Abstract
Objectives
We explored the influence of e-trust, e-health literacy, e-health information seeking, and e-health information consumerism on medical satisfaction and positive health perceptions.
Methods
Our sample consisted of 499 randomly selected panel members aged 40–93. We employed hierarchical ordinary least squares (OLS) regression analyses and structural equation modeling (SEM). We examined the moderating role of age on the relationship between medical satisfaction and positive health perceptions.
Results
A significant interaction was found between age and medical satisfaction in predicting positive health perceptions in the OLS regression models. Medical satisfaction has a stronger association with self-care, health-related quality of life, and health status in the older adult sample as compared with the middle-aged sample. SEM analyses revealed that e-health information seeking has an indirect effect on both medical satisfaction and positive health perceptions through its significant direct effect on e-health information consumerism. Both e-trust and e-health consumerism were significant predictors. The e-health literacy and e-trust measures were significant predictors of the positive health perception index in the OLS regression models.
Discussion
The results contribute to our understanding of the potential benefits information technologies have for the health and well-being of computer-connected aging adults.
Keywords: Information, Medical encounter, Perception, Technology
Translational Significance
As patients become better informed of their medical conditions through e-health information seeking and e-health literacy, communication with their health care provider is likely to improve due to the patient’s improved ability to articulate concerns or questions to their providers.
The subjective experience of one’s own health and self-perception of the aging process are important indicators of well-being and longevity as demonstrated by numerous studies (Craciun, Gellert, & Flick, 2017; Ferraro & Wilkinson, 2015; Sims, Reed, & Carr, 2016). Health-related use of the Internet (hereafter referred to as e-health information seeking) has come to represent an important health management strategy among aging baby boomers that appears to empower individuals by increasing their knowledge and understanding with respect to health promotion and maintenance (Cotten, 2017; Czaja, 2017; Seckin, Hughes, Hudson, Laljer, & Yeatts, 2018). Previous research has consistently linked personal perceptions of aging to health outcomes (Carpentieri, Elliot, Brett, & Deary, 2017; Whitley, Popham, & Benzeval, 2016; Young, Frick, & Phelan, 2009). A substantial amount of research has also focused on the impact personal and social resources (or lack thereof) have on an individual’s evaluation of his or her health. However, limited research has examined whether health-related perceptions, subjective health outcomes, and perhaps, even an illness trajectory are impacted by health information technology (Kahana, Kelley-Moore, & Kahana, 2012).
Maintaining health and quality of life through proactive use of technology is of growing interest among researchers who seek to understand the pathways that support increasing longevity in the 21st century (Schulz et al., 2015). In general, older adults prefer health professionals as a trusted health information source, however, they are adopting digital health technologies for their informational needs in an increasingly consumer-driven health care system, wherein the responsibility to maintain/promote health rests on the patient (X. Hu, Bell, Kravitz, & Orrange, 2012).
In the United States, older adults are the fastest growing group of Internet users, who view technology as a resource to promote and support their health and well-being (Choi, 2011; Ernsting, et al., 2017; Gell, Rosenberg, Demiris, LaCroix, & Patel, 2015; Spanakis et al., 2012). Pew Research Center reports that 67% of adults aged 65 and older use the Internet (Anderson & Perrin, 2017). Research has also shown that information gathering from the Internet is positively associated with a feeling of empowerment in managing health, better self-care ability, better health-related quality of life, subjective sense of better health, and better psychological well-being (Cotten, Ford, Ford, & Hale, 2012; Seckin et al., 2018). It has been argued that within the past decade, the digital revolution’s greatest benefit is facilitating self-health management, health promotion, and active and healthy aging (Cotton, 2017). Even though research in the area of health, technology, and aging is growing, there have not been many studies examining factors that may potentially act as moderating and mediating influences on the relationship between technology use and health (Czaja, 2017). We need to better understand the pathways linking technology use to subjective health and well-being (Sassenberg & Greving, 2016; Paige, Krieger, & Stellefson, 2017; Rowe & Kahn, 2015; Stellefson et al., 2013).
The objective of the current article is to examine the role of e-health information seeking within the context of healthy aging among middle-aged and older computer-connected adults who use the Internet to locate health information. Even though prior research has revealed predictive pathways from personal perceptions to physical health outcomes, few studies have explored mediating and moderating factors that potentially affect the relationship. We address the following questions: (a) Does e-health information seeking contribute to positive health perceptions? (b) Does e-health information consumerism contribute to positive health perceptions? (c) Does satisfaction with perceived changes in medical encounters (hereafter referred to as medical satisfaction) contribute to positive health perceptions? (d) Does age moderate the influence of medical satisfaction on positive health perceptions? (e) Does e-health literacy contribute to positive health perceptions? (f) Does e-trust contribute to positive health perceptions? Data from a nationally representative sample were analyzed to examine these relationships with particular emphasis on older users of e-health information. In addition to using a composite index for positive health perceptions, we also employed item-based analyses to provide a detailed examination of our research questions.
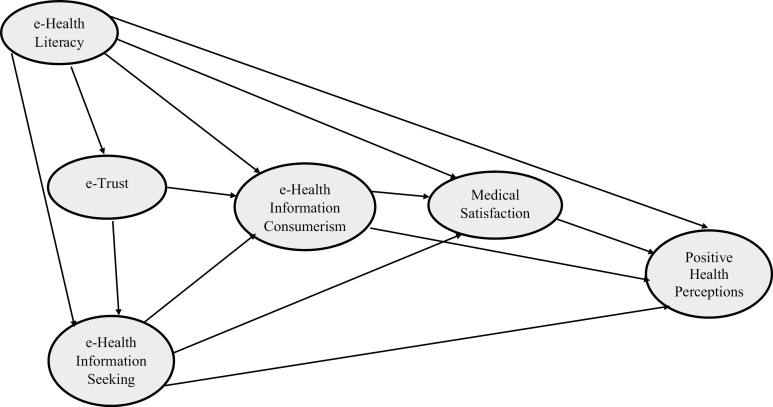
The current study defined e-health information seeking as using the Internet to obtain information for health purposes to restore, maintain, and/or promote health. Building on previous research, the fundamental premise of the conceptual model (Figure 1) is that health-related information seeking on the Internet (e-health information seeking) and utilization of Internet information in the management of health care needs (e-health information consumerism) are associated with medical satisfaction, which in turn, is associated with information users’ health-related perceptions (Dedding, van Doorn, Winkler, & Reis, 2011; Seckin et al., 2018; Tan & Goonawardene, 2017). We examined the impact of age and medical satisfaction separately and as joint moderators by creating an interaction term.
Figure 1.
Conceptual framework.
Taking an active role in managing health depends largely on understanding and utilizing information, which is increasingly available on the web (Tennant et al., 2015). Previous research indicates that individuals who utilized online information sources exposed themselves to more information that enabled them to monitor their health and engage in more proactive consumption of health services leading to better health outcomes (Hale, Chou, & Cotten, 2018). However, the rapid proliferation of health-related information on the Internet and the increased acceptance and utilization of such information raise concerns among health care providers (Sbaffi & Rowley, 2017). While the Internet quickly connects consumers with the latest health and medical information, most Internet users face challenges when deciding the trustworthiness of the information they find and struggle with assessing the credibility of information in the ever-expanding digital health landscape (Thai et al., 2018).
Critical evaluation and appraisal of information is needed to perform self-care and other health-related tasks, which are a crucial challenge for the aging population. We conceptualize e-health literacy as an Internet user’s competence to appraise the credibility and trustworthiness of the online health information that is used to make decisions concerning their health care (Sørensen et al., 2012). Furthermore, given that traditional methods of acquiring information and gaining knowledge have increasingly shifted to the Internet, it is also important to examine the extent of user trust in e-health information, to which we refer as e-trust. We believe e-health literacy and e-trust are important variables to consider as they may affect the extent to which the information-seeker perceives that information on the Internet is credible and trustworthy (Townsend et al., 2015). Thus, both e-health literacy and e-trust variables were modeled as pathways leading to e-health information seeking in our research. We examined whether differential patterns of associations are observed among respondents 60 years of age and older following the full sample analyses.
We propose the following hypotheses predicting main effects in the OLS regression models:
• H1: e-health information seeking is associated with positive health perceptions.
