Abstract
The aim of the present study was to investigate the function of microRNA-146b on myocardial infarction and the mechanism. An MTT assay, Annexin V/propidium iodide (PI) apoptosis assay, ELISA kits, western blot analysis and a caspase-3/8 activity assay were used to measure cell growth, vascular apoptosis inflammatory factors, and the B-cell lymphoma 2-associated X protein (Bax), phosphatase and tensin homolog (PTEN), phosphoinositide 3-kinase (PI3K)/Akt/nuclear factor (NF)-κB signaling pathway. The expression of microRNA-146b was downregulated in the myocardial infarction rat model, compared with the control group. In an in vitro model of myocardial infarction, the downregulation of microRNA-146b increased inflammatory factors, vascular apoptosis, caspase-3/8 activity and the protein expression of Bax. MicroRNA-146b reduced vascular apoptosis, caspase-3/8 activity and the protein expression of Bax. MicroRNA-146b also regulated the PI3K/Akt/NF-κB signaling pathway to mediate vascular inflammation and apoptosis in myocardial infarction by PTEN. A PI3K inhibitor decreased the effect of microRNA-146b on vascular inflammation and apoptosis following myocardial infarction. In conclusion, microRNA-146b mediated vascular inflammation and apoptosis in patients with myocardial infarction, which may be associated with activation of the PI3K/Akt/NF-κB signaling pathway by PTEN.
Keywords: microRNA-146b, vascular apoptosis, phosphatase and tensin homolog, myocardial infarction, phosphoinositide 3-kinase, Akt, nuclear factor-κB
Introduction
Cardiac failure, a complex clinical syndrome, represents the serious stage of several heart diseases (1). It has a high incidence, with a 5-year mortality rate of >50% (1). The incidence of cardiac failure has continued to increase in recent years, posing a serious threat to human health in the 21st century. As myocardial infarction is a serious threat to human health (2), how to effectively reduce the cell apoptosis caused by myocardial injury and protect cardiac function remains an important question in the clinical cardiovascular field (2). Myocardial infarction leads to markedly increased myocardial ischemia hypoxia, inflammation, oxidative stress, and myocardial cell necrosis and apoptosis (3). As a result, it causes myocardial collagen hyperplasia, alternative fibrosis and cardiac function disorder (3).
Cell apoptosis occupies an important position in the process of the pathological evolution of myocardial ischemia injury (4). In early acute ischemia, apoptosis is the main form of myocardial infarction (5). It is associated with the entire pathological evolution process of myocardial injury. Inhibiting myocardial cell apoptosis following acute heart ischemia, and increasing the quantity of surviving myocardial cells is undoubtedly conducive to the prevention and treatment of myocardial ischemia (6). In addition, it can promote the recovery of cardiac function, and the long-term prognosis of patients (5).
The phosphoinositide 3-kinase (PI3K)/akt pathway is an important signal transduction pathway in organisms. It has been confirmed to exert important biological functions in activities including cell survival, apoptosis and proliferation (7). PI3K can phosphorylate the 3′ hydrogen base on the inositol ring to produce phosphatidylinositol 3,4,5 trisphosphate (PIP3), which can be activated following the phosphorylation of AKT as a secondary messenger (8). The phosphorylated AKT can activate endothelial nitric oxide synthase, glycogen synthase kinase-3β and heat shock protein. Therefore, it can exert myocardial protective effects (9). It has been verified in experiments in vivo and in vitro that the PI3K/AKT signal transduction pathway is important in protecting against myocardial ischemia reperfusion injury (9). Ischemic preconditioning or active drug stimulation can activate the PI3K/AKT signaling pathway in myocardial cells. The activation of such a signal pathway has a decisive role in the protective mechanism of myocardial ischemia reperfusion injury (10).
As an important nuclear transcription factor, nuclear factor (NF)-κB is a transcription factor for fast response nucleated cells commonly distributed in the cytoplasm. It locates at the hub location of the Toll-like receptor downstream signal pathway. In addition, it can regulate the cascade reaction between immunity and inflammation associated factors and inflammatory transmitters. Therefore, it can synthesize and release inflammatory cytokines, cyclooyxgenase-2, inducible nitric oxide synthase, chemotaxis granulocytes and macrophages. Subsequently, it can increase capillary permeability, induce lymphocyte infiltration, and complete the transmission of inflammatory signals. In addition, it can exert the early immune response effects and is pivotal in inflammatory and immune responses. Myocardial ischemia and hypoxia can induce myocardial inflammation, whereas the phosphorylation and degradation of NF-κB subunit inhibitor of NF-κB (IκB) leads to the nuclear translocation of NF-κB. This accounts for the initiation mechanism of the genesis and development of acute inflammation. NF-κB is a type of transcription factor with a multi-directional regulatory effect. It can regulate the expression of multiple inflammatory cytokines, therefore, it is closely associated with the inflammatory response (11).
