ABSTRACT
Surgical treatment of hip dysplasia by arthroscopic procedures remains controversial. The aim of this study was to compare outcomes of periacetabular osteotomy (PAO) after failed hip arthroscopy to a matched-control group without previous arthroscopy. Fifty-two patients who underwent PAO after failed hip arthroscopy were matched to two subjects without arthroscopy based on age, sex, BMI and radiographic severity. Pre- and post-operative patient self-reported outcomes and radiographic parameters were compared at minimum 1-year follow-up. Prior to PAO the failed hip arthroscopy group exhibited lower modified Harris hip scores (mHHS; 57 versus 62; P = 0.04), WOMAC (59.9 versus 66.3; P = 0.08), UCLA activity (5 versus 7; P = 0.001) and SF12 physical scores (34 versus 40; P = 0.001) compared with the non-arthroscopy group. At minimum 1-year follow-up, the failed hip arthroscopy group had lower mHHS (78 versus 87; P = 0.003); worse WOMAC (84.1 versus 90.8; P = 0.02) and SF-12 physical component (46 versus 50; P = 0.02) with similar UCLA (7 versus 8; P = 0.21) compared with the non-arthroscopy group. No differences were detected regarding radiographic parameters or in patient-reported outcomes from preoperative to follow up. PAO achieved the desired radiographic correction and significant improvement in pain and function after a failed previous hip arthroscopy, however, the patient-reported outcomes were inferior to those of PAO without previous failed arthroscopy.
INTRODUCTION
Acetabular dysplasia is characterized by inadequate femoral head coverage by the acetabulum, which results in abnormal mechanics and potential labral and cartilage damage [1, 2]. Isolated hip arthroscopy has been suggested for the treatment of labral pathology, FAI and capsular laxity in the setting of mild hip dysplasia [3–12]. However, because previous studies reported conflicting results, the role of an isolated hip arthroscopy for the treatment of hip dysplasia remains controversial [3–11, 13–21]. While few studies [3–5, 7, 9, 12] report short-term improvement in pain and function after hip arthroscopy for patients with borderline dysplasia, others report inferior results and high failure rates (around 30%) in patients with mild-to-moderate dysplasia [6, 7, 10, 20] with an additional risk of potential iatrogenic instability and rapid progression of osteoarthritis [18, 20, 22–24].
A recent prospective study investigating hip arthroscopy failures suggested that amongst patients who did not improve with hip arthroscopy, 24% were diagnosed with acetabular dysplasia and underwent a periacetabular osteotomy (PAO) for definitive treatment [21]. PAO is a well-recognized treatment for symptomatic acetabular dysplasia with supportive literature regarding its safety [25] and good clinical outcomes relative to improved symptoms, function and preservation of the native hip at the intermediate [26] and over 20 [27] and 30 years [28] after surgery. However, there is limited literature [15, 16] reporting outcomes of patients undergoing PAO after a previous failed hip arthroscopy.
The purpose of this study was to compare patient-reported outcomes and radiographic correction in a cohort of patients with symptomatic acetabular dysplasia who underwent PAO after failed hip arthroscopy to a matched control cohort of patients who underwent PAO as an index procedure without previous hip arthroscopy.