• H2: e-health information consumerism is associated with positive health perceptions.
• H3: Medical satisfaction is associated with positive health perceptions.
• H4: e-trust is associated with positive health perceptions.
• H5: e-health literacy is associated with positive health perceptions.
We propose the following hypothesis predicting interaction effects in the OLS regression models:
• H6: Chronological age moderates the influence of medical satisfaction on positive health perceptions.
We propose the following hypotheses predicting mediation effects in the SEM model:
• H7: Medical satisfaction will mediate the effect of e-health consumerism on positive health perceptions.
• H8: e-heath information seeking will have a direct effect on positive health perceptions.
• H9: The indirect effect of e-health information seeking on positive health perceptions will be mediated via e-health information consumerism.
• H10: The indirect effect of e-health information seeking on positive health perceptions will be mediated via medical satisfaction.
• H11: e-health information consumerism will have a direct effect on positive health perceptions.
In addition to the analyses of the composite index for positive health perceptions, we examined whether differential patterns of associations are obtained at the item level by performing item-based analyses.
Design and Methods
Sample
Respondents were randomly sampled from the largest national online probability-based research panel developed by Knowledge Networks (KN). KN employed an address-based sampling frame derived from the U.S. Postal Service Delivery Sequence File, which covers 97% of U.S. households, thereby maximizing sample representativeness. Analyses are representative of the larger U.S. population because all KN panel households were selected randomly with a known probability of selection, and our sample members were further randomly selected from the larger panel for recruitment. KN sent a recruitment email invitation to 1,315 randomly selected panel members. A screening question asked whether the respondent had sought health or medical information on the Internet; and of the 1,315 invited panel members, 870 completed the screening question. One hundred sixty respondents did not qualify for participation in the study since they never used the Internet to locate health information, which left a sample size of 710 respondents. Our sample includes a broad age range (40–93), which allows for examination of the moderating role of chronological age in hypothesized associations and the ability to make age-group comparisons between middle-aged and older adults.
Measures
Demographic variables included age, gender, race/ethnicity, marital status, education, and income levels. Age was measured as a continuous variable. For age-based comparisons, we collapsed this continuous variable into two groups: (a) middle-aged respondents: 40–59 and (b) older respondents: 60 and older. Gender was coded as 0 (male) and 1 (female). Race was coded as 0 (Caucasian) and 1 (Minority). Marital status was coded as 0 (married) and 1 (unmarried). Education was coded as 1 (high school or less), 2 (some college or associate’s degree), 3 (college degree), and 4 (postgraduate degree). Income was coded as follows: 1 ($29,999 or less), 2 ($30,000–$59,999), 3 ($60,000–$99,999), and 4 ($100,000 and above).
e-Health Information Seeking was assessed with five items: (a) “How often do you seek health information on the Internet?” (b) “Do you consult the Internet before you visit a health care provider?” (c) “Do you consult the Internet after your visit to a health care provider?” (d) “Do you discuss the information you obtain from the Internet with a health care provider?” and (e) “Do you ask a health care provider for advice about where to find credible health or medical information on the Internet?” Each item was rated using a 5-point Likert scale ranging from 1 = “never” to 5 = “always.” The Cronbach’s alpha is .77.
e-Health Literacy was measured with the e-HLS scale (Seçkin, Yeatts, Hughes, Hudson, & Bell, 2016). Items assessed whether respondents perform the following when seeking health information from the Internet: (a) “read disclosure statements on health websites,” (b) “check for credentials and institutional affiliations of those who provide information,” (c) “check the ownership of a health website,” (d) “check a website’s sponsor(s),” (e) “check for financial ties between the website information and the website’s sponsor(s),” (f) “appraise the adequacy and integrity of the information providers’ credentials,” (g) “check to see whether a physical address is provided,” (h) “check for stated goals and objectives,” (i) “appraise whether coverage of health topics is clear and comprehensive,” (j) “check whether other print or web resources confirm information provided,” (k) “check whether information is current and updated,” and (l) “check the last time the information was updated.” The Cronbach’s alpha is .95. Responses ranged from 1 = “never” to 5 = “always.”
e-Trust was measured by four items that asked whether respondents (a) “believe the information provided on the Internet was credible,” (b) “believe the information provided on the Internet was balanced and accurate,” (c) “think the information provided on the Internet was the same as or better than what most health professionals provided,” and (d) “trust the Internet for obtaining accurate health information.” Items were rated on a scale ranging from 1 = “strongly disagree” to 5 = “strongly agree.” The Cronbach’s alpha is .83.
e-Health Information Consumerism was measured with the following eight items: (a) “Do you seek information on the Internet to self-diagnose?” (b) “Do you use information from the Internet to identify appropriate treatments for yourself?” (c) “Do you request medications from a health care provider based on the Internet information?” (d) “Do you request medical examinations from a health care provider based on the Internet information?” (e) “Do you request treatments from a health care provider based on the Internet information?” (f) “Do you purchase medications based on the Internet information?” (g) “Do you treat a health issue based on the Internet information?” and (h) “Do you use information from the Internet to make treatment decisions?” Response options ranged from 1 = “never” to 5 = “always” Cronbach’s alpha is .89.
Satisfaction with Perceived Changes in Medical Encounters (Medical Satisfaction) as a result of information gathering from the Internet was measured with seven indicators that assessed the extent to which respondents agree with the following statements: (a) “Information on the Internet helps me to communicate more effectively with health providers during appointments,” (b) “Information on the Internet helps me to ask more informed questions to health providers,” (c) “Information on the Internet helps me to better understand what my health provider is telling me during appointments,” (d) “Interactions of health care providers with me have become more respectful as a result of gathering health or medical information from the Internet resources,” (e) “I receive more information from health care providers as a result of gathering health or medical information from the Internet resources,” (f) “I receive more attention from health care providers as a result of gathering health or medical information from the Internet,” and (g) “Interactions with health care providers have become strained as a result of gathering health or medical information from the Internet” (reverse coded). Response options ranged from 1 = “strongly disagree” to 5 = “strongly agree.” The Cronbach’s alpha is .83.
Positive Health Perceptions were measured by respondents’ perceptions of their own health-related outcomes in three separate health domains that are found to be of particular relevance to older adults. The first one reflects personal efficacy beliefs regarding one’s ability to provide better self-health care while the second and third reflect beliefs about one’s perceived improvements in health status and subjective health quality of life. These items include: (a) “I take better care of my health as a result of gathering health or medical information from the Internet,” (b) “My quality of life has improved as a result of gathering health or medical information from the Internet,” and (c) “My health has improved as a result of gathering health or medical information from the Internet.” Responses ranged from 1 = “strongly disagree” to 5 = “strongly agree.” We created a composite scale by taking an average of these items, which we refer to as the positive health perception index. The Cronbach’s alpha coefficient for the 3-item composite scale is .88. In addition to a composite scale, we also conducted item-based analyses.
Data Analysis Strategy
Data analyses proceeded in four steps. First, we examined descriptive statistics and bivariate correlations. Next, we examined OLS regression models to test our Hypotheses 1–6. We ran a separate regression model for each indicator of health perceptions in addition to our base model (a total of four models). In the first step of each model (Model A), we entered the main effects. In the second step of each model (Model B), we added the interaction term between age and medical satisfaction. We performed age-stratified analyses by running parallel models for the middle-aged and older adult sample. Our analytical approach includes using a composite measure of positive health perceptions and item-based analyses. The positive health perception index is a composite scale that yields a single score. The ability of the composite scale to provide information regarding the extent to which people report positive health perceptions makes it a valuable assessment tool. However, combining data from multiple items into a single score may suppress a potential differential association of each indicator with the predictor. Analyses were conducted using SPSS 22.
