ABSTRACT
While radiographic findings of frank hip dysplasia are well defined, there is a lack of diagnostic criteria for patients with radiographically ‘normal’ hips who have borderline morphologic deficits and clinical instability. In this study, we aim to define and validate a new radiographic finding associated with hip instability known as the upsloping lateral sourcil (ULS). Patients (316) were reviewed for lateral center edge angles, generalized joint laxity assessed with the Beighton Hypermobility Score and the presence of the ULS. The ULS was defined as a caudal-to-cranial inclination of the middle-to-far lateral aspect of the acetabular sourcil with loss of the normal lateral acetabular concavity. The prevalence of the ULS correspondingly increased with the degree of under-coverage as defined by LCEA. Within the normal coverage group, hips with a ULS had smaller LCEAs than those without ULS (29° versus 32°, P < 0.001). Among hips with a ULS, 59.00% had generalized joint laxity. The association between the ULS finding and generalized joint laxity was statistically significant (P < 0.01). The ULS is seen with higher prevalence in patients with clinical hip laxity and radiographically decreasing LCEA and may serve as an adjunctive finding in patients presenting with hip pain and instability. The ULS may help to characterize patients with borderline hip dysplasia and laxity that fall outside conventional imaging criteria for dysplasia.
INTRODUCTION
Hip instability is a functional abnormality in which the femoral head fails to maintain full congruency with the acetabular cup and which results in hip subluxation and pain [1]. Several proposed factors have been implicated in the development of hip instability, including acetabular coverage [2], femoral torsion [3] and insufficiency of the soft tissue stabilizers [4]. Although developmental hip dysplasia (DDH) is found in only about 0.2% of the newborn population [5], up to 40% of individuals with osteoarthritis of the hip have some involvement of dysplasia [6]. In DDH, a deficient acetabular cup leads to an increase in acetabular roof inclination, decrease in the lateral coverage of the femoral head and increase in anteversion of the acetabular cup [6–8]. These findings present as excessive femoral torsion and acetabular version [9, 10]. The conventional radiographic means of detecting adult hip dysplasia includes measurements such as a Tönnis angle >10° or lateral center edge angle (LCEA) <20° [11–15]. A LCEA of 20–25° is technically within the normal range but is considered by some authors to be more appropriately defined as ‘borderline dysplastic’ and therefore a poor indicator of true congruency of the hip. These borderline patients present a clinical challenge, as some cases can be successfully addressed with hip arthroscopy alone, while some may require open bony realignment procedures [1, 16–18].
Patients with chronic instability associated with hip dysplasia are predisposed to premature osteoarthrosis [19–21], a fact that has undoubtedly driven the push for aggressive and early treatment once diagnosis is established. In the past, treatment for adult dysplastic patients was largely comprised of arthroplasty procedures as a means for symptomatic relief. Recently, orthopedic surgeons have shifted treatment focus to preventative measures aiming to halting the progressive cartilage damage and early joint failure enabling return to pain-free, active life [16, 18, 22–27].
While radiographic findings of frank hip dysplasia are well defined on anteroposterior (AP) and false profile radiographs, these measurements do not always speak to the presence of chronic hip instability arising from a combination of other parameters, such as tissue laxity, patient’s weight, or femoral and acetabular version [14]. Furthermore, when considering patients with borderline acetabular coverage (LCEA 20–25°), the ability to radiographically discern the inherent instability of the hip has substantial benefit in treatment planning. The purpose of this study was to define and validate a new radiographic finding associated with generalized joint laxity in these patients known as the upsloping lateral sourcil (ULS).
PATIENTS AND METHODS
After Institutional Review Board approval was obtained, a retrospective chart review of prospectively collected data was performed on a consecutive series of patients who presented to a hip preservation clinic between 2013 and 2014. Inclusion criteria for patients selected for this study were as follows: (i) persistent hip pain and mechanical symptoms refractory to nonoperative management (physical therapy, non-steroidal anti-inflammatory drugs, activity modifications, corticosteroid injections) lasting at least 3 months, (ii) joint-space width exceeding 3 mm on all views of plain radiography and cross-sectional imaging and (iii) no previous hip joint surgery. All patients underwent routine comprehensive physical examination of the lower spine and lower limbs with emphasis on the evaluation of hip pain and generalized joint laxity. Passive hip range of motion (supine, lateral, prone), the FADIR (flexion, adduction, internal rotation) test, the FABER (flexion, abduction, external rotation) test, the ligamentum teres test, the posterior impingement test and use of the Beighton Hypermobility Score (BHS) [28]. BHS was categorized as follows: no laxity (0–2 points), mild laxity (3–5 points), moderate to severe laxity (6–9 points). BHS allows for a standardized and quantifiable assessment for joint laxity.