MATERIALS AND METHODS
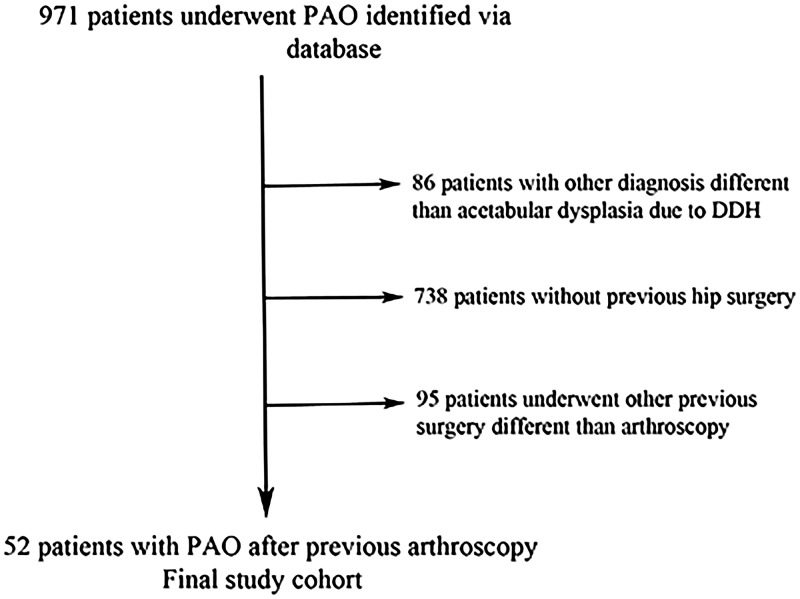
After approval by the institutional review board at the participating institutions, a query of the Academic Network for Conservational Hip Outcomes Research (ANCHOR) database identified 971 patients who underwent a PAO over a 4-year period. ANCHOR is a multicenter research group that has collected prospective longitudinal data for hip preservation surgeries including PAO. Inclusion criteria for the study group were patients who underwent PAO for the treatment of residual or persistent pain after an ipsilateral hip arthroscopy and the diagnosis of acetabular dysplasia associated with developmental dysplasia of the hip (DDH) based on lateral center-edge angle (LCEA) of Wiberg [29] lower than 25° or acetabular roof inclination of Tönnis [30] greater than 10°. Exclusion criteria were diagnosis different than DDH and previous open surgeries. Eight hundred and eighty-five patients underwent PAO for acetabular dysplasia associated with DDH and 147 patients underwent previous surgery. Our final study cohort consisted of 52 patients who underwent PAO for the treatment of symptomatic acetabular dysplasia after previous failed hip arthroscopy (Fig. 1).
Fig. 1.
Schematic demonstration of the study group sample.
The ANCHOR database was searched for control subjects who underwent PAO as an index procedure with the following inclusion criteria: (i) diagnosis of acetabular dysplasia due to DDH; (ii) no previous hip surgery; (iii) no concurrent femoral osteotomy procedure. Each patient with PAO after failed hip arthroscopy was matched with two control subjects (no previous arthroscopy) using a modified nearest neighbor approach based on sex, age, BMI and LCEA. Subjects in the previous arthroscopy group were stratified in blocks based on sex. Controls were assigned to an appropriate block and control subjects closest in age (±2 years) and body mass index (BMI; kg/m2; ±5 units) were matched together with each patient in the previous arthroscopy group. Finally, two control subjects with the closest LCEA to the study patient were selected if more than two potential subjects were identified. Minimum follow-up was 12 months and was achieved for all subjects enrolled in the study. For patients in the failed hip arthroscopy group, PAO was performed after a mean of 29.6 months (±21.4 months) following the initial hip arthroscopy procedure.
Surgery was performed according to a previous described technique [31, 32]. At the time of PAO 25 (48%) patients in the previous arthroscopy group underwent an arthrotomy and 15 (33%) underwent a concomitant arthroscopy. Femoral head neck osteochondroplasty was performed in 29 (56%) patients, the labrum was repaired in 7 (14%) patients and debrided in 9 (17%) patients. In the non-previous arthroscopy group, 55 (53%) patients underwent an open arthrotomy at the time of PAO, while 25 (24%) patients underwent a concomitant hip arthroscopy. Femoral head neck osteochondroplasty was performed in 59 (57%) patients; labral repair in 9 (9%) and labral debridement in 10 (10%) patients.
Clinical outcome scores were prospectively collected before surgery and at minimum 1-year follow-up using the modified Harris hip score (mHHS) [33], the WOMAC [34], the 12-Item Short-form healthy survey (SF-12 including physical and mental components) [35] and the UCLA activity scores [36]. At latest follow-up, patients were considered to have an excellent mHHS outcome if the scores were higher than 90 points [37].