Next, we performed path modeling (SEM) using AMOS version 22 to test hypotheses 7–11. We examined direct, indirect (mediational), and total effects of e-health literacy, e-trust, and e-health consumerism on the relationship between e-health information seeking and the positive health perception index. SEM employs a latent-construct modeling strategy that tests model fit for multiple observed indicators of each latent construct while minimizing multicollinearity among variables and controlling for measurement error (Kline, 2011). Multiple goodness of fit criteria were examined as chi-square is sensitive to sample size and tends to reach significance easily for samples of more than 400 cases, leading to rejection of model fit (L. T. Hu & Bentler, 1999; Kline, 2011; Steiger, 2007). We utilized the following cutoff points for model fit: RMSEA = .005, CFI = 0.90, NFI = .90, and TLI = 0.90 (Arbuckle, 2010; Kenny, 2015). This article treats OLS regressions (moderation analyses) and path modeling (SEM analyses) as complementary rather than as alternative data analytical approaches to the examination of our research questions, and both as important statistical models in the overall explanatory structure of the article.
Results
We present descriptive statistics in Table 1. Bivariate correlations for the full sample are provided in Table 2. Older age is negatively correlated with e-health information seeking, e-health information consumerism, and the positive health perception index. The positive health perception index has significant positive correlations with both e-health information seeking and medical satisfaction. In the older sample, e-health information gathering is positively related to medical satisfaction (r = .511, p ≤ .0001) and the positive health perception index (r = .351, p ≤ .0001). A positive correlation exists between e-health consumerism and the positive health perception index (r = .491, p ≤ .0001). Additionally, medical satisfaction is significantly correlated with the positive health perception index (r = .630, p ≤ .0001). In the middle-aged sample, we found that e-health information gathering is positively associated with the positive health perception index (r = .411, p ≤ .0001). There are also positive correlations between the positive health perception index and e-health consumerism (r = .477, p ≤ .0001) and satisfaction with medical encounters (r = .480, p ≤ .0001).
Table 1.
Descriptive Statistics for Key Variables by Age Groups (N = 499)
| Mean (SD)/percentages | |||||
|---|---|---|---|---|---|
| Covariates | Full sample 40–93 (N = 499) |
Middle-aged sample 40–59 (N = 305) |
Older adult sample 60–93 (N = 194) |
F-value/χ2 | p Value |
| Age | 57.25 (11.26) | 49.94 (5.85) | 68.74 (7.48) | 6.56 | .50 |
| Gender (female) | 52.3% | 49.5% | 55.2% | 1.03 | .31 |
| Race (Caucasian) | 78.65% | 76.1% | 82.5% | 2.89 | .08 |
| Education (bachelor degree or higher) | 39.0% | 40.0% | 37.6% | 0.49 | .48 |
| Marital status (married) | 65.7% | 67.9% | 62.4% | 1.60 | .21 |
| Income ($60,000 and above) | 58.0% | 40.0% | 51.1% | 7.54 | .01 |
| Medical satisfaction | 3.33 (0.56) | 3.32 (0.55) | 3.35 (0.58) | 1.56 | .94 |
| e-Health information seeking | 2.41 (0.68) | 2.44 (0.67) | 2.36 (0.68) | .045 | .17 |
| e-Trust | 2.80 (0.63) | 2.82 (0.61) | 2.78 (0.65) | 1.44 | .56 |
| e-Health information consumerism | 1.84 (0.62) | 3.38 (1.86) | 1.79 (0.65) | 1.91 | .20 |
| e-Health literacy | 2.44 (1.04) | 2.43 (0.99) | 2.46 (1.09) | 3.95 | .79 |
| Positive health perception index | 3.00 (0.69) | 3.05 (0.65) | 2.92 (0.76) | 6.06 | .05 |
Table 2.
Pearson Correlation Matrix (N = 499)
| Covariates | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1 | |||||||||||
| 2. Gender | .04 | 1 | ||||||||||
| 3. Race | .11** | −.03 | 1 | |||||||||
| 4. Education | −.07 | −.10* | .02 | 1 | ||||||||
| 5. Marital status | −.12** | −.02 | .02 | .03 | 1 | . | . | |||||
| 6. Income | −.14** | −.09* | .02 | .41*** | .33*** | 1 | ||||||
| 7. Medical satisfaction | −.02 | −.03 | .07 | .06 | .03 | .07 | 1 | |||||
| 8. e- Information seeking | −.11** | .10 | .08 | .18*** | .07 | .11** | .54*** | 1 | ||||
| 9. e-Trust | −.06 | −.04 | −.03 | −.08 | −.04 | −.03 | .35*** | .23*** | 1 | |||
| 10. Information consumerism | −.13** | .02 | .04 | .08* | .05 | .04 | .52*** | .69*** | .40*** | 1 | ||
| 11. e-Health literacy | −.04 | .07 | .09* | .25*** | −.02 | .07 | .40*** | .66*** | .11** | .52*** | 1 | |
| 12. Positive health perception index | −.10* | −.11* | .06 | .12** | .04 | .03 | .54*** | .39*** | .40*** | .48*** | .36*** | 1 |
***p < .001. **p < .01. *p < .05.
We hypothesized that each one of our predictors, that is, e-health literacy, e-trust, e-health information seeking, e-health information consumerism, and medical satisfaction would have a significant main effect on positive health perceptions. We also predicted that there would be a significant interaction between age and medical satisfaction. We present regression models for the full sample in Table 3. We tested multiple regression models for both age groups using each indicator of the positive health perception index as the dependent variable. We also provide the results separately for the older adult sample (Supplementary Table 1) and the middle-aged sample (Supplementary Table 2). The first model in each table is the main effect model (Models 1A, 2A, 3A, etc.). In the second step (Models 1B, 2B, 3B, etc.), we added the interaction term (age × medical satisfaction) as a predictor.
Table 3.
Ordinary Least Squares Regression Analyses of the Full Sample (N = 499)
| Positive Health Perception Index | Better Self-Health Care | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1A | Model 1B | Model 2A | Model 2B | |||||
| Covariates | β | SE | β | SE | β | SE | β | SE |
| Intercept | .778*** | .239 | 2.511*** | .427 | .438 | .289 | 1.688*** | .471 |
| Age | −.056 | .002 | −.561*** | −.035 | −.011 | .003 | −.328*** | .007 |
| Education | .076 | .025 | .095** | .024 | .035 | .030 | .047 | .030 |
| Gender | −.081* | .049 | −.077* | .048 | −.033 | .060 | −.031 | .059 |
| Race | .027 | .060 | .024 | .058 | −.006 | .073 | −.009 | .072 |
| Income | −.065 | .027 | −.062 | .026 | −.006 | .032 | −.004 | .003 |
| Marital status | .063 | .055 | .059 | .053 | .044 | .067 | .041 | .066 |
| e-Health information seeking | −.097 | .059 | −.075 | .057 | −.073 | .071 | −.059 | .070 |
| Medical satisfaction | .357*** | .054 | .076 | .107 | .344*** | .066 | .072 | .132 |
| e-Trust | .205*** | .044 | .191*** | .043 | .217*** | .053 | .208*** | .053 |
| e-Health information consumerism | .199*** | .060 | .170*** | .058 | .182*** | .072 | .164** | .072 |
| e-Health literacy | .142** | .032 | .143** | .031 | .076 | .039 | .076 | .038 |
| Age × Medical satisfaction | — | — | .692*** | .002 | — | .434*** | .002 | |
| R 2 | .408 | .445 | .344 | .359 | ||||
| Improvement in Health Quality of Life | Improvement in Health Status | |||||||
| Model 3A | Model 3B | Model 4A | Model 4B | |||||
| Covariates | β | SE | β | SE | β | SE | β | SE |
| Intercept | .873* | .277 | 2.649** | .445 | 1.022*** | .288 | 3.195*** | .458 |
| Age | −.058 | .003 | −.532*** | .007 | −.083* | .003 | −.648*** | .007 |
| Education | .078 | .029 | .096* | .028 | .091* | .030 | .113** | .029 |
| Gender | −.097** | .057 | −.093** | .056 | −.088* | .060 | −.083* | .058 |
| Race | .024 | .069 | .020 | .068 | .057 | .072 | .053 | .070 |
| Income | −066 | .031 | −.062 | .030 | −.105** | .032 | −.101** | .031 |
| Marital status | .072 | .064 | .068 | .062 | .054 | .066 | .049 | .064 |
| e-Health information seeking | −.063 | .068 | −.042 | −.048 | −.124* | .071 | −.099 | .069 |
| Medical satisfaction | .302*** | .063 | −.105 | .125 | .309*** | .066 | −.175 | .129 |
| e-Trust | .160*** | .051 | .146*** | .050 | .171** | .053 | .154*** | .051 |
| e-Health information consumerism | .176*** | .069 | .149** | .0680 | .174** | .072 | .142** | .070 |
| e-Health literacy | .152** | .037 | .153** | .036 | .154** | .039 | .155** | .037 |
| Age × Medical satisfaction | — | — | .649*** | .002 | — | — | .774*** | .002 |
| R 2 | .334 | .367 | .315 | .361 | ||||
OLS analyses in the full sample showed that the association of e-health information seeking with the positive health perception index was not significant. E-health information seeking was negatively associated with perceived improvement in health (β = −.124, p ≤ .05), which became nonsignificant when the interaction term between age and medical satisfaction was included. On the other hand, the nonsignificant main effect of age on the positive health perception index became significant with the inclusion of the interaction (β = −.561, p ≤ .001). Additionally, the significant association of age with perceived health status increased in strength (from β = −.083, p ≤ .05 to β = −.648, p ≤ .0001). Furthermore, e-health literacy, e-trust, and e-health information consumerism were significant predictors of the positive health perception index and for each one of its individual indicators, with the exception of e-health literacy being nonsignificant for self-health care. The significant relationship between e-health information consumerism and the positive health perception index decreased (from β = .199, p ≤ .0001 to β = .170, p ≤ .0001) with the inclusion of the interaction term. Women reported lower scores on the positive health perception index including its individual indicators except, self-care.
