Abstract
Aim of the Study
The present study evaluated the cardiovascular changes related to anxiety of the patient undergoing local anesthesia injection for extraction in Indian population.
Methodology
In total, 100 Indian male patients were enrolled in the prospective study. Anxiety was measured at 15 min before local anesthetic delivery using Corah’s Dental Anxiety Scale (DAS). Cardiovascular response data including blood pressure, heart rate, oxygen saturation and electrocardiographic changes were measured at five time points from 5 min before to 15 min after the administration of anesthetic.
Results
The mean anxiety scale score before administration of anesthetic was 8.24 (± 3.55) with a range from 4 to 20. Younger age was associated with a higher anxiety scale score. Severe preoperative anxiety (DAS > 12) was associated with significantly increased heart rate and blood pressure during administration of anesthetic. Significant ECG change was present at the time and 5 min after local anesthesia administration. Pain on injection was also associated with increased heart rate and blood pressure during anesthetic administration.
Conclusion
The present study shows that significant cardiovascular changes do occur due to dental anxiety at the time of local anesthesia administration for tooth extraction in Indian population.
Keywords: Local anesthetic, Cardiovascular changes, Anxiety
Introduction
Anxiety or fear during dental treatment has been a concern to dentist from time immemorial. Approximately 6–15% of the population suffers from dental fear and anxiety which leads to avoidance of dental treatment worldwide [1]. Although every procedure that is performed in the dental office is capable of being viewed as frightening, by the patient, anxiety related to injection of an anesthetic is probably one of the most important psychological responses. The anticipation of the anesthesia injection produces more fear than the actual injection itself [2]. Anxiety related to local anesthesia injection has a significant effect on patient’s cardiovascular status. Many patients have been reported of having cardiac attack and vasovagal syncope due to high level of stress generated in response to local anesthetic injection.
A vasovagal fainting is characteristic of blood–injection–injury-type-specific phobia. The physiologic response is characterized by an initial brief acceleration of heart rate and increase in blood pressure followed by a falling of heart rate and a drop in blood pressure [3].
The administration of local anesthetics containing vasoconstrictor seems to be a source of exogenous catecholamine [2], which, when combines with unmarked endogenous catecholamine induced from increased anxiety due to anticipation of the dental procedure [4], may further aggravate the condition making vigilant monitoring of cardiac status of patients a necessity.
Thus we conducted a study is to evaluate the cardiovascular changes related to anxiety of the patient undergoing local anesthesia injection for extraction in Indian population, using Corah’s Dental Anxiety Scale (DAS), patient’s vitals like blood pressure, heart rate, oxygen saturation and electrocardiograph. To the best of our knowledge, no such study in Indian population has been ever conducted.
Material and Methods
The study was conducted on 100 patients of Indian origin who reported to the Department of Oral and Maxillofacial Surgery, to evaluate the cardiovascular response related to anxiety undergoing local anesthesia injection for extraction.
All procedures performed in study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
A written informed consent was obtained from all individual participants included in the study.
Inclusion criteria:
Male patients of 18–55 years age. (Male patients were taken to remove the gender bias)
Patients with mandibular tooth extraction where inferior alveolar nerve block is required.
Patient willing to participate in the study.
Exclusion criteria:
Patients not medically fit to undergo extraction (especially any current history of cardiovascular disease, hypertension, psychiatric disorder or any motor and neurosensory disorders)
Local anesthesia allergies.
Uncooperative patients.
Method
All the patient were given the Corah’s Dental Anxiety Scale (Table 1) to be filled prior in waiting area 15 min before the procedure. Corah’s Dental Anxiety Scale was published in 1969 for assessing dental anxiety. It is reliable and useful tool to assess patient’s distress during dental treatment. It consists of four multiple-choice questions to be filled by the patient. The possible score ranges from 4 to 20, and on the basis of scores, patients were divided into mild (4–8), moderate (9–12) and severe (> 12) dental anxiety groups [1]. Patients were also divided on the basis of perception of pain into (a) pain on injection and (b) no pain on injection.
