Abstract
Objectives:
This study assessed the impact of the Integrated Care Program (ICP), a new Medicaid managed care model in Illinois, on health services utilization and costs for adults with behavioral health conditions.
Methods:
Data sources included Medicaid claims, encounter records, and state payment data for 28,127 persons with a behavioral health diagnosis. Difference-in-differences models, in conjunction with propensity score weighting, were used to compare utilization and costs between ICP enrollees and a fee-for-service (FFS) comparison group. The model considered the impact of the SMART Act, which restricted access to care for the comparison group.
Results:
Before the SMART Act, ICP was associated with 2.8 fewer all-cause primary care visits, 34.6 fewer behavioral health-specific outpatient visits, and 2.5 fewer all-cause inpatient admissions per 100 persons per month, and $228 lower total costs per member per month relative to the FFS group. After the SMART Act, ICP enrollees had increased outpatient and dental services utilization without significantly higher costs. The relative increase in utilization was due primarily to decreased utilization in the restricted FFS group after the SMART Act. By the end of the study period, the ICP group had 13.3 more all-cause primary care visits, 1.5 more emergency department visits, and 1.4 more dental visits per 100 persons per month relative to the FFS program.
Conclusions:
A fully-capitated, integrated managed care program has the potential to reduce overall Medicaid costs for people with behavioral health conditions without negative effects on service utilization.
Keywords: Medicaid, Managed care, Behavioral health, Mental Health
INTRODUCTION
State Medicaid programs are increasingly expanding the use of comprehensive risk-based managed care organizations (MCOs) to serve high-need populations, including adults with behavioral health conditions. As of July 2017, 39 states had contracts with comprehensive risk-based MCOs to serve all or part of their Medicaid population. In 23 of the 39 MCO states, at least half of elderly Medicaid beneficiaries and those with disabilities were enrolled in MCOs rather than fee-for-service (FFS) (Gifford et al., 2017). Comprehensive risk-based management of health expenditures has the potential to reduce overall treatment costs (Jones et al., 2006). Adults with behavioral health conditions—encompassing both mental health and substance use disorders— account for half of Medicaid beneficiaries with disabilities and are one of the most medically needy and high cost populations (Kronick, Bella, & Gilmer, 2009). As the reliance on Medicaid managed care (MMC) continues to grow, it is important to examine how this high-need population has fared under MMC.
Previous studies by have examined the general impact of MMC (The Lewin Group, 2009; Marton, Yelowitz, Talbert, 2014; Duggan, Hayford, 2013; Bindman, Chattopadhyay, Osmond, Huen, Bacchetti, 2004), and several have focused on beneficiaries with behavioral health conditions (Hutchinson, Foster, 2003; Callahan, Shepard, Beinecke, Larson, Cavanaugh, 1995; Bianconi, Mahler, McFarland, 2006; Bouchery, Harwood, 2003; Leff, et al., 2005; Masland, Snowden, Wallace, 2007), but the findings have been mixed. While the review from Kronick, Bella, and Gilmer (2009) of MMC programs from the 1990s and early 2000s showed potential for cost savings, an analysis of MMC mandates and state Medicaid expenditures during a similar timeframe reported that shifting from FFS to MMC did not reduce Medicaid spending in most states (Marton, Yelowitz, & Talbert, 2014). A few studies reported negligible differences between MMC and FFS in access and utilization of health services for people with behavioral health conditions (Bianconi, Mahler, McFarland, 2006; Leff, 2005) while an evaluation of the Nebraska’s MMC program showed a significant decline in inpatient mental health treatment (Bouchery, & Harwood, 2003). According to Hutchinson, and Foster (2003) varying programmatic features, beneficiaries’ characteristics, and length of follow-up likely have contributed to the mixed findings.
These early studies have predominantly examined programs that involved behavioral health “carve-out” (Jones, et al., 2006; Hutchinson, Foster, 2003; Callahan, Shepard, Beinecke, Larson, Cavanaugh, 1995; Bianconi, Mahler, McFarland, 2006; Bouchery, Harwood, 2003; Leff, et al., 2005; Masland, Snowden, Wallace, 2007), where behavioral health services are administered and financed separately by specialty providers or managed behavioral health care organizations. Prior to passage of the Affordable Care Act (ACA), behavioral health carve-outs were the dominant arrangement in Medicaid programs (Masland, Snowden, and Wallace, 2007). The belief that lower rates can be negotiated with the creation of specialty provider networks and concerns of adverse selection propelled the popularity of behavioral health carve-outs. However, the focus on clinical integration and payment reforms in ACA has driven more states to move towards comprehensive “carve-in”, or integrated MMC, to finance and administer different types of services within a single managed care plan (Smith, et al., 2016). Yet, there is a dearth of research on the impact of integrated MMC programs for people with behavioral health conditions.
This study assesses the effects of the Illinois Integrated Care Program (ICP) on health services utilization and costs for adults with behavioral health conditions. This study is part of a larger evaluation that examined the impact of ICP across types of disabilities (Heller, et al., 20015). ICP is a fully-capitated, risk-adjusted, and mandatory MMC program for seniors and people with disabilities who do not also qualify for Medicare. ICP involves comprehensive “carve-in” of behavioral health and long-term care. The state rolled out the ICP in May 2011 in a pilot region consisting of 6 suburban counties surrounding Chicago and selected two large, for-profit MCOs to administer the plans during this pilot phase. Medicaid beneficiaries who lived in the pilot region were required to enroll in the ICP. The state contracted with a larger number of MCOs to expand the ICP to most of the state, including the city of Chicago, in the summer of 2014.
