Abstract
Aim
Athletes who suffer sport‐related concussions but continue playing have a high probability of experiencing more severe symptoms with any subsequent concussion. This study used data from the authors’ clinical department to retrospectively investigate the clinical characteristics of sport‐related concussion and factors associated with delays in examinations.
Methods
The study included 38 patients with sport‐related concussions who were treated at the authors’ hospital. The sports during which the injuries occurred, occasions of injury, factors affecting the time from injury until examination at hospital, and prognoses were evaluated retrospectively.
Results
Sport‐related concussions most frequently occurred in rugby and judo, where tackling, throwing, and other types of physical contact can result in impacts to the head region at high angular or linear velocity with acceleration. Some subjects showed consciousness disturbance and/or clear subjective symptoms immediately after the injury and were therefore examined at the hospital rapidly. However, other subjects who suffered amnesia or less obvious symptoms continued to play after the injury and had delayed examinations. In addition, there was a tendency for examinations to be delayed when an on‐site physician was present.
Conclusions
In contact sports where injury‐resulting events occur, such as impacts to the head at high angular or linear velocity with acceleration, athletes should be immediately withdrawn from play and evaluated for concussion, even if there are no obvious head injuries or symptoms. The immediate ascertainment of symptoms after physical contact would improve the rapid detection of sport‐related concussion.
Keywords: Athlete, concussion, sports, trauma, consciousness
Introduction
In the USA, 3.8 million athletes per year experience a sport‐related concussion (SRC),1 which accounts for 5–9% of sport‐related injuries.2 If an athlete continues to play despite suffering a SRC, his or her risk of suffering another SRC within the same season is increased by approximately threefold.3 Most patients recover from SRC symptoms within 7–10 days.4 In addition, symptoms such as consciousness disturbance can increase in severity if another SRC occurs before full recovery from the symptoms.5 Furthermore, repeated concussions can lead to cognitive function disorders and chronic traumatic encephalopathy, such as Parkinsonism.6 In addition, some patients diagnosed with concussion also have shallow acute subdural hematoma; if such patients suffer additional head impact, expansion of the subdural hematoma could occur and can be fatal.7, 8 Therefore, if concussion is suspected while taking part in sports, it is essential for the athlete to immediately leave the match and undergo examination at a medical institution. Even if the athlete subsequently resumes play, it is important to give him or her appropriate instructions in accordance with the “Concussion Consensus Guidelines to Help Safe Return of Athletes to Play,” which is a graduated return‐to‐play protocol published by the Centers for Disease Control and Prevention.9, 10
Trainers who are involved with sport are greatly concerned about SRC.11 The Sport Concussion Assessment Tool (SCAT), which was developed by the Concussion in Sport Group, is now widely used as a tool for making such judgments.12 In addition, Nagahiro et al.13 have made recommendations for medical professionals about neurosurgeons’ handling of sport‐related external head injuries. Nevertheless, in clinical practice, examinations by medical institutions are often carried out a considerable time after the injury occurs, and it cannot be denied that medical professionals are slow in recognizing the importance of rapid detection of SRC. Furthermore, when there are no obvious symptoms, such as consciousness loss, marked dizziness, or other subjective symptoms, there is often uncertainty in ascertaining the presence or absence of concussion and whether the athlete should be withdrawn from play.
Considering these issues, we undertook a retrospective study of SRC cases that were treated at the authors’ institution. We investigated the clinical characteristics of SRC and factors associated with delays in examination.
Subjects and methods
Of the 3,834 cases of head injury examined at the Department of Traumatology and Critical Care Medicine, University of Miyazaki Hospital (Miyazaki, Japan), between April 2012 and March 2016, 58 (1.5%) were sport‐related. This cohort included 50 male and 8 female patients, and the mean age was 21.9 ± 12.5 years. Of these subjects, 38 had concussions and were included in the study. The other 20 patients were excluded from this study because they had no symptoms suggesting cerebral concussion, only bruises or lacerations of the scalp. The 38 cases with concussions were evaluated retrospectively; information regarding sports during which the injuries occurred, the occasions of injury, factors affecting time from injury until examination at hospital, and prognosis was obtained from the medical records (Fig. 1).
