Abstract
The quality and cost of care in nursing homes depend critically on the number and types of nurses. Recent research suggests that the nursing supply adjusts to macroeconomic conditions. However, prior work has failed to consider the effect of macroeconomic conditions on demand for nurses through the effect on revenues. We test how county-level unemployment rates affect direct-care staffing rates in nursing homes using California data. We exploit the wide variation in the unemployment rates across counties and over time in 2005–2012. We also test whether there are heterogeneous effects of unemployment rates by facility size, staffing level, and profit status. We find that as unemployment rates increase, staffing by registered nurses (RNs) decreases but staffing by licensed practical nurses (LPNs) increases. The increase in LPNs is larger in large nursing homes, nursing homes with higher staffing levels, and in for-profit nursing homes. We also find that as unemployment rates increase, nursing home revenue decreases. While the effect of macroeconomic conditions on nursing supply may be important for cost and quality of care, the mechanism is not simple, direct, or homogeneous for all types of nurses and nursing homes.
Keywords: Recessions, business cycles, nursing homes, nurses
I. Introduction
The quality and cost of care in nursing homes depend critically on the number and types of nurses (Castle, 2008; Zhang, Xinzhi, & Grabowski 2004; Spilsbury et al. 2011; Backhaus et al.2014; Dellefield et al. 2015). Therefore, an important question for policy is what determines both the demand for nurses and the supply of nurses. Health care providers are increasingly being held accountable for the quality and cost of care, and nurses will play an important role in how providers are judged and rewarded under value-based payments (Das et al. 2016). Public and private sector efforts have attempted to grow the nursing supply (Johnson & Johnson 2017; Institute of Medicine 2011), including policies that have focused on minimum staffing levels (Assembly Bill 394) and whether to accredit new schools of nursing (Buerhaus, Auerbach, & Staiger 2014).
Recent research has proposed new ideas about how the number of employed nurses adjusts to macroeconomic conditions in ways unrelated to minimum staffing levels or the number of nursing school graduates. This line of research was originally motivated by Ruhm’s observation that population health improves during recessions. Over a series of papers Ruhm documented that total mortality across the population is inversely correlated with unemployment rates (Ruhm 2000, 2003). More recent research finds that this relationship has changed over time, specifically that the decline in mortality with increased unemployment rates has become smaller and not statistically significant in recent years (Ruhm 2015; Böckerman et al. 2015). Nonetheless, Ruhm’s original observations motivated research that more generally explores the relationship between population health and macroeconomic conditions in ways that remain relevant despite attenuation of the original finding. One line of research has examined this relationship across a number of population groups, including those at prime working age but also in older age groups (Ruhm 2000, 2003) and infants (Dehejia and Lleras-Muney 2004). Given that the effects are seen for segments of the population not typically in the labor force and that the magnitude is too large to derive only from working-age adults, it is hypothesized that mortality changes stem from other mechanisms that fluctuate with unemployment. Explaining the mechanisms behind pro-cyclic mortality has motivated another line of research, including our own.
One prior paper has addressed the question of the mechanism of pro-cyclic mortality. Stevens and colleagues (2015) use state-year panel data models and find that own-group employment-to-population ratios are not positivity correlated with mortality within groups of men and women who are 25–44 years old, 45–61 years old, and older than 62. They also find that nursing home deaths among those age 65 years and older account for the total cyclic variation in mortality. They posit that nursing homes’ contribution to cyclic variation in mortality is driven by counter cyclical staffing in nursing homes. That is, nursing home staffing improves when the economy falters, driving reductions in nursing home deaths. Using nursing home staffing data from the Online Survey Certification and Reporting (OSCAR) from 1990 to 2006, Stevens and colleagues find that as the state unemployment rates rise, the number of nurses working in a nursing home in that state rises as well. They estimate that a 1 percentage-point increase in the unemployment rate raises full-time employment of nurses and aides by about 3 percent. Based on this, they suggest that when the unemployment rate rises, the number of nurses in nursing homes improves to such a degree to explain the decline inmortality rates observed among the elderly.
Our research extends this literature, taking into account both supply and demand of all direct-care staff including nurses and nurses’ aides, whereas prior work has ignored the fact that macroeconomic conditions also affect demand for nurses. We provide a conceptual framework for how changes in the macro economy could affect both the supply and the demand of nursing care. In particular, our frame work explains why the macro economy affects demand, which in turn affects revenues, and builds on the discussion of supply in the prior literature. When unemployment rises and the supply of nurses increases, nursing homes will shift staffing to respond to both greater supply of nurses and lower demand (lower revenues) for nursing home care.
We argue that the effect of macroeconomic conditions on nursing demand is not simple, direct, or homogeneous for all types of providers and direct-care staff — the macro economy affects the different types of staff within nursing homes differently. The change in the supply of direct-care staff may also differ by the unemployment rate. We expect heterogeneity in the response to the unemployment rate — both by types of nurses and by types of providers. Heterogeneity is an important and interesting part of this story.
The main empirical research question is: how does the macroeconomy (as measured by the unemployment rate) affect the net direct-care staffing rates in nursing homes, considering that the effect may vary across types of nurses and types of facilities ? We exploit the wide variation in the unemployment rate across counties and over time during 2005–12 and use data on direct-care staffing in California nursing homes.
Our paper has several innovations. It lays out a conceptual framework of how unemployment affects direct-care staffing levels through both changes in supply and demand, and how that effect may be heterogeneous across types of staff in nursing homes and across types of nursing homes. The conceptual framework motivates the empirical work, which tests how staffing changed in nursing homes as a function of the local unemployment rate. We analyze the best available data on staffing in California, combined with data on county-level unemployment rates. We also conduct a sensitivity analysis using a national sample of nursing homes.
Our results are largely consistent with our conceptual framework, although different than results found by Stevens and colleagues (2015). In general we find that during economic downturns, nursing homes do not change total employment of nurses, but shift from more expensive registered nurses (RNs) to less expensive licensed practical nurses (LPNs). At the same time, they experience a decline in net revenues.
II. Background on Nursing Homes and Staffing
Individuals reside in nursing homes for assistance with long-term care needs, which typically arise from degenerative cognitive and functional impairment. Many nursing homes also provide short-term rehabilitative or post-acute care for patients who need assistance with the transition between a hospital stay and a return home. Nursing home care is typically paid by one of three main sources: Medicaid, covering 63 percent of residents on average; Medicare, covering only post-acute care for 14 percent of residents on average; and private resources, covering 23 percent of residents on average, all based on 2014 statistics (Kaiser Family Foundation 2015).
Nursing homes employ a mix of three main direct-care staff types: Registered Nurses (RNs), who typically have at least a bachelor’s degree; Licensed Practical Nurses (LPNs), who typically complete an associate’s degree; and nurse aides, who are generally minimum-wage workers without post-secondary education or formal nurse training. RNs command higher wages than LPNs (and than nurse aides). RNs observe, assess, and record resident symptoms and progress, overseeing the work of nurse aides and LPNs. RNs also collaborate with physicians in treatment, administration of medications, and development of care plans. LPN responsibilities often include administering medication, charting in the medical record, taking vital signs, and performing wound care (Assisted Living Today 2017). While scope of practice regulations vary somewhat from state to state, LPNs are generally more limited in what they are allowed to do and must practice under supervision of an RN. At the same time, there is some overlap in potential duties and thus the potential for substitution, and duties often look similar for RNs and LPNs in nursing homes (Burger et al. 2009). Finally, nurse aides provide the majority of direct care to residents. This care consists primarily of helping residents with activities of daily living (ADLs) such as eating, dressing, bathing, toileting, and walking (Cawley, Grabowski, and Hirth 2006).
Nursing homes face federal and state regulatory requirements to have a minimum RN presence in the facility and must employ sufficient staff overall to meet care needs, but have some flexibility as to staff mix. For example, nursing homes face federal regulatory requirements to have an RN for at least eight consecutive hours per day and one RN or LPN for the remaining 16 hours. California nursing homes with 60 or more beds must additionally have one full-time RN as the Director of Nursing (Harrington 2010).