Two policy changes affected the evaluation of the ICP program after the its initial rollout in May 2011. In June 2012, Illinois passed the Save Medicaid Access and Resources Together (SMART) Act to reduce the operation cost of Medicaid. The SMART Act lowered reimbursement rates for many providers, eliminated certain optional services such as group psychotherapy and non-emergency adult dental services, and placed utilization controls on some services such as adult podiatry services for non-diabetics. Copays were increased to the federal maximum for prescriptions, non-emergent care in the emergency room, and for visits to Federally Qualified Health Centers. In addition, a program that helped beneficiaries pay for prescriptions was terminated. People enrolled in the ICP were sheltered from most of these changes because the MCOs decided to continue services according to managed care contracts. In March 2013, Illinois renegotiated the capitation rates it paid to the MCOs running the ICP program, resulting in slightly lower capitation rates.
METHODS
Study design
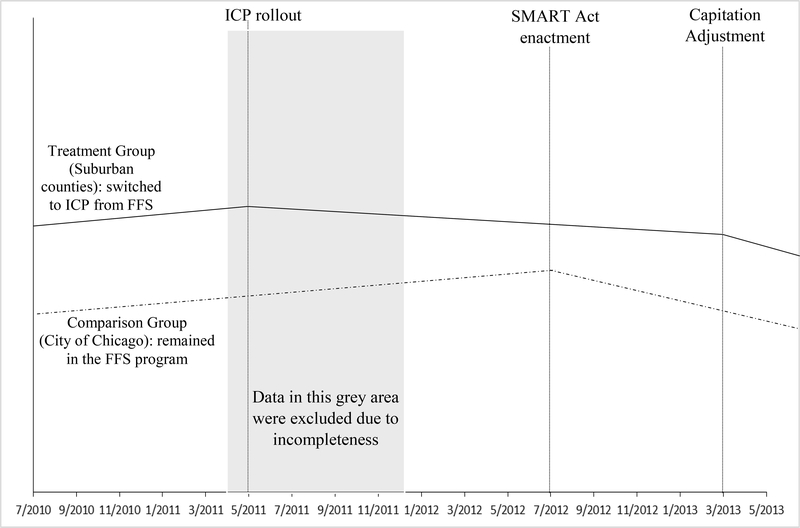
This study leverages a natural experiment by comparing health services utilization and cost outcomes between Medicaid beneficiaries from 6 Chicago suburban counties in the ICP pilot region and a comparison group of ICP eligible Medicaid beneficiaries residing in the city of Chicago prior to the state-wide implementation of ICP. This is equivalent to a non-randomized, waiting list design. Following the intent to treat concept, study population were organized into two groups based on their residence in July 2010. Both groups were enrolled in the FFS Medicaid program from July 2010 through April 2011. In May 2011, the suburban group switched to ICP whereas the Chicago group continued enrollment in the FFS program. The study design considered the influence of the SMART Act and capitation adjustment that went into effect after the ICP rollout (Figure 1).
Figure 1.
Illustration of the study design. Lines are for illustration purposes and do not represent real data. ICP=Integrated Care Program. SMART Act=Save Medicaid Access and Resources Together Act. FFS=Fee-for-service
Data and participants
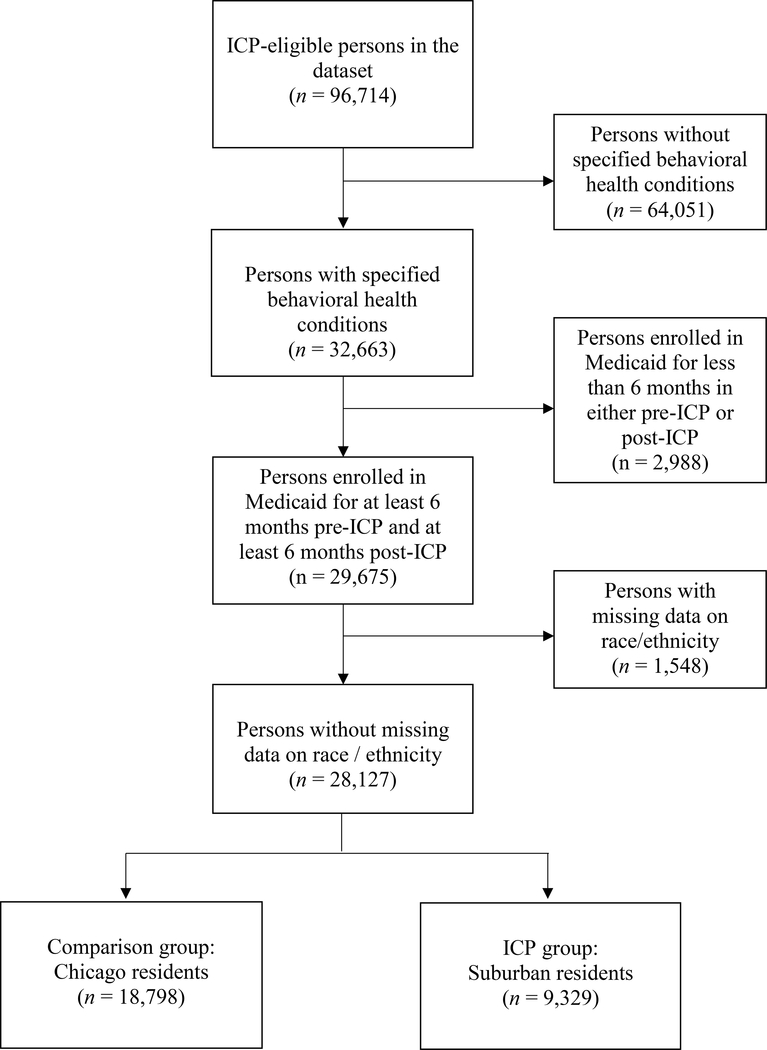
Data sources included Medicaid FFS claims, encounter records from MCOs, and state capitation payment data after a rigorous validation process for the period of July 2010 through December 2013 for ICP eligible Medicaid beneficiaries residing in the city of Chicago and the suburban counties in the ICP pilot region (Heller, et al., 2015). Data from the initial 9 months after the ICP rollout were excluded from our analysis because the transition between plans and data systems made the data incomplete. Medicaid beneficiaries were included in the study sample if they met all of the following criteria: (1) had a diagnosis of a behavioral health condition during the pre-ICP months; (2) enrolled in the Medicaid program 6 months and over during the periods before and after ICP rollout. A minimum of 6-month enrollment was imposed to reduce biases due to coverage lapses and to allow sufficient time to observe changes before and after the intervention; and (3) had complete demographic data. The final study sample consisted of 28,127 unique persons with a diagnosis of a behavioral health condition during the pre-ICP months (see Figure 2 for the sample selection process).