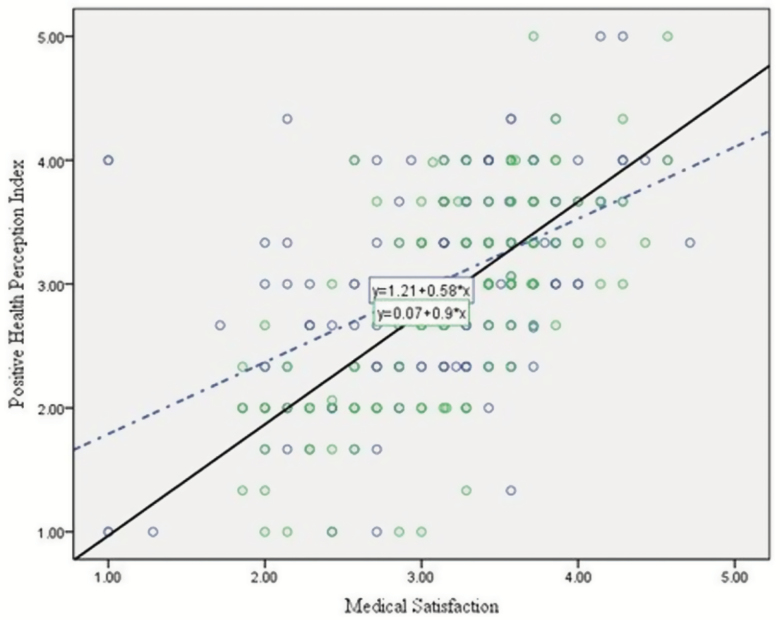
The significant interaction term in the full sample revealed that age moderated the relationship between medical satisfaction and positive health perceptions. Figure 2 illustrates the age-stratified comparison of simple slopes of the interaction between satisfaction with medical encounters and the positive health perception index. After controlling for the effects of covariates, medical satisfaction explained 46% of the variance in the positive health perception index for the older sample while it explained 26% in the middle-aged group. In other words, the interaction term explained a greater variance in the older age sample as compared with the middle-aged sample. This significant moderation effect was maintained in all regression models for each indicator of positive health perceptions (Table 3). These significant interactions indicate that the impact of medical satisfaction on each of the positive health perception indicators was stronger in the older sample compared to the middle-aged respondents (figures showing age-stratified simple slopes of the interactions are available on request). Further analysis of the full sample by creating an interaction term between e-trust and medical satisfaction (not shown in Table 3) revealed that those who reported higher levels of e-trust but less medical satisfaction indicated lower scores on the positive health perception index (β = −.491, p ≤ .05).
Figure 2.
Moderation effect of age on medical satisfaction and the positive health perception index. Solid line represents the older adults sample. Dashed line represents the middle-aged sample.
Even though older adults reported lower averages on the health perception index (β = −.561, p ≤ .001), those who indicated greater medical satisfaction also reported greater positive health perceptions, as evidenced by a significant positive interaction effect (β = .692, p ≤ .001). When the interaction term was included in the regression models, the relationship between e-trust, e-health literacy, e-health consumerism, and the positive health perception index decreased, but remained significant for each (Table 3). However, when we included the interaction term, the main effect of e-health consumerism on the positive health perception index was no longer significant for older adults (Supplementary Table 1). In contrast, it retained its significance for the middle-aged group and was also significant in all models (Supplementary Table 2). We found that e-health information seeking has no significant main effect on positive health perceptions among middle-aged adults. Conversely, it was a negative predictor in the older sample. Older adults who reported a higher average on e-health information seeking reported a lower average on both health status at the item level and the positive health perception index. The association of e-health literacy with the positive health perception index and the individual indicators, except self-reported ability to provide self-care, were significant for both the older and middle-aged sample. Furthermore, e-trust and medical satisfaction were significant predictors of the positive health perception index in the older sample.
In the older sample, when the interaction term between age and medical satisfaction was included, the relationship between e-health consumerism and the positive health perception index became nonsignificant; however, the association remained significant in the middle-aged sample. Furthermore, the nonsignificant relationship between age and the positive health perception index became significant after adding the interaction term (β = −.295, p ≤ .01) in both the older and the middle-aged sample. Finally, education had a positive influence on positive health perceptions in all models when the interaction term was included in the older sample. In contrast, in the middle-aged sample, gender was a significant negative predictor in all regression models except self-care. Similar to the full sample, when the interaction term was included, the relationship between gender and the positive health perception index decreased from β = −.117, p ≤ .01 to β = −.109, p ≤ .01.
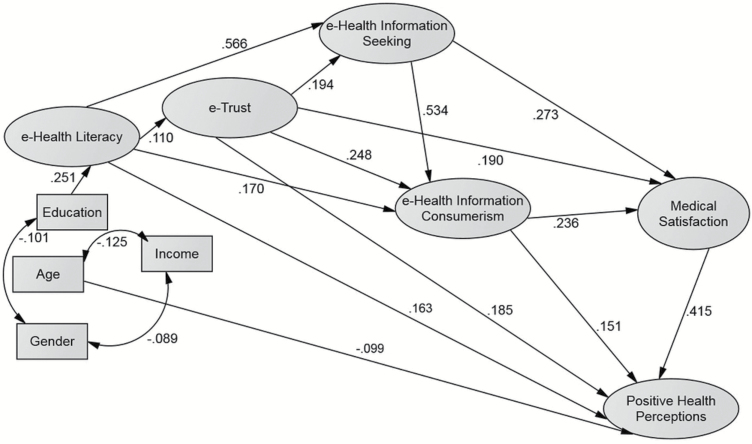
We also hypothesized significant direct effects of e-health information seeking, e-health information consumerism on positive health perceptions. Medical satisfaction was hypothesized to mediate the effect of e-health information consumerism on positive health perceptions. Additionally, we expected to find e-health information consumerism and medical satisfaction to mediate the effect of e-health information seeking on positive health perceptions. SEM analyses revealed that the hypothesized model fit the data well. Based on modification indices using a cutoff value of 10, we implemented a series of modifications (freely estimating formerly fixed parameters) to produce the best-fitting models (Byrne, 2016). We added regression paths from e-health literacy to e-health information consumerism and e-health information seeking and correlated error terms on observed indicators of e-health information consumerism and medical satisfaction and reran our analyses. As a result, we obtained the following goodness of fit indices in the full sample: χ2(499) = 35.037, df = 20, p < .05, CFI = .985, NFI = .965, RMSEA = .038, TLI = .970. The fit indices for older adults are as follows: χ2(194) = 31.575, df = 24, p > .05, CFI = .988, NFI = .952, RMSEA = .040, and TLI = .977.