Although there is some substitutability among types of staff in nursing homes, the mix of staff is likely to affect quality. Specifically, a substantial literature associates more RN hours, or more RN hours as a proportion of total staff hours, with better patient outcomes as measured by various process and outcome indicators. Examples include improved survival and better functional status (Cohen and Spector 1996), fewer pressure sores (Cohen and Spector 1996; Horn et al. 2005; Konetzka Stearns and Park 2008), fewer urinary tract infections (Horn et al. 2005; Konetzka Stearns and Park 2008), and fewer hospitalizations (Horn et al. 2005). Consumers appear to recognize the importance of staffing as a determinant of quality when choosing a nursing home (Konetzka and Coca Perraillon 2016). Thus, nursing homes face incentives to maintain adequate staffing in order to maintain quality and to attract consumers in addition to regulatory requirements.
III. Review of Relevant Literature
Our conceptual and empirical approach is informed by prior literature on labor supply and demand for nursing home services in response to macroeconomic changes. First, there is evidence to support the idea that changes in nurse labor supply are driven by recessions. During an economic boom, work in a nursing home may be seen as less desirable than work in other settings or than leaving the labor force, due to stress and shift work or to better alternative opportunities (Hanel, Kalb, and Scott 2014). During a recession, however, nurses may increase their nursing labor supply either due to direct loss of non-nursing jobs or due to the added worker effect, which stipulates that the labor supply of one spouse increases when the other spouse loses a job (Stephens 2002). Starting with the direct effect, consider someone with a nursing background who is working in a non-nursing job but then loses her job during a recession. In a recession, as other types of jobs disappear or cut back on hours, those with a nursing degree will be more likely to rejoin the labor force as a nurse (Buerhaus, Auerbach, and Staiger 2009). The labor economics literature has documented that displaced workers on average lose wages and earnings not only in the short-run but also in the long-run (Elsby, Shin, Solon 2016; Krolikowski 2017). The effects are strongest for early career workers who may not yet have found the best match for their skills. Therefore, a person with a nursing background has a great advantage during a recession compared to an otherwise similar person with no nursing background in that the nurse has more options for a new job. Although there is typically downward wage rigidity within the same job, displaced workers often take a new job at a lower wage (Elsby, Shin, Solon 2016).
The added worker effect, whereby one spouse increases labor supply after the other loses a job, is the second important way that nursing supply could change during a recession. Using the Current Population Survey, Buerhaus and colleagues (2009) show that trends in nurse employment increased during two recent recessions. The authors speculate that this is motivated in part by anticipated declines in spousal income during recessions, when the spouse loses (or fears losing) a job, or is forced to cut back on hours. In short, as other jobs disappear, the labor supply of nurses can increase as people come out of retirement, are willing to increase their hours, or in the longer run, get more education and training.
In the general population, evidence for an added worker effects is weak (Maloney 1991; Stephens 2002). However, an added worker effect for nurses in particular is supported by empirical economic research (Nicholson and Propper 2012). A 2003 review of the nurse labor supply literature found that a number of studies documented that a spouse’s wage and household income are negatively associated with a nurse’s labor force participation (Antonazzo et al. 2003). The added worker effect has been posited to be stronger for nurses than for other types of professions, in part because health care jobs are seen as less vulnerable to recessions and in part because the majority of RNs are married women who might move in and out of the labor force in response to the spouse’s employment status (Staiger, Auerbach, and Buerhaus 2012). Stephens (2002) finds that high-income families have much stronger added worker effects than low-income families, but also points out that theoeretically the result could go either way and it is an empirical issue. A person with a nursing background, including training to be an LPN or aide, is in a much stronger position to seek employment than a person who lacks such training.
Research on the nursing workforce may not apply equally across all categories of direct-care staff. Studies of the labor supply of nurse aides are scarcer than for licensed nurses, but evidence also suggests that local economic conditions have a significant effect on nurse aide turnover and retention in nursing homes similar in direction to that for nurses (Stone and Wiener 2001). The supply of nurse aides may increase as workers shift from non-health sectors more affected by a recession (such as child care or retail or manufacturing) to health care. These shifts may be more pronounced for LPNs and nurse aides because they earn lower wages than RNs and their education (especially for nurse aides) is not as sector-specific. Thus, increases in the wage rate for nursing home work during a recession are even more likely to elicit additional participation by LPNs and nurse aides than for RNs.
Empirical evidence is consistent with heterogeneity by nurse type. Hanel and colleagues (2014) found that the nursing supply elastiticy varies by education — specifically that nurses with higher education have more inelastic supply. A recent economic analysis of California data found that RN employment fell slightly during the recession of 2008–10 but increased slightly during the recovery (Yoo et al. 2017). However, the responsiveness to unemployment does not appear to be the same for LPNs and aides as for RNs. Baughman and Smith (2012) show that direct-care workers in nursing homes are more responsive and have longer duration of employment when the unemployment rate is high. One of the contributions of our study is to capture this heterogeneity, comparing changes in nursing home employment for RNs, LPNs, and aides. separately in response to changes in the economy.
For all categories of staff, the outward shifts in labor supply during a recession may be mitigated by the availability of unemployment insurance; however, the broader literature on unemployment benefits has generally found these effects to be small – neglible for unemployment status and effectively zero for labor force participation (Figura and Barnichon 2014). Given these small effects and the empirical evidence on the increased supply of nurses during recessions, we can think of the net increase in supply of nurses during a recession as positive.
In theory, wages should fall during a recession as the supply of unemployed nurses increases; however, empirical evidence supporting this theory is mixed. Studies testing this theory have been limited by empirical difficulties in identifying the relationship between economic cycles and wages (Antonazzo et al. 2003). Additionally, wage rates may be “sticky,” or slow to respond to changes in the economic cycle. The wages of workers who remain employed may stay the same or even grow during a recession rather than falling with the general decrease in demand for labor. In our study, we do not have data on wage rates and instead focus on the net effect of changes in the supply and demand for direct-care staff on the resulting staffing ratios in nursing homes.
A second area of literature pertinent to our approach is the evidence on health care demand during recessions, as we posit that recessions also affect nursing home staffing through this channel. Because typical users of nursing home care are elderly and not in the labor force, recessions are unlikely to affect demand for nursing home care through changes in wages. However, empirical evidence points to two other mechanisms: asset shocks and the availability of informal care. Surveys of the elderly found that during the Great Recession, spending by the elderly on health care declined on the order of 10 percent (National Research Council 2011) and that the elderly felt substantially worse about their asset position than other segments of the population (Petev and Pistaferri 2012). Similarly, a recent study finds evidence of both increased informal care and decreased purchase of formal care among older adults during the European Great Recession (Costa-Font, Karlsson, and Oien 2015). Thus, evidence supports several mechanisms for declining demand for nursing home care during a recession.
IV. Conceptual Framework
Building on the evidence presented in the prior section, our conceptual framework considers both the supply of nursing by individuals and the demand for staffing by nursing homes, and how supply and demand will change during a recession. We start with labor supply, then discuss labor demand, which derives in part from patient demand for health care services. The conceptual framework leads to testable predictions with more nuance than in the prior literature.