All patient charts were reviewed for pre-operative AP hip radiographs that conformed to standard radiographic quality parameters. Standard AP pelvis films were obtained with the lower extremities internally rotated 15° to maximize femoral neck length. The X-ray beam was directed midway between the anterior superior iliac spine (ASIS) and the pubic symphysis, with a focus-film-distance of 120 cm [29]. Radiographs were determined to be adequate given symmetric obturator foramina and a distance of 1–3 cm between the coccyx and pubic symphysis [30].
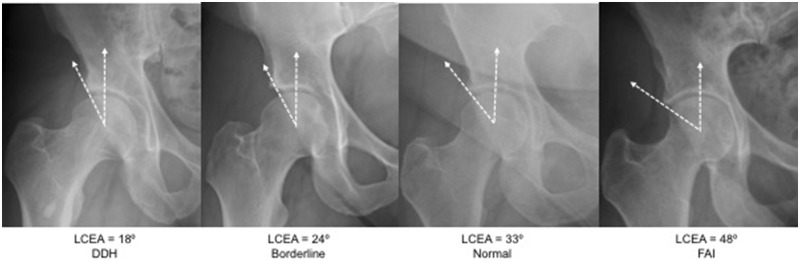
LCEAs were measured using the Ogata technique, where an angle is formed between the orthogonal line drawn from the tear-drop line and a line through the center of the femoral head to the lateral margin of the acetabulum. Both left and right hips were analyzed for a ULS (described below) and LCEA measurement via AP pelvic radiograph. Based on LCEA, patients were segmented into the following categories: frank dysplasia (LCEA <20°), borderline dysplasia (20° ≤ LCEA <25°), normal (25° ≤ LCEA <40°) and pincer-type femoroacetabular impingement (FAI; LCEA ≥40°) (Fig. 1).
Fig. 1.
Four patient groups defined by lateral center edge angle.
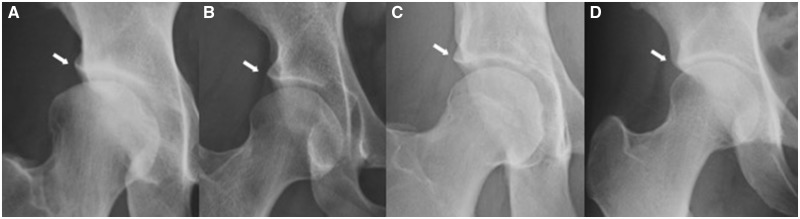
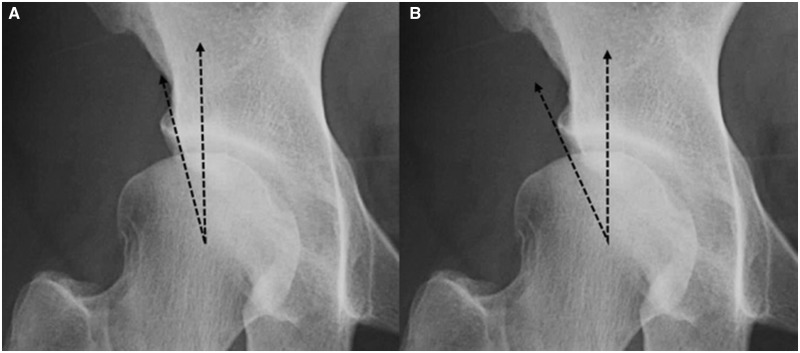
Criteria to determine the presence or absence of the ULS was determined prior to radiographic review of images. A ULS was defined as a caudal-to-cranial inclination of the middle-to-far lateral aspect of the acetabular sourcil with loss of the normal lateral acetabular concavity (Fig. 2). We documented a ULS finding if the sourcil was sloped cranially beyond neutral, which may be referenced by the tear-drop line. All images were reviewed independently by two of the authors (MKJ, TYW) who were both blinded to exact LCEA measurements, BHS classification and findings of the other reviewer. Patients were excluded from analysis if no pre-operative images were available, imaging did not meet the set quality parameters, or if there was dramatic dysplasia of the acetabular cup (negative LCEA) or gross deformity of the femoral head such as Perthes or SCFE.