Figure 1.
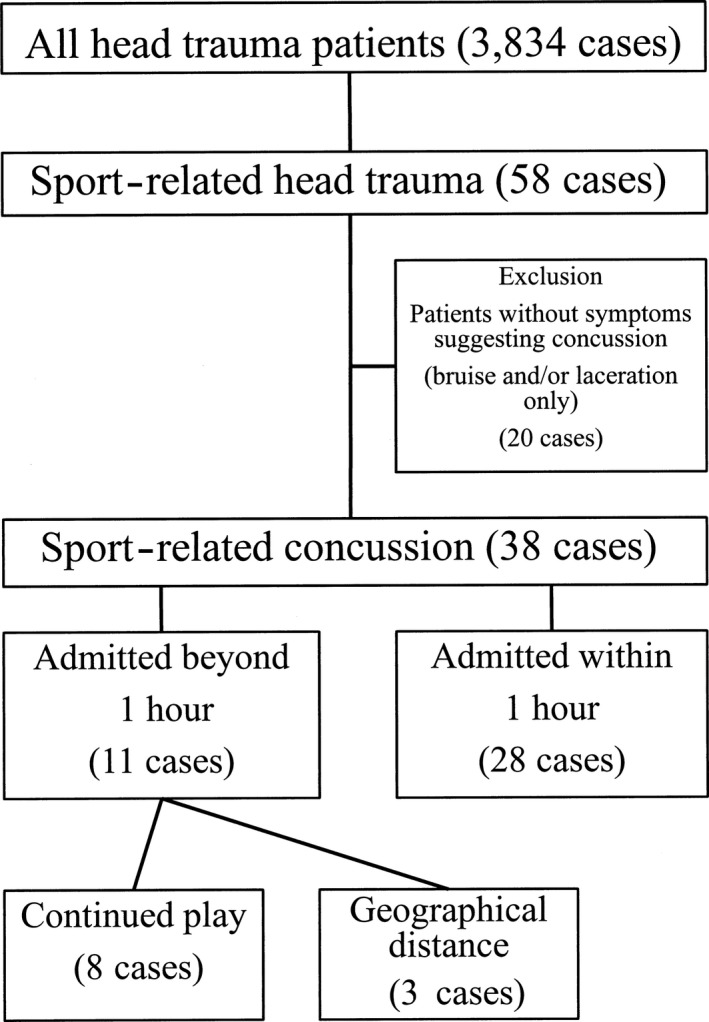
Flow chart of the patients included in this study.
In this study, only the patients who met the following four criteria were diagnosed with cerebral concussions: (i) the patient hit his or her head, (ii) the patient had symptoms suggesting cerebral concussion, such as loss of consciousness, headache, nausea, vomiting, amnesia, dizziness, vertigo, blurred vision, and disorientation, (iii) these symptoms did not exist before the patient hit his or her head, (iv) there were no intracranial lesions related to the head trauma. All patients were examined for the absence of intracranial lesions related to the head trauma by computed tomography scan immediately after admission. We defined “time from injury to hospital” as the time from injury to examination by a physician.
Statistical analysis was carried out using GraphPad Prism (GraphPad Software, La Jolla, CA). Three groups were compared using the non‐parametric Kruskal–Wallis test, with significant set at P < 0.05. Because the number of subjects in this study was small, multivariate analysis was not carried out.