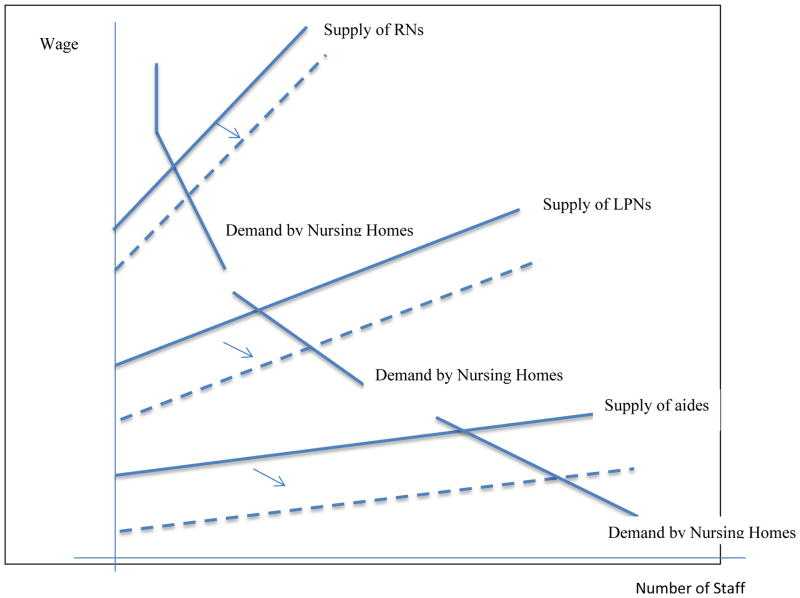
Starting with labor supply, as in the prior literature, we expect the supply of nurses and nurse aides to increase during a recession. Thus, during a recession nursing homes will face a labor supply curve that shifts outward. Ceteris paribus, during a recession nursing homes would be expected to hire more direct-care staff, pay lower wages, or both. Figure 1 presents stylized pictures of labor supply and demand in nursing homes for each type of direct-care worker, with the expected outward shift in labor supply during a recession. Nursing home demand for each type of staff is as described in Section II: Regulations require a minimum number of RNs but, beyond meeting those regulations, RNs are used sparingly because of the high cost. Nursing homes demand LPNs for most other tasks requiring a licensed nurse. Finally, demand is higher for nurse aides, who are the lowest-paid and provide the most direct-care hours, than for licensed nurses. The supply curves are shaped differently for different types of nurse staffing. RNs, having invested more time in training, would be expected to have less elastic supply than LPNs and aides. Therefore, the supply curve for RNs is steeper than for LPNs and nurse aides. Consistent with the prior literature discussed in the previous section, the outward shift in supply during a recession is larger for LPNs and nurse aides than for the higher-paid and more educated RNs.
Figure 1.
Supply and demand of direct-care staff in nursing homes, with supply shift during a recession
On the demand side, however, health care providers face additional consequences of a recession due to shifts in the demand for services. In a recession, demand by nursing home residents will likely decline, especially for those who pay out of pocket (we test this later in the paper). The decline in demand among private-pay residents derives from several mechanisms, consistent with suggestive empirical evidence. First, although the elderly are less affected than working-age adults by shocks to income and employment, they are potentially more affected than other groups by shocks to wealth, lowering demand for private-pay stays. Second, during a recession the opportunity cost of informal care decreases as adult children work fewer hours. Therefore, during a recession more elderly should substitute informal care for formal nursing home care.
The change in demand from Medicaid residents during a recession is more ambiguous than in the private-pay case. The fraction of Medicaid residents may increase because more people will qualify for Medicaid as declining wealth makes it easier to meet Medicaid’s asset tests. However, demand by Medicaid residents could also decrease due to greater availability of informal care, similar to the private-pay case. The direction of the net effect is uncertain.
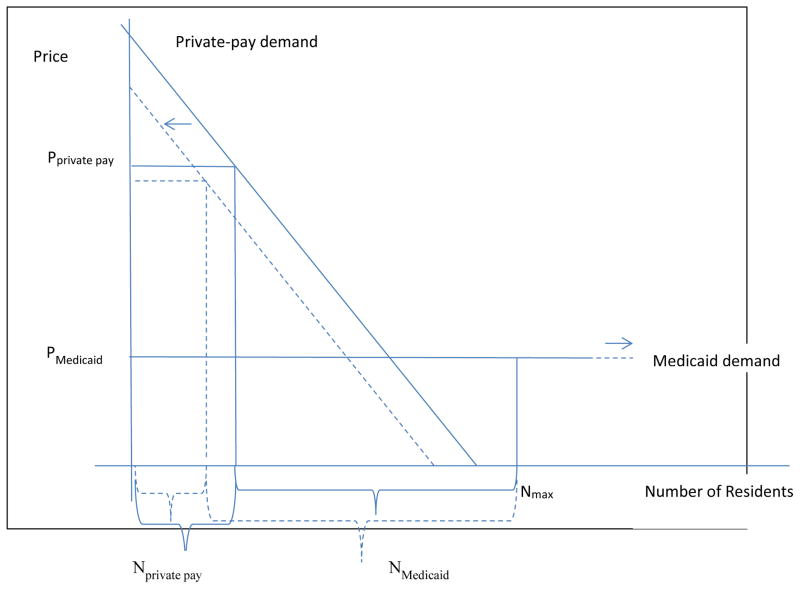
Figure 2 depicts the shift in demand for nursing home care that might be expected in a recession, using a traditional Scanlon (1980) and Nyman (1985) two-payer framework (see also Norton 2000). A nursing home faces a downward-sloping demand curve from private-pay residents but a flat demand curve from Medicaid residents due to administratively set prices by Medicaid. The Medicaid price is lower than the private-pay price. The private-pay price is set to maximize private-pay revenues, and private-pay residents are accepted up to the point where marginal private-pay revenues equal the Medicaid rate. After that, Medicaid residents are accepted. In a recession, for the reasons outlined above, demand from private-pay residents shifts to the left, resulting in fewer private-pay residents and a lower private-pay price. If demand among Medicaid recipients increases or even stays the same, the number of Medicaid residents may increase due to greater availability of beds when private-pay demand declines. Although the ultimate effect on payer mix and the total number of residents is ambiguous, we unambiguously expect lower nursing home revenues during a recession, whether through lower price, more disadvantageous payer mix, or both.
Figure 2.
Demand for nursing home care with shift during a recession
We intentionally ignore Medicare-funded nursing home care in this simple framework, but the addition of Medicare would not affect our predictions. Eligibility for Medicare is universal after age 65, so that eligibility is unrelated to the economy, and demand for Medicare-funded post-acute care is fairly unresponsive to the macro economy (Levine and Buntin 2013). Besides, private-pay and Medicaid residents make up the vast majority of residents.
When the supply curve for nurses and nurse aides shifts out during a recession, nursing homes may be able to hire more staff at potentially lower wages. While the issue of sticky wages creates some uncertainty about whether wages will fall for nurses employed in nursing homes, it does not affect the prediction that the total supply of nurses available to nursing homes should increase during a recession, especially for LPNs and aides. Unfortunately, without data on wage rates, we cannot directly observe whether changes in wage rates is a specific mechanism for changes in the demand for nurses. Nonetheless, we can still comment on the outcomes of interest—that is, net direct-care staffing levels.
We would not expect a uniform increase in all types of staff or in all types of nursing homes. Because private-pay demand is likely to decrease in a recession, lowering the fraction of residents in a typical nursing home who can be charged a market price, the fraction of residents whose demand is sensitive to changes in quality decreases and the overall elasticity of demand for quality could change (Nyman 1985; Grabowksi 2001). This means that nursing homes can shift resources from RNs to lower-cost LPNs and aides without resulting in further risk to demand. At the same time, the shift to lower-cost staff is consistent with the expected greater availability of lower-cost LPNs and nurse aides during a recession. Thus, in addition to an increase in staffing, our framework leads us to expect a shift from RNs to lower-cost staffing in a recession.
Beyond these overall hypotheses, our framework also leads us to expect heterogeneity by nursing home type. First, the overall expected shift in staffing composition does not apply to small nursing homes, which face binding regulatory constraints on the minimum number of RNs. Small nursing homes will typically be at the minimum threshold for RNs and therefore have no ability to substitute away from RNs to LPNs and aides. Therefore we expect a larger response from larger nursing homes, specifically those with more than 60 beds. Second, similarly, we expect that nursing homes with a high staffing ratio to have more flexibility, in terms of not being near regulatory minimums. Therefore, nursing homes with high staffing ratios should be more responsive to changes in the economy than nursing homes with low staffing ratios. Third, the mechanisms we have discussed all relate to profit maximization given changes in the supply of the most costly input to nursing home care. For-profit nursing homes should be more responsive to these financial changes than non-profit nursing homes that may care more about other factors, such as quality of care (Newhouse 1970; Sloan 2001).
In summary, our conceptual framework has four testable hypotheses. First, as unemployment rises, nursing home revenues will decrease. Second, nursing homes will hire more nurses overall. Third, nursing homes will shift away from RNs to LPNs and aides. Fourth, this shift will be larger 1) in the largest nursing homes (those with more than 60 beds) and potentially zero in small nursing homes that are constrained by staffing regulations; 2) in nursing homes with higher staffing; and 3) in for-profit nursing homes.