Supplementary Table 3 presents standardized direct, indirect, and total effects resulting from tests of our Hypotheses (7–11) for the SEM model. Total effects include direct and indirect effects. Significant direct effects are denoted with asterisks to indicate the level of significance. Indirect effects consist of a combination of statistically significant direct paths. The direct effects of e-trust, e-health information seeking, and e-health information consumerism on medical satisfaction are significant, which in turn had a significant effect on the positive health perception index. E-health literacy, e-trust, and e-health information consumerism all exerted a significant direct effect on positive health perceptions. E-health information seeking had no significant direct effect but had a significant indirect effect on positive health perceptions through the mediating variables, e-health information consumerism, and medical satisfaction.
The SEM model for the full sample (Supplementary Table 3) revealed that e-health information seeking had the strongest total effect (β = .399, p ≤ .0001) on satisfaction with medical encounters, which, in turn had the strongest total effect on the positive health perception index (β = .415, p ≤ .0001). In other words, e-health information seeking has an indirect effect on positive health perceptions by having a direct effect on medical satisfaction. We also observed significant direct effects of e-trust on e-health consumerism (β = .248, p ≤ .001), satisfaction with medical encounters (β = .190, p ≤ .001), and positive health perceptions (β = .185, p ≤ .001). When we ran the SEM model for older adults (available upon request), we observed similarities as well as changes in some of the mediating paths from the full sample. For example, the significant direct path from e-health information consumerism to the positive health perception index becomes nonsignificant in the older sample. There is also no significant direct effect of e-health information seeking on satisfaction with medical encounters in the older sample (Supplementary Table 4). The SEM model showed that e-trust (β = .388, p ≤ .0001), followed by e-health consumerism (β = .373, p ≤ .0001), had the strongest total effects on medical satisfaction, which in turn, had the strongest total effect on the positive health perception index (β = .546, p ≤ .0001). The results also indicated that medical satisfaction has a stronger impact on positive health perceptions particularly for the older sample while e-health information consumerism has a direct effect on positive health perceptions in the full sample. Overall, the hypothesized variables had direct and indirect effects on positive health perceptions through the significant pathways (Figure 3), thus confirming our expectations as stated in Hypotheses 7 through 11. However, contrary to the hypothesized association, there is no significant direct association between e-health information seeking and the positive health perception index. In other words, we did not find support for Hypothesis 8; however, e-health information seeking exerted a significant influence via the mediating effects of e-health information consumerism and medical satisfaction. All the other paths were significant in the hypothesized directions. In the older sample, e-health information consumerism had no significant direct association with the positive health perception index.
Figure 3.
Full sample structural equation modeling. Rectangles represent observed variables; ellipses represent latent variables. Arrows represent significant pathways (p ≤ .05). Two-headed arrows represent significant correlations (p ≤ .05). Nonsignificant paths are not shown.
Discussion
As researchers expand their focus on digital health technology use among older adults, the current article adds new evidence to this emerging area of research. Prior research has indicated personal perceptions about health and aging impact a range of health outcomes among older adults (Koch-Weser, Bradshaw, Gualtieri, & Gallagher, 2010). Czaja (2017) called attention to the role that information and communication technologies can play in enhancing the well-being of older adults. Even though the age-based digital divide continues to exist, the Internet is changing the way older adults access health information by providing resources that help them locate both general health-related information, and information that is specific to their health concerns (Hong & Cho, 2017; Yang & Chen, 2015).
In this article, we build on prior research by providing insights into how proactive use of technology is associated with the subjective evaluation of health-related outcomes. Although much of the previous research has focused on younger adults, the current study demonstrates that the influence of technology use on subjective health extends to older adults. The first goal of the current study was to examine the cross-sectional relationship between e-health information seeking and the three indicators of positive health perceptions. The second goal of the study was to examine the moderating role of chronological age on the relationship between medical satisfaction and positive health perceptions. The final goal was to examine whether e-health literacy, e-trust, and e-health information consumerism were significant in the proposed association between e-health information seeking and positive health perceptions.
This study provides evidence that medical satisfaction (i.e., satisfaction with perceived changes in medical encounters) helps explain the relationship between Internet use for health-related information and health perceptions. Our findings provide insight into the ways in which information technology use affects perceived health benefits and suggests that medical satisfaction is a more powerful predictor of positive health perceptions among older respondents. In particular, the relationship between satisfaction with medical encounters and the positive health perception index, including its indicators was significantly stronger for the older adult sample as compared with the middle-aged sample. We also found that when the interaction term was included, a nonsignificant e-health information-seeking variable became a significant negative predictor of the positive health perception index in the older sample. Engaging in higher levels of e-health information seeking activity might be indicative of a greater need or attempt to provide better self-health care and improve health.
Path modeling analyses revealed a pattern of significant effects that largely parallel those from regression models. We found that even though e-health information seeking has a direct impact on medical satisfaction in the full sample, there is no direct association in the older sample. However, both e-trust and e-health consumerism predicted medical satisfaction in the older adult sample. Additionally, both e-health literacy and e-trust were found to be significant predictors of positive health perceptions among older respondents. On the other hand, e-health information consumerism had no direct effect on positive health perceptions in the older sample.
In the full sample, we did not find support for Hypothesis 1 as there was not a significant association between e-health information seeking and positive health perceptions. However, we found strong support for Hypotheses 2 and 3 as study participants who indicated greater e-health information consumerism reported higher scores on the positive health perception index, particularly greater ability to provide self-care, improved health status and health-related quality of life. Respondents who reported greater medical satisfaction also reported more positive health perceptions. We also found support for Hypothesis 6. The relationship between medical satisfaction and the positive health perception index (including the individual indicators) was significantly stronger for the older adult sample as compared with the middle-aged sample. Overall, these findings are consistent with prior research demonstrating the beneficial effects of health-related Internet use (Cotten, 2017; Hale et al., 2018; Sims et al., 2016).
In the older sample, we did not find support for Hypothesis 1, as the data confirmed that e-health information seeking was not significantly associated with the positive health perception index. We found partial support for Hypothesis 2. The OLS regression results showed a significant effect of e-health information consumerism on the positive health perception index. However, SEM analyses, which corrects for measurement errors and provides more reliable coefficient estimates than regression models (Byrne, 2016), revealed that e-health information consumerism had no significant direct effect. Yet, e-health information consumerism exerted an indirect effect through medical satisfaction. The pre-1980 context of medical culture was characterized by heightened physician authority and the patient’s obligation to comply with the medical advice and treatment prescribed by the physician; a patient was not to pick and choose a treatment nor act like a consumer selecting a treatment according to personal preference (Spencer, 2018). This socialization of the older generation of adults into the sick role, which taught people to be reliant on doctors and not to exercise autonomy in managing personal health, can help us to better understand this differential result in the older adult sample compared with the full sample, which included middle-aged respondents (Kahana & Kahana, 2003; Parsons, 1975).
We found evidence that medical satisfaction was a significant predictor of positive health perceptions, with age moderating this association (Hypotheses 3 and 6). Both e-trust and e-health literacy have a significant positive impact on positive health perceptions (Hypotheses 4 and 5). Respondents, including those in the older sample, who reported greater e-health literacy by engaging in the evaluation of online information and greater e-trust in online health information sources reported the ability to provide better self-care, improved health quality of life, and better health status as a result of information gathering. Lastly, we found gender to be a negative predictor for the positive health perception index in the full sample, which is consistent with previous research (Ybarra & Suman, 2008). Women’s higher level of engagement with online health or medical information resources allows them to decide on the content and depth of information collected (Seckin, 2014; Stern, Cotten, & Drentea, 2012). They are more likely to utilize online information, possibly because they tend to experience more chronic health conditions, functional limitations, and utilize health care services, all of which increase their informational needs (Bottorff et al., 2007; Kim, Lee, Christensen, & Merighi, 2017). Interestingly, women are less likely to be satisfied than men with Internet-based health information, particularly when different sources conflict with each other (Ybarra & Suman, 2008). This may help to explain the negative association we found in our study. However, as reported in the results section, it was not a significant predictor in the older sample, which may be due to reduced variation in the age variable in the older sample. Alternatively, gender-based differences may diminish later in life reducing the statistical power of the gender variable to detect a differential effect on subjective perceptions of health, particularly as both men and women use the Internet for health purposes.