Results
The sport responsible for the largest number of concussions was rugby, which had 18 cases (47.4%), followed by judo with eight cases (21.1%). Fifty‐seven percent of all patients were injured during matches (Table 1). The causes of injury included tackling (10 cases, 35.7%), throwing (eight cases, 21.0%), falling down (seven cases, 18.4%), being kicked (four cases, 12.5%), and other contact (six cases, 15.7%). In three cases, the mechanism of injury was unknown because of amnesia. The amount of time until arrival at the hospital differed significantly between subjects who came to hospital themselves and those who were brought in as emergencies (P = 0.04; Fig. 2). In addition, subjects brought in as emergencies showed significantly higher rates of consciousness disturbance than those who arrived on their own (Fig. 3). On examination at the hospital, the symptoms most commonly associated with concussion‐like behavior were headache (with or without nausea and/or vomiting), followed by amnesia, disorientation/incoherent speech, loss of strength and/or numbness in the arms, vertigo/dizziness, laceration of the scalp, blurred vision, and unusual behavior (Table 2).
Table 1.
Causative sports for cerebral concussion among 38 cases in Japan
| Sports that caused concussion | No. of cases (%) |
|---|---|
| Rugby | 18 (47.4) |
| Judo | 8 (21.1) |
| Soccer | 4 (10.6) |
| Karate | 3 (7.9) |
| Baseball | 1 (2.6) |
| Bicycle race | 1 (2.6) |
| Handball | 1 (2.6) |
| Equestrianism | 1 (2.6) |
| Skate board | 1 (2.6) |
Figure 2.
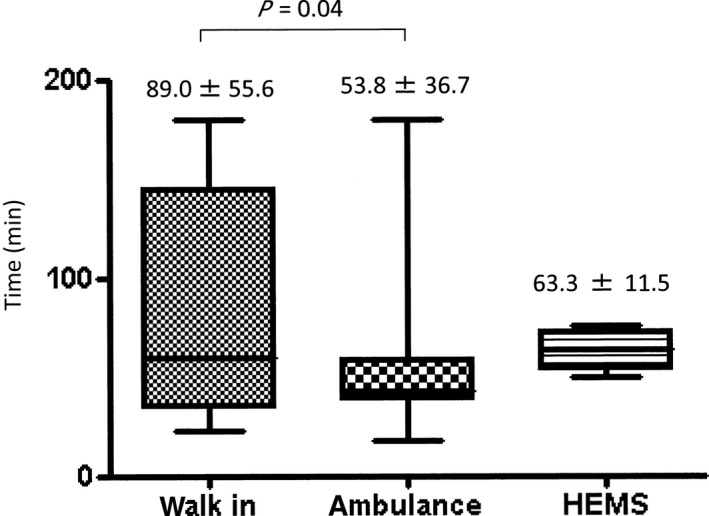
Time from injury until hospital examination among 38 cases of sport‐related concussion. HEMS, helicopter emergency medical system.
Figure 3.
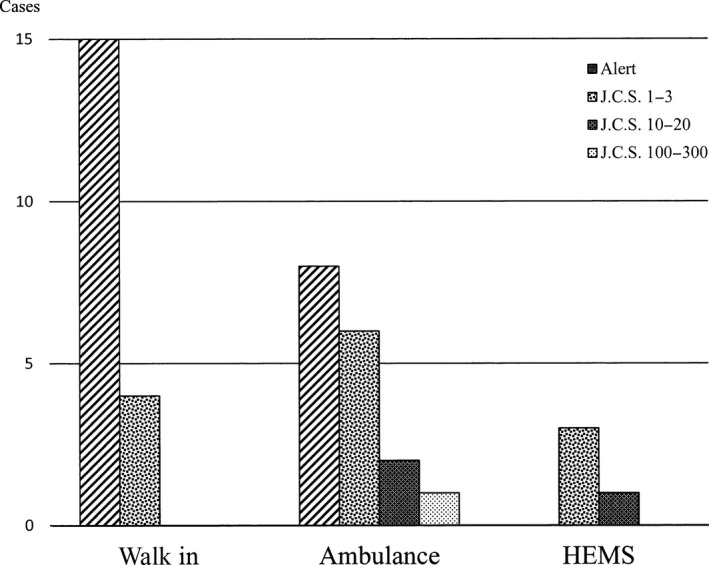
Consciousness disturbance and method of transport to hospital among 38 cases of sport‐related concussion. HEMS, helicopter emergency medical system; J.C.S., Japan Coma Scale.