V. Empirical Strategy
We use a longitudinal nursing home fixed-effects strategy to examine how the local unemployment rate affects direct-care staffing levels and net revenue in nursing homes, using variation in the local unemployment rate across counties and over time to identify the effect. To analyze the effect of the unemployment rate on direct-care staffing we estimate the following reduced-form ordinary least squares regression:
| (1) |
where our outcome of interest is the number of staff hours per resident day (Staffjmt) for nursing home j, located in county m, in year t. We control for time fixed effects τt and nursing home fixed effects γj. In some models we stratify by nursing home characteristics. The error term is ε. We consider staffing hours separately for RNs, LPNs, and aides, and a facility’s total staff hours across all three staff types. We also consider the ratio of RN hours to total staff hours as an outcome, for a total of five staffing-related outcomes and regressions. Finally, to test our primary demand-driven mechanism for any observed changes in staffing during a recession, we re-estimate equation (1) replacing net revenues for staffing levels as the dependent variable. In all specifications, standard errors are clustered at the facility level.
The Stevens and colleagues (2015) paper finds that an increase in unemployment leads to an increase in nursing home staffing, meaning that β> 0. Following from our conceptual model, we hypothesize a more nuanced view that β will be positive for some, but not all, types of direct-care nursing home staff. We also explore whether there are heterogeneous effects of unemployment rates by facility characteristics. We test whether there are different effects by facility size (number of beds), staffing level, and profit status.
Specifically, our testable hypotheses from the conceptual framework are:
In a model to predict nursing home net revenues, β< 0.
In a model to predict overall nurse staffing in nursing homes, β > 0.
In a model to predict RN staffing in nursing homes, β < 0, but in models to predict LPN and nurse aide staffing, β > 0
When stratified by nursing home size, staffing, and profit status, the results for hypothesis 3 will be larger for nursing homes that are large, have high staffing, and are for-profit.
The facility fixed effects account for any facility time-invariant unobservable (and observable) factors that affect the outcomes of interest. They also subsume county fixed effects. The inclusion of year fixed effects in the above specifications allows us to control for any systematic trends in staffing or revenue that affect all nursing homes. This is a conservative approach, as it controls for secular trends affecting the nursing supply or health care demand but, in doing so, does not allow us to exploit the large increase in unemployment during the 2008/9 recession. Thus, identification relies on the extent to which trends over time in unemployment vary from county to county, and the corresponding within-facility variation in our outcomes. We test the robustness of this specification by replacing year fixed effects with county-specific trends and, in a national sample, state-specific trends and state-time dummies. In a final robustness check, we weight each regression by the bed size of each nursing home to assess whether under weighting large facilities in facility-level regression affects the results.
VI. Data
This study uses secondary data sets from multiple sources. For the main analysis, we obtain data on staffing and organizational characteristics in California nursing homes from the annual data files from California’s Office of Statewide Health Planning and Development (OSHPD). We collect county-level unemployment rates from the Area Health Resources File. We restrict our main analysis to California nursing homes due to concerns of biased over-reporting among nursing homes nationally in the Centers for Medicare & Medicaid Services’ (CMS) Online Survery, Certification and Reporting (OSCAR) database. OSHPD data is rigorously audited by the state of California. In our comparisons with OSCAR, nursing home-year level staffing estimates are substantially lower in OSHPD (tables of comparisons available upon request) and our estimates of staffing levels from OSHPD are consistent with prior work (Kim et al. 2009). We use OSCAR data to conduct a sensitivity analysis of our main findings in a national sample of nursing homes.
A. STUDY SAMPLE
Our sample of California nursing homes comprises non-governmental skilled or intermediate care nursing homes from 2005–12. The California minimum nurse staffing regulations were implemented before our study period begins. The initial sample includes 9,081 unique observations from 1,172 nursing homes. We exclude nursing homes that are neither skilled nursing nor intermediate care (n = 113). We also exclude nursing homes that are less likely to make staffing decisions independent of the entity that owned them: hospital-owned (n = 8) and government-owned nursing homes (n = 2). To eliminate outliers that are most likely due to data errors, we also exclude nursing homes with more than 12 total nurse hours per patient day (n = 3), and those with no reported RNs in nursing homes greater than 60 beds (n = 2) (Park and Stearns 2009). The final sample of California nursing homes includes 8,086 unique observations from 1,044 nursing homes from 2005–12.
For the sensitivity analyses, we created a national sample of nursing homes using OSCAR data and followed the same conventions used to create the sample of California nursing homes. The final sample of national nursing homes includes 95,068 unique observations from 7,637 nursing homes from 2005–12.
B. DEPENDENT VARIABLES
We examine two sets of outcome measures — facilities’ direct-care staffing levels and revenues (see Table 1). Facility direct-care staffing is measured in minutes per resident day (PRD), and categorized by the types of staff: RNs, LPNs, aides, total direct-care staff (the sum of RN, LPN, and aide hours), and skill mix (the ratio of RN hours to total direct-care staff hours). Our measure of net revenues is a facility’s total net health care revenue (the sum of the net routine services revenue, net ancillary services revenue, and other operating revenue from providing health care services to residents).
Table 1.
Characteristics of California Nursing Homes, 2005–12
| Characteristics | California Nursing Homes, (N = 1,044) |
|---|---|
| Dependent variables | |
| Mean Total Nurse Minutes PRD, [std. dev.] | 214.1 [28.7] |
| Mean RN Minutes PRD, [std. dev.] | 20.0 [11.7] |
| Mean LPN Minutes PRD, [std. dev.] | 45.6 [12.9] |
| Mean Aides Minutes PRD, [std. dev.] | 148.5 [19.9] |
| Mean RN/Total Minutes PRD, [std. dev.] | 0.09 [0.05] |
| Other facility characteristics | |
| Mean Number of Beds, [std. dev.] | 95.02 [47.56] |
| Percentage Small Size, (n) | 30.08 (314) |
| Percentage Large Size, (n) | 69.92 (730) |
| Percentage Low Staffing, (n) | 66.19 (691) |
| Percentage High Staffing, (n) | 33.81 (353) |
| Percentage For-Profit, (n) | 86.59 (904) |
| Percentage Non-Profit, (n) | 13.41 (140) |
| Mean Net Revenue [std. dev.] | 6,898.48 [3,789.17] |
PRD (per resident day)
Small size is defined by nursing homes with <=60 beds
Large size is defined by nursing homes with >60 beds
Low staffing is defined by a mean total nurse staffing less than or equal to the mean of total nurse staffing across all nursing homes; Mean total staffing within low staffing nursing homes is 200.4.
High staffing is defined by a mean total nurse staffing greater than the mean of total nurse staffing across all nursing homes; Mean total staffing within high staffing nursing homes is 240.7..
Mean net revenue reported in thousands of dollars.
C. UNEMPLOYMENT VARIABLE
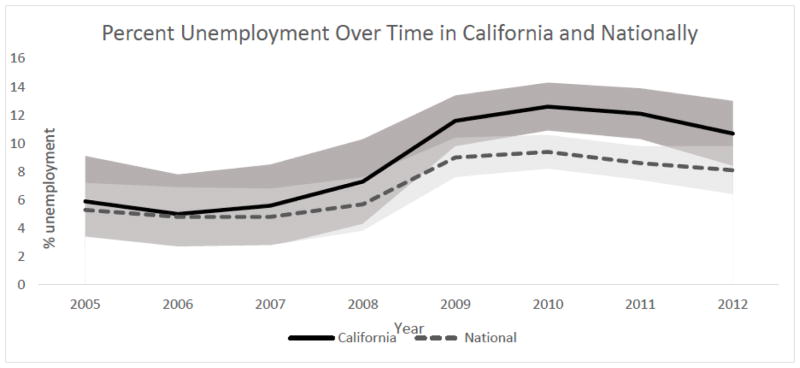
The explanatory variable of interest is the county-level unemployment rate. Unemployment rates are measured annually using data obtained from the Area Health Resources File. In each study year, the unemployment rate is reported among individuals 16 years and older. This definition has been widely used in the health services literature (Maeda et al. 2014). The average county-level unemployment rate in California during the study period was 8.9 percent, and ranged from 2.2 percent to 29.9 percent over the study period (see Figure 3). The average national county-level unemployment rate was 7.0 percent, and ranged from 1.7 percent to 29.7 percent. The typical within-county fluctuation across the eight years was 19.8 percent in California and 16.1 percent nationally. We rely on this variation within county over time to identify the effect of economic booms and busts on the outcomes. The unemployment rate thus serves as a proxy for the effects of these macroeconomic trends, where the mechanism of effect may be unemployment itself or, for example, wealth shocks to the elderly that affect spending on nursing home care. We note that nursing homes in each county in California employ at most about 2 percent of employed individuals in the county, so there is no concern of monopsony behavior biasing our estimates.
