ABSTRACT
Although there are well described radiological criteria for diagnosing DDH, our experience has highlighted that a new sub-category of hips exists in which the classic radiographic characteristics for DDH may be normal but the coverage of the femoral head is compromised. The purpose of this study was to validate a simple radiographic measurement method for calculating the depth of the acetabulum in order to detect individuals with ‘low-volume’ acetabuli and under-covered femoral heads. We identified 24 patients who were suspected of having low-volume acetabuli and compared their radiographs with those of 150 patients with non-dysplastic hips. The radiographic indices measured included the lateral center-edge (CE) angle, the anterior CE angle, the femoral neck-shaft angle, the extrusion index, integrity of the Shenton’s line, the crossover sign, and ischial spine sign. We have developed a novel, but a simple method, named the ‘coverage index’ (CI) to identify the presence of a low-volume acetabulum on plain radiographs. Comparisons were made between the low-volume hips and the non-dysplastic hips. The radiographic parameters indicative of developmental dysplasia of the hip (DDH) were within normal limits in all patients with low-volume acetabuli and therefore these hips could not be classified as ‘dysplastic’ based on the traditional radiological parameters. There was no difference between the mean radius of the femoral head in two groups. The mean CI was significantly greater in the non-dysplastic group compared with the low-volume acetabula cohort (1.62 ± 0.117 in non-dysplastic group versus 1.07 ± 0.11 in low-volume hips) (P = 0.0001). Orthopaedic surgeons should be aware of a hip abnormality in which the femoral head coverage is deficient, yet all the conventional parameters for measuring coverage, including the center edge angle, are within normal limits. We have introduced a simple radiographic measurement method that may help surgeons identify these patients using the anteroposterior radiographs of the hip.
INTRODUCTION
Hip dysplasia and femoroacetabular impingement are well known as predisposing factors of secondary hip osteoarthritis [1, 2]. Increased mechanical stress on the cartilage of the hip joint due to a globally shallow acetabulum causes higher and asymmetrical forces to be transferred to the labrum and cartilage which may lead to early degenerative hip disease [3–6]. High quality anteroposterior (AP) and lateral hip radiography is the standard method for diagnosing DDH and classical radiologic signs have been described. On the AP views, lateral center-edge angle (LCEA) of <20°, Tönnis angle of >10°, valgus femoral neck-shaft angle of >135°, varus femoral neck-shaft angle of <120°, extrusion index of >25% and a broken shenton line are the classical findings of hip dysplasia [3, 7–9]. Anterior center edge angle (ACEA) of <20° in false-profile radiography is the other sign of DDH [7]. Crossover sign and ischial tuberosity prominancy are also known as classical radiographic findings of acetabular retroversion which is another subgroup of dysplasia [10] (Table I). Senior author’s experience has highlighted that a new category of hips exists in which the classic radiographic characteristics for DDH may be normal but the coverage of the femoral head is compromised. This condition is as a result of very low-volume acetabulum. The purpose of this study was to validate a simple and practical radiographic measurement method for estimating the depth of acetabulum to characterize the low-volume acetabulum and under-covered femoral head.
Table I.
Radiographic characteristic of DDH and acetabular retroversion
| AP radiograph | False profile lateral radiograph | |
|---|---|---|
| DDH | LCEA < 20°, Tönnis angle > 10°, valgus femoral neck-shaft angle >135°, varus femoral neck-shaft angle <120°, extrusion index >25%, broken shenton line | ACEA < 20 |
| Acetabular retroversion | Crossover sign, ischial tuberosity prominence | NA |
LCEA, lateral center-edge angle; ACEA, anterior center-edge angle; NA, not applicable.
METHODS
Upon IRB approval, by using our institutional database over 1000 who had undergone hip joint preservation surgery, we identified 24 individuals who were suspected of having low-volume acetabulum and compared their radiographs with a control group of 150 patients with non-dysplastic hips. All cases had well-centered, high-quality AP and false profile view radiographs of the pelvic and affected hip. All radiographs were calibrated and taken in the supine position. We measured all radiographic indices of DDH and retroversion which are categorized in Table I. We then measured a novel but simple radiologic index named ‘coverage index’ (CI) on AP radiographs of all cases to identify the difference of femoral head coverage in the two groups. To determine the CI the following is performed (Fig. 1). After determining the center of femoral head a line was drawn from this point which connected the anterior wall border of the acetabulum to the fovea in the femoral head (Distance A). A second line was then drawn from the posterior wall border of the acetabulum to the fovea in line with the center of the femoral head (Distance P). Distance A was added to Distance P and divided by the radius of the femoral head therefore giving the CI (CI = A + P/R). Comparisons were made between the low-volume hips and the non-dysplastic hips. A comparison between non-dysplastic and low-volume hip is shown in Fig. 2. All measurements were done by two orthopedic surgeons. Analysis of the data demonstrated very good kappa levels (>0.81) for inter-observer reliability.