Table 2.
Symptoms other than consciousness disturbance for hospital admission following sport‐related injury
| Symptoms | Cases |
|---|---|
| Headache/nausea/vomiting | 23 |
| Amnesia/loss of memory during play | 8 |
| Incoherent speech/disorientation | 6 |
| Weakness/numbness of upper limb | 3 |
| Laceration of scalp | 2 |
| Blurred vision | 1 |
| Unusual behavior | 1 |
For 11 subjects, one or more hours elapsed between the injury and examination at the hospital; three of these delays were due to the geographical distance between the sport location and the medical institution. However, for the other eight subjects, no concussion symptoms were found immediately after their injuries; therefore, the subjects continued to play. For these subjects, the symptoms that did eventually lead to medical examination included incoherent speech, unusual behavior, loss of memory during play, headache, and vomiting, which presented during an intermission in play (Table 2). In addition, three subjects were diagnosed as having SRC when examined after completion of the match; their symptoms included loss or deterioration of memory. Furthermore, for four subjects, 4 h or more elapsed between the injury and examination; their most common symptoms were headache, nausea, and dizziness (data not shown).
In this study, 18 subjects (46.15%) were hospitalized for continued observation. However, their symptoms had ceased by the following day, and their prognosis was favorable. When an on‐site physician intervened at the scene, the time until examination at the hospital tended to be longer; however, no significant difference was found in this study. Overall, there was wide variability in the time until examination at hospital (Fig. 4).
Figure 4.
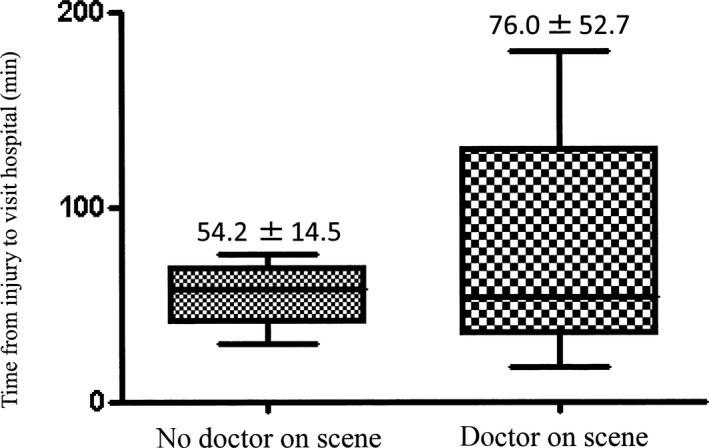
Difference in time from injury to hospital admission among 38 cases of sport‐related concussion, grouped according to the presence or absence of an on‐site physician.
Discussion
In this study, rugby and judo resulted in the most cases of SRC. The most common causes of injury involved head impact at high angular or linear velocity with acceleration, such as tackling, throwing, or other physical contact. Subjects who suffered consciousness disturbance and/or clear subjective symptoms immediately after injury were rapidly examined at medical institutions. However, there were also cases of athletes continuing to play after suffering injuries, which resulted in delays in examination.
American football and rugby most frequently resulted in SRC in the USA, whereas judo and other sports were reported to cause most SRC cases in Japan.14, 15 In these sports, the most common injuries were head impacts at high angular or linear velocity with acceleration. The most common time at which these events occurred was during the first years of high school and junior high school, which means that beginners in sports tend to suffer these events.16, 17 Consistent with previous findings, our study found that SRC occurs most frequently in connection with actions such as jolting of the head, which occurs in rugby and judo.