Fig. 2.
Radiographs demonstrating the ULS finding in various LCEA categories: (A) frank dysplasia, (B) borderline dysplasia and (C) normal, with a (D) negative ULS finding for comparison.
Statistical analysis
Interrater reliability was conducted on the ULS categorization between the two raters using a Fleiss Kappa statistic, independently calculated for the left and right hips. Due to the constraints in the calculation of the statistic, any hips with missing data were removed from the analysis. Further analysis was performed after Kappa statistics were deemed appropriate.
Utilizing the ULS rating from the first rater and pooling ratings between left and right hips, Fisher’s exact tests were conducted to determine if significant associations existed between the acetabular ULS and LCEA as well as generalized joint laxity. A Cochran–Mantel–Haenszel test was performed to determine if a significant association existed between the ULS and generalized joint laxity, while controlling for the potential confounder of LCEA categorization. Finally, positive and negative predictive values were calculated using two different ‘gold standards’: categorization of dysplasia when the LCEA is less than 25° and a BHS of five or fewer points, respectively.
RESULTS
A total of 316 patient charts were reviewed. Sixty-seven patients were excluded based on aforementioned radiographic criteria, leaving 246 patients (492 hips) available for analysis, 70.3% female with a mean age of 33.3 ± 11.4 years. With both hips pooled together, the study sample comprised the following categorizations based on the LCEA: 18 frank dysplasia, 42 borderline dysplasia, 358 normal and 74 pincer-type FAI. Half of all borderline patients had BHS ≥3 points, as did 44% of normal patients (Table I). Stratifying LCEA groups by BHS was not statistically significant in either borderline or normal LCEA groups (Table II).
Table I.
Generalized joint laxity and LCEA category
| No laxity | Mild laxity | Moderate/severe laxity | |
|---|---|---|---|
| Dysplasia | 9 (50.00%) | 5 (27.78%) | 4 (22.22%) |
| Borderline | 21 (50.00%) | 16 (38.10%) | 5 (11.90%) |
| Normal | 194 (55.75%) | 106 (30.46%) | 48 (13.79%) |
| Pincer | 48 (64.86%) | 19 (25.68%) | 7 (9.46%) |
Table II.
LCEA category stratified by generalized joint laxity
| LCEA category | Generalized joint laxity | LCEA |
|
|---|---|---|---|
| Mean (SD) | Median (IQR) | ||
| Dysplasia | None | 16.02 (4.65) | 17.50 (2.00) |
| Mild | 12.28 (7.07) | 14.50 (3.90) | |
| Moderate/severe | 16.00 (2.94) | 16.50 (4.00) | |
| Borderline | None | 22.64 (1.60) | 23.00 (3.00) |
| Mild | 22.31 (1.31) | 22.00 (2.25) | |
| Moderate/severe | 22.00 (1.87) | 23.00 (3.00) | |
| Normal | None | 31.81 (4.15) | 31.00 (6.00) |
| Mild | 31.81 (4.25) | 31.00 (7.50) | |
| Moderate/severe | 31.60 (3.80) | 31.00 (6.00) | |
| Pincera | None | 43.21 (3.32) | 42.00 (4.50) |
| Mild | 42.87 (2.52) | 42.00 (3.00) | |
| Moderate/severe | 46.57 (4.28) | 48.00 (8.00) | |
aStatistically significant by ANOVA test, <0.03
The overall Fleiss-Kappa statistic for ULS in the left hip was 0.67 and for the right hip was 0.63 (Tables III and IV), indicating adequate agreement between the raters [31, 32]. The frank dysplasia category contained the most disagreement for both hip sides, while the other two categories contained similar levels of agreement between the raters.
Table III.
Left hipa
| Rater by upslope | ||
|---|---|---|
| No ULS | ULS | |
| Rater #1 | 200 (81.30%) | 46 (18.70%) |
| Rater #2 | 212 (86.18%) | 34 (13.82%) |
aOverall Fleiss-Kappa statistic: 0.67.