Anteroposterior (AP) pelvic and false profile [38] radiographs were assessed preoperative and at most recent follow-up visit by measurements of the LCEA of Wiberg [29], acetabular index of Tönnis [30] and anterior center-edge angle (ACEA) [38]. Osteoarthritis was classified on AP pelvic radiographs using the Tönnis classification [30]. Radiographs were assessed by the same orthopedic surgeon not involved in the clinical care of the patients. The intra-class correlation coefficients (ICCs) for intra-observer variability in a radiographic performed study of this same patient group was reported as being between 0.82 and 1.0, and the inter-observer reliability for LCEA between 0.42 and 0.92, Tönnis angle between 0.45 and 0.85, and ACEA from 0.55 to 0.88 [39].
Statistical analysis
Patient characteristics were summarized using mean and standard deviation for continuous characteristics and by frequency and percent for categorical characteristics. Patient-reported outcomes and radiographic measurements were summarized and compared across treatment groups at baseline and at most-recent follow-up. Continuous measurements were compared at baseline and follow-up using Student’s t-tests while binary characteristics where compared using a χ2 test and ordinal characteristics using the Cochran–Armitage test for trends. Change in patient-reported outcomes and radiographic measurements was analyzed across treatment groups using linear mixed model analysis. Modeling controlled for the matched design of the study and for repeated measures on the same subject. All tests were two-sided and P-values less than 0.05 were considered significant.
RESULTS
There were a total of 52 patients in the previous failed arthroscopy group who were matched to 104 patients treated with PAO without previous arthroscopy. Mean patient age at time of PAO in each group was 25 years (P = 0.93) on average at PAO, with average BMI of 24 (±4) (P = 0.74). Each cohort was 6% male (P = 1.00) (Table I). The arthroscopy cohort was followed for a median of 1.8 years (range 1–5 years) and the non-arthroscopy cohort for a median of 2.1 years (range 1–7 years) (P = 0.01).
Table I.
Baseline characteristics by cohort
| Arthroscopy(n = 52) |
No arthroscopy (n = 104) |
P | |
|---|---|---|---|
| Characteristic | Mean±SD | Mean±SD | |
| Demographics | |||
| Age | 24.6±7.29 | 24.8±7.80 | 0.93 |
| Gender | 3 (6%) | 6 (6%) | 1.00 |
| BMI | 23.9±4.44 | 23.6±3.82 | 0.75 |
| Preoperative measurements | |||
| Radiographic measurements | |||
| Tönnis classification | |||
| 0 | 0 (0%) | 1 (1%) | 0.11 |
| 1 | 35 (67%) | 56 (54%) | |
| 2 | 17 (33%) | 41 (40%) | |
| 3 | 0 (0%) | 4 (4%) | |
| 4 | 0 (0%) | 1 (1%) | |
| LCEA (°) | 15.6±8.77 | 15.0±6.66 | 0.68 |
| LCEA/DDH category | |||
| Mild (>15) | 47 (90%) | 93 (90%) | 1.00 |
| Moderate (5–15) | 0 (0%) | 0 (0%) | |
| Severe (<5) | 5 (10%) | 10 (10%) | |
| ACEA (°) | 16.3±9.51 | 13.5±9.29 | 0.11 |
| Acetabular index | 15.8±5.74 | 17.2±6.42 | 0.17 |
| Patient-reported outcomes | |||
| Modified Harris hip score | 57.0±15.64 | 62.3±13.81 | 0.04 |
| UCLA activity score | 5.1±2.57 | 6.7±2.68 | 0.001 |
| WOMAC pain | 53.5±20.21 | 60.5±19.78 | 0.04 |
| WOMAC stiffness | 57.0±26.13 | 58.5±23.84 | 0.72 |
| WOMAC physical | 61.1±23.47 | 68.6±18.92 | 0.06 |
| WOMAC total | 59.9±21.67 | 66.3±18.35 | 0.08 |
| SF12 PCS | 34.2±9.99 | 40.1±10.52 | 0.001 |
| SF12 MCS | 52.2±10.62 | 52.0±9.73 | 0.92 |
At baseline before PAO the patients who underwent PAO after failed hip arthroscopy exhibited worse pain, function, and quality of life and lower level of physical activity as measured by lower mHHS (57 versus 62; P = 0.04), lower WOMAC pain scores (53.5 versus 60.5; P = 0.04), lower SF12 physical component scores (34 versus 40; P = 0.001) and lower UCLA activity scores (5 versus 7; P = 0.001) compared with the non-previous arthroscopy cohort (Table I). At the most recent follow-up, patients in the previous failed arthroscopy group had persistent lower mHHS (78 versus 87; P = 0.003) including a lower proportion of patients with an excellent (mHHS > 90) mHHS outcome (31% versus 54%; P = 0.01). The WOMAC pain scores (P = 0.01) and the SF12 physical component scores were also lower (P = 0.02) in the previous failed arthroscopy group although no difference was observed for the UCLA activities scores (P = 0.21) (Table II). No difference was detected across the two groups with respect to the magnitude of change in the patient-reported outcomes from preoperative to most-recent follow-up (Table III).