Figure 2.
Sample selection process. ICP=Integrated Care Program.
Behavioral health diagnosis
Identification of disease and diagnoses was based on International Classification of Disease, 9th Edition (ICD-9-CM) codes. Clark, et al. (2009) reported that specification and classification of ICD-9-CM codes were based on the Clinical Classifications Software (CCS) developed as part of the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project, with a modification to distinguish major depressive disorder (296.2x, 296.3x) from other depressive disorders (293.83, 300.4, 311). Appendix A lists the 13 categories of behavioral health diagnoses and associated ICD-9-CM codes. These categories are not mutually exclusive. The study sample included individuals who had at least one claim associated with these 13 categories, either principal or secondary diagnosis, during the pre-ICP months.
Outcome measures
Utilization rate is defined as number of visits per month per 100 persons in each service category. Seven service categories were examined, including all-cause primary care, emergency department, acute inpatient, and dental services, as well as behavioral health-specific outpatient, emergency department, and acute inpatient services. Identification of service categories was based on a combination of Healthcare Common Procedure Coding System (HCPCS) codes, place of service, provider type, and principal diagnosis. All-cause primary care services referred to HCPCS level I codes eligible for Primary Care Incentive Payments in calendar year 2011, a program established by section 5501(a) of the Affordable Care Action (Department of Health & Human Services, Centers for Medicare & Medicaid Services, 2011). Identification of all-cause emergency department and acute inpatient services used Healthcare Effectiveness Data and Information Set (HEDIS) utilization-of-care measures from the National Quality Measures Clearinghouse, with a modification to forgo the application of HEDIS behavioral health exclusion criteria. Identification of dental services used HCPCS level II codes starting with a letter “D”. Identification of the 3 categories of behavioral health-specific services used HEDIS mental health utilization measures (National Committee for Quality Assurance, 2015) (See Appendix B for details).
Expenditures are total FFS and capitated payments made by the state Medicaid agency for each beneficiary per month. Payments covered all services including medications and long-term services and supports. Costs associated with the Developmental Disabilities Waiver services were excluded because these services were carved out of the ICP during the study period.
Data analysis
We used a matched-comparison difference-in-differences (DID) model to assess the effect of the ICP program on measures of health services utilization and cost. The basic DID model compares changes over time in the suburban group with the changes over time in the Chicago comparison group, and attributes the difference in differences to the effect of ICP. We augmented the basic model to allow the effects of ICP to change as the SMART Act and capitation adjustment were implemented during the post-treatment period. Because the suburban and Chicago populations differed substantially during the pre-ICP period, we applied the inverse probability of treatment weighting (IPTW) to mitigate the bias associated with the baseline differences between these two groups. IPTW induced a weighted sample in which the distribution of measured baseline covariates become similar between the Suburban group and the Chicago comparison group. An advantage of IPTW relative to other propensity score methods (matching and stratification) is retention of the entire study sample in the final analysis for optimal power, variability, and representativeness of the study sample.
The first step of IPTW involved estimation of propensity scores via a logistic regression model to predict group assignment (suburban vs city of Chicago). Estimation of propensity score involved the following baseline covariates: demographic characteristics (age, race/ethnicity, and sex), type of Medicaid home and community based services (HCBS) waivers, nursing home resident (yes/no), total months enrolled in Medicaid, behavioral health category (using the 13 categories previously described), physical health conditions (using the 27 conditions from the Elixhauser comorbidity index using ICD-9-CM diagnosis codes from Quan et al. (2005)), average number of monthly visits in each service category, and average monthly expenditures during pre-ICP months. Model specification included various transformations of the covariates with the goal to find a specification that created a Chicago comparison group that resembled the Suburban treatment group. We checked the performance of the matching by comparing the distribution of covariates between the Suburban and weighted Chicago samples using significance testing. After balance checks, we constructed subjects’ weights, equal to the inverse of the probability of receiving the treatment that the subject received (Austin, & Stuart, 2015).