Rapid detection of SRC during play and rapid examination at an appropriate medical institution are important in order to not miss any intracranial hematomas, which can develop as complications resulting from head injuries. It is also important to provide appropriate instructions for resuming play in order to avoid increased SRC severity and chronic traumatic encephalopathy. If consciousness disturbance develops after injury and is associated with a superficial wound and clear subjective symptoms then rapid examination at a medical institution is required. However, it is difficult to determine whether rapid examination is required in situations where a fall or physical contact has occurred, but the presence of head injury and associated amnesia is uncertain, and the athlete continues to play.
The 5th version of SCAT, a tool for concussion diagnosis in the field, is now in wide use among sport coaches, health‐care providers, and field doctors. The use of SCAT involves making judgments on‐site immediately after the injury has occurred in the following five steps12:
Step 1: Judging the presence or absence of red‐flag signs.
Step 2: Ascertaining the subjective symptoms.
Step 3: Testing memory strength using the Maddocks questions.
Step 4: Assessment on the basis of the Glasgow Coma Scale.
Step 5: Assessment of the cervical vertebrae.
In addition, after evaluation at the site of injury, evaluation by the following six steps should be carried out at the first‐aid station:
Step 1: Assessment of the athlete's background.
Step 2: Confirmation of symptoms.
Step 3: Screening of cognitive function.
Step 4: Neurological evaluation.
Step 5: Evaluation of memory retrieval.
Step 6: Overall judgment on the presence or absence of concussion.
There have also been reports of evaluation methods other than the above used at locations where SRC occurs.5 Although several different tools are used to make on‐site judgments about concussions, they all share the feature of initiating confirmation when concussion‐related symptoms are suspected. The 4th and 5th International Conferences on Concussion in Sport defined concussion as “a complex pathophysiological process affecting the brain, induced by a biomechanical force to the head.”9, 10 The symptoms vary but frequently include headache and dizziness. In addition, symptoms could include amnesia, confusion, balance disturbance, blurred vision, photophobia, numbness, emotional disorder (increasing irritability), and less frequently, consciousness disturbance.9, 18, 19, 20 Thus, unless a patient clearly suffers a forceful impact on the head and loses consciousness or complains of subjective symptoms, even if various symptoms are suspected during play, it is difficult to make the judgment that the athlete should be withdrawn from play in order to confirm the presence or absence of SRC. Therefore, the findings in the present study suggest that, when head collision occurs at high angular or linear velocity with acceleration, even if there is no clear head injury, athletes should be withdrawn from play to ascertain the presence or absence of concussion symptoms. This will be useful for the rapid detection of SRC.
Finally, although we could not obtain significance because of the small sample size in this study, we found that the time period before hospital examination occurs tends to be extended if an on‐site physician is present. A possible reason for this is that on‐site physicians might have insufficient recognition of and understanding about concussion; as a result, the physician might instruct a patient to rest while being observed by the physician, then allow the athlete to resume play instead of going to the hospital for examination. However, this issue requires further investigation.
A limitation of this study is that the number of subjects was too small for multivariate analysis of potential factors affecting the time from injury to examination at hospital.
Conclusions
In conclusion, in contact sports where there are injuries involving head impact at high angular or linear velocity with acceleration, even if there is no clear head injury or symptoms, proactive withdrawal of the athlete from play and ascertainment of the presence or absence of concussion symptoms will lead to more rapid SRC detection. On the basis of the current study, even if concussion symptoms are not clearly evident, it is important to immediately withdraw athletes from play and ascertain the presence or absence of concussion symptoms if head impact at high angular velocity has occurred. The results of this study will provide useful information for emergency physicians who are dispatched as on‐site physicians at sport events, so that they can avoid the main pitfalls related to SRC evaluation.
Disclosure
Approval of the research protocol: The protocol for this research project was approved by a suitably constituted Ethics Committee of the institution and conforms to the provisions of the Declaration of Helsinki (Committee of University of Miyazaki, Approval No. 0‐0074).
Informed consent: All informed consent was obtained by opt‐out in publicity documents from the subjects or guardians.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Conflict of interest: None.