Table II.
Post-operative outcome measurements
| Arthroscopy (n = 52) |
No arthroscopy (n = 104) |
P | |
|---|---|---|---|
| Outcome | Mean ± SD | Mean±SD | |
| Radiographic measurements | |||
| Tönnis classification | |||
| 0 | 0 (0%) | 0 (0%) | 0.45 |
| 1 | 24 (53%) | 51 (61%) | |
| 2 | 18 (40%) | 27 (33%) | |
| 3 | 3 (7%) | 5 (6%) | |
| 4 | 0 (0%) | 0 (0%) | |
| LCEA (°) | 30.8±7.62 | 30.6±6.34 | 0.86 |
| ACEA (°) | 35.9±9.84 | 31.6±10.57 | 0.03 |
| Acetabular index | 4.3±4.24 | 4.3±4.67 | 0.95 |
| Patient-reported outcomes | |||
| Modified Harris hip score | 77.9±17.88 | 86.7±13.82 | 0.003 |
| >80 | 24 (46%) | 77 (74%) | 0.001 |
| >90 | 16 (31%) | 56 (54%) | 0.01 |
| UCLA activity score | 7.1±2.40 | 7.6±2.13 | 0.21 |
| WOMAC pain | 80.1±20.67 | 89.6±14.62 | 0.01 |
| WOMAC stiffness | 76.8±20.79 | 83.8±16.60 | 0.046 |
| WOMAC physical | 85.5±17.43 | 91.9±13.02 | 0.03 |
| WOMAC total | 84.1±17.14 | 90.8±13.06 | 0.02 |
| SF12 PCS | 46.0±10.55 | 50.1±8.85 | 0.02 |
| SF12 MCS | 55.0±9.26 | 54.7±7.22 | 0.83 |
Table III.
Change in radiographic and patient-reported outcome measurements
| Arthroscopy (n = 52) |
No arthroscopy(n = 104) |
P | |||
|---|---|---|---|---|---|
| Outcome | Mean | 95% CI | Mean | 95% CI | |
| Radiographic measurements | |||||
| LCEA (°) | 28.8 | (26.4 to 31.2) | 28.2 | (26.8 to 29.6) | 0.55 |
| ACEA (°) | −11.4 | (−13.6 to 27.6) | −13.0 | (−14.5 to 28.0) | 0.32 |
| Acetabular index | 19.0 | (14.5 to 27.5) | 19.1 | (16.0 to 29.5) | 0.85 |
| Patient-reported outcomes | |||||
| Modified Harris hip score | 20.8 | (14.9 to 26.7) | 24.3 | (21.1 to 27.6) | 0.30 |
| Change >10 (freq. (%)) | 35 | (67%) | 80 | (77%) | 0.27 |
| Change >20 (freq. (%)) | 28 | (54%) | 60 | (58%) | 0.78 |
| UCLA activity score | 1.9 | (1.1 to 2.7) | 0.9 | (0.4 to 1.5) | 0.06 |
| WOMAC pain | 28.1 | (19.9 to 36.4) | 29.8 | (25.6 to 34.1) | 0.54 |
| WOMAC stiffness | 20.8 | (12.1 to 29.6) | 25.1 | (20.3 to 30.0) | 0.28 |
| WOMAC physical | 27.6 | (19 to 36.1) | 27.9 | (22.9 to 32.9) | 0.73 |
| WOMAC total | 30.1 | (21.4 to 38.9) | 28.8 | (24.0 to 38.9) | 0.95 |
| SF12 PCS | 11.9 | (8.5 to 15.2) | 10.2 | (7.9 to 12.6) | 0.42 |
| SF12 MCS | 3.0 | (0.0 to 6.0) | 2.7 | (0.7 to 4.8) | 0.95 |
Radiographic measurements obtained before PAO showed that patients in each cohort had comparable severity of acetabular dysplasia as assessed by the LCEA (P = 0.68), AI (P = 0.17) and ACEA (P = 0.11) as well as severity of hip osteoarthritis grade (P = 0.35) (Table I). At most-recent follow-up, LCEA (P = 0.86) and AI (P = 0.95) were comparable across treatment groups; however, average ACEA was slightly higher in the previous failed arthroscopy group (36 versus 32; P = 0.03) compared with the non-previous arthroscopy group (Table II). No difference in the degree of correction of acetabular dysplasia, assessed by change in the radiographic measurements were observed between the two groups. (Table III).