After baseline covariates were balanced between the treated and comparison subjects in the weighted sample (Table 1), ICP effect was estimated in a weighted regression model. Clustered robust standard errors were estimated to account for correlation within subjects. The model setup allowed the effects of ICP to change with the implementation of the SMART Act and capitation adjustments.
Table 1.
Baseline sample characteristics
| Before weighting | After weightinga | |||||||
|---|---|---|---|---|---|---|---|---|
| All(N=28,127) | Suburban ICP group(N=9,329) | Chicago comparison group(N=18,798) | Chicago comparison group(N=18,798) | |||||
| Baseline covariates | N | % | N | % | N | % | p | % |
| Sex | .005 | |||||||
| Male | 14,102 | 50.1 | 4,567 | 49.0 | 9,535 | 50.7 | 48.1 | |
| Female | 14,025 | 49.9 | 4,762 | 51.0 | 9,263 | 49.3 | 50.2 | |
| Race/ethnicity | <.001 | |||||||
| White, non-Hispanic | 7,459 | 26.5 | 4,416 | 47.3 | 3,043 | 16.2 | 51.4 | |
| Black, non-Hispanic | 16,341 | 58.1 | 3,635 | 39.0 | 12,706 | 67.6 | 36.3 | |
| Other, non-Hispanic | 597 | 2.1 | 302 | 3.2 | 295 | 1.6 | 2.9 | |
| Hispanic | 3,730 | 13.3 | 976 | 10.5 | 2,754 | 14.7 | 9.4 | |
| Medicaid waiver type | <.001 | |||||||
| Persons with Disabilities | 907 | 3.2 | 262 | 2.8 | 645 | 3.4 | 2.4 | |
| Persons with Brain Injuries | 175 | .6 | 46 | .5 | 129 | .7 | .5 | |
| Adults with Development Disabilities | 798 | 2.8 | 454 | 4.9 | 344 | 1.8 | 4.9 | |
| Persons who are Elderly | 722 | 2.6 | 155 | 1.7 | 567 | 3.0 | 1.7 | |
| Persons with HIV or AIDS | 169 | .6 | 25 | .3 | 144 | .8 | .3 | |
| Supportive Living Facilities | 103 | .4 | 77 | .8 | 26 | .1 | .8 | |
| Nursing home resident | 4,205 | 15.0 | 1,426 | 15.3 | 2,779 | 14.8 | .266 | 15.6 |
| Common behavioral health conditions | ||||||||
| Schizophrenia and other psychotic disorders | 10,612 | 37.7 | 3,262 | 35.0 | 7,350 | 39.1 | <.001 | 4.3 |
| Bipolar disorder | 8,352 | 29.7 | 2,957 | 31.7 | 5,395 | 28.7 | <.001 | 28.3 |
| Major depression | 8,274 | 29.4 | 2,632 | 28.2 | 5,642 | 30.0 | .002 | 29.5 |
| Substance use disorders | 7,168 | 25.5 | 1,589 | 17.0 | 5,579 | 29.7 | <.001 | 15.2 |
| Anxiety disorder | 6,896 | 24.5 | 2,554 | 27.4 | 4,342 | 23.1 | <.001 | 29.1 |
| Alcohol use disorder | 4,742 | 16.9 | 1,337 | 14.3 | 3,405 | 18.1 | <.001 | 15.3 |
| Common physical health conditions | ||||||||
| Hypertension, uncomplicated & complicated | 13,927 | 49.5 | 4,306 | 46.2 | 9,621 | 51.2 | <.001 | 47.4 |
| Chronic pulmonary disease | 9,064 | 32.2 | 2,543 | 27.3 | 6,521 | 34.7 | <.001 | 25.8 |
| Diabetes, uncomplicated & complicated | 7,760 | 27.6 | 2,444 | 26.2 | 5,203 | 27.7 | .009 | 29.4 |
| Obesity | 3,521 | 12.5 | 1,277 | 13.7 | 2,244 | 11.9 | <.001 | 13.5 |
| Cardiac arrhythmia | 3,469 | 12.3 | 1,149 | 12.3 | 2,320 | 12.3 | .952 | 1.3 |
| Congestive heart failure | 2,709 | 9.6 | 838 | 9.0 | 1,871 | 10.0 | .009 | 8.9 |
| Mean | SD | Mean | SD | Mean | SD | Mean | ||
| Age in 2011 | 46.7 | 13.0 | 45.9 | 14.3 | 47.1 | 12.3 | <.001 | 46.1 |
| Average number of visits per month per 100 persons during pre-ICP months | ||||||||
| Primary care visits, all-cause | 35.6 | 48.8 | 36.5 | 48.6 | 35.1 | 48.8 | .018 | 36.0 |
| Outpatient visits, behavioral health-specific | 114.0 | 361.6 | 110.2 | 345.5 | 115.9 | 369.4 | .201 | 115.9 |
| Emergency department visits, all-cause | 14.0 | 33.0 | 14.0 | 33.5 | 14.0 | 32.8 | .997 | 14.1 |
| Emergency department, behavioral health-specific | 1.5 | 7.5 | 1.3 | 6.8 | 1.6 | 7.8 | .001 | 1.8 |
| Inpatient admissions, all-cause | 12.4 | 40.1 | 8.3 | 22.6 | 14.5 | 46.3 | <.001 | 9.1 |
| Inpatient admissions, behavioral health-specific | 4.0 | 15.8 | 2.6 | 9.6 | 4.7 | 18.1 | <.001 | 3.1 |
| Dental visits | 5.1 | 12.0 | 6.0 | 13.4 | 4.6 | 11.3 | <.001 | 6.0 |
| Average Medicaid expenditures per member per month ($) | 2187 | 3646 | 2426 | 3646 | 2259 | 3725 | .572 | 2706 |
Yit denotes the outcome measure for person i at month t. Suburbani is a dichotomous indicator of group assignment (Suburban treatment group vs Chicago comparison group). ICPt, SMARTt, and CapitationAdjt are time-period indicators of the period after the implementation of ICP, SMART Act, and capitation adjustment, respectively. θt is a set of month indicators capturing monthly fixed effects. Parameter of interests β5 denotes the DD estimate of the ICP effect relative to the original FFS program (before the SMART Act). β6 represents the incremental change in the DD estimate of the ICP effect relative to the FFS program after the SMART Act (hereafter referred to as the restrictive FFS program). The sum of β5 and β6 denotes the cumulative effect of ICP relative to the restrictive FFS program. β7 is the incremental change in the DD estimate of the ICP effect after capitation adjustment. The sum of β5, β6, and β7 denotes the cumulative effect of the re-capitated ICP program relative to the restrictive FFS program. Supplementary analysis was performed to estimate the percentage of people who incurred one or more visits in each service category per month. Patients who use large amounts of health services disproportionally drive the distribution of number of health care visits. Assessing the percentage of people who utilized any services provides additional information on access to care.