Our results should also be interpreted within the context of the study’s limitations. The theorized direction of relationships as portrayed in our conceptual model can only be confirmed through use of a longitudinal research design. An alternative interpretation of our findings could be that individuals with more positive health perceptions engage in more Internet use for health information to promote and/or maintain their health (Feng & Xie, 2015; Goldner, 2006). However, most previous research supports the theoretical approach taken here that use of the Internet affects health perceptions (Cotten, Goldner, Hale, & Drentea, 2011; Rooks, Wiltshire, Elder, BeLue, & Gary, 2012; Sassenberg & Greving, 2016).
Moreover, the age variable is likely to be confounded due to chronic and disabling conditions. We cannot determine whether the results reflect specifically age differences in health technology use and health perceptions or unaccounted differences in chronic and disabling conditions given that younger adults generally have fewer health problems than older adults. Another methodological concern is having a large number of outcome variables (as in path modeling) and, therefore, increasing the likelihood of finding effects. However, use of SEM as one of our analytical approaches increases our confidence in our results as SEM employs a latent-construct modeling strategy that tests model fit for multiple observed indicators of each latent construct while controlling for measurement error using multiple goodness of fit criteria to rule out nonsignificant and/or trivial associations (Kline, 2011).
Another concern is that individuals who never used the Internet to locate health information were excluded from the analysis which deters us from concluding whether e-health information seeking results in positive health perceptions through mediating mechanisms involved or whether people who report positive perceptions are more motivated to use the Internet for health information. Moreover, excluding people who never used the Internet to find health information may have biased the estimates. For example, a respondent may report greater trust, higher levels of health information consumerism and more positive health perceptions because she or he is already a user of health information technology. Additionally, some important predictors of health perceptions, for example, social support or having a health condition for which information was sought, were not included in the analyses. The positive health perception index captured limited dimensions of a multidimensional construct. We are also concerned about the extent to which self-reported improvement in health status or perceived ability to provide better self-care reflect actual improvement or better ability.
Despite these limitations, the present study contributes to the literature on e-health information technology use and subjective health outcomes in several novel and important ways. First, it provides additional evidence supporting the association between technology usage and health, particularly among older adults. Second, the present study examines the separate and joint impact of variables that were not previously examined together as mediating pathways. These pathways and their direct and indirect mediating mechanisms leading to positive subjective perceptions of health-related outcomes could be potential targets for intervention studies. Third, the present study illustrates the mechanisms through which age moderates the association between medical satisfaction and the positive health perception index. Fourth, this study demonstrates that e-health information-seeking and positive health perceptions have differential associations in pathway modeling depending on age (e.g., e-health information seeking not having a direct effect on medical satisfaction in the older sample) and the extent to which people report satisfaction with medical encounters.
Our findings provide evidence of the complex associations between the use of health information technology and subjective health outcomes. Invoking adaptive strategies by engaging in goal-directed, instrumental behaviors to pursue health-related goals, among which is the use of health information technology, is consistent with the selective optimization with compensation (SOC) approach to successful aging (Baltes & Baltes, 1993) and with the proactive and corrective model of successful aging developed by Kahana and Kahana (2003). As individuals use web resources to promote health maintenance and/or aid with restoration of their health, they change their roles and responsibilities from being passive patients to proactive health consumers and health care partners empowered with technology-mediated knowledge (Seckin et al., 2018). This capacity can positively affect their subjective assessments of their health and well-being as being empowered with information supports the proactive management of health (Cosco, Prina, Perales, Stephan, & Brayne, 2014; Cotten, 2017; Martin, Palmer, Rock, Gelston, & Jeste, 2015; Pace & Grenier, 2017; Pruchno & Carr, 2017; Rowe & Kahn, 2015).
The present study addresses a timely and important subject and contributes to our understanding of the potential benefit that information and communication technologies have for the health and well-being of computer-connected aging adults. Our results underscore the importance of proactive involvement in health management through information gathering. As computer-literate baby boomers age into older adults, they will utilize the opportunities offered by digital technologies to find information they need to manage their health. Given that relatively few recent studies have examined the role of information technology in the context of subjectively reported health-related outcomes (Baskin & Davey, 2015; Martin et al., 2015), we believe our study is a novel contribution to the research on technology use of middle-aged and older adults.
Additionally, the current study makes a novel contribution to emerging research that focuses on the impact of information technology on subjective health perceptions by illustrating its conceptual link to the successful aging 2.0 framework (Griffith, Cornish, Bergner, Bruce, & Beech, 2018; Mintus-Latham, Vowels, & Huskins, 2018). The successful aging model highlights the process of adaptation to health challenges as described in the selective optimization with compensation model (Baltes & Baltes, 1993). People with a higher sense of control over personal health through information acquisition and/or better self-care practices have significantly slower rates of health-related decline over time (Kempen, Ranchor, van Sonderen, van Jaarsveld, & Sanderman, 2006; Hicks & Siedlecki, 2017). Obtaining health information from online sources is a proactive behavioral adaptation to health challenges that increase in later life (Cotten, Ford, Ford, & Hale, 2012; Drentea, Goldner, Cotten, & Hale, 2008; Stowe & Cooney, 2015). This represents an agentic approach of engagement in positive health behaviors along with a greater sense of individual responsibility for self-care (Sassenberg & Greving, 2016). However, more research is needed to understand the complex relationship between health information technology and subjective health outcomes. Interventions need to be developed to ensure that older adults who are at-risk of being left out of the digital world of health information and communication do not fall victim to a digital health divide. Access to Internet-based information technologies has important implications for health care (Ignatow & Robinson, 2017; Robinson et al., 2015). Evidence shows that differential access to digital information technologies may exacerbate digital health disparities, particularly for older adults (Neter, Brainin, & Baron-Epel, 2018).
The critical translational significance of our study for future research is how to optimize the informed use of health information technologies, such as the Internet, tablet PCs, and smartphones among older individuals, particularly those over the age of 60, who have been relatively later adopters of technologies. Addressing health care needs with technology in the broader context of aging is a fruitful area of research that can play an important role in maintaining and promoting health and well-being. Educational interventions can potentially counteract the cumulative disadvantage that limits health literacy skills and help overcome digital health disparities (Chiu & Liu, 2017; Diviani, van den Putte, Giani, & van Weert, 2015; Paige, Miller, Krieger, Stellefson, & Cheong, 2018; Sudbury-Riley, FitzPatrick, & Schulz, 2017). Developing health literacy interventions to inform the population of the tasks involved in evaluating information is a much-needed area of research with potential implications for more informed and effective self-care and health management practices outside of clinical encounters. Our results provide insight that can be used to develop educational programs to support improvement of medical encounters such as better doctor–patient communication and increased effectiveness of medical encounters. As patients become better informed of their medical conditions through e-health information seeking and e-health literacy, communication with their healthcare provider is likely to improve due to the patient’s improved ability to articulate concerns or questions to their providers.
Funding
This work is supported by the University of Maryland, Baltimore County.
Conflict of Interest
None reported.
Author Contributions
G. Seckin planned the study, performed the data analysis, and wrote the article. S. Hughes, D. Yeatts, and T. Degreve contributed to multiple revisions of the article.