Among the numerous signal transduction pathways, the phosphatase and tensin homolog (PTEN) pathway is closely correlated with PI3K/AKT (12). PI3K/AKT can be gradually phosphorylated through activating the enzyme system (13). Therefore, it can activate pathway regulatory cytokines, including vascular endothelial growth factors. PTEN is the tumor suppressor gene, phosphatase and tensin homolog deleted on chromosome 10, and is the negative regulatory factor of the PI3K/AKT pathway (13). PTEN can suppress activation of the PI3K/AKT pathway and catalyze the dephosphorylation of PIP3. Thus, it can antagonize the activity of the PI3K/AKT pathway (14). Therefore, PTEN is important in regulating embryonic development, cell growth, differentiation, apoptosis and migration (14). Ramirez-Moya et al showed that microRNA-146b promoted PI3K/AKT pathway hyperactivation and thyroid cancer progression by targeting PTEN (15). Hendgen-Cotta et al (16) showed that microRNA-146b was inhibited in acute myocardial ischemia/reperfusion injury in vivo. In the present study, the function of microRNA-146b in myocardial infarction and the underlying mechanism were evaluated.
Materials and methods
Animals and acute myocardial I/R (AMI) injury
Sprague-Dawley rats (male; 5–6 weeks; 160–200 g) were housed at 22–23°C and a humidity of 55–60%, with a 12 h light/dark cycle and free access to food and water. All rats were obtained from the Experiment Animal Center of Shandong University (Shandong, China) and were divided into two groups randomly: Control (n=6) and AMI (n=6) groups. The rats were anesthetized by intraperitoneal injection of 35 mg/kg pentobarbital sodium. Thoracotomy was performed and the left anterior descending coronary artery was ligated 2–3 mm away for 30 min. All experimental manipulations were undertaken in accordance with the Guide for the Care and Use of Laboratory Animals by the National Institutes of Health, with the approval of the Animal Experimental Ethics Committee of Jining No. 1 People's Hospital (Jining, China).
Hematoxylin and eosin (HE) staining assay
Following induction for 30 min, the rats were anesthetized by intraperitoneal injection of 35 mg/kg pentobarbital sodium and sacrificed via decollation. Heart samples were acquired and fixed with 4% paraformaldehyde for 24 h. The heart samples were then embedded in plastic and sectioned at 10-µM. The samples were stained with an HE assay for 15 min and observed using a confocal microscope (magnification, ×100; Leica Microsystems GmbH, Wetzlar, Germany).
Reverse transcription-polymerase chain reaction (RT-PCR) and quantitative PCR (qPCR) analysis
Total RNA was extracted from the transfected cells using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) and total RNA was used for the synthesis of first-strand cDNA using the PrimeScript RT reagent kit (Takara Bio, Inc., Shiga, Japan). The RT-PCR analysis was performed using a 7500 Fast real-time PCR system and SYBR Premix Ex Taq kit (Takara Bio, Inc.). The primers utilized were as follows: U6 forward, 5′GCTTCGGCAGCACATATACTAAAAT3′ and reverse, 5′CGCTTCACGAATTTGCGTGTCAT3′; miR-146b-5p forward, 5′-TGACCCATCCTGGGCCTCAA-3′ and reverse, 5′-CCAGTGGGCAAGATGTGGGCC-3′. The amplification conditions were as follows: 95°C for 10 min, 40 cycles of denaturation at 95°C for 30 sec, followed by annealing and extension at 58°C for 10 sec, 72°C for 10 sec. The 2−ΔΔCq method was used to calculate the relative gene expression (17).
GeneChip miRNA array
Total RNA (500 ng) was isolated using Cyanine-5-CTP and hybridized into the SurePrint G3 Mouse Whole Genome GE 8×_60 K Microarray G4852A platform (Stratagene; Agilent Technologies, Inc., Santa Clara, CA, USA). The results were quantified using Agilent Feature Extraction software (version A.10.7.3.1).
Cell culture and transfection
H9c2 cells were purchased from Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China) and cultured in Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.) at 37°C in a 95% air/5% CO2 atmosphere. The H9c2 cells were incubated by continuously flushing a chamber with 5% CO2 and 95% N2 for 3 h at 37°C. MicroRNA-146b mimics, si-microRNA-146b and negative control mimics were transfected into cells; transfection was performed with Lipofectamine™ 2000 reagent (Invitrogen; Thermo Fisher Scientific, Inc.). Following 4 h of transfection, VO-Ohpic trihydrate (10 µM; PTEN inhibitor) was added to cells for 44 h.