The Institutional Review Boards at the University of Illinois-Chicago and Northwestern University approved this study.
RESULTS
Table 1 presents sample characteristics during the pre-ICP months (N=28,127). Schizophrenia and other psychotic disorders were the most common behavioral health condition (37.7%). More than one-quarter of the sample had a diagnosis of bipolar disorder, major depression, or substance use disorder. Physical comorbidity was common. Half of the sample had hypertension (49.5%), one-third had chronic pulmonary disease (32.2%), and more than one quarter had diabetes (27.6%). Average Medicaid payments were $2187 per member per month under FFS. In the unweighted sample, the ICP group was younger and had more females and whites compared with the comparison group. The comparison group had higher prevalence of hypertension, chronic pulmonary disease, and diabetes. Baseline covariates did not differ significantly in the weighted sample from bivariate comparisons.
Outpatient service
Table 2 presents main results. ICP was initially associated with 2.8 fewer all-cause primary care visits per 100 persons per month relative to the original FFS program (p<.01). The SMART Act reversed this trend, resulting in an incremental increase of 10.1 visits per 100 persons per month for the ICP group (p<.001). Capitation adjustment was associated with an incremental increase of 5.9 visits per 100 persons per month (p<.001). The Heteroscedasticity-Robust F tests of the combined effects showed that ICP group had 7.3 (p<.001) more primary care visits per 100 persons per month relative to the restrictive FFS program (Wooldridge, 2013). By the end of the study period, the ICP group had 13.3 more primary care visits per 100 persons per month relative to the restrictive FFS program.
Table 2.
Estimates of the ICP effects from matched-comparison difference-in-differences models
| Outcomes | β5 | β6 | β7 | β5 + β6 | β5 + β6 + β7 | |||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | b | 95% CI | b | 95% CI | b | b | |
| Primary care visits, all-cause | −2.8** | −4.8, −.81 | 10.1*** | 8.7, 11.6 | 5.9*** | 4.5, 7.3 | 7.3*** | 13.3*** |
| Outpatient visits, behavioral health-specific | −34.6*** | −51.4, −17.8 | 28.1 | 10.8, 45.4 | −1.5 | −7.2, 4.3 | −6.5 | −8.0 |
| Emergency department visits, all-cause | 1.63 | −.12, 3.4 | −.8 | −2.4, .8 | .8 | −.6, 2.1 | .8 | 1.5*** |
| Emergency department visits, behavioral health-specific | .6 | −.0, 1.3 | .0 | −.9, .9 | .7** | .2, 1.2 | .7* | 1.4*** |
| Inpatient admissions, all-cause | −2.5* | −4.7, −.2 | −5.3 | −19.7, 9.0 | −1.4 | −3.3, .5 | −7.8 | −9.3 |
| Inpatient admissions, behavioral-health specific | .7 | −.8, 2.2 | 0 | −1.3, 1.3 | .7 | −1.7, .3 | −.7 | 0 |
| Dental visits | −.4 | −1.0, .1 | 2.1*** | 1.7, 2.6 | −.3* | −.6, −.1 | 1.7*** | 1.4*** |
| Medicaid expenditures per person per month ($) | −228** | −368, −87 | 96 | −171, 364 | −247*** | −374, −119 | −132 | −378 |
Notes. Visits are the number of visits per month per 100 persons. Parameter of interests β5 denotes the DID estimate of the ICP effect relative to the original FFS program (before the SMART Act). β6 represents the incremental change in the DD estimate of the ICP effect relative to the FFS program after the SMART Act. β7 is the incremental change in the DD estimate of the ICP effect after capitation adjustment The sum of β5 and β6 denotes the cumulative effect of ICP relative to the restrictive FFS program. The sum of β5, β6, and β7 denotes the cumulative effect of the re-capitated ICP program relative to the restrictive FFS program.
p<.05
p<.01
p<.001
Utilization of behavioral health-specific outpatient services showed similar patterns of change, from a net decrease of 34.6 visits per 100 persons per month during the initial ICP period (p<.001) to an incremental increase of 28.1 visits per 100 persons per month after implementation of the restrictive FFS program (p<.05). F tests of the combined effects were not significant, suggesting the overall utilization rates of behavioral health-specific outpatient services did not differ between the ICP group and the restrictive FFS program. Supplementary analysis showed that the percentage of people who used behavioral health-specific outpatient services increased by 4.1% for the ICP group relative to the restrictive FFS program by the end of the study period (p<.001; data not shown).