Table IV.
Right hipa
| Rater by upslope | ||
|---|---|---|
| No ULS | ULS | |
| Rater #1 | 192 (78.05%) | 54 (21.95%) |
| Rater #2 | 198 (80.49%) | 48 (19.51%) |
aOverall Fleiss-Kappa statistic: 0.63.
Fisher’s exact test showed a significant association between LCEA category and ULS (P < 0.0001). ULS was most common among patients with frank dysplasia, occurring in 83.33% of all cases. The prevalence of the ULS decreased as the LCEA increased (Table V). Stratifying by LCEA category, two-sample t-tests demonstrated a significant difference in mean LCEA between normal hips with and without ULS (29° versus 32°, P < 0.001) (Table VI).
Table V.
LCEA categorya
| Prevalence of ULS by LCEA category | ||||
|---|---|---|---|---|
| Dysplasia | Borderline | Normal | Pincer | |
| No ULS | 3 (16.67%) | 19 (45.24%) | 298 (83.24%) | 72 (97.30%) |
| ULS | 15 (83.33%) | 23 (54.76%) | 60 (16.76%) | 2 (2.70%) |
aFisher’s exact test P-values: <0.0001.
Table VI.
ULS stratified by LCEAa
| LCEA category | ULS | LCEA |
|
|---|---|---|---|
| Mean (SD) | Median (IQR) | ||
| Dysplasia | Absent | 13.23 (8.21) | 16.00 (15.70) |
| Present | 15.33 (4.66) | 17.00 (3.50) | |
| Borderline | Absent | 22.42 (1.50) | 23.00 (3.00) |
| Present | 22.46 (1.54) | 22.00 (3.00) | |
| Normala | Absent | 31.80 (4.12) | 32.00 (6.50) |
| Present | 29.42 (3.86) | 28.50 (5.50) | |
| Pincer | Absent | 43.49 (3.38) | 42.00 (4.50) |
| Present | 41.75 (1.06) | 41.75 (1.50) | |
aStatistically significant by two-sample t-test, P < 0.001.
Of the 100 hips that demonstrated the ULS finding, 59 hips (59.00%) were in patients with a BHS ≥3 points. Conversely, the ULS finding was relatively less common in patients with a BHS <3 points, present in only 41 of the 272 (15.07%) cases. The association between the ULS finding and generalized joint laxity was found to be statistically significant (Table VII, P < 0.01). As well, the Cochran–Mantel–Haenszel test showed that the LCEA category was a significant variable when evaluating the association between the presence of ULS and generalized joint laxity (P < 0.01). Finally, Table VIII details the positive and negative predictive values of the ULS measurement when compared against the ‘gold standard’ measurements of dysplasia (LCEA <25°) or laxity (BHS of ≤5), respectively. The ULS is shown to be more discriminatory at correspondence to a negative, rather than positive, diagnosis of either dysplasia or laxity.
Table VII.
Generalized joint laxitya
| ULS by Beighton Hypermobility Score categorization | |||
|---|---|---|---|
| No laxity | Mild laxity | Moderate/severe laxity | |
| No ULS | 231 (84.93%) | 107 (73.29%) | 44 (68.75%) |
| ULS | 41 (15.07%) | 39 (26.71%) | 20 (31.25%) |
aFisher’s exact text P-values: <0.01.
Table VIII.
ULS positive (PPV) and negative (NPV) predictive values
| PPV | NPV | Accuracy | |
|---|---|---|---|
| Dysplasia (LCEA <25°) | 0.38 (0.28, 0.48) | 0.94 (0.92, 0.97) | 0.83 (0.80, 0.86) |
| Laxity (BHS ≤5pts) | 0.20 (0.12, 0.28) | 0.88 (0.85, 0.92) | 0.75 (0.71, 0.79) |
DISCUSSION
Based on the results of this study, the presence of the ULS demonstrated a statistically significant association with the LCEA and the presence of generalized joint laxity. It is not surprising that patients with frank hip dysplasia are found to have additional, secondary findings of hip instability given the morphologic and mechanical alterations known to be present in these patients [6]. This study, however, provides new insight into the prevalence of the ULS finding in patients with borderline dysplastic and normal hips.