Table 1.
Corah’s dental anxiety scale
Cardiovascular response was evaluated using parameters like blood pressure, heart rate, oxygen saturation and electrocardiographic changes. All parameters were evaluated at 5 min prior to injection, at the time of local anesthesia administration and after 5-, 10- and 15-min interval of administration of local anesthesia.
Anesthesia used was 2% lidocaine with 1:80000 epinephrine with 1.8-ml dose. We also used positive communication skills to relax and calm patients generally.
Result
A total of 100 male patients, aged from 18 to 55 years (mean age 38.49 ± 11.76 years), volunteered for participation in the study (Fig. 1). The mean DAS was 8.24 ± 3.55. However, the patients having the higher DAS score were having positive dental anxiety history (p < 0.01). In contrast, pain on injection was also observed in patients who were having mild dental anxiety and was significant (p = 0.03) (Fig. 2).
Heart Rate.
Fig. 1.
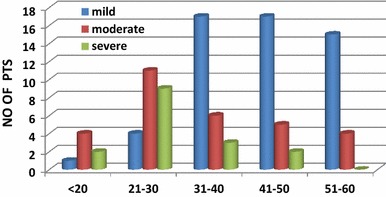
Frequency distribution of patient’s according to dental anxiety groups in relation to age
Fig. 2.
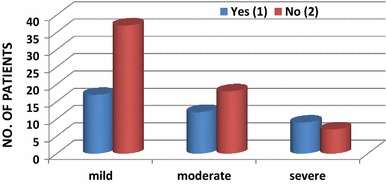
Frequency distribution of patient’s according to dental anxiety groups in relation to pain
The cardiovascular changes in the peri-injection period in various anxiety groups are summarized (Table 2). Patients with mild dental anxiety had a lower heart rate during anesthetic delivery than those with moderate or severe dental anxiety. After the delivery of local anesthesia, the heart rate increased in all groups, but this increase was greater in the severe dental anxiety group. The maximum increase in heart rate in the severe (from 85 ± 11.46 to 94 ± 11.89 bpm) dental anxiety group was greater than in the moderate (from 78.20 ± 11.76 to 84.65 ± 13.31 bpm) and the mild (from 72.87 ± 12.59 to 78.04 ± 12.12 bpm) anxiety groups (Fig. 2). The difference in the heart rate was most significant between the mild and severe dental anxiety groups (p < 0.01).
-
b.
Blood Pressure.
Table 2.
Average systolic blood pressure (BP, in mm Hg), diastolic blood pressure, O2 saturation (SpO2) and heart rate (in beats/min) of patients in different anxiety groups in the peri-injection period with 5-min intervals
| Mild (< 9) N = 54 |
Moderate (9–12) N = 30 |
Severe (> 12) N = 16 |
p valuea | Compare each pair of groupsb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mild and Mod | Mod and Sev. | Mild and Sev. | ||
| DAS score | ||||||||||
| Heart rate | ||||||||||
| Preinjection | 72.87 | 12.597 | 78.20 | 11.759 | 85.00 | 11.468 | < 0.02 | * | * | * |
| Injection | 74.80 | 12.034 | 82.00 | 12.900 | 89.81 | 12.010 | < 0.01 | * | * | * |
| 5 min | 77.22 | 13.223 | 84.65 | 13.307 | 94.46 | 11.890 | < 0.01 | * | * | * |
| 10 min | 78.04 | 12.125 | 83.95 | 8.906 | 90.96 | 11.358 | < 0.02 | * | * | * |
| 15 min | 76.26 | 13.421 | 81.60 | 9.698 | 88.35 | 10.384 | < 0.01 | * | * | * |
| Systolic BP | ||||||||||
| Preinjection | 128.91 | 13.304 | 121.40 | 9.875 | 127.23 | 8.738 | < 0.06 | * | * | |
| Injection | 129.80 | 12.774 | 124.90 | 12.751 | 133.65 | 7.526 | < 0.01 | * | * | * |
