10.1080/10641963.2018.1431252 [DOI] [PubMed] [Google Scholar]
- 35.Yao S, Zhang Z. Regional growth in China under economic reforms. Journal of Development Studies, 2001. 38(2): 167–186. 10.1080/00220380412331322301 [DOI] [Google Scholar]
- 36.Dong B, Wang HJ, Wang Z, Liu JS, Ma J. Trends in blood pressure and body mass index among Chinese children and adolescents from 2005 to 2010. American journal of hypertension. 2013;26(8):997–1004. 10.1093/ajh/hpt050 [DOI] [PubMed] [Google Scholar]
- 37.Ji CY, Cheng TO. Epidemic increase in overweight and obesity in Chinese children from 1985 to 2005. International journal of cardiology. 2009;132(1):1–10. 10.1016/j.ijcard.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 38.Yiannikouris F, Gupte M, Putnam K, Cassis L. Adipokines and blood pressure control. Current opinion in nephrology and hypertension. 2010;19(2):195–200. 10.1097/MNH.0b013e3283366cd0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Willig AL, Casazza K, Dulin-Keita A, Franklin FA, Amaya M, Fernandez JR. Adjusting adiposity and body weight measurements for height alters the relationship with blood pressure in children. American journal of hypertension. 2010;23(8):904–10. 10.1038/ajh.2010.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Daniels SR, Obarzanek E, Barton BA, Kimm SY, Similo SL, Morrison JA. Sexual maturation and racial differences in blood pressure in girls: the National Heart, Lung, and Blood Institute Growth and Health Study. The Journal of pediatrics. 1996;129(2):208–13. 10.1016/S0022-3476(96)70244-5 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed during this study is available on https://www.cpc.unc.edu/projects/china/data/datasets.