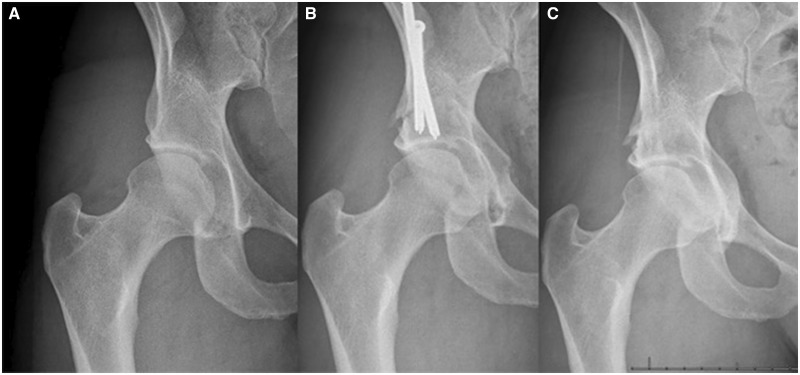
Borderline patients are considered to have ‘low-normal’ acetabular coverage based on standard imaging criteria but often demonstrate hip instability symptoms. Our study shows a considerable proportion of borderline dysplastic hips have the ULS finding on hip radiographs; the ULS finding was more than three-times prevalent in borderline dysplastic hips compared to hips with normal acetabular coverage. Even within the category of a normal LCEA, hips that had the ULS finding had significantly smaller LCEAs. These results are in line with labral hypertrophy [33], increased cartilage thickness [34] and medialization of the iliofemoral line [35], which have all been reported in greater prevalence in borderline and frankly dysplastic hips. As with these examples, it may be feasible, based on our study findings, for the clinician to use the ULS as an additional radiographic finding to identify patients with possible abnormal mechanics that result in hip instability in the setting of otherwise ‘normal’ morphology. This may also assist the clinician in determining which borderline dysplastic patients are expected to yield good long-term outcomes from arthroscopy-only treatment, and which patients will require more invasive bony realignment procedures, though further studies are necessary to determine these outcomes (Fig. 3).
Fig. 3.
A case of a 26-year old, avid skier presenting with right hip pain. Initial pre-surgical radiograph demonstrates a LCEA 21° with an ULS (A). The patient initially underwent arthroscopy for femoracetabular impingement and labral reconstruction. The patient returned 18 months post-operatively with ongoing hip pain. Assuming an instability component to the hip pain, the patient then underwent peri-acetabular osteotomy (PAO) to correct for the acetabular insufficiency (B). At 3 years post-operative follow up the patient has no re-emergence of hip pain (C).
In addition to finding an association between the presence of the ULS and degree of acetabular coverage, we also found patients with higher BHS demonstrate an increased risk of presenting with the ULS. The observed association between ULS with bony undercoverage and instability, as well as between ULS and BHS, suggests that generalized joint laxity may be a significant contributor to radiographic and clinical hip instability. Moreover, the lack of statistically significant relationship between LCEA and BHS stratification in borderline and normal patients may further support the ULS as a useful, independent delineator for instability.
Previous studies have investigated the relationships between generalized joint laxity and instability of the shoulder [36, 37], patellofemoral [38] and ankle joints [39]. As in these joints, there may be an association between generalized joint laxity and instability of the hip joint, in some cases resulting in the ULS finding even if other radiographic findings are normal. Although our study does not specifically provide an association between generalized joint laxity and hip instability, it does present some evidence that this relationship may exist and provides the foundation for future studies on this topic.