DISCUSSION
This study shows that PAO achieved pain, function and radiographic improvement in patients with failed hip arthroscopy with no differences across groups with respect to change in radiographic measures or in patient-reported outcomes from preoperative to follow-up. Although the improvement observed after failed hip arthroscopy supports PAO as a salvage operation, patients in the failed arthroscopy group had worse hip scores assessed by the mHHS, WOMAC, UCLA and SF-12 PCS at the most recent follow-up.
The of hip arthroscopy in the setting of acetabular dysplasia remains controversial with conflicting results regarding patient-reported outcomes improvement and proportion of surgical failure [3–11, 13–21]. A recent systematic review suggested an overall high rate of re-operation and conversion to THA [11]. Arthroscopic treatment in the setting of acetabular dysplasia achieved inferior results and had higher failure when compared with hip arthroscopy for FAI without dysplasia. [7] Fukui et al. [6] described 5/28 patients (18%) underwent conversion to THA, 2 (7%) underwent a PAO and 2 (7%) required a revision hip arthroscopy for an overall proportion of 32% failure of arthroscopic treatment of mild-to-moderate dysplasia (LCEA 15°–19°). Another study reported similar proportion of failure (9/28 patients; 32%) in patients with hip dysplasia after arthroscopic labral repair, femoral osteoplasty and capsular closure [10]. An even higher rate of failure (24 of 34 patients, 70%) was reported after hip arthroscopy when the hip capsule is not adequately closed and labrum debridement is performed instead of repair in in the setting of dysplasia [20]. Further concerns have been raised after previous reports demonstrating hip instability and progressive osteoarthritis after hip arthroscopic surgery in the setting of hip dysplasia [18, 23, 24].
Poor femoral head coverage assessed by LCEA is associated with up to three to five times higher risk of progression to osteoarthritis in population-based studies [40–42]. This is concerning because hip arthroscopy does not allow for correction of the abnormal hip mechanics in the setting of structural instability associated with inadequate femoral head coverage by a dysplastic acetabulum. At best, hip arthroscopy may allow for short-term improvement in symptoms without any evidence of long-term benefit regarding patient-reported outcomes or hip survivorship. In contrast, PAO allows biomechanical improvement by medializing and reducing cartilage stress in patients with hip dysplasia [43] and is an effective treatment of symptomatic hip dysplasia with reported survival of the native hip joint in 96% at 5-year [44], 60% at 20-year [27] follow-up and 30% at 30-year follow-up [28]. Despite lack of long-term studies supporting hip arthroscopy in the treatment of hip dysplasia, a recent prospective study reported that 24% of the patients that failed hip arthroscopy were diagnosed with acetabular dysplasia and underwent a PAO for definitive treatment [21].