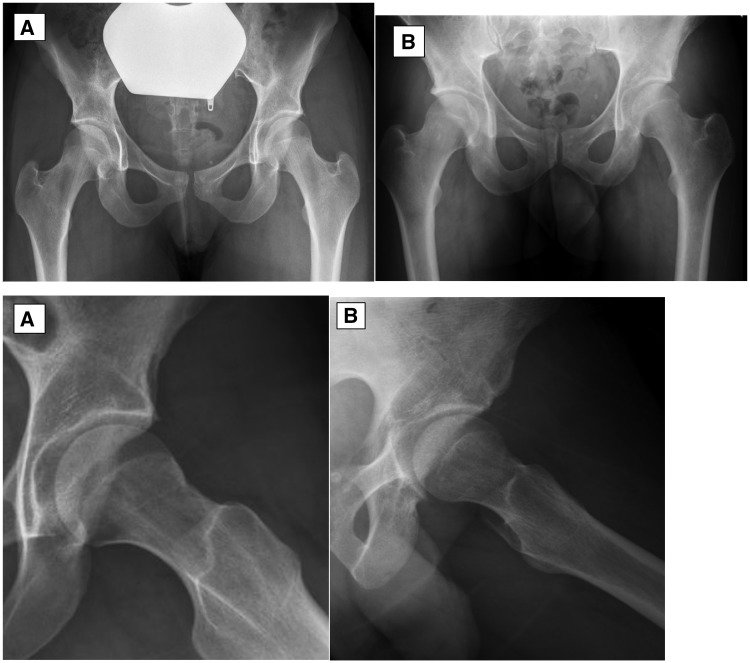
Fig. 1.
AP radiograph of a low-volume hip. A, black arrow; P, blue arrow; R, orange arrow. CI=A + P/R.
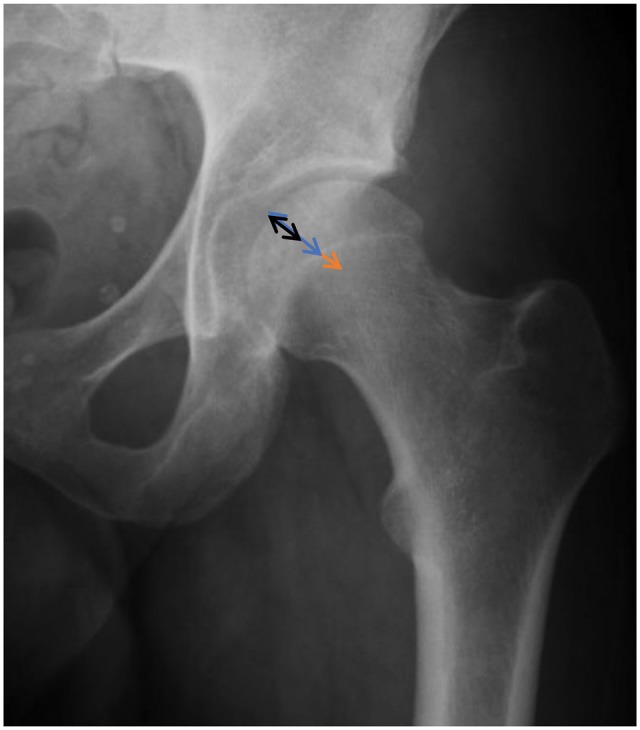
Fig. 2.
(A) AP and lateral view of non-dysplastic hip with all normal measured parameters of dysplasia and normal acetabular coverage [CI (left hip)=1.59], (B) AP and lateral view of low-volume hip with normal parameters of dysplasia [CI (left hip)=1.08].