| 5 min | 127.13 | 13.285 | 124.10 | 10.307 | 132.92 | 8.948 | < 0.01 | * | * | * |
| 10 min | 126.11 | 12.764 | 122.05 | 13.809 | 129.50 | 8.291 | < 0.02 | * | * | * |
| 15 min | 124.69 | 13.025 | 120.80 | 8.995 | 128.46 | 6.671 | < 0.01 | * | * | * |
| Diastolic BP | ||||||||||
| Preinjection | 79.10 | 9.676 | 76.75 | 8.019 | 79.00 | 7.020 | < 0.06 | * | * | |
| Injection | 79.82 | 9.620 | 77.25 | 9.164 | 80.88 | 8.226 | < 0.04 | * | * | |
| 5 min | 77.94 | 9.545 | 75.75 | 10.376 | 80.62 | 6.859 | < 0.05 | * | * | |
| 10 min | 77.13 | 9.335 | 75.40 | 8.726 | 78.38 | 6.494 | < 0.07 | * | * | |
| 15 min | 78.61 | 9.398 | 76.20 | 9.046 | 79.50 | 8.349 | < 0.06 | * | * | |
| SpO 2 | ||||||||||
| Preinjection | 97.61 | 1.295 | 97.30 | .979 | 97.77 | 1.107 | 0.78 | |||
| Injection | 95.78 | 2.062 | 95.90 | 1.861 | 96.12 | 2.215 | 0.86 | |||
| 5 min | 96.28 | 1.917 | 96.15 | 2.084 | 96.00 | 2.280 | 0.81 | |||
| 10 min | 96.83 | 1.668 | 97.00 | 1.451 | 96.46 | 1.860 | 0.69 | |||
| 15 min | 97.28 | 1.433 | 97.30 | .923 | 97.23 | 1.478 | 0.93 | |||
Bold indicates the significant of p value ( p < 0.05)
*p ≤ 0.05
aKruskal–Wallis test
bPost-HOC test
No significant difference in blood pressure was noted in mild, moderate and severe dental anxiety groups at any time in the peri-injection period (p < 0.06). After the delivery of local anesthetic, significant increase in both systolic and diastolic blood pressure occurred. The maximum increase in systolic blood pressure in the severe dental anxiety group (6.37 ± 5.5 mm Hg) was greater than in mild dental anxiety group (1.79 ± 1.51 mm Hg); this difference was significant (p < 0.01). The maximum increase in diastolic blood pressure in the severe dental anxiety group (1.88 ± 7.68 mm Hg) was higher than in the mild dental anxiety group (0.72 ± 9.6 mm Hg); this difference was significant (p < 0.04). There was little fluctuation in systolic and diastolic blood pressure in mild dental anxiety group in comparison with moderate and severe dental anxiety group. Both the systolic and diastolic blood pressure showed a tendency to increase during the administration of local anesthetic in all three groups (Table 2).
-
c.
O2 Saturation.
The mean baseline level of O2 saturation during the peri-injection in the dental chair was almost same in all the three dental anxiety groups and was not significant (p = 0.78). At the time of injection and 5 min, there is a decrease in O2 saturation in all the three groups, but it was not significant (p = 0.86). O2 saturation started increasing at 10 and 15 min and became normal in all the three groups (Table 2).
-
d.
Electrocardiographic Changes.
There were significant differences in the change in ECG between patients with different levels of anxiety at the time of injection and 5 min after local anesthetic injection (Table 3). The most common electrocardiographic changes present were tachycardia which was not present in the mild dental anxiety group. Tachycardia was developed at time of injection in 10 and 62.5%, whereas after 5 min of local anesthesia it was developed in 13.33 and 68.75% in moderate and severe dental anxiety group.
Table 3.