Figure 3.
Percent unemployment over time in California and nationally
Note. Mean and standard deviation of county-level percent unemployment in California and nationally.
D. OTHER VARIABLES
To test the fourth hypothesis, we stratified the regression models by the following facility characteristics: size, total nurse staffing level, and profit status (see Table 1). We classified facilities into two groups according to their size defined by the number of beds: small (<=60 beds) and large (>60 beds). The threshold of 60 beds is based on thresholds used in both federal and California state staffing regulations. Specifically, all nursing homes are required to have one RN serving as the full-time Director of Nursing; however, if nursing homes have 60 beds or fewer, the Director of Nursing may also serve as the charge nurse. Otherwise, the positions must be performed by separate individuals (Harrington 2010). Therefore, there is a natural cutoff of 60 beds based on both federal and state policy in terms of staffing regulations. Similarly, we classified direct-care staffing levels into two groups defined as: low (mean total staffing in all nursing homes) and high (> mean total staffing in all nursing homes). Profit status was either for-profit or nonprofit.
VII. RESULTS
For California nursing homes, an increase in unemployment led to an increase in the staffing level of LPNs, a decrease in RNs, and no change in aides or total direct-care staffing levels (see the first column of Table 2 for unstratified results). A one-percentage point increase in the unemployment rate was associated with a decrease in RN minutes per resident day (PRD) of 0.57 and an increase in LPN minutes PRD of 0.77. In relative terms, this translates into a 2.8 percent decline in RN staffing and a 1.7 percent increase in LPN staffing. There was no statistically significant effect of the unemployment rate on the ratio of RN to total hours.
Table 2.
Effect of a 1%-point change in unemployment on nurse staffing minutes per resident day in California nursing homes, 2005–12
| California nursing homes | Stratified by Number of Beds | Stratified by Staffing | Stratified by Profit Status | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Small | Large | Low staffing | High staffing | For-Profit | Non-Profit | ||
|
| |||||||
| RNs | −0.566c | −0.290 | −0.728b | 0.0712 | −1.235b | −0.460 | −0.431 |
| (0.292) | (0.497) | (0.362) | (0.270) | (0.601) | (0.290) | (0.664) | |
|
| |||||||
| LPNs | 0.770a | 0.785 | 0.814a | 0.450b | 1.508a | 0.905a | 0.758 |
| (0.266) | (0.550) | (0.285) | (0.250) | (0.534) | (0.263) | (0.897) | |
|
| |||||||
| Aides | −0.523 | −0.846 | −0.203 | −0.265 | −0.504 | −0.278 | −0.682 |
| (0.496) | (1.202) | (0.428) | (0.314) | (1.147) | (0.389) | (2.118) | |
|
| |||||||
| Total | −0.318 | −0.351 | −0.118 | 0.256 | −0.232 | 0.167 | −0.356 |
| (0.678) | (1.467) | (0.690) | (0.350) | (1.586) | (0.543) | (2.652) | |
|
| |||||||
| RN/Total | −0.001 | 0.0003 | −0.002 | 0.001 | −0.004c | −0.001 | 0.0002 |
| (0.001) | (0.002) | (0.001) | (0.001) | (0.002) | (0.001) | (0.003) | |
|
| |||||||
| No. nursing homes | 1,044 | 314 | 730 | 691 | 353 | 904 | 140 |
|
| |||||||
| No. observations | 8,086 | 2,388 | 5,698 | 5,379 | 2,707 | 7,047 | 1,039 |
All of the models include year and nursing home fixed effects. Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
When stratifying by nursing home characteristics, we also find results that are generally consistent with the predictions from the conceptual framework (see second through seventh columns of Table 2). Our hypothesis was that any effect on staffing would be greater in nursing homes with more beds, and we found exactly that. The coefficients on RNs and LPNs were larger in absolute magnitude for larger nursing homes than for small nursing homes and statistically significant at conventional levels. Similarly, the coefficients on nursing homes with high staffing ratios were also much larger in absolute magnitude than for low-staffing nursing homes and statistically significant. In fact, the magnitudes were roughly twice as large for high-staffing nursing homes as for the overall effect. However, the effect on LPNs was statistically significant for low-staffing nursing homes, but only one-third as large in magnitude. Combined, these results imply that the effect of unemployment on nurse staffing is driven predominantly by nursing homes with many beds or with high staffing ratios, that is, those that have more flexibility in adjusting their staffing. In addition, there seems to be approximately a one-for-one tradeoff between RNs and LPNs, with more LPNs when unemployment rises. Finally, the results for for-profit nursing homes are also consistent with the conceptual framework, with for-profit nursing homes significantly increasing LPN staffing during recessions, and with a magnitude larger than non-profit nursing homes. In sum, the empirical results are in accord with the hypotheses generated from the conceptual framework.
Consistent with the hypothesized effect of recessions on demand for nursing home care, we also estimate declines in net revenue among California nursing homes during recessions (see Table 3). We find that a one-percentage point increase in unemployment was associated with a decrease in net revenue of over $114,000, a relative decline of 1.7%. Similar to the results of recession on staffing, we also find that an increase in unemployment is associated with a larger decline in revenue for large nursing homes, nursing homes with low staffing, and for-profit nursing homes.
Table 3.
Effect of a 1%-point change in unemployment on total net revenue in California nursing homes, 2005–12
| California nursing homes | Stratified by Number of Beds | Stratified by Staffing | Stratified by Profit Status | ||||
|---|---|---|---|---|---|---|---|
| Small | Large | Low staffing | High staffing | For-Profit | Non-Profit | ||
| Nursing Homes | −114.96a | 32.89 | −235.18a | −195.41a | 42.28 | −169.46a | 41.41 |
| (39.85) | (41.80) | (50.37) | (50.78) | (62.25) | (45.44) | (74.21) | |
Total net revenue reported in thousands of dollars.
All of the models include year and facility fixed effects. Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
Finally, because prior estimates of the effect of changes in unemployment rates on nurse and aide staffing levels in nursing homes have been positive (Stevens et al. 2015), we estimate a number of alternative specifications to try to recreate prior results (see Table 4) in a national sample of nursing homes using the OSCAR database. To do so, we focus on the two types of nurse staffing examined by Stevens (nurses, or the combination of RNs and LPNs, and aides) as well as RNs and LPNs seperately. In various specifications we add a set of control variables (population demographics and number of nursing home beds) plus alternative controls for time (state-specific time trends, state-year dummies, and county-specific time trends) with and without taking the log of the dependent variable. In these specifications our estimates remain close to zero and insignificant.
Table 4.
Alternative Specifications of the Effect of a 1%-point Change in Unemployment on Nurse Staffing Minutes per Resident Day in National Nursing Homes, 2005–2012
| Alternative specifications for national nursing homes | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| RNs | −0.142b | −0.002 | −0.113 | <0.0001 | −0.082 | −0.0008 |
| (0.070) | (0.002) | (0.087) | (0.002) | (0.066) | (0.0016) | |
|
| ||||||
| LPNs | 0.109 | 0.003b | 0.138 | 0.004 | 0.013 | −0.001 |
| (0.082) | (0.002) | (0.106) | (0.002) | (0.079) | (0.002) | |
|
| ||||||
| Aides | −0.082 | −0.0003 | −0.266 | −0.001 | 0.026 | −0.0003 |
| (0.154) | (0.001) | (0.199) | (0.002) | (0.148) | (0.001) | |
|
| ||||||
| RNs + LPNs | −0.033 | −0.0001 | 0.026 | 0.001 | −0.069 | −0.001 |
| (0.109) | (0.001) | (0.139) | (0.002) | (0.105) | (0.001) | |
|
| ||||||
| Demographic controls | X | X | X | X | X | X |
|
| ||||||
| Total number of beds | X | X | X | X | X | X |
|
| ||||||
| Logged dependent variable | X | X | X | |||
|
| ||||||
| State-specific trends | X | X | ||||
|
| ||||||
| State-year dummies | X | X | ||||
|
| ||||||
| County-specific trends | X | X | ||||
Demographic controls include fraction of the population who are less than 5 years old, 5 to 17 years old, 20 to 29 years old, greater than 65 years old, high school dropouts, with some college, college graduates, black, and Hispanic.