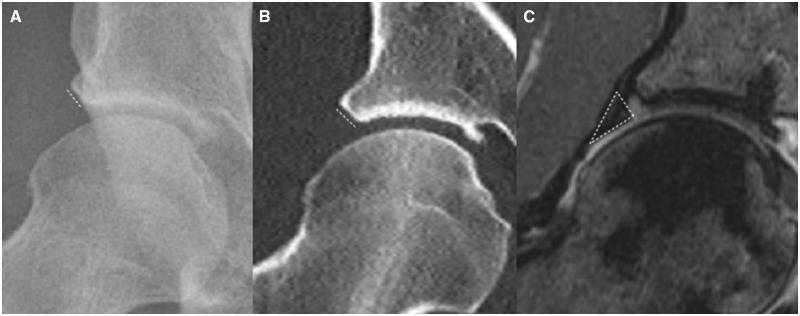
Studies have shown that patients with reduced acetabular coverage demonstrate an associated linear increase in the size of the acetabular labrum [33, 40]. The labral lengthening may be a compensatory loading mechanism by the joint to accommodate excessive stress put on this structure in borderline and frankly dysplastic patients [41]. Although the presence of labral hypertrophy is compelling evidence of chronic instability, this finding requires costly and time-consuming magnetic resonance imaging (MRI) and cannot be feasibly performed on all patients as an initial imaging evaluation. The ULS may be an osseous surrogate to the enlargement of the labrum. As can be seen clearly on MRI, the hypertrophied acetabular labrum in dysplastic patients results in a wider and more robust labro-osseous base, which is consistent with the appearance of the ULS (Fig. 4). Past studies suggest a similar association between dysplastic loading of the capsular limbus with damage to the bony acetabular rim, which may be seen as an ‘os acetabuli’ on radiographs [42]. With these assumptions, we may then potentially glean the same important information and conclusions about the soft tissue compensation of the hip through radiographs alone.
Fig. 4.
Dashed lines demonstrate a corresponding ULS finding on (A) radiograph and (B) coronal CT, as well as an associated hypertrophic labro-osseous base on (C) coronal MRI.
Incorporation of the ULS into a diagnostic algorithm may help to identify patients who suffer from chronic hip instability and are at risk for early joint deterioration despite normal LCEA parameters for hip dysplasia [11, 21]. The ULS, as a secondary finding visible on standard hip radiographs, is advantageous in its simplicity as well as its cost and time-effectiveness. It can serve as a quick, bedside tool utilized in the clinic during the initial assessment. In our results, the ULS finding demonstrated a prominent negative predictive value for both acetabular undercoverage and generalized laxity. Toward this end, the lack of a ULS finding may also be helpful as a secondary confirmation of stability. Traditional radiographic signs and measurements of hip instability and dysplasia, such as the Tönnis angle or neck-shaft angles, remain an important step in the evaluation of the painful and unstable hip. However, it is also critical to measure LCEA in the context of sourcil morphology, as the presence of a ULS may appear to increase the LCEA without necessarily providing more coverage of the femoral head (Fig. 5). The benefit of the ULS is not to replace the current standard in determining hip dysplasia but rather to help suggest underlying issues with chronic instability.
Fig. 5.
The LCEA should be measured to the medial border of the ULS (A) rather than the lateral border of the ULS (B). Measurement of the LCEA at the lateral margin of the ULS will overestimate the effective acetabular coverage of the femoral head.
The limitations of this study should be noted. In particular, there exists a potential sample bias in that all patients presented to a hip preservation surgeon and, therefore, do not represent a fully generalizable sample. Thus, it is likely that our patient sample over-represents the prevalence of the ULS finding in a general population. However, we do not feel that this overrepresentation in our select patient population threatens the validity of this radiographic finding. In addition, as a retrospective cross-sectional study, we did not specifically evaluate subjective reports of instability, treatment outcome, disease progression or changes in the ULS finding following operative management of pre-osteoarthritic hip conditions. Data analysis consisted only of objective factors such as radiographic findings and laxity scores, thereby eliminating subjective symptomatology. Therefore, our data do not directly quantify the effect of the ULS finding in long-term outcomes.
CONCLUSIONS
The ULS is a novel radiographic description characterized as an upslope in the lateral quarter of the acetabular sourcil. The ULS finding carries a statistically significant association with the degree of acetabular dysplasia as defined by LCEA. The ULS finding not only occurs in a considerable proportion of patients who have borderline hip dysplasia, but also relates to a significantly smaller LCEA even in normal hips. Moreover, this radiographic sign carries a significant association with generalized joint laxity, which supports its utility as a secondary finding to incorporate into the diagnosis of patients at-risk for instability. Further investigations are needed to validate the clinical applicability of this radiographic finding for use alongside traditional markers of hip dysplasia.
FUNDING
No source of funding.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLOSURE
Dr. Jesse is a paid presenter for Medtronic. Dr. Mei-Dan is a paid consultant for and receives IP royalties and research support from Stryker, and receives stock or stock options from MITA.