ECG change of patients in different anxiety groups in the peri-injection period with 5-min intervals
| Mild (< 9) (n = 54) |
Moderate (9–12) (n = 30) |
Severe (> 12) (n = 16) |
p valuea | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| DAS score | |||||||
| Preinjection | |||||||
| Normal | 48 | 88.89 | 24 | 80 | 7 | 43.75 | .24 |
| With abnormal findings | 6 | 11.11 | 6 | 20 | 9 | 56.25 | |
| Sinus tachycardia | 0 | 0 | 2 | 6.67 | 9 | 56.25 | |
| Sinus bradycardia | 6 | 11.11 | 4 | 13.33 | 0 | 0 | |
| Injection | |||||||
| Normal | 49 | 90.74 | 24 | 80 | 6 | 37.5 | |
| With abnormal findings | 5 | 9.26 | 6 | 20 | 10 | 62.5 | |
| Sinus tachycardia | 0 | 0 | 3 | 10 | 10 | 62.5 | |
| Sinus bradycardia | 5 | 9.26 | 3 | 10 | 0 | 0 | < .01 |
| 5 min | |||||||
| Normal | 50 | 92.59 | 25 | 83.33 | 5 | 31.25 | .03 |
| With abnormal findings | 4 | 7.41 | 5 | 16.67 | 11 | 68.75 | |
| Sinus tachycardia | 0 | 0 | 4 | 13.33 | 11 | 68.75 | |
| Sinus bradycardia | 4 | 7.41 | 1 | 3.33 | 0 | 0 | |
| 10 min | |||||||
| Normal | 50 | 92.59 | 26 | 86.67 | 7 | 43.75 | .49 |
| With abnormal findings | 4 | 7.41 | 4 | 13.33 | 9 | 56.25 | |
| Sinus tachycardia | 0 | 0 | 3 | 10 | 9 | 56.25 | |
| Sinus bradycardia | 4 | 7.41 | 1 | 3.33 | 0 | 0 | |
| 15 min | |||||||
| Normal | 49 | 90.74 | 25 | 83.33 | 7 | 43.75 | .27 |
| With abnormal findings | 5 | 9.26 | 5 | 16.67 | 9 | 56.25 | |
| Sinus tachycardia | 0 | 0 | 3 | 10 | 9 | 56.25 | |
| Sinus bradycardia | 5 | 9.26 | 2 | 6.67 | 0 | 0 | |
Bold indicates the significant of p value ( p < 0.05)
aKruskal–Wallis test
The cardiovascular changes in the peri-injection period in groups with pain (1) and no pain (2) on injection are summarized in Table 4. Significant differences were found in the heart rate at time of injection (p < 0.01) and 5 min (p = 0.03) after local anesthesia injection among patient groups divided according to pain and no pain during injection. Before the injection, patients with no pain (2) on injection had lower mean systolic and diastolic blood pressure than patients with pain on injection (1). There was a significant increase in the systolic (p = 0.04) and diastolic (p < 0.05) blood pressure at the time of local anesthesia in both the groups.
Table 4.
Average systolic blood pressure (BP, in mm Hg), diastolic blood pressure, O2 saturation (SpO2) and heart rate (in beats/min) of patients in different reporting pain groups in the peri-injection period with 5-min intervals
| YES (1) N = 38 |
NO (2) N = 62 |
P valuea | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Pain during injection | |||||
| Heart rate | |||||
| Preinjection | 74.66 | 13.302 | 73.87 | 11.733 | 0.23 |
| Injection | 80.84 | 11.698 | 76.10 | 12.706 | < 0.01 |
| 5 min | 79.42 | 12.116 | 75.79 | 14.140 | 0.03 |
| 10 min | 76.39 | 11.315 | 74.11 | 11.620 | 0.43 |
| 15 min | 76.12 | 11.056 | 73.21 | 12.718 | 0.54 |
| Systolic BP | |||||
| Preinjection | 127.21 | 12.641 | 125.44 | 11.466 | 0.65 |
| Injection | 132.42 | 13.377 | 127.35 | 11.516 | 0.04 |
| 5 min | 129.13 | 12.493 | 127.11 | 12.159 | 0.58 |
| 10 min | 128.53 | 13.264 | 126.81 | 11.742 | 0.75 |
| 15 min | 127.98 | 10.770 | 126.56 | 12.019 | 0.45 |
| Diastolic BP | |||||
| Preinjection | 78.18 | 9.926 | 77.00 | 7.951 | 0.58 |
| Injection | 80.45 | 10.058 | 78.89 | 8.997 | 0.06 |
| 5 min | 79.97 | 9.844 | 78.16 | 9.244 | 0.06 |
| 10 min | 78.57 | 8.719 | 77.13 | 9.038 | 0.07 |
| 15 min | 78.15 | 8.877 | 77.58 | 9.666 | |
| SpO 2 | |||||
| Preinjection | 97.53 | 1.330 | 97.63 | 1.105 | 0.67 |
| Injection | 95.84 | 1.994 | 95.92 | 2.098 | 0.56 |
| 5 min | 96.11 | 2.141 | 96.23 | 1.979 | 0.35 |
| 10 min | 96.82 | 1.706 | 96.74 | 1.669 | 0.08 |
| 15 min | 97.18 | 1.291 | 97.32 | 1.388 | 0.26 |
Bold indicates the significant of p value ( p < 0.05)
aChi-square test