Supplementary Material
References
- Anderson M., & Perrin A (2017). Tech adoption climbs among older adults Retrieved from http://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/
- Arbuckle J. L. (2010). IBM SPSS Amos 19 User’s Guide. Chicago, IL: IBM. [Google Scholar]
- Baltes P. B., & Baltes M. B (1993). Successful aging: Perspectives from the behavioral sciences. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Baskin C., & Davey C. J. (2015). Grannies, elders, and friends. aging Aboriginal women in Toronto. Journal of Gerontological Social Work, 1, 45–65. doi: 10.1080/01634372.2014.912997 [DOI] [PubMed] [Google Scholar]
- Bottorff J. L. Oliffe J. L. Halpin M. Phillips M. McLean G. & Mroz L (2008). Women and prostate cancer support groups: The gender connect?Social Science & Medicine (1982), 66, 1217–1227. doi: 10.1016/j.socscimed.2007.11.018 [DOI] [PubMed] [Google Scholar]
- Byrne B. M. (2016). Structural equation modeling with AMOS. Basic concepts, applications, and programming (3rd ed.). New York, NY: Routledge. [Google Scholar]
- Carpentieri J. D. Elliott J. Brett C. E. & Deary I. J (2017). Adapting to aging: Older people talk about their use of selection, optimization, and compensation to maximize well-being in the context of physical decline. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 351–361. doi: 10.1093/geronb/gbw132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu C. J. & Liu C. W (2017). Understanding older adult’s technology adoption and withdrawal for elderly care and education: Mixed method analysis from national survey. Journal of Medical Internet Research, 19, e374. doi: 10.2196/jmir.7401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi N. (2011). Relationship between health service use and health information technology use among older adults: Analysis of the US national health interview survey. Journal of Medical Internet Research, 13, e33. doi: 10.2196/jmir.1753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosco T. D. Prina A. M. Perales J. Stephan B. C. & Brayne C (2014). Operational definitions of successful aging: A systematic review. International Psychogeriatrics, 26, 373–381. doi: 10.1017/S1041610213002287 [DOI] [PubMed] [Google Scholar]
- Cotten S. R. (2017). Examining the roles of technology in aging and quality of life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 823–826. doi: 10.1093/geronb/gbx109 [DOI] [PubMed] [Google Scholar]
- Cotten S. R., Ford G., Ford S., & Hale T. M. (2012). Internet use and depression among older adults. Computers in Human Behavior, 28, 496–499. doi: 10.1016/j.chb.2011.10.021 [DOI] [Google Scholar]
- Cotten S. R. Goldner M. Hale T. M. & Drentea P (2011). The importance of type, amount, and timing of internet use for understanding psychological distress. Social Science Quarterly, 92, 119–139. [DOI] [PubMed] [Google Scholar]
- Craciun C. Gellert P. & Flick U (2017). Aging in precarious circumstances: Do positive views on aging make a difference?The Gerontologist, 57, 517–528. doi: 10.1093/geront/gnv135 [DOI] [PubMed] [Google Scholar]
- Czaja S. J. (2017). The role of technology in supporting social engagement among older adults. Public Policy & Aging Report, 27, 145–148. doi: 10.1093/ppar/prx034 [DOI] [Google Scholar]
- Dedding C. van Doorn R. Winkler L. & Reis R (2011). How will e-health affect patient participation in the clinic? A review of e-health studies and the current evidence for changes in the relationship between medical professionals and patients. Social Science & Medicine (1982), 72, 49–53. doi: 10.1016/j.socscimed.2010.10.017 [DOI] [PubMed] [Google Scholar]
- Diviani N. van den Putte B. Giani S. & van Weert J. C (2015). Low health literacy and evaluation of online health information: A systematic review of the literature. Journal of Medical Internet Research, 17, e112. doi: 10.2196/jmir.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drentea P., Goldner M., Cotten S., & Hale T. (2008). The association among gender, computer use, and online health searching, and mental health. Information, Communication, and Society, 11, 509–525. doi:1010.1080/13691180801999019 [Google Scholar]
- Ernsting C. Dombrowski S. U. Oedekoven M. O Sullivan J. L. Kanzler M. Kuhlmey A. & Gellert P (2017). Using smartphones and health apps to change and manage health behaviors: A population-based survey. Journal of Medical Internet Research, 19, e101. doi: 10.2196/jmir.6838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y. & Xie W (2015). Digital divide 2.0: The role of social networking sites in seeking health information online from a longitudinal perspective. Journal of Health Communication, 20, 60–68. doi: 10.1080/10810730.2014.906522 [DOI] [PubMed] [Google Scholar]
- Ferraro K. F. & Wilkinson L. R (2015). Alternative measures of self-rated health for predicting mortality among older people: Is past or future orientation more important?The Gerontologist, 55, 836–844. doi: 10.1093/geront/gnt098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gell N. M. Rosenberg D. E. Demiris G. LaCroix A. Z. & Patel K. V (2015). Patterns of technology use among older adults with and without disabilities. The Gerontologist, 55, 412–421. doi: 10.1093/geront/gnt166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldner M. (2006). Using the Internet and email for health purposes: The impact of health status. Social Science Quarterly, 87, 690–710. doi: 10.1111/j.1540-6237.2006.00404.x [DOI] [Google Scholar]
- Griffith D. M. Cornish E. K. Bergner E. M. Bruce M. A. & Beech B. M (2018). “Health is the ability to manage yourself without help”: How older African American men define health and successful aging. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 240–247. doi: 10.1093/geronb/gbx075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T. M., Chou W. Y. S., & Cotten S. R (2018). E-health: Current evidence, promises, perils, and future directions. Bingley, UK: Emerald Publishing Limited. doi: 10.1108/S2050-2060201815 [DOI] [Google Scholar]
- Hicks S. A. & Siedlecki K. L (2017). Leisure activity engagement and positive affect partially mediate the relationship between positive views on aging and physical health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 259–267. doi: 10.1093/geronb/gbw049 [DOI] [PubMed] [Google Scholar]
- Hong Y. A. & Cho J (2017). Has the digital health divide widened? Trends of health-related internet use among older adults from 2003 to 2011. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 856–863. doi: 10.1093/geronb/gbw100 [DOI] [PubMed] [Google Scholar]
- Hu X. Bell R. A. Kravitz R. L. & Orrange S (2012). The prepared patient: Information seeking of online support group members before their medical appointments. Journal of Health Communication, 17, 960–978. doi: 10.1080/10810730.2011.650828 [DOI] [PubMed] [Google Scholar]
- Hu L. T., & Bentler P. M (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Ignatow G. & Robinson L (2017). Pierre bourdieu: Theorizing the digital. Information, Communication, & Society, 20, 950–966. doi: 10.1080/1369118X.2017.1301519 [DOI] [Google Scholar]
- Kahana E., & Kahana B (2003). Contextualizing successful aging: New directions in an age-old search. In R. Settersten (Ed.), Invitation to the life course: A new look at old age (pp. 225–255). Amityville, NY: Baywood Publishing Company. [Google Scholar]
- Kahana E. Kelley-Moore J. & Kahana B (2012). Proactive aging: A longitudinal study of stress, resources, agency, and well-being in late life. Aging & Mental Health, 16, 438–451. doi: 10.1080/13607863.2011.644519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempen G. I., Ranchor A.V., van Sonderen E., van Jaarsveld C.H.M., & Sanderman R. (2006). Risk and protective factors of different functional trajectories in older persons: are these the same?The Journals of Gerontology. Series B: Psychological Sciences and Social Sciences, 61, 95–101. doi: 10.1093/geronb/61.2.P.95 [DOI] [PubMed] [Google Scholar]
- Kenny D. A. (2015). Measuring model fit Retrieved from http://davidakenny.net/cm/fit.htm
- Kim J. Lee H. Y. Christensen M. C. & Merighi J. R (2017). Technology access and use, and their associations with social engagement among older adults: Do women and men differ?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 836–845. doi: 10.1093/geronb/gbw123 [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2011). Principles and practice of structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Koch-Weser S., Bradshaw Y. S., Gualtieri L., & Gallagher S. S (2010). The internet as a health information source: Findings from the 2007 Health Information National Trends Survey and implications for health communication. Journal of Health Communication, 15(Suppl. 3), 279–293. doi: 10.1080/10810730.2010.522700 [DOI] [PubMed] [Google Scholar]
- Mintus-Latham K. Vowels A. & Huskins K (2018). Healthy aging among older black and white men: What is the role of mastery?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73, 248–257. doi: 10.1093/geronb/gbx105 [DOI] [PubMed] [Google Scholar]