REFERENCES
- 1. Kraeutler MJ, Garabekyan T, Pascual-Garrido C et al. Hip instability: a review of hip dysplasia and other contributing factors. Muscles Ligaments Tendons J 2016; 6: 343–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Canham CD, Yen Y-M, Giordano BD. Does femoroacetabular impingement cause hip instability? A systematic review. Arthrosc J Arthrosc Relat Surg 2016; 32: 203–8. [DOI] [PubMed] [Google Scholar]
- 3. Laplaza JF, Root L. Femoral anteversion and neck-shaft angles in hip instability in cerebral palsy. J Pediatr Orthop 1994; 14: 719–23. [DOI] [PubMed] [Google Scholar]
- 4. Larson CM, Stone RM, Grossi EF et al. Ehlers–Danlos syndrome: arthroscopic management for extreme soft-tissue hip instability. Arthrosc J Arthrosc Relat Surg 2015; 31: 2287–94. [DOI] [PubMed] [Google Scholar]
- 5. Kolb A, Schweiger N, Mailath-Pokorny M et al. Low incidence of early developmental dysplasia of the hip in universal ultrasonographic screening of newborns: analysis and evaluation of risk factors. Int Orthop 2016; 40: 123–7. [DOI] [PubMed] [Google Scholar]
- 6. Gala L, Clohisy JC, Beaule PE. Hip dysplasia in the young adult. J Bone Jt Surg 2016; 98: 63–73. [DOI] [PubMed] [Google Scholar]
- 7. Anda S, Terjesen T, Kvistad KA et al. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr 1991; 15: 115–20. [DOI] [PubMed] [Google Scholar]
- 8. Kim SS, Frick SL, Wenger DR. Anteversion of the acetabulum in developmental dysplasia of the hip: analysis with computed tomography. J Pediatr Orthop 1999; 19: 438–42. [DOI] [PubMed] [Google Scholar]
- 9. Jamali AA, Mladenov K, Meyer DC et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res 2007; 25: 758–65. [DOI] [PubMed] [Google Scholar]
- 10. Kalberer F, Sierra RJ, Madan SS et al. Ischial spine projection into the pelvis. Clin Orthop 2008; 466: 677–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cooperman D. What is the evidence to support acetabular dysplasia as a cause of osteoarthritis? J Pediatr Orthop 2013; 33(Suppl. 1): S2–S7. [DOI] [PubMed] [Google Scholar]
- 12. Ogata S, Moriya H, Tsuchiya K et al. Acetabular cover in congenital dislocation of the hip. Bone Jt J 1990; 72: 190–6. [DOI] [PubMed] [Google Scholar]
- 13. Sharp IK. Acetabular dysplasia: the acetabular angle. Bone Jt J 1961; 43-B: 268–72. [Google Scholar]
- 14. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Jt Surg Am 1999; 81: 1747–70. [DOI] [PubMed] [Google Scholar]
- 15. Umer M, Sepah YJ, Asif S et al. Acetabular morphometry and prevalence of hip dysplasia in the South Asian population. Orthop Rev 2009; 1: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lodhia P, Chandrasekaran S, Gui C et al. Open and arthroscopic treatment of adult hip dysplasia: a systematic review. Arthrosc J Arthrosc Relat Surg 2016; 32: 374–83. [DOI] [PubMed] [Google Scholar]
- 17. Domb BG, Stake CE, Lindner D et al. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med 2013; 41: 2591–8. [DOI] [PubMed] [Google Scholar]
- 18. Philippon MJ. New frontiers in hip arthroscopy: the role of arthroscopic hip labral repair and capsulorrhaphy in the treatment of hip disorders. Instr Course Lect 2006; 55: 309–16. [PubMed] [Google Scholar]
- 19. Birrell F, Silman A, Croft P et al. Syndrome of symptomatic adult acetabular dysplasia (SAAD syndrome). Ann Rheum Dis 2003; 62: 356–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology 2005; 44: 211–8. [DOI] [PubMed] [Google Scholar]
- 21. Murphy S, Kijewski P, Millis M et al. Acetabular dysplasia in the adolescent and young adult. Clin Orthop 1990; 261: 214–23. [PubMed] [Google Scholar]
- 22. Sanchez-Sotelo J, Berry DJ, Trousdale RT et al. Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. J Am Acad Orthop Surg 2002; 10: 334–44. [DOI] [PubMed] [Google Scholar]