The mean level of O2 saturation does not show any significant (p = 0.56) change, but there was a slight drop at the time of local anesthesia administration present. These results prove that significant cardiovascular changes do occur in patients undergoing local anesthesia injection due to anxiety.
Discussion
The lignocaine–adrenaline combination is the most widely used local anesthetic solution in dental practice. The administration of a vasoconstrictor and local anesthetics combination seems to be a source of exogenous catecholamine, which, when combined with unmarked endogenous catecholamine induced from increased anxiety due to anticipation of the dental procedure, may cause unwanted side effects which can be life threatening [4]. Vasoconstrictors have been reported to influence blood pressure in the same way as other factors such as anxiety and stress [5]. Also response to stress and anxiety is time dependent with parabolic nature. This starts to increase gradually as the stressful event approximates, reaches a peak generally at the time of event and slowly fades off with completion of the event [6]. Thus in the present study, evaluation of clinical parameters in preinjection during injection and post-injection phases was done.
Although several methods and scale are given for the assessment of anxiety before any dental procedure, we took Corah’s Dental Anxiety Scale (DAS) as it is a reliable indicator of physiologic stress levels and widely used self-report measure of the overall dental anxiety. The scale’s validity and reliability have been widely accepted [6]. In Corah’s Dental Anxiety Scale, there are four different sets of question concerning, which were evaluated and the score was given according to the option [7]. The overall mean DAS score was 8.24 ± 3.55 which ranged from 4 to 20. This mean DAS score was approximately same which was reported in earlier studies in adult patients, in the range from 7.26 to 9.3 [1, 6, 8, 9].
In the present study, majority of the patients who reported a history of eventful dental experiences during previous dental treatments exhibited moderate to severe dental anxiety. Vassend reported that among individuals aged 15 years or above, 4.2–7.1% had dental anxiety, and 60% of these had experienced at least one very painful dental visit. Such dental anxiety may result in delays in making a needed dental appointment and canceling or failing to show up for a booked appointment [10]. Berggren and Meynert reported that 76.3% of 160 adult patients with severe dental fear and avoidance of dental treatment had one or several previous traumatic dental experiences [11]. In our study, 50% of the patients in moderate and severe dental anxiety groups had a positive history of eventful dental experience.
In our study, the severe dental anxiety group patients were younger than those in the mild and moderate groups, a finding matching with several other studies on dental apprehension [1, 2]. Although increased anxiety in younger patients may be partially due to less experience and familiarity with dental treatment, these impressions are relatively difficult to assess. However, our finding that patients in the high dental anxiety group had younger age suggests that experience and familiarity, as far as they can be measured or represented in terms of age, are potentially important factors.
We also found in our study that pain on injection is present in all the three groups and does not depend upon the anxiety of the patients. The previous study by Liau et al. [1] also found that pain was present in all the anxiety groups. De Jongh et al. [12] postulate that patients are less likely to develop dental anxiety if they undergo prior conditioning of a number of relatively painless treatments. In our study, we have not quantified the pain which can be a possible reason that pain was present in all the three groups.