All of the models include nursing home fixed effects.
Models that do not control for time trends include year fixed effects.
Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
A. SENSITIVIY ANALYSES
We perform a number of tests of the robustness of our results. First, we weight each regression by the bed size of each California nursing home to assess whether underweighting large facilities in facility-level regression affects the results (see Appendix Table A1). Results from this specification are qualitatively similar to the main results. Second, we re-estimate the relationship between unemployment in all nursing homes nationally, using OSCAR data (see Appendix Table A2). We find similar results to our California results among the total sample, large nursing homes, nursing homes with low staffing levels, and for-profit nursing homes, though the magnitude and statistical significance differ somewhat. This gives us more confidence that our results from California generalize to the entire country, despite concerns about the national data. Finally, we re-estimate the main regressions using alterative controls for time (see Appendix Table A3). We find similar results for California nursing homes, with estimates in the same direction and most not statistically significant. In the national sample of nursing homes, the effect of unemployment on RN staffing becomes negative and marginally significant with state-specific time trends, a consistent result with the California sample.
VIII. Conclusions
The macro economy has a strong influence on nurse staffing in nursing homes. We find that when the unemployment rate increases, nursing homes substitute LPNs for RNs. Furthermore, the results are stronger in both magnitude and statistical significance for nursing homes that are larger, have a higher staffing ratio, and are for-profit. However, the overall staffing level is not affected by the unemployment rate, nor is the number of nurses aides. Our empirical results are consistent with our conceptual framework that incorporates both demand and supply-side shifts during a recession.
Our results also identify a plausible economic mechanism for these changes in nurse staffing. During recessions, nursing home revenues decline. To re-optimize staffing under reduced revenues, nursing homes shift to less expensive nurses, but this is only possible for nursing homes large enough to be above minimum staffing levels required by regulations.
We find a different, more complex pattern than the one reported by Stevens and colleagues (2015). Unlike them, we find no significant increase in total employment in nursing homes when the unemployment rate rises. A key difference might explain why our results are not the same—we measure staffing as a ratio of nursing time (e.g., minutes) per resident-day whereas Stevens measures staffing as the number of nurses. Stevens’ approach could overstate true employment levels particularly if there is an increase in the use of part-time workers during a recession.
Our findings should be viewed with respect to several limitations. First, to control for secular trends that may be collinear with recession, our primary specification does not capitalize fully on the increase in unemployment during the recession starting in 2008, the most dramatic change during our study period. Rather, our identification depends on variation in county-specific changes in unemployment, as some counties were affected more than others. However, alternative specifcations that do not include time fixed effects are consistent with our main specification. Second, our data on staffing allows us only to examine staffing type and staffing ratios, not the quality or tenure of staff within type. Thus, if facilities shift from highly experienced RNs to less experienced RNs at lower wages, our analysis will not be able to detect it. Third, although we would ideally control for nurses’ marital status, the data do not have this information, which would in principle allow for a direct test of the added worker effect. Furthermore, Auerbach, Buerhaus, and Staiger (2015) found that RNs with an associate degree are increasingly employed in long-term care, while RNs with a bachelors degree are increasingly employed in hospitals. Finally, because we do not observe private-pay prices, we focus on total revenues and are unable to parse out the exact mechanisms behind declining revenues in a recession.
Nonetheless, our findings have several important implications. First, they show that it is important to consider changes in demand for health care services when assessing the effect of macroeconomic cycles on health care staffing. In the presence of changes in patient demand, the net effect of a shift in nursing supply becomes theoretically ambiguous, and we show that revenues are affected by economic booms and busts. Second, many nursing homes respond to changes in the macroeconomy by adjusting their mix of RNs and LPNs, but those that are larger, have higher staffing ratios, and for-profit are the most responsive. Regulations and administratively set payment rates for nursing home care should potentially consider the state of the economy and the nurse labor market if minimum RN staffing is to be required. At the same time, policymakers may want to take a closer look at the scope of practice between RNs and LPNs in nursing homes to assess the extent of substitutability desired or allowed in order for nursing homes to meet minimum quality standards. Finally, we show evidence that the market for nurses in nursing homes is somewhat sensitive to the macro economy. Whether or not these changes in staffing affect morbidity and mortality is a question that should be pursued further.
Acknowledgments
The authors thank participants at the International Long-term Care Policy Network conference in London for comments. The authors declare that they have no relevant or material financial interests that relate to the research described in this paper.
Funding Information: Karen Lasater received support from the National Institute of Nursing Research (T32-NR0714). Rachel Werner received support from the National Institute on Aging (K24-AG047908). The funders played no role in the study design, analysis, writing, or the decision to submit the paper for publication.
APPENDIX
Table A1.
Effect of a 1%-point Change in Unemployment on Nurse Staffing Minutes per Resident Day in California Nursing Homes, Weighted by Bedsize, 2005–2012
| California nursing homes | Stratified by Number of Beds | Stratified by Staffing | Stratified by Profit Status | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Small | Large | Low staffing | High staffing | For-Profit | Non-Profit | ||
|
| |||||||
| RNs | −0.521c | −0.428 | −0.540c | 0.143 | −1.575a | −0.353 | −0.687 |
| (0.272) | (0.514) | (0.311) | (0.253) | (0.589) | (0.265) | (0.746) | |
|
| |||||||
| LPNs | 0.692a | 0.650 | 0.714c | 0.282 | 1.600a | 0.716a | 1.123 |
| (0.252) | (0.583) | (0.278) | (0.250) | (0.526) | (0.261) | (0.939) | |
|
| |||||||
| Aides | −0.326 | −1.061 | −0.121 | −0.375 | −0.033 | −0.147 | −1.289 |
| (0.414) | (1.229) | (0.430) | (0.309) | (1.044) | (0.398) | (1.925) | |
|
| |||||||
| Total | −0.155 | −0.840 | −0.052 | 0.049 | −0.008 | −0.216 | −0.853 |
| (0.613) | (1.541) | (0.666) | (0.380) | (1.594) | (0.588) | (2.505) | |
|
| |||||||
| RN/Total | −0.001 | −0.001 | −0.001 | 0.0012 | −0.005a | −0.001 | −0.002 |
| (0.001) | (0.002) | (0.001) | (0.0012) | (0.002) | (0.001) | (0.003) | |
|
| |||||||
| No. nursing homes | 1,044 | 314 | 730 | 691 | 353 | 904 | 140 |
|
| |||||||
| No. observations | 8,086 | 2,388 | 5,698 | 5,379 | 2,707 | 7,047 | 1,039 |
All of the models include year and nursing home fixed effects. Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
Table A2.
Effect of a 1%-point change in unemployment on nurse staffing minutes per resident day in national nursing homes, 2005–12
| National nursing homes | Stratified by Number of Beds | Stratified by Staffing | Stratified by Profit Status | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Small | Large | Low staffing | High staffing | For-Profit | Non-Profit | ||
|
| |||||||
| RNs | 0.078 | 0.022 | 0.087 | 0.077 | 0.150 | 0.124c | −0.153 |
| (0.057) | (0.131) | (0.063) | (0.049) | (0.130) | (0.067) | (0.105) | |
|
| |||||||
| LPNs | 0.064 | 0.015 | 0.052 | 0.164b | −0.038 | 0.149b | −0.270b |
| (0.063) | (0.162) | (0.067) | (0.067) | (0.127) | (0.074) | (0.122) | |
|
| |||||||
| Aides | −0.161 | −0.205 | −0.130 | −0.352a | 0.075 | −0.190 | −0.007 |
| (0.117) | (0.302) | (0.126) | (0.126) | (0.238) | (0.133) | (0.262) | |
|
| |||||||
| Total | −0.019 | −0.169 | 0.009 | −0.111 | 0.187 | 0.086 | −0.429 |
| (0.155) | (0.394) | (0.166) | (0.151) | (0.337) | (0.175) | (0.346) | |
|
| |||||||
| RN/Total | 0.0003 | 0.001 | 0.0002 | 0.0004c | 0.001 | 0.0003 | −0.0003 |
| (0.0002) | (0.001) | (0.0002) | (0.0002) | (0.0003) | (0.0002) | (0.0004) | |
|
| |||||||
| No. nursing homes | 7,637 | 1,633 | 6,004 | 4,707 | 2,930 | 5,701 | 1,936 |
|
| |||||||
| No. observations | 95,068 | 18,254 | 76,814 | 62,323 | 32,745 | 71,365 | 23,703 |
All of the models include year and nursing home fixed effects. Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
Table A3.