Cell viability assay and Annexin V/propidium iodide (PI) apoptosis assay
To the transfected cells, 20 µl of MTT assay was added for 4 h at 37°C and DMSO was added to the cell and shaken at 37°C for 20 min. The cell viability was measured using a VERSAmax microplate reader (Molecular Devices LLC; Sunnyvale, CA, USA) at 492 nm. The transfected cells were washed with PBS, and stained with Annexin V-FITC and PI fluorescence (all 5 µl, BD Biosciences, Franklin Lakes, NJ, USA) for 15 min in the dark. Apoptosis was analyzed with a FACSCalibur flow cytometer (BD Biosciences).
ELISA
The transfected cells were lysed with modified radioimmunoprecipitation assay (RIPA) buffer at 4°C for 30 min. Protein concentration was determined using the BCA protein determination kit (Beyotime Institute of Biotechnology, Shanghai, China), and 10 µg was used to measure the levels of TNF-α, IL-1β, IL-6 and IL-18 using ELISA kits. The absorbance was measured using a VERSAmax microplate reader (Molecular Devices, LLC) at 405 nm.
Luciferase assay
The potential binding sites of miR146b in the 3′-untranslated region (UTR) of PTEN were determined using TargetScan (http://www.targetscan.org/vert_71). The pGL3-PTEN-3′-UTR and microRNA-146b and negative control mimics were added to cells, with transfection performed with Lipofectamine™ 2000 reagent (Invitrogen; Thermo Fisher Scientific, Inc.). Following transfection 48 h, the cells were analyzed with the Dual-Luciferase Reporter Assay kit (Promega Corporation, Madison, WI, USA).
Western blot analysis and caspase-3/8 activity assay
The transfected cells were lysed with modified RIPA buffer at 4°C for 30 min. Protein concentration was determined using the BCA protein determination kit (Beyotime Institute of Biotechnology), and 30–50 µg of the protein samples were electrophoresed on 8–12% SDS-PAGE gels and transferred onto PVDF membranes (EMD Millipore, Billerica, MA, USA). Subsequently, 5% milk was used to block the membranes in a shaker at 37°C for 1 h. Antibodies for Bax (cat. no. sc-6236, 1:1,000), phosphorylated Akt (cat. no. sc-7985-R, 1:1,000), PI3K (cat. no. sc-7174, 1:1,000), NF-κB (p65, cat. no. sc-109, 1:1,000) and GAPDH (cat. no. sc-25778, 1:5,000) antibodies, all from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA) were used for incubation at 4°C overnight. The membranes were then washed with TBST buffer and incubated with horseradish peroxidase-labeled goat anti-rabbit IgG (cat. no. sc-2004, 1:5,000, Santa Cruz Biotechnology) at 37°C for 1 h. The protein bands were visualized by ECL (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
For the analysis of caspase activity, total protein (3–5 µg) was incubated with caspase-3 and caspase-8 activity kits (Beyotime Institute of Biotechnology) at 37°C for 1 h. Caspase-3/8 activity was measured using a VERSAmax microplate reader (Molecular Devices, LLC) at 405 nm.
Statistical analysis
The data are presented as the mean ± standard deviation using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). All data were analyzed for significance using Student's t-test for two groups or one-way analysis of variance with Tukey's post hoc test (three groups). P<0.05 was considered to indicate a statistically different difference.