Emergency department services
The ICP group had 1.6 more all-cause emergency department visits per 100 persons per month relative to the original FFS program before the enactment of the SMART Act; however, this increase was not statistically significant. F tests suggest that the ICP group had 1.5 more all-cause emergency department visits per 100 persons per month compared with the restrictive FFS program by the end of the study period (p<.001). Supplementary analysis suggested that the percentage of people who visited the emergency department did not differ between the ICP group and the FFS program.
The ICP group had 1.4 more behavioral health-specific emergency department visits per 100 persons per month relative to the restrictive FFS program (p<.001). Supplementary analysis suggested that the percentage of people with at least one behavioral health-specific emergency department visits increased by 0.9% for the ICP group relative to the restrictive FFS program (p<.001; data not shown).
Inpatient services
Number of all-cause inpatient admissions decreased by 2.5 per 100 persons per month for the ICP group compared with the original FFS program (p<.05). The relative difference in inpatient utilization grew larger with the implementation of the SMART Act and capitation adjustments but was not significantly different. Supplementary analysis showed that the percentage of people with at least one inpatient admission per month decreased by 1.3% for the ICP group compared with the original FFS program (p<.01; data not shown).
Behavioral health-specific inpatient utilization rates did not change significantly with the implementation of ICP, SMART Act, or capitation adjustment.
Dental services
ICP was not associated with a significant change in dental services utilization during the initial ICP period. After the SMART Act, however, the number of dental visits increased by 2.1 per 100 persons per month for the ICP group relative to the restrictive FFS program (p<.001). This relative increase was largely maintained after capitation adjustments. Supplementary analysis showed that the percentage of people who had at least one dental visit in each month increased by 1% in the ICP group relative to the FFS program at the end of the study period (p<.001).
Expenditures
Medicaid expenditures decreased by $228 (p<.05) per member per month during the initial ICP implementation. Cost savings associated with ICP disappeared following the implementation of the SMART Act. There was no discernible difference in average cost per member per month between the two groups after the SMART Act and before capitation adjustments. Capitation adjustment was associated with an incremental savings of $247 (p<.001) per member per month for the ICP group relative to the FFS program. Although the re-capitated ICP group incurred $378 less per member per month relative to the FFS program at the end of the study period, this combined effect was not statistically significant due to large standard errors (F(1,28125)=3.42, p=.065).
DISCUSSION
This study provides evidence of the effects of ICP—a fully-capitated, integrated MMC (“carve-in”) program for Medicaid beneficiaries with behavioral health conditions. The impact of ICP was affected by additional policy initiatives, including the implementation of the SMART Act that restricted access to care for the FFS comparison group and the implementation of capitation adjustments that lowered payments to MCOs. Before the SMART Act, ICP achieved cost savings to the state Medicaid program relative to a FFS program; however, the relative impact of ICP on services utilization were mixed. Under the SMART Act, ICP outperformed the restrictive FFS program such that utilization of outpatient and dental services increased without incurring significantly higher costs to the state Medicaid program. Lowering capitation rates resulted in additional, significant cost savings for ICP.
Changes in the relative impact of ICP after the SMART Act are not surprising as the Act reduced access and reimbursement rates for many outpatient services and eliminated non-emergency dental services. MCOs administering ICP decided against these changes. Because the SMART Act brought substantial changes, the DD estimates of the ICP effect during this period were heavily influenced by the large reductions in services utilization and costs in the FFS comparison group rather than changes in the ICP group. Absent the SMART Act, it is likely that ICP would have significantly reduced Medicaid spending per person per month.
The initial decrease in the utilization rates of primary care and behavioral health-specific outpatient services associated with the ICP program may reflect the “learning curve” MCOs experience as they become responsible for serving new populations and providing new services (Sturm, 1999). The two MCOs serving the ICP pilot population were large, for-profit companies that were new to the Medicaid population and the state. Because provider networks were slow to develop during the initial phase, disruptions in services might have occurred. A survey conducted by the ICP evaluation team revealed that nearly two-thirds of ICP enrollees could not continue to see at least one provider and one-third had to find new providers after transitioning from FFS to ICP (Owen, Heller, & Bowers, 2016).
The increase in behavioral health-specific emergency department utilization may be the result of increased reporting of diagnoses in the managed care program. The state uses the Chronic Illness and Disability Payment System (CDPS)—a diagnostic classification system—to adjust capitation rates to MCOs. As shown in the Medicare Advantage Program, diagnosis-based risk adjustment creates greater incentive for managed care providers than FFS providers to report diagnoses (Kronick, & Welch, 2014). Because we identified behavioral health-specific emergency department utilization based on the diagnoses rather than the nature of services, the corresponding result could merely reflect the tendency to report diagnosis under managed care.