Statistics
Inter-observer reliability for the two surgeons was determined Cohen’s (1960) Kappa statistic for dichotomous ratings with two judges [11]. Data are presented as mean, minimum, and maximum values. The Student t test was used to compare the continuous variables. All statistical analyses were performed with the use of R 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria). An alpha level of 0.05 was used to determine significance.
RESULTS
All DDH and retroversion parameters were found to be within normal limits in both groups of non-dysplastic and low-volume hips. There was no statistically significant difference between the mean radius of the femoral head in two groups of non-dysplastic (26.51 ± 2.67 mm) and low-volume hips (27.62 ± 3.25 mm). The mean Distance A was 28.7 ± 3.5 mm in non-dysplastic group and 19.2 ± 3.1 mm in low-volume hips (P = 0.00005). The mean Distance P was 14.1 ± 2.6 mm in the non-dysplastic cases and 10.7 ± 3.3 mm in the low-volume group (P = 0.0002). The mean CI was significantly greater in the non-dysplastic group compared with the low-volume acetabula cohort (1.62 ± 0.117 in non-dysplastic group versus 1.07 ± 0.11 in low-volume hips; P = 0.0001) (Table II).
Table II.
Mean, minimum, maximum value of A, P, R distances and CI in non-dysplastic and low-volume hips
| Minimum | Maximum | Mean | SD | P-value | |
|---|---|---|---|---|---|
| R distance in non-dysplastic group | 20.4 mm | 33.3 mm | 26.51 mm | 2.67 mm | 0.201 |
| R distance in low-volume hips | 23.2 mm | 33.6 mm | 27.62 mm | 3.25 mm | 0.201 |
| A distance in non-dysplastic group | 9.7 mm | 23.9 mm | 28.7 mm | 3.5 mm | 0.00005 |
| A distance in low-volume hips | 6.7 mm | 19.5 mm | 19.2 mm | 3.1 mm | 0.00005 |
| P distance in non-dysplastic group | 21.3 mm | 36.4 mm | 14.1 mm | 2.6 mm | 0.0002 |
| P distance in low-volume hips | 14.7 mm | 24.7 mm | 10.7 mm | 3.3 mm | 0.0002 |
| CI (non-dysplastic hips) | 1.36 | 1.83 | 1.62 | 0.117 | 0.0001 |
| CI (low-volume hips) | 0.85 | 1.24 | 1.07 | 0.11 | 0.0001 |
DISCUSSION
These results of this study suggest that there is a new category of patients who do not meet the conventional radiographic criteria of hip dysplasia but still have low coverage of their femoral heads. The current diagnosis of hip dysplasia is based on described radiographic parameters [12] and advanced imaging techniques (CT or MRI) are not employed in non-complicated situations. Three-dimensional studies on dysplastic hips were conducted to help diagnosis, preoperative planning and evaluate the acetabular cartilage defect [13–19]. However, determining dysplastic condition that shows the under-coverage of femoral head is possible based on available diagnostic radiographic parameters on plain multi-view radiographs. Based on senior author’s experience there is a group of patients who are not dysplastic based on available diagnostic measurements and still have clinical behavior of dysplastic hips. We have developed a new and simple measurement method to estimate femoral head coverage by using a standard AP radiograph of the pelvic. This method is simple, fast, and cost-effective method in comparison with using 3D imaging modalities such as MRI or CT. Based on there being no significant difference in the mean radius of the femoral heads between the two groups in this study, the only parameters that will affect the coverage of femoral head will be the anterior and posterior walls of the acetabulum. A positive posterior wall sign (defined as medially situated position of the posterior wall of the acetabulum in comparison to the center of femoral head [10]) in non-dysplastic hips should be considered as the primary sign of low-volume acetabulum in patients who do not have the radiologic signs of dysplasia. We therefore strongly recommend measuring the CI in non-dysplastic hips with positive posterior wall sign. CI can provide a good estimation of femoral head coverage which is an important factor in optimum hip biomechanics.
Based on the findings of this study, the Mean CI in the low-volume hips was 1.07. To define a threshold for CI further validation is required with long-term follow-up studies and also in another sub-group of suspected low-volume and control patients in order to determine their utility.