Effect of a 1%-point change in unemployment on nurse staffing minutes per resident day, using alternative specifications to control for time, 2005–12
| County-specific trends | State-specific trends | State-time dummies | ||
|---|---|---|---|---|
|
| ||||
| California Nursing Homes | National Nursing Homes | National Nursing Homes | National Nursing Homes | |
|
| ||||
| RNs | −0.284 | −0.077 | −0.129c | −0.125 |
| (0.313) | (0.064) | (0.069) | (0.085) | |
|
| ||||
| LPNs | −0.269 | −0.014 | 0.066 | 0.075 |
| (0.377) | (0.077) | (0.081) | (0.104) | |
|
| ||||
| Aides | −1.043 | 0.021 | −0.079 | −0.270 |
| (0.661) | (0.145) | (0.151) | (0.194) | |
|
| ||||
| Total | −1.596c | −0.071 | −0.142 | −0.320 |
| (0.815) | (0.189) | (0.200) | (0.259) | |
|
| ||||
| RN/Total | 0.0003 | −0.0003 | −0.0004 | <0.0001 |
| (0.001) | (0.0002) | (0.0002) | (0.0003) | |
|
| ||||
| No. nursing homes | 1,044 | 7,637 | 7,637 | 7,637 |
|
| ||||
| No. observations | 8,086 | 95,068 | 95,068 | 95,068 |
All of the models include nursing home fixed effects. Robust standard errors in parentheses.
p < 0.01,
p < 0.05,
p < 0.10.
Footnotes
JEL CLASSIFICATION: E32, I11, J44, L84
Contributor Information
R. Tamara Konetzka, Department of Public Health Sciences, University of Chicago.
Karen B. Lasater, Center for Health Outcomes and Policy Research, School of Nursing, University of Pennsylvania
Edward C. Norton, Department of Health Management and Policy and Department of Economics, University of Michigan, and NBER
Rachel M. Werner, Division of General Internal Medicine and Leonard Davis Institute of Health Economics, University of Pennsylvania
References
- Antonazzo Emanuela, Scott Anthony, Skatun Diane, Elliott Robert F. The Labour Market for Nursing: a Review of the Labour Supply Literature. Health Economics. 2003;12(6):465–78. doi: 10.1002/hec.737. [DOI] [PubMed] [Google Scholar]
- Assembly Bill 394. 1999. Cal Bus Prof Code §2725.3; Health Safety Code §1276.4.
- Assisted Living Today. The Role of Nurses in a Nursing Home (blog) [Accessed June 20, 2017];2017 http://assistedlivingtoday.com/blog/the-role-of-nurses-in-a-nursing-home/
- Auerbach David I, Buerhaus Peter I, Staiger Douglas O. Do Associate Degree Registered Nurses Fare Differently in the Nurse Labor Market Compared to Baccalaureate-Prepared RNs? Nursing Economics. 2015;33(1):8–13. [PubMed] [Google Scholar]
- Backhaus Ramona, Verbeek Hilde, van Rossum Erik, Capezuti Elizabeth, Hamers Jan PH. Nurse Staffing Impact on Quality of Care in Nursing Homes: A Systematic Review of Longitudinal Studies. Journal of the American Medical Directors Association. 2014;15(6):383–393. doi: 10.1016/j.jamda.2013.12.080. [DOI] [PubMed] [Google Scholar]
- Baughman Reagan A, Smith Kristin E. Labor Mobility of the Direct Care Workforce: Implications for the Provision of Long-Term Care. Health Economics. 2012;21(12):1402–15. doi: 10.1002/hec.1798. [DOI] [PubMed] [Google Scholar]
- Böckerman Petri, Johansson Edvard, Helakorpi Satu, Prättälä Ritva, Vartiainen Erkki, Uutela Antti. Does a Slump Really Make You Thinner? Finnish Micro-Level Evidence 1978–2002. Health Economics Letters. 2015;16:103–107. doi: 10.1002/hec.1156. [DOI] [PubMed] [Google Scholar]
- Buerhaus Peter I, Auerbach David I, Staiger Douglas O. The Rapid Growth of Graduates from Associate, Baccalaureate, and Graduate Programs in Nursing. Nursing Economics. 2014;32(6):290–95. 311. [PubMed] [Google Scholar]
- Buerhaus Peter I, Auerbach David I, Staiger Douglas O. The Recent Surge in Nurse Employment: Causes and Implications. Health Affairs. 2009;28(4):657–68. doi: 10.1377/hlthaff.28.4.w657. [DOI] [PubMed] [Google Scholar]
- Burger Sarah Green, Cantor Bonnie, Mezey Mathy, Mitty Ethel, Kluger Malvina, Algase Donna, Anderson Kathryn, Beck Cornelia, Mueller Christine, Rader Joanne. Issue Paper. Hartford Institute for Geriatric Nursing, New York University College of Nursing; 2009. [Accessed June 20, 2017]. Nurses Involvement in Nursing Home Culture Change: Overcoming Barriers, Advancing Opportunities. http://www.socialworkers.org/practice/aging/documents/issuePaper0609.pdf. [Google Scholar]
- Castle Nicholas G. Nursing Home Caregiver Staffing Levels and Quality of Care a Literature Review. Journal of Applied Gerontology. 2008;27(4):375–405. [Google Scholar]
- Cawley John, Grabowski David C, Hirth Richard A. Factor Substitution in Nursing Homes. Journal of Health Economics. 2006;25(2):234–247. doi: 10.1016/j.jhealeco.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Cohen Joel W, Spector William D. The Effect of Medicaid Reimbursement on Quality of Care in Nursing Homes. Journal of Health Economics. 1996;15(1):23–48. doi: 10.1016/0167-6296(95)00030-5. [DOI] [PubMed] [Google Scholar]
- Costa-Font Joan, Karlsson Martin, Oien Henning. CEP Discussion Paper No. 1360. Centre for Economic Performance, London School of Economics and Political Science; 2015. [Accessed June 17, 2017]. Informal Care and the Great Recession. http://cep.lse.ac.uk/pubs/download/dp1360.pdf. [Google Scholar]
- Das Anup, Norton Edward C, Miller David C, Ryan Andrew M, Birkmeyer John D, Chen Lena M. Adding a Spending Metric to Medicare’s Value-Based Purchasing Program Rewarded Low-Quality Hospitals. Health Affairs. 2016;35(5):898–906. doi: 10.1377/hlthaff.2015.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehejia Rajeev, Lleras-Muney Adriana. Booms, Busts, and Babies’ Health. Quarterly Journal of Economics. 2004;119(3):1091–1130. [Google Scholar]
- Dellefield Mary Ellen, Castle Nickolas G, McGilton Katherine S, Spilsbury Karen. The Relationship between Registered Nurses and Nursing Home Quality: An Integrative Review (2008–2014) Nursing Economics. 2015;33(2):95–108. 116. [PubMed] [Google Scholar]
- Elsby Michael WL, Shin Donggyun, Solon Gary. Wage Adjustments in the Great Recession and Other Downturns: Evidence from the United States and Great Britain. Journal of Labor Economics. 2016;34(1):S249–91. [Google Scholar]
- Figura Andrew, Barnichon Regis. The Effects of Unemployment Benefits on Unemployment and Labor Force Participation: Evidence From 35 Years of Benefits Extensions. [Accessed June 20, 2017];2014 https://www.federalreserve.gov/pubs/feds/2014/201465/201465pap.pdf.