This study has several limitations. First, although we employed IPTW to mitigate bias associated with baseline differences in the treated and comparison groups, IPTW relies on observed covariates and does not address potential group differences that are not observed. Potential confounders due to unobserved differences between the Suburban and Chicago populations may bias the study estimates. Second, the DID regressions estimated the intention-to-treat effect of ICP using initial residence (suburban county vs city of Chicago) as group assignment. Change in residence and non-compliance may have occurred, however, additional analyses did not reveal substantial changes in ICP effects estimated in a treatment-on-the-treated framework. Third, identification of mental health specific-utilization of emergency department and acute inpatient services relies on the assumption that a primary diagnosis represents actual treatment for the respective disorder. Fourth, we did not examine costs associated with each service category and, therefore, could not elucidate the mechanisms of change in costs. Only costs to the state Medicaid program were examined; assessment of the societal costs was beyond the study scope. Furthermore, the study period was limited. The impact of ICP may have changed as the program stabilized and provider networks were established. The changing effect of ICP with the introduction of the SMART Act and adjustment of capitation arrangements may reflect, to some extent, the impact of the stability and maturity of the ICP with time. In addition, this study was based on experience from a single state. Heterogeneity of Medicaid programs across states means caution is important when generalizing our findings.
Whether ICP improves quality of care and long-term health outcomes remains to be seen. The true impact of changes in utilization rates cannot be fully ascertained without considering the effect on care quality. Improvement in utilization rates does not guarantee adequate access to care, nor does it assure quality of care. Future studies using quality metrics based on claims and administrative data, studies linking claims to mortality data, and studies including survey data capturing enrollees’ experiences will help provide a more complete picture of the impact of ICP.
Future MMC research needs to consider the heterogeneity of the FFS programs that serve as a comparison and how the characteristics of these FFS programs may affect conclusions regarding the effect of MMC. This study showed that changes in the FFS program could produce conflicting results about the effects of managed care. Future studies synthesizing data from multiple sites and programs can add value by testing the moderating effect of the heterogeneity of the FFS programs on the effects of managed care. Studies comparing behavioral health “carve-in” and “carve-out” MMC programs will be helpful in guiding Medicaid policy making. In addition, future studies will add value by exploring the potential differential effects of MMC across population subgroups based on severity or type of mental illness (e.g., serious mental illness, mild to moderate depression and anxiety, substance use disorders).
For state Medicaid policy makers, this study suggests that restricting the scope of services in the FFS program compromises access to care and may not yield significant cost savings compared to managed care for Medicaid beneficiaries with behavioral health conditions. Reducing or eliminating services may cause harm and redistribute costs to other private and public sectors. For example, the elimination of non-emergency adult dental services under the SMART Act may reduce quality of life and increase risk for other chronic health conditions. The first U.S. Surgeon General’s report from Satcher (2000), on oral health reviewed evidence linking chronic oral infections and chronic health conditions such as heart disease, lung disease, and stroke, and concluded that oral health is integral to general health. People in need of dental services may turn to other sectors for help, offsetting decreased Medicaid spending associated with dental services. Over 700,000 emergency department visits for dental-related complaints occur annually in the Unites States, and Medicaid beneficiaries incur a disproportionate share of these visits (Lewis, Lynch, & Johnston, 2003). Whether such substitution occurred in the Illinois Medicaid program needs to be confirmed.
Overall, the Illinois ICP improved utilization of certain services without incurring substantially higher costs. Fully-capitated, integrated MMC programs have the potential to reduce overall Medicaid costs without negative effects on utilization. Setting appropriate capitation rates may help realize cost savings without compromising utilization.
Supplementary Material
Acknowledgments
Funding: This research was funded by the following sources:
National Institutes of Health, grant# R24 P2CHD065702, and K01HD086290; and National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR), grant # 90AR5019, #90RT5023–01-00, #90RT5020–01-00, and #90RT5026–01-00
Footnotes
Compliance with ethical standards:
Conflicts of interest: The authors declare no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Austin PC, Stuart EA (2015). Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Statistics in Medicine, 34(28), 3661–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianconi JM, Mahler JM, McFarland BH (2006). Outcomes for rural Medicaid clients with severe mental illness in fee for service versus managed care. Administration and Policy in Mental Health, 33(4), 411–422. [DOI] [PubMed] [Google Scholar]
- Bindman AB, Chattopadhyay A, Osmond D, Huen W, Bacchetti P (2004). Preventing unnecessary hospitalizations in Medi-Cal: Comparing fee-for-service with managed care. California HealthCare Foundation. Retrieved from http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20P/PDF%20PreventableHospitalizationsInMediCal.pdf [Google Scholar]
- Bouchery E, Harwood H (2003). The Nebraska Medicaid managed behavioral health care initiative: impacts on utilization, expenditures, and quality of care for mental health. The Journal of Behavioral Health Services & Research, 30(1), 93–108. [DOI] [PubMed] [Google Scholar]
- Callahan JJ, Shepard DS, Beinecke RH, Larson MJ, Cavanaugh D (1995). Mental health/substance abuse treatment in managed care: the Massachusetts Medicaid experience. Health Affairs (Millwood), 14(3), 173–184. [DOI] [PubMed] [Google Scholar]
- Clark RE, Leung YH, Lin W, Little FC, O’Connell E, O’Connor DM,… Browne MK. (2009). Twelve-month diagnosed prevalence of mental illness, substance use disorders, and medical comorbidity in Massachusetts Medicare and Medicaid members aged 55 and over. Clinical & Population Health Research, 26 Retrieved from http://escholarship.umassmed.edu/gsbs_cphr/26. [Google Scholar]
- Department of Health & Human Services, Centers for Medicare & Medicaid Services. (2011). CMS Manual System. Pub 100–04 Medicare Claims Processing. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2161CP.pdf.