The importance of DDH as the precursor of early hip osteoarthritis is well studied before [1, 2]. Based on previous studies low coverage of femoral head may cause increased mechanical stress on labrum and hip joint cartilage and lead to early degenerative hip disease [3–6]. We need to conduct the new long-term follow-up studies to identify the clinical importance of the low-volume acetabulum as the predisposing factor of early hip degenerative disease and hip pain in young adults.
Our study has some limitations. First, the number of cases was low and another study with larger group of patients is recommended to examine the validity of the CI. However, the numbers are acceptable statistically. Second, our findings are based on plain radiographs and 3D imaging (MRI or CT), which are more accurate can be employed to validate the CI in future studies. Third, we did not detect the clinical importance of CI. To determine the clinical significance of our findings, we need to investigate the correlation between radiographic and clinical findings in this group of patients in a new study design.
CONCLUSION
Orthopedic surgeons should be aware of the new group of patients who cannot be classed as having DDH based on traditional radiologic parameters but should be considered as having low-volume acetabuli due to under-coverage of the femoral head. The long-term clinical relevance of this new entity requires further investigation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Ganz R, Leunig M, Leunig-Ganz K, Harris WH.. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466: 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clohisy JC, Beaulé PE, O'Malley A. et al. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am 2008; 90: 2267–81. [DOI] [PubMed] [Google Scholar]
- 3. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand 1939; 83: 5–135. [Google Scholar]
- 4. Van Bosse H, Wedge JH, Babyn P.. How are dysplastic hips different? A threedimensional CT study. Clin Orthop Relat Res 2015; 473: 1712–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armand M, Lepistö J, Tallroth K. et al. Outcome of periacetabular osteotomy: joint contact pressure calculation using standing AP radiographs, 12 patients followed for average 2 years. Acta Orthop 2005; 76: 303–13. [PMC free article] [PubMed] [Google Scholar]
- 6. Michaeli DA, Murphy SB, Hipp JA.. Comparison of predicted and measured contact pressures in normal and dysplastic hips. Med Eng Phys 1997; 19: 180–6. [DOI] [PubMed] [Google Scholar]
- 7. Lequesne M. de Seze. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev Rhum Mal Osteoartic 1961; 28: 643–52. [PubMed] [Google Scholar]
- 8. Reikerås O, Høiseth A, Reigstad A, Fönstelien E.. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand 1982; 53: 775–9. [DOI] [PubMed] [Google Scholar]
- 9. Tonnis D. Surgical treatment of congenital dislocation of the hip. Clin Orthop Relat Res 1990; 258: 33–40. [PubMed] [Google Scholar]
- 10. Kiyama T, Naito M, Shiramizu K, Shinoda T.. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop 2009; 33: 625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960; 20: 37–46. [Google Scholar]
- 12. Gala L, Clohisy JC, Beaulé PE.. Hip dysplasia in the young adult. J Bone Joint Surg Am 2016; 98: 63–73. [DOI] [PubMed] [Google Scholar]
- 13. Dandachli W, Kannan V, Richards R. et al. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br 2008; 90: 1428–34. [DOI] [PubMed] [Google Scholar]
- 14. Haddad FS, Garbuz DS, Duncan CP. et al. CT evaluation of periacetabular osteotomies. J Bone Joint Surg Br 2000; 82: 526–31. [DOI] [PubMed] [Google Scholar]
- 15. Tallroth K, Lepistö J.. Computed tomography measurement of acetabular dimensions: normal values for correction of dysplasia. Acta Orthop 2006; 77: 598–602. [DOI] [PubMed] [Google Scholar]
- 16. James S, Miocevic M, Malara F. et al. MR imaging findings of acetabular dysplasia in adults. Skeletal Radiol 2006; 35: 378–84. [DOI] [PubMed] [Google Scholar]
- 17. Beltran LS, Mayo JD, Rosenberg ZS. et al. Fovea alta on MR images: is it a marker of hip dysplasia in young adults? AJR Am J Roentgenol 2012; 199: 879–83. [DOI] [PubMed] [Google Scholar]
- 18. Beaule PE, Kim YJ, Rakhra KS. et al. New frontiers in cartilage imaging of the hip. Instr Course Lect 2012; 61: 253–62. [PubMed] [Google Scholar]
- 19. Kim YJ, Jaramillo D, Millis MB. et al. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am 2003; 85: 1987–92. [DOI] [PubMed] [Google Scholar]