During the peri-injection period in the dental chair before the administration of anesthetic, DAS score was not associated with blood pressure (p < 0.06) but was significantly associated with heart rate (p < 0.02). During this time, the heart rate of the severe dental anxiety group averaged 13 bpm higher than that of the mild dental anxiety group. This difference was much greater than an earlier study that found that the average heart rate of anxious patients was only 4 bpm higher than in non-anxious patients [3]. This variation may be due to various definitions of dental anxiety or study design patterns.
At the time of delivery of local anesthesia in the present study, the heart rate, mean systolic and diastolic blood pressure in the mild, moderate and severe dental anxiety group increased significantly. The maximum increase in heart rate (9 bpm) and blood pressure (6.37 ± 5.5 mm Hg) was present in the severe dental anxiety group. The present finding that both heart rate and blood pressure were increased during the delivery of local anesthesia is similar to earlier studies [1, 13]. Brand and Abraham-Inpijn [3] state that injecting a local anesthetic to a patient followed by extraction induces a considerable average increase in heart rate (+ 12%) and systolic (+ 24%) and diastolic blood pressure (+ 18%). The increase in heart rate and the alterations in blood pressure during the injection in the present study may have been mostly due to endogenous epinephrine release as a result of the emotional stress.
After 5 min of local anesthesia administration, there was still increase in the heart rate in mild, moderate and severe dental anxiety groups. The maximum increase was still present in the severe dental anxiety group (4.55 bpm), whereas the blood pressure shows a downfall in all the three groups. At 10 and 15 min of local anesthesia administration, the heart rate and blood pressure started to normalize.
The mean baseline level of O2 saturation during the peri-injection in the dental chair was almost same in all the three dental anxiety groups and was not significant (p = 0.78). At the time of injection and 5 min, there was a decrease in O2 saturation in all the three groups, but it was not significant (p = 0.86). O2 saturation started increasing at 10 and 15 min and become normal in all the three groups. In the previous study by Ryhänen et al. [14], the blood oxygen saturation values were constant and the displayed SpO2 values were between 96 and 98% before and after the local anesthesia administration. Vasconcellos also told that, at no moment of evaluation in all the groups, even under the effect of the anesthetics, the mean measurement of SPO2 was not outside the normal range [15]. The results of these studies are in accordance with our studies.
ECG changes noted in our study due to dental anxiety before and after local anesthesia delivery were bradycardia and tachycardia. No other type of dysrhythmias, such as ventricular premature contracture and atrial fibrillation, was noted as medically compromised patients were excluded in our study. At the time of administration of local anesthesia, tachycardia was present in moderate (10%) and severe (62.5%) dental anxiety group, whereas bradycardia was present in mild (9.26%) dental anxiety group. After 5 min of local anesthetic delivery, tachycardia percentage increases in moderate (13.33%) and severe (68.75%) dental anxiety group, whereas bradycardia percentage decreases in mild (7.41%) dental anxiety group. This shows that the heart rate was increasing in all the three groups. At 10 and 15 min after local anesthesia delivery, the ECG changes start to normalize in our study. Previous studies on ECG change during local anesthesia delivery found incidences of abnormal ECG change in 35–37.5% of patients [16–18].
We also evaluated cardiovascular changes on the basis of pain (1) and no pain (2) on injection. In the present study, the heart rate and blood pressure were higher in pain on injection group (1) as compared to no-pain group (2) at the peri-injection period, but it was not significant. At the time of local anesthesia administration, increase in heart rate (p < 0.01) and blood pressure was associated with pain on injection and was significant. The previous study by Liau et al. [1] suggests that pain on injection has an additive effect on increase in heart rate in patients undergoing routine dental extraction. Brand HS also told that change in mean heart rate and in mean systolic and diastolic blood pressure is induced by both the patient’s anticipation of scheduled treatment and the actual dental treatment. Most of these changes are within the normal physiologic variations, but significant changes are observed before administration of a local anesthetic, during extractions [19]. The oxygen saturation was not correlated with pain on injection at time of local anesthesia and was not significant, but it was slightly lowered at the time of local anesthesia administration.