Funding Information
No funding information provided
References
- 1. Langlois JA, Rutland‐Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: A brief overview. J Head Trauma Rehabil. 2006; 21: 375–8. [DOI] [PubMed] [Google Scholar]
- 2. Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States High school and collegiate athletes. J Athl Train. 2007; 42: 495–503. [PMC free article] [PubMed] [Google Scholar]
- 3. Guskiewicz KM, Wiaver NL, Padua DA, Garrett WE Jr. Epidemiology of concussion in collegiate and high school football player. Am. J. Sports Med. 2000; 28: 643–50. [DOI] [PubMed] [Google Scholar]
- 4. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am. J. Sports Med. 2012; 40: 747–55. [DOI] [PubMed] [Google Scholar]
- 5. Hobbs JG, Young JS, Bailes JE. Sports‐related concussions: Diagnosis, complications, and current management strategies. Neurosurg. Focus 2016; 40: 1–14. [DOI] [PubMed] [Google Scholar]
- 6. Rabadi MH, Jordan BD. The cumulative effect of repetitive concussion in sports. Clin. J. Sport Med. 2001; 11: 194–8. [DOI] [PubMed] [Google Scholar]
- 7. Cantu RC, Gean AD. Second‐impact syndrome and a small subdural hematoma: An uncommon catastrophic result of repetitive head injury with a characteristic imaging appearance. J. Neurotrauma 2010; 27: 1557–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McCrory PR, Davis G, Makdissi M. Second impact syndrome or cerebral swelling after sporting head injury. Curr Sports Med Rep. 2012; 11: 21–12. [DOI] [PubMed] [Google Scholar]
- 9. McCrory P, Meeuwisse WH, Aubry M. et al. Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport held in Zurich, November 2012. J. Am. Coll. Surg.. 2013; 216: e55–71. [DOI] [PubMed] [Google Scholar]
- 10. McCrory P, Meeuwisse WH, Dvořák J et al. 5th International Conference on Concussion in Sport (Berlin). Br. J. Sports Med.. 2017; 51: 837. [DOI] [PubMed] [Google Scholar]
- 11. Ogino M, Kawamoto T, Shingo T, Kim P. Sports‐related head injuries: Management and future problems. Jpn J Neurosurg. 2017; 26: 195–9. [Google Scholar]
- 12. Echemendia RJ, Meeuwisse W, McCrory P et al The sport concussion assessment tool 5th edition (SCAT5): Background and rationale. Br. J. Sports Med.. 2017; 51: 848–50. [DOI] [PubMed] [Google Scholar]
- 13. Nagahiro S, Tani S, Ogino M et al Neurosurgical management of sports‐related head injuries —Interim consensus statement for guideline development. Neurotraumatology. 2013; 36: 119–28. [Google Scholar]
- 14. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics 2010; 126: e550–6. [DOI] [PubMed] [Google Scholar]
- 15. Ogino M, Kawamoto T, Kim P. Head and neck injuries in sports: Overview. Jpn J Neurosurg. 2004; 13: 96–103. [Google Scholar]
- 16. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J Athl Train. 2007; 42: 311–9. [PMC free article] [PubMed] [Google Scholar]
- 17. Lincoln AE, Hinton RY, Almquist JL, Lager SL, Dick RW. Head, face, and eye injuries in scholastic and collegiate lacrosse: A 4‐year prospective study. Am. J. Sports Med. 2007; 35: 207–15. [DOI] [PubMed] [Google Scholar]
- 18. Mansell JL, Tierney RT, Higgins M, McDevitt J, Toone N, Glutting J. Concussive signs and symptoms following head impacts in collegiate athletes. Brain Inj. 2010; 24: 1070–4. [DOI] [PubMed] [Google Scholar]
- 19. McCrory P. When to retire after concussion? Br. J. Sports Med. 2001; 35: 380–2. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20. Meehan WP III, d'Hemecourt P, Comstock RD. High school concussions in the 2008‐2009 academic year: Mechanism, symptoms, and management. Am. J. Sports Med. 2010; 38: 2405–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