To the best of our knowledge only two studies have investigated the impact of a previously failed arthroscopy on the outcomes of PAO. Jackson et al. [15] reported improvement in clinical outcomes at 2-year follow-up of a 31-year-old female who underwent concomitant arthroscopic labral repair and PAO after a failed hip arthroscopy in the setting of acetabular dysplasia. Kain et al. [16] compared 17 female patients who underwent PAO after previous failed arthroscopy to 34 patients that underwent PAO as index procedures. They reported no difference in change in the pre- and post-operative WOMAC scores between the two groups as well as no difference in the outcomes assessed before and after surgery. Although the authors suggested that failed arthroscopic treatment prior to PAO may not have an impact on the short-term outcomes after PAO, their findings should be interpreted with caution. Only 12 patients completed pre- and post-operative WOMAC scores and 3 of 17 (17%) of the patients in the failed arthroscopy group had progressed to a THA compared with only 1 (3%) patient in the non-arthroscopy group. Our data also showed improvement in patient-reported outcomes after PAO in patients who had failed previous arthroscopy and the magnitude of change in outcome scores was not different than the change in patients that underwent PAO as an index procedure. However, we found that patients who had a failed arthroscopy had worse hip function, pain and quality of life assessed by the mHHS, WOMAC and SF-12 before the PAO and at the most recent follow-up. Most importantly, the percentage of patients with an excellent clinical result (mHHS ≥90) was markedly reduced in those with a failed arthroscopy when compared with those without previous arthroscopy.
This study has limitations. First and most important there is a potential for selection bias. The reason why arthroscopy was selected as the treatment of choice in the failed arthroscopy group is not clear because most patients underwent surgery outside the centers of the ANCHOR study group. Furthermore, the lack of patient-reported outcomes and intra-operative information does not allow us to establish a baseline comparison to the group that did not undergo a hip arthroscopy. The patients undergoing PAO with a previous failed arthroscopy could potentially not have the same clinical indication or severity of dysplasia as those who underwent PAO only. We attempt to compensate this potential bias by matching patients by severity of dysplasia based on the LCEA. Second, we do not have information about all patients who may have been treated successfully with arthroscopy and to this date have not required PAO. However, our goal was not to identify proportion of success/failure of arthroscopy in the setting of dysplasia. Rather we focused on improve the understanding on a challenging clinical scenario we have seen in clinical practice: the patient with symptomatic hip dysplasia that undergoes hip arthroscopy and do not obtain the pain relief they were expecting after surgery. Third, the short-term results reported herein do not allow any comparison regarding long-term hip survivorship between the two groups. We currently follow these patients and expect to address this issue in further studies. Fourth, there may have been slight variation of PAO technique as multiple surgeons were included in the study. However, all surgeons have extensive experience with the procedure with lower reported rates of complication [25] and by including multiple surgeons our findings may be better generalized.
The long-term outcomes and hip survival of arthroscopic treatment of intra-articular pathology in the setting of acetabular dysplasia are unknown, and the proportion of early failure and reoperation appear to be higher than those after PAO even in mild dysplasia [45]. Some surgeons may offer hip arthroscopy for the treatment of labral tear in the setting of hip dysplasia based on the premise that it is a less invasive procedure and if it fails PAO could be performed later. In this study, we compared patient-reported outcomes and radiographic measurements in a cohort of patients who had undergone a previous failed hip arthroscopy to a matched cohort of patients who underwent PAO as the index procedure without prior arthroscopy. We found lower preoperative scores suggesting that patients with underlying acetabular dysplasia who do not experience improvement after hip arthroscopy have worse pain and function and lower physical activity level than patients with acetabular dysplasia undergoing PAO as the index procedure. We observed a similar magnitude of change in patient-reported outcomes between the groups suggesting that it is reasonable to consider PAO for the definitive management of patients with acetabular dysplasia that have recurrent or persistent symptoms after prior failed hip arthroscopy. However, at most recent follow-up after PAO, the clinical outcomes for the failed arthroscopy group were worse and the percentage of patients with excellent results was lower when compared with the non-arthroscopy group. Although we favor PAO for correction of the structural deformity, further studies are necessary to determine the best surgical strategy for symptomatic patients with hip instability associated with mild acetabular dysplasia (LCEA between 20° and 25°).
ACKNOWLEDGEMENTS
ANCHOR Study Group Members who contributed to this article: Paul E. Beaulé, MD, FRCSC, Young-Jo Kim, MD, PhD, Michael B. Millis, MD, David A. Podeszwa, MD, Perry L. Schoenecker, MD, Rafael J. Sierra, MD, Ernest L. Sink, MD, Daniel J. Sucato, MD, Robert T. Trousdale, MD, and Ira Zaltz, MD.