- Duggan M, Hayford T (2013). Has the shift to managed care reduced Medicaid expenditures? Evidence from state and local-level mandates. Journal of Policy Analysis and Management, 32(3), 505–35. [DOI] [PubMed] [Google Scholar]
- Frank RG, Huskamp HA, McGuire TG, Newhouse JP (1996). Some economics of mental health ‘carve-outs’. Archives of General Psychiatry, 53(10), 933–937. [DOI] [PubMed] [Google Scholar]
- Gifford K, Ellis E, Edwards B, Aimee Lashbrook Health Management Associates, Hinton E, Antonisse L, Valentine A, & Robin Rudowitz Kaiser Family Foundation (2017). Medicaid moving ahead in uncertain times: Resuls from a 50-state Medicaid Budget Survey for State Fiscal Years 2017 and 2018. Available at: http://files.kff.org/attachment/Report-Results-from-a-50-State-Medicaid-Budget-Survey-for-State-Fiscal-Years-2017-and-2018 Accessed August 10, 2018. [Google Scholar]
- Heller T, Owen R, Mitchell D, Eisenberg Y, Wing C, Bowers A,… Viola J (2015). An independent evaluation of the integrated care program: Final report findings through the third year (FY14). Institute on Disability and Human Development, University of Illinois at Chicago. Retrieved from http://www.cbha.net/Resources/Documents/ICP%20Final%202015%20Report%20-%20August%202015.pdf.
- Hutchinson AB, Foster EM (2003). The effect of Medicaid managed care on mental health care for children: A review of the literature. Mental Health Services Research, 5(1), 39–54. [DOI] [PubMed] [Google Scholar]
- Jones K, Huey JC, Jordan N, Boothroyd RA, Ramoni-Perazzi J, & Shern DL (2006). Examination of the effects of financial risk on the formal treatment costs for a Medicaid population with psychiatric disabilities. Medical Care, 44(4), 320–327. [DOI] [PubMed] [Google Scholar]
- Kronick RG, Bella M, Gilmer TP (2009). The faces of Medicaid III: Refining the portrait of people with multiple chronic conditions. Retrieved from http://www.chcs.org/media/Faces_of_Medicaid_III.pdf.
- Kronick R, Welch WP (2014). Measuring coding intensity in the Medicare Advantage program. Medicare & Medicaid Research Review, 4(2). Retrieved from https://www.cms.gov/mmrr/downloads/mmrr2014_004_02_a06.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff HS, Wieman DA, McFarland BH, Morrissey JP, Rothbard A, Shern DL,… Allen IE (2005). Assessment of Medicaid managed behavioral health care for persons with serious mental illness. Psychiatric Services, 56(10), 1245–1253. [DOI] [PubMed] [Google Scholar]
- Lewis C, Lynch H, Johnston B (2003). Dental complaints in emergency departments: a national perspective. Annals of Emergency Medicine, 42(1), 93–99. [DOI] [PubMed] [Google Scholar]
- Marton J, Yelowitz A, Talbert JC (2014). A tale of two cities? The heterogeneous impact of Medicaid managed care. Journal of Health Economics, 36(2014), 47–68. [DOI] [PubMed] [Google Scholar]
- Masland MC, Snowden LR, Wallace NT (2007). Assessment, authorization and access to medicaid managed mental health care. Administrationa and Policy in Mental Health, 34(6):548–562. [DOI] [PubMed] [Google Scholar]
- National Quality Measures Clearing House. Retrieved from https://www.qualitymeasures.ahrq.gov/browse/domain Accessed January 10, 2017.
- National Committee for Quality Assurance. (2015). Mental health mental health utilization: number and percentage of members receiving the following mental health services during the measurement year: any service, inpatient, intensive outpatient or partial hospitalization, and outpatient or ed. Retrieved from https://www.qualitymeasures.ahrq.gov/summaries/summary/49826.
- Owen R, Heller T, Bowers A (2016). Health services appraisal and the transition to Medicaid Managed Care from fee for service. Disability and Health Journal, 9(2), 239–247. [DOI] [PubMed] [Google Scholar]
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthe J,… Ghali WA. (2005). Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care, 43(11), 1130–1139. [DOI] [PubMed] [Google Scholar]
- Satcher DS (2000). Surgeon General’s report on oral health. Public Health Reports, 115(5), 489–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith VK, Gifford K, Ellis E, Edwards B, Rudowitz R, Hinton E,… Valentine A. (2016, October 15). Implementing coverage and payment initiatives: results from a 50-state Medicaid budget survey for state fiscal years 2016 and 2017. Retrieved from http://www.kff.org/medicaid/report/implementing-coverage-and-payment-initiatives-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2016-and-2017/.
- Sturm R (1999). Cost and quality trends under managed care: Is there a learning curve in behavioral health carve-out plans? Journal of Health Economics, 18(5), 593–604. [DOI] [PubMed] [Google Scholar]
- The Lewin Group. (2009). Medicaid Managed Care cost savings—A synthesis of 24 studies. Working Paper 17236. Retrieved from http://blogs.chicagotribune.com/files/lewinmedicaid.pdf
- Wooldridge JM (2013). Introductory Econometrics: A Modern Approach (5th ed.) Cincinnati, OH: Southwestern College Publishing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.