- Grabowski David C. Medicaid Reimbursement and the Quality of Nursing Home Care. Journal of Health Economics. 2001;20(4):549–69. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- Hanel Barbara, Kalb Guyonne, Scott Anthony. Nurses’ Labour Supply Elasticities: The Importance of Accounting for Extensive Margins. Journal of Health Economics. 2014;33:94–112. doi: 10.1016/j.jhealeco.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Harrington Charlene. [Accessed June 20, 2017];Nursing Home Staffing Standards in State Statutes and Regulations. 2010 http://ltcombudsman.org/uploads/files/support/Harrington-state-staffing-table-2010_%281%29.pdf.
- Horn Susan D, Buerhaus Peter, Bergstrom Nancy, Smout Randall J. RN Staffing Time and Outcomes of Long-Stay Nursing Home Residents. American Journal of Nursing. 2005;105(11):58–70. doi: 10.1097/00000446-200511000-00028. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Johnson & Johnson. [Accessed June 20, 2017];The Campaign for Nursing’s Future. 2017 https://www.discovernursing.com/
- Kaiser Family Foundation. [Accessed June 20, 2017];Nursing Facilities, Staffing, Residents and Facility Deficiencies, 2009 Through 2014. 2015 http://kff.org/medicaid/report/nursing-facilities-staffing-residents-and-facility-deficiencies-2009-through-2014/
- Kim Hongsoo, Kovner Christine, Harrington Charlene, Greene William, Mezey Mathy. A Panel Data Analysis of the Relationships of Nursing Home Staffing Levels and Standards to Regulatory Deficiencies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64B(2):269–78. doi: 10.1093/geronb/gbn019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka R Tamara, Stearns Sally C, Park Jeongyoung. The Staffing-Outcomes Relationship in Nursing Homes. Health Services Research. 2008;43(3):1025–42. doi: 10.1111/j.1475-6773.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka R Tamara, Perraillon Marcelo Coca. Use of Nursing Home Compare Website Appears Limited by Lack of Awareness and Initial Mistrust of the Data. Health Affairs. 2016;35(4):706–13. doi: 10.1377/hlthaff.2015.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krolikowski Pawel. Job Ladders and Earnings of Displaced Workers. American Economic Journal: Macroeconomics. 2017;9(2):1–31. [Google Scholar]
- Levine Michael, Buntin Melinda. Congressional Budget Office Working Paper 2013-06. Washington, D.C: 2013. [Accessed June 20, 2017]. Why Has Growth in Spending for Fee-For-Service Medicare Slowed? https://www.cbo.gov/sites/default/files/44513_MedicareSpendingGrowth-8-22.pdf. [Google Scholar]
- Maeda Jared Lane K, Henke Rachel Mosher, Marder William D, Karaca Zeynal, Friedman Bernard S, Wong Herbert S. Association Between the Unemployment Rate and Inpatient Cost Per Discharge by Payer in the United States, 2005–2010. BMC Health Services Research. 2014;14:378. doi: 10.1186/1472-6963-14-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney Tim. Unobserved Variables and the Elusive Added Worker Effect. Economica. 1991;58(230):173–187. [Google Scholar]
- National Research Council. Consumption, Savings, Pensions, and Wealth. In: Majmundar M, editor. Assessing the Impact of Severe Economic Recession on the Elderly:Summary of a Workshop. Washington, DC: The National Academies Press; 2011. Steering Committee on the Challenges of Assessing the Impact of Severe Economic Recession on the Elderly. Committee on Population, Division of Behavioral and Social Sciences and Education. [PubMed] [Google Scholar]
- Newhouse Joseph P. Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital. American Economic Review. 1970;60(1):64–74. [Google Scholar]
- Nicholson Sean, Propper Carol. Medical Workforce. In: Pauly Mark V, McGuire Thomas G, Barros Pedro P., editors. Handbook of Health Economics. Vol. 2. New York, NY: Elsevier Science B.V; 2012. pp. 873–925. [Google Scholar]
- Norton Edward C. Long-Term Care. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. IB. New York, NY: Elsevier Science B.V; 2000. pp. 956–994. [Google Scholar]
- Nyman John A. Prospective and Cost-Plus Medicaid Reimbursement, Excess Medicaid Demand, and the Quality of Nursing Home Care. Journal of Health Economics. 1985;4(3):237–259. doi: 10.1016/0167-6296(85)90031-1. [DOI] [PubMed] [Google Scholar]
- Park Jeongyoung, Stearns Sally C. Effects of State Minimum Staffing Standards on Nursing Home Staffing and Quality of Care. Health Services Research. 2009;44(1):56–78. doi: 10.1111/j.1475-6773.2008.00906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petev Ivaylo D, Pistaferri Luigi. A Great Recession Brief. Standford, CA: Stanford Center on Poverty and Inequality; 2012. [Accessed June 20, 2017]. Consumption in the Great Recession. https://web.stanford.edu/group/recessiontrends/cgi-bin/web/sites/all/themes/barron/pdf/Consumption_fact_sheet.pdf. [Google Scholar]
- Ruhm Christopher J. Are Recessions Good for Your Health? Quarterly Journal of Economics. 2000;115(2):617–650. [Google Scholar]
- Ruhm Christopher J. Good Times Make You Sick. Journal of Health Economics. 2003;22(4):637–658. doi: 10.1016/S0167-6296(03)00041-9. [DOI] [PubMed] [Google Scholar]
- Ruhm Christopher J. Recessions, Healthy No More? Journal of Health Economics. 2015;42:17–28. doi: 10.1016/j.jhealeco.2015.03.004. [DOI] [PubMed] [Google Scholar]
- Scanlon WJ. A Theory of the Nursing Home Market. Inquiry. 1980;17:25–41. [PubMed] [Google Scholar]
- Sloan Frank A. Hospital Ownership and Cost and Quality of Care: Is There a Dime’s Worth of Difference? Journal of Health Economics. 2001;20(1):1–21. doi: 10.1016/s0167-6296(00)00066-7. [DOI] [PubMed] [Google Scholar]
- Spilsbury Karen, Hewitt Catherine, Stirk Lisa, Bowman Clive. The Relationship Between Nurse Staffing and Quality of Care in Nursing Homes: a Systematic Review. International Journal of Nursing Studies. 2011;48(6):732–50. doi: 10.1016/j.ijnurstu.2011.02.014. [DOI] [PubMed] [Google Scholar]
- Staiger Douglas O, Auerbach David I, Buerhaus Peter I. Registered Nurse Labor Supply and the Recession—Are We in a Bubble? New England Journal of Medicine. 2012;366:1463–65. doi: 10.1056/NEJMp1200641. [DOI] [PubMed] [Google Scholar]
- Stephens Melvin., Jr Worker Displacement and the Added Worker Effect. Journal of Labor Economics. 2002;20(3):504–37. [Google Scholar]
- Stevens Ann H, Miller Douglas L, Page Marianne E, Filipski Mateusz. The Best of Times, the Worst of Times: Understanding Pro-Cyclical Mortality. American Economic Journal: Economic Policy. 2015;7(4):279–311. doi: 10.1257/pol.20130057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone Robyn I, Wiener Joshua M. Who Will Care for Us? Addressing the Long-Term Care Workforce Crisis. The Urban Institute and the American Association of Homes and Services for the Aging; 2001. [Accessed June 20, 2017]. https://aspe.hhs.gov/system/files/pdf/73111/ltcwf.pdf. [Google Scholar]
- Yoo Byung_Kwang, Kim Minchul, Sasaki Tomoko, Ward Debbie, Spetz Joanne. The Impact of Economic Recession on Registered Nurse Workforce Supply in California. Nursing Economics. 2017;35(1):21–29. [PubMed] [Google Scholar]
- Zhang Xinzhi, Grabowski David C. Nursing Home Staffing and Quality Under the Nursing Home Reform Act. The Gerontologist. 2004;44(1):13–23. doi: 10.1093/geront/44.1.13. [DOI] [PubMed] [Google Scholar]