FUNDING
This work was supported in part by Award UL1RR024992 from the National Center for Research Resources (J.C.C.). It was also supported in part by the Curing Hip Disease Fund (J.C.C.), the ANCHOR Research Fund, Smith & Nephew (J.C.C.), and the NFL Charities (J.C.C.).
Footnotes
Investigation performed at Department of Orthopaedic Surgery, Washington University St. Louis.
Contributor Information
ANCHOR Study Group:
Paul E Beaulé, Young-Jo Kim, Michael B Millis, David A Podeszwa, Perry L Schoenecker, Rafael J Sierra, Ernest L Sink, Daniel J Sucato, Robert T Trousdale, and Ira Zaltz
REFERENCES
- 1. Henak CR, Abraham CL, Anderson AE. et al. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage 2014; 22: 210–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Domb BG, Lareau JM, Baydoun H. et al. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res 2014; 472: 674–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Byrd JW, Jones KS.. Hip arthroscopy in the presence of dysplasia. Arthroscopy 2003; 19: 1055–60. [DOI] [PubMed] [Google Scholar]
- 4. Domb BG, Stake CE, Lindner D. et al. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med 2013; 41: 2591–8. [DOI] [PubMed] [Google Scholar]
- 5. Fukui K, Briggs KK, Trindade CA, Philippon MJ.. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy 2015; 31: 2371–9. [DOI] [PubMed] [Google Scholar]
- 6. Fukui K, Trindade CA, Briggs KK, Philippon MJ.. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J 2015; 97-B: 1316–21. [DOI] [PubMed] [Google Scholar]
- 7. Larson CM, Ross JR, Stone RM. et al. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med 2016; 44: 447–53. [DOI] [PubMed] [Google Scholar]
- 8. Kalisvaart MM, Safran MR.. Microinstability of the hip-it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg 2015; 2: 123–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nawabi DH, Degen RM, Fields KG. et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med 2016; 44: 1017–23. [DOI] [PubMed] [Google Scholar]
- 10. Uchida S, Utsunomiya H, Mori T. et al. Clinical and radiographic predictors for worsened clinical outcomes after hip arthroscopic labral preservation and capsular closure in developmental dysplasia of the hip. Am J Sports Med 2016; 44: 28–38. [DOI] [PubMed] [Google Scholar]
- 11. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR.. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res 2016; 5: 225–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jayasekera N, Aprato A, Villar RN.. Hip arthroscopy in the presence of acetabular dysplasia. Open Orthop J 2015; 9: 185–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Domb BG, LaReau J, Redmond JM.. Combined hip arthroscopy and periacetabular osteotomy: indications, advantages, technique, and complications. Arthrosc Tech 2014; 3: e95–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Duplantier NL, McCulloch PC, Nho SJ. et al. Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthroscopy 2016; 32: 1428–34. [DOI] [PubMed] [Google Scholar]
- 15. Jackson TJ, Watson J, LaReau JM, Domb BG.. Periacetabular osteotomy and arthroscopic labral repair after failed hip arthroscopy due to iatrogenic aggravation of hip dysplasia. Knee Surg Sports Traumatol Arthrosc 2014; 22: 911–4. [DOI] [PubMed] [Google Scholar]
- 16. Kain MS, Novais EN, Vallim C. et al. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg Am 2011; 93(Suppl 2): 57–61. [DOI] [PubMed] [Google Scholar]
- 17. Kim KI, Cho YJ, Ramteke AA, Yoo MC.. Peri-acetabular rotational osteotomy with concomitant hip arthroscopy for treatment of hip dysplasia. J Bone Joint Surg Br 2011; 93: 732–7. [DOI] [PubMed] [Google Scholar]
- 18. Matsuda DK, Khatod M.. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy 2012; 28: 1738–43. [DOI] [PubMed] [Google Scholar]
- 19. McCarthy JC, Mason JB, Wardell SR.. Hip arthroscopy for acetabular dysplasia: a pipe dream? Orthopedics 1998; 21: 977–9. [DOI] [PubMed] [Google Scholar]
- 20. Parvizi J, Bican O, Bender B. et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty 2009; 24: 110–3. [DOI] [PubMed] [Google Scholar]