Pain was present in all the groups irrespective of Corah’s Dental Anxiety Scale score. Although changes in systolic blood pressure, diastolic blood pressure and heart rate on injection were associated with pain on injection, they were also associated with DAS score. The reason can be due to the different perception of pain on injection. In the present study, none of the patients had undergone syncope. Thus the effect of biphasic reflex bradycardia was not noted.
Thus from the study, we can find out that cardiovascular changes do occur due to dental anxiety, which seems be more influential than the epinephrine in local anesthesia, during local anesthesia administration for tooth extraction in Indian male population and follow the trend worldwide. We also suggest that stress and anxiety reduction protocols should be followed while giving local anesthesia injection. These measures must begin as soon as the patient enters the dental office for the first time. These measures can be in the form of (a) calm and soothing dental office environment, (b) positive communication skills by all personals working in the dental office, (c) behavior management techniques like relaxation techniques, biofeedback methods, hypnotherapy, positive reinforcements, distraction methods, desensitization, cognitive therapy and acupressure, (d) pharmacological management like deanxiety drugs, diazepam, and conscious sedation, (e) advanced technological tools and devices like electronic dental anesthesia and computer-controlled local anesthesia delivery system [20]. Although positive communication skills to relax and calm the patients were used in the study, still the anxiety had persisted.
Conclusion
The present results suggest that the anxiety levels of patients may be correlated with past dental experiences. Screening for high anxiety levels before dental procedures using an objective scale such as Corah’s DAS may identify patients with high anxiety levels, thereby enabling additional precautions to be taken which may improve quality of care, patient’s experience and prevent any medical emergency. So a proper monitoring prior to any dental procedure should be done more intensely. We further suggest continuing the study in cardiac patients since we have not included medically compromised patients in our study. We also suggest a similar study in female population as we just included male patients in our study to reduce gender bias and on the basis of general perception that males are more prone to cardiovascular changes than females as males tend to hide their anxiety and fear during the dental procedures
Contributor Information
Ashish Sharma, Email: ashgdc06@yahoo.co.in, Email: drsiddhi.tripathi@gmail.com.
Rudraksh Pant, Email: rudrakshpant@gmail.com.
Sameer Priyadarshi, Email: sameerpriyadarshi@hotmail.com.
Nimish Agarwal, Email: nimish.agarwal9@gmail.com.
Siddhi Tripathi, Email: drashishsharma.omfs@gmail.com.
Manoj Chaudhary, Email: manojchaudhary15@gmail.com.
References
- 1.LilianiLiau F, Kuo R-C, Lin C-P, Chang H-H. Cardiovascular influence of dental anxiety during local anesthesia for tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:16–26. doi: 10.1016/j.tripleo.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 2.Brand HS, Gortzak RA, Palmer-Bouva CC, Abraham RE, Abraham IL. Cardiovascular and neuroendocrine responses during acute stress induced by different types of dental treatment. Int Dent J. 1995;45:45–48. [PubMed] [Google Scholar]
- 3.Brand HS, Abraham-lnpijn L. Cardiovascular responses induced by dental treatment. Eur J Oral Sci. 1996;104:245–252. doi: 10.1111/j.1600-0722.1996.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 4.Pallasch TJ (1998) Vasoconstrictors and the heart. J Calif Dent Assoc 26(9):668–673, 676 [PubMed]