- 23. Engesæter LB, Furnes O, Havelin LI. Developmental dysplasia of the hip—good results of later total hip arthroplasty: 7135 primary total hip arthroplasties after developmental dysplasia of the hip compared with 59 774 total hip arthroplasties in idiopathic coxarthrosis followed for 0 to 15 years in the Norwegian Arthroplasty Register. J Arthroplasty 2008; 23: 235–40. [DOI] [PubMed] [Google Scholar]
- 24. Argenson J-NA, Flecher X, Parratte S et al. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop 2007; 465: 40–5. [DOI] [PubMed] [Google Scholar]
- 25. Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Jt Surg Am 1979; 61:15–23. [PubMed] [Google Scholar]
- 26. Mei-Dan O, Garabekyan T, McConkey M et al. Arthroscopic anterior capsular reconstruction of the hip for recurrent instability. Arthrosc Tech 2015; 4: e711–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Steppacher SD, Tannast M, Ganz R et al. Mean 20-year followup of bernese periacetabular osteotomy. Clin Orthop 2008; 466: 1633–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kraeutler MJ, Garabekyan T, Pascual-Garrido C et al. Ligamentum teres tendinopathy and tears. Muscles Ligaments Tendons J 2016; 6: 337–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jesse MK, Petersen B, Strickland C et al. Normal anatomy and imaging of the hip: emphasis on impingement assessment. Semin Musculoskelet Radiol 2013; 17: 229–47. [DOI] [PubMed] [Google Scholar]
- 30. Clohisy JC, Carlisle JC, Beaulé PE et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Jt Surg Am 2008; 90: 47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. [PubMed] [Google Scholar]
- 32. Sim J, Wright CC. The Kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 2005; 85: 257–68. [PubMed] [Google Scholar]
- 33. Petersen BD, Wolf B, Lambert JR et al. Lateral acetabular labral length is inversely related to acetabular coverage as measured by lateral center edge angle of Wiberg. J Hip Preserv Surg 2016; 3: 190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nishii T, Sugano N, Sato Y et al. Three-dimensional distribution of acetabular cartilage thickness in patients with hip dysplasia: a fully automated computational analysis of MR imaging. Osteoarthritis Cartilage 2004; 12: 650–7. [DOI] [PubMed] [Google Scholar]
- 35. Kraeutler MJ, Ashwell ZR, Garabekyan T et al. The iliofemoral line: a radiographic sign of acetabular dysplasia in the adult hip. Am J Sports Med 2017; 45: 2493–500. [DOI] [PubMed] [Google Scholar]
- 36. Cameron KL, Duffey ML, DeBerardino TM et al. Association of generalized joint hypermobility with a history of glenohumeral joint instability. J Athl Train 2010; 45: 253–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Koyonos L, Kraeutler MJ, O’Brien DF et al. A prospective cohort study investigating the effect of generalized joint hypermobility on outcomes after arthroscopic anterior shoulder stabilization. Phys Sportsmed 2016; 44: 380–4. [DOI] [PubMed] [Google Scholar]
- 38. Howells NR, Eldridge JD. Medial patellofemoral ligament reconstruction for patellar instability in patients with hypermobility: a case control study. J Bone Jt Surg Br 2012; 94: 1655–9. [DOI] [PubMed] [Google Scholar]
- 39. Huang B, Kim YT, Kim JU et al. Modified Broström procedure for chronic ankle instability with generalized joint hypermobility. Am J Sports Med 2016; 44: 1011–6. [DOI] [PubMed] [Google Scholar]
- 40. Garabekyan T, Ashwell Z, Chadayammuri V et al. Lateral acetabular coverage predicts the size of the hip labrum. Am J Sports Med 2016; 44: 1582–9. [DOI] [PubMed] [Google Scholar]
- 41. Henak CR, Ellis BJ, Harris MD et al. Role of the acetabular labrum in load support across the hip joint. J Biomech 2011; 44: 2201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. Bone Jt J 1991; 73: 423–9. [DOI] [PubMed] [Google Scholar]