- 21. Ross JR, Clohisy JC, Baca G. et al. Patient and disease characteristics associated with hip arthroscopy failure in acetabular dysplasia. J Arthroplasty 2014; 29: 160–3. [DOI] [PubMed] [Google Scholar]
- 22. Bogunovic L, Gottlieb M, Pashos G. et al. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res 2013; 471: 2523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mei-Dan O, McConkey MO, Brick M.. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy 2012; 28: 440–5. [DOI] [PubMed] [Google Scholar]
- 24. Yeung M, Memon M, Simunovic N. et al. Gross instability after hip arthroscopy: an analysis of case reports evaluating surgical and patient factors. Arthroscopy 2016; 32: 1196–204.e1. [DOI] [PubMed] [Google Scholar]
- 25. Zaltz I, Baca G, Kim YJ. et al. Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg Am 2014; 96: 1967–74. [DOI] [PubMed] [Google Scholar]
- 26. Matheney T, Kim YJ, Zurakowski D. et al. Intermediate to long-term results following the bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am 2010;92(Suppl 1 Pt 2):115–29. [DOI] [PubMed] [Google Scholar]
- 27. Steppacher SD, Tannast M, Ganz R, Siebenrock KA.. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res 2008; 466: 1633–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lerch TD, Steppacher SD, Liechti EF. et al. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2016; 475: 1154–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand 1939; 83: 7–38. [Google Scholar]
- 30. Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res 1976; 119: 39–47. [PubMed] [Google Scholar]
- 31. Clohisy JC, Barrett SE, Gordon JE. et al. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am 2006; 88(Suppl 1 Pt 1):65–83. [DOI] [PubMed] [Google Scholar]
- 32. Ganz R, Klaue K, Vinh TS, Mast JW.. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 1988; (232):26–36. [PubMed] [Google Scholar]
- 33. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737–55. [PubMed] [Google Scholar]
- 34. Bellamy N, Buchanan WW, Goldsmith CH. et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988; 15: 1833–40. [PubMed] [Google Scholar]
- 35. Ware J Jr., Kosinski M, Keller SD.. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–33. [DOI] [PubMed] [Google Scholar]
- 36. Amstutz HC, Thomas BJ, Jinnah R. et al. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am 1984; 66: 228–41. [PubMed] [Google Scholar]
- 37. Byrd JW, Jones KS.. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy 2011; 27: 1379–88. [DOI] [PubMed] [Google Scholar]
- 38. Lequesne M. de S. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies.]. Rev Rhum Mal Osteoartic 1961; 28: 643–52. [PubMed] [Google Scholar]
- 39. Lehmann CL, Nepple JJ, Baca G. et al. Do fluoroscopy and postoperative radiographs correlate for periacetabular osteotomy corrections? Clin Orthop Relat Res 2012; 470: 3508–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lane NE, Lin P, Christiansen L. et al. Association of mild acetabular dysplasia with an increased risk of incident hip osteoarthritis in elderly white women: the study of osteoporotic fractures. Arthritis Rheum 2000; 43: 400.. [DOI] [PubMed] [Google Scholar]
- 41. Reijman M, Hazes JM, Pols HA. et al. Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum 2005; 52: 787–93. [DOI] [PubMed] [Google Scholar]
- 42. Agricola R, Heijboer MP, Roze RH. et al. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis Cartilage 2013; 21: 1514–21. [DOI] [PubMed] [Google Scholar]
- 43. Abraham CL, Knight SJ, Peters CL. et al. Patient-specific chondrolabral contact mechanics in patients with acetabular dysplasia following treatment with peri-acetabular osteotomy. Osteoarthritis Cartilage 2017; 25: 676–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Matheney T, Kim YJ, Zurakowski D. et al. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am 2009; 91: 2113–23. [DOI] [PubMed] [Google Scholar]
- 45. Ricciardi BF, Fields KG, Wentzel C. et al. Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int 2016; 27: 42–8. [DOI] [PubMed] [Google Scholar]