- 5.Ogunlewe MO, James O, Ajuluchukwu JNA, Ladeinde AL, Adeyemo WL, Gbotolorun OM. Evaluation of haemodynamic changes in hypertensive patients during tooth extraction under local anaesthesia. West Indian Med J. 2011;60(1):91. [PubMed] [Google Scholar]
- 6.Neverlien PO. Normative data for Corah’s Dental Anxiety Scale (DAS) for the Norwegian adult population. Commun Dent Oral Epidemiol. 1990;18:162. doi: 10.1111/j.1600-0528.1990.tb00045.x. [DOI] [PubMed] [Google Scholar]
- 7.Corah NL, Gale EN, Illig SJ. Assessment of a dental anxiety scale. J Am Dent Assoc. 1978;97:816–819. doi: 10.14219/jada.archive.1978.0394. [DOI] [PubMed] [Google Scholar]
- 8.Kunzelmann K-H, Dtinninger P. Dental fear and pain: effect on patient’s perception of the dentist. Commun Dent Oral Epidemiol. 1990;18:264–266. doi: 10.1111/j.1600-0528.1990.tb00073.x. [DOI] [PubMed] [Google Scholar]
- 9.Sehwarz E. Dental anxiety in young adult Danes under alternative dental care programs. Seand J Dent Res. 1990;98:442–450. doi: 10.1111/j.1600-0722.1990.tb00996.x. [DOI] [PubMed] [Google Scholar]
- 10.Vassend O. Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther. 1993;31(7):659–666. doi: 10.1016/0005-7967(93)90119-F. [DOI] [PubMed] [Google Scholar]
- 11.Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. 1984;109:247–251. doi: 10.14219/jada.archive.1984.0328. [DOI] [PubMed] [Google Scholar]
- 12.De Jongh A, Muris P, Ter Horst G, Duyx MP. Acquisition and maintenance of anxiety: the role of experiences and cognitive factors. Behav Res Ther. 1995;33(2):205–210. doi: 10.1016/0005-7967(94)P4442-W. [DOI] [PubMed] [Google Scholar]
- 13.Ketabi M, Alaie M, Shamami MS, Shamami MS. Influence of local anesthetics with or without epinephrine 1/80000 on blood pressure and heart rate: a randomized double-blind experimental clinical trial. Dent Res J (Isfahan) 2012;9(4):437–440. [PMC free article] [PubMed] [Google Scholar]
- 14.Ryhänen JM, Kotilainen RM, Luotio K, Mattila MA. Lidocaine and prilocaine with vasoconstrictors as cause for cardiovascular reactions. A pulse oximetric study. Preliminary report. Oral Surg Oral Diagn. 1996;7:21–24. [PubMed] [Google Scholar]
- 15.de Holanda Vasconcellos RJ, do EgitoVasconcelos BC, Genú PR. Influence of local anesthethics with adrenalina 1:100.000 in basic vital constants during 3rd molar surgery. Med Oral Patol Oral Cir Bucal. 2008;13(7):E431–E437. [PubMed] [Google Scholar]
- 16.Blinder D, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients undergoing dental extractions under local anesthesia. J Oral Maxillofac Surg. 1996;54:162–165. doi: 10.1016/S0278-2391(96)90438-3. [DOI] [PubMed] [Google Scholar]
- 17.Brand HS. Cardiovascular responses in patients and dentists during dental treatment. Int Dent J. 1999;49(1):60–66. doi: 10.1111/j.1875-595X.1999.tb00509.x. [DOI] [PubMed] [Google Scholar]
- 18.Elad S, Admon D, MeiravKedmi E, Ayalon S, Tuchband A, Lutan H, Kaufman E. The cardiovascular effect of local anesthesia with articaine plus 1:200,000 adrenalin versus lidocaine plus 1:100,000 adrenalin in medically compromised cardiac patients: a prospective, randomized, double blinded study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:725–730. doi: 10.1016/j.tripleo.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Blinder D, Manor Y, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients having dental extractions under a local anesthetic containing a vasopressor. J Oral Maxillofac Surg. 1998;56(12):1399–1402. doi: 10.1016/S0278-2391(98)90403-7. [DOI] [PubMed] [Google Scholar]
- 20.Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Invest Dent. 2016;8:35–50. doi: 10.2147/CCIDE.S63626. [DOI] [PMC free article] [PubMed] [Google Scholar]