- Martin A. S. Palmer B. W. Rock D. Gelston C. V. & Jeste D. V (2015). Associations of self-perceived successful aging in young-old versus old-old adults. International Psychogeriatrics, 27, 601–609. doi: 10.1017/S104161021400221X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neter E., Brainin E., & Baron-Epel O (2018). The third digital divide in the health domain: Is internet use for health purposes associated with health benefits?Hale T. M., Chou W. Y. S., & S. R. Cotten (Eds.), eHealth: Current evidence, promises, perils, and future directions. Studies in media and communications (Vol. 15; pp. 153–175). Bingley, UK: Emerald Publishing Limited. doi: 10.1108/S2050-206020180000015011 [DOI] [Google Scholar]
- Pace J. E. & Grenier A (2017). Expanding the circle of knowledge: Reconceptualizing successful aging among North American older indigenous peoples. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 248–258. doi: 10.1093/geronb/gbw128 [DOI] [PubMed] [Google Scholar]
- Paige S. R. Krieger J. L. & Stellefson M. L (2017). The influence of ehealth literacy on perceived trust in online health communication channels and sources. Journal of Health Communication, 22, 53–65. doi: 10.1080/10810730.2016.1250846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paige S. R., Miller M. D., Krieger J. L., Stellefson M., & Cheong J. W (2018). Electronic health literacy across the lifespan: Measurement Invariance Study. Journal of Medical Internet Research, 20, e10434. doi: 10.2196/jmir.10434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons T. (1975). The sick role and the role of the physician reconsidered. The Milbank Memorial Fund Quarterly. Health and Society, 53, 257–278. Retrieved from https://www.jstor.org/stable/3349493 [PubMed] [Google Scholar]
- Pruchno R. & Carr D (2017). Successful aging 2.0: Resilience and beyond. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 201–203. doi: 10.1093/geronb/gbw214 [DOI] [PubMed] [Google Scholar]
- Robinson L., Cotton S. R., Ono H., Quan-Haase A., Mesch G., Chen W., & Schulz J (2015). Digital inequalities and why they matter. Information, Communication, and Society, 18, 569–582. doi: 10.1080/1369118X.2015.1012532 [DOI] [Google Scholar]
- Rooks R. N. Wiltshire J. C. Elder K. BeLue R. & Gary L. C (2012). Health information seeking and use outside of the medical encounter: Is it associated with race and ethnicity?Social Science & Medicine (1982), 74, 176–184. doi: 10.1016/j.socscimed.2011.09.040 [DOI] [PubMed] [Google Scholar]
- Rowe J. W. & Kahn R. L (2015). Successful aging 2.0: Conceptual expansions for the 21st century. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 593–596. doi: 10.1093/geronb/gbv025 [DOI] [PubMed] [Google Scholar]
- Sassenberg K. & Greving H (2016). Internet searching about disease elicits a positive perception of own health when severity of illness is high: A longitudinal questionnaire study. Journal of Medical Internet Research, 18, e56. doi: 10.2196/jmir.5140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sbaffi L. & Rowley J (2017). Trust and credibility in web-based health information: A review and agenda for future research. Journal of Medical Internet Research, 19, e218. doi: 10.2196/jmir.7579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R. Wahl H. W. Matthews J. T. De Vito Dabbs A. Beach S. R. & Czaja S. J (2015). Advancing the aging and technology agenda in gerontology. The Gerontologist, 55, 724–734. doi: 10.1093/geront/gnu071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seckin G. (2014). Online health information seeking and gender. In Cockerham W. C., Dingwall R., & S. R. Quah (Eds.), The Wiley Blackwell encyclopedia of health, illness, behavior, and society. Oxford, UK: Blackwell Publishing Ltd. doi: 10.1002/9781118410868.wbehibs176 [DOI] [Google Scholar]
- Seckin G., Hughes S., Hudson C., Laljer D., & Yeatts D (2018). Positive impacts of online health information seeking on health perceptions. In Hale T. M., Chou W. Y. S., & S. R. Cotten (Eds.), eHealth: Current evidence, promises, perils, and future directions. Studies in media and communications (Vol. 15; pp. 205–240). Bingley, UK: Emerald Publishing Limited. doi: 10.1108/S2050-206020180000015010 [DOI] [Google Scholar]
- Seçkin G. Yeatts D. Hughes S. Hudson C. & Bell V (2016). Being an informed consumer of health information and assessment of electronic health literacy in a national sample of internet users: Validity and reliability of the e-HLS instrument. Journal of Medical Internet Research, 18, e161. doi: 10.2196/jmir.5496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims T., Reed A. E., & Carr D. C (2016). Information and communication technology use is related to higher well-being among the oldest-old, The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72, 761–770. doi: 10.1093/geronb/gbw130 [DOI] [PubMed] [Google Scholar]
- Sørensen K. Van den Broucke S. Fullam J. Doyle G. Pelikan J. Slonska Z.…Brand H; (HLS-EU) Consortium Health Literacy Project European (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80. doi: 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanakis E. G. Chiarugi F. Kouroubali A. Spat S. Beck P. Asanin S.…Thestrup J (2012). Diabetes management using modern information and communication technologies and new care models. Interactive Journal of Medical Research, 1, e8. doi: 10.2196/ijmr.2193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer K. L. (2018). Transforming patient compliance research in an era of biomedicalization. Journal of Health and Social Behavior, 59, 170–184. doi: 10.1177/0022146518756860 [DOI] [PubMed] [Google Scholar]
- Steiger J. H. (2007). Understanding the limitations of global fit assessment in structural equation modeling. Personality and Individual Differences, 42, 893–898. doi: 10.1016/j.paid.2006.09.017 [DOI] [Google Scholar]
- Stellefson M. Chaney B. Barry A. E. Chavarria E. Tennant B. Walsh-Childers K.…Zagora J (2013). Web 2.0 chronic disease self-management for older adults: A systematic review. Journal of Medical Internet Research, 15, e35. doi: 10.2196/jmir.2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern M. J., Cotten S. R., & Drentea P (2012). The separate spheres of online health: Gender, parenting, and online health information searching in the information age. Journal of Family Issues, 33, 1324–1350. doi: 10.1177/0192513X11425459. [DOI] [Google Scholar]
- Stowe J. D., & Cooney T. M. (2015). Examining Rowe and Kahn’s concept of successful aging: importance of taking a life course perspective. The Gerontologist, 55, 43–50. doi: 10.1093/geront/gnu055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudbury-Riley L. FitzPatrick M. & Schulz P. J (2017). Exploring the measurement properties of the ehealth literacy scale (eheals) among baby boomers: A multinational test of measurement invariance. Journal of Medical Internet Research, 19, e53. doi: 10.2196/jmir.5998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan S. S. & Goonawardene N (2017). Internet health information seeking and the patient–physician relationship: A systematic review. Journal of Medical Internet Research, 19, e9. doi: 10.2196/jmir.5729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennant B. Stellefson M. Dodd V. Chaney B. Chaney D. Paige S. & Alber J (2015). Ehealth literacy and web 2.0 health information seeking behaviors among baby boomers and older adults. Journal of Medical Internet Research, 17, e70. doi: 10.2196/jmir.3992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thai C. L., Gaysynsky A., Falisi A., Chou W. S., Blake K., & Hesse B. W (2018). Trust in health information sources and channels, then and now: Evidence from the Health Information National Trends Survey (2005–2013). In Hale T. M., Chou W. S., & S. R. Cotten (Eds.), eHealth: Current evidence, promises, perils and future directions. Studies in media and communications (Vol. 15; pp. 43–67). Bingley, UK: Emerald Publishing Limited. doi: 10.1108/S2050-206020180000015002 [DOI] [Google Scholar]
- Townsend A. Leese J. Adam P. McDonald M. Li L. C. Kerr S. & Backman C. L (2015). ehealth, participatory medicine, and ethical care: A focus group study of patients’ and health care providers’ use of health-related internet information. Journal of Medical Internet Research, 17, e155. doi: 10.2196/jmir.3792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley E. Popham F. & Benzeval M (2016). Comparison of the Rowe-Kahn model of successful aging with self-rated health and life satisfaction: The West of Scotland Twenty-07 Prospective Cohort Study. The Gerontologist, 56, 1082–1092. doi: 10.1093/geront/gnv054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y. T. & Chen B (2015). Web accessibility for older adults: A comparative analysis of disability laws. The Gerontologist, 55, 854–864. doi: 10.1093/geront/gnv057 [DOI] [PubMed] [Google Scholar]
- Ybarra M., & Suman M (2008). Reasons, assessments and actions taken: Sex and age differences in uses of internet health information. Health Education Research, 23, 512–521. doi: 10.1093/her/cyl062 [DOI] [PubMed] [Google Scholar]
- Young Y., Frick K. D., & Phelan E. A (2009). Can successful aging and chronic illness coexist in the same individual? A multidimensional concept of successful aging. Journal of the American Medical Directors Association, 10, 87–92. doi: 10.1016/j.jamda.2008.11.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.