Results
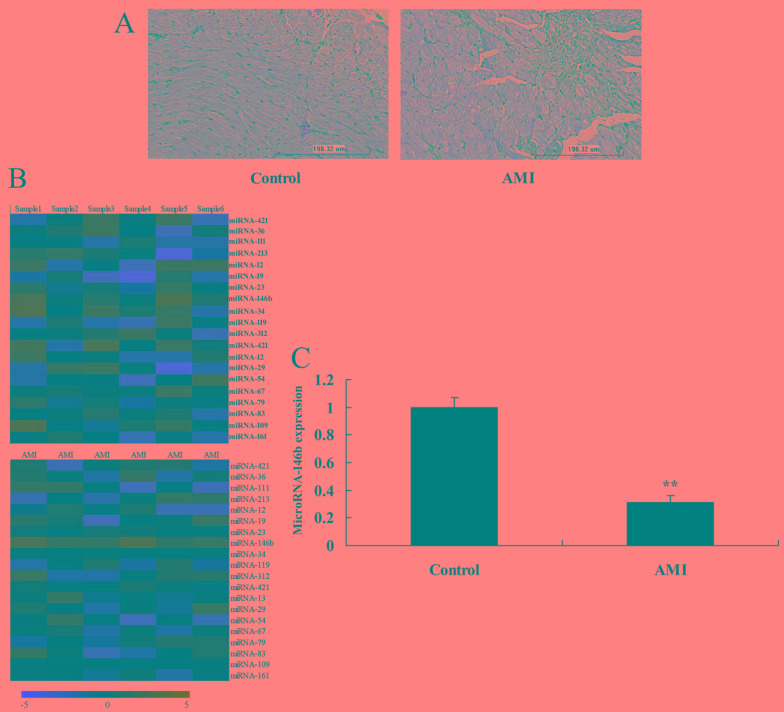
Expression of microRNA-146b in the AMI rat
To determine whether the expression of microRNAs regulates myocardial infarction in the AMI rat model, changes in the expression of microRNAs were analyzed. The HE staining showed myocardial damage in the AMI rat model, compared with the sham control group (Fig. 1A). The expression of microRNA-146b was downregulated in the myocardial infarction rat, compared with that in the control group (Fig. 1B and C).
Figure 1.
Expression of microRNA-146b in myocardial infarction rat. (A) Hematoxylin and eosin staining showed myocardial sdamage. Expression of microRNA-146b using a (B) gene chip and (C) polymerase chain reaction analysis. **P<0.01, vs. sham control group. Control, sham control rat group; AMI, acute myocardial infarction rat group.
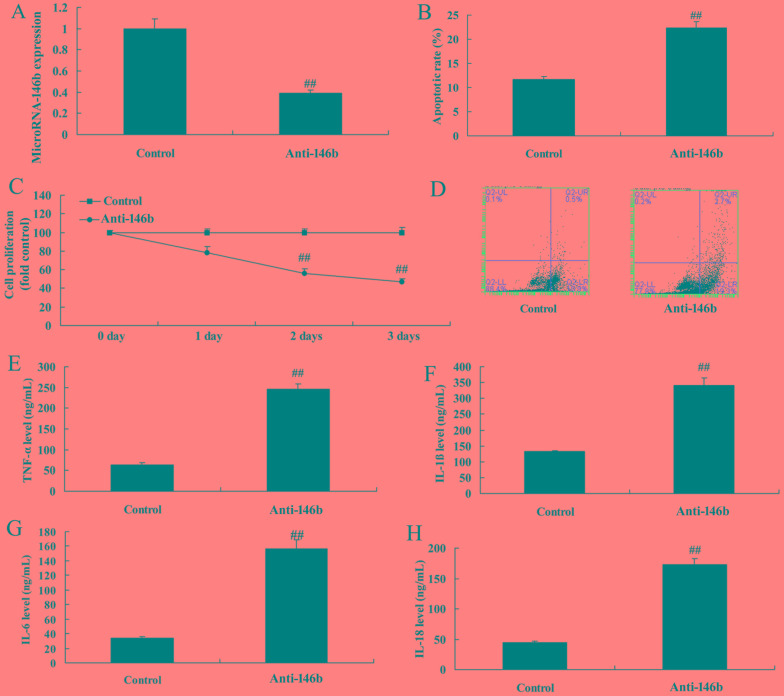
Downregulation of microRNA-146b increases inflammatory factors and apoptosis in vitro
The function of microRNA-146b in myocardial infarction was then examined using anti-microRNA-146b mimics to decrease the expression of microRNA-146b in the in vitro model. As shown in Fig. 2A, there was significant inhibition of the expression of microRNA-146b in the in vitro model in the anti-microRNA-146b mimics group, compared with that in the negative control group. The downregulation of microRNA-146b inhibited cell viability, induced apoptosis, increased levels of inflammatory factors TNF-α, IL-1β, IL-6 and IL-18, and increased apoptosis in the in vitro model, compared with the negative control group (Fig. 2B-H).
Figure 2.
Downregulation of microRNA-146b increases inflammatory factors and apoptosis in an in vitro model. (A) Expression of microRNA-146b, (B) vascular apoptotic rate, (C) cell viability, and (D) vascular apoptosis, detected using flow cytometry, of myocardial infarction. Levels of (E) TNF-α, (F) IL-1β, (G) IL-6 and (H) IL-18 in the in vitro model. ##P<0.01, vs. Control group. Control, negative control group; Anti-146b, microRNA-146b downregulation group; TNF-α, tumor necrosis factor-α; IL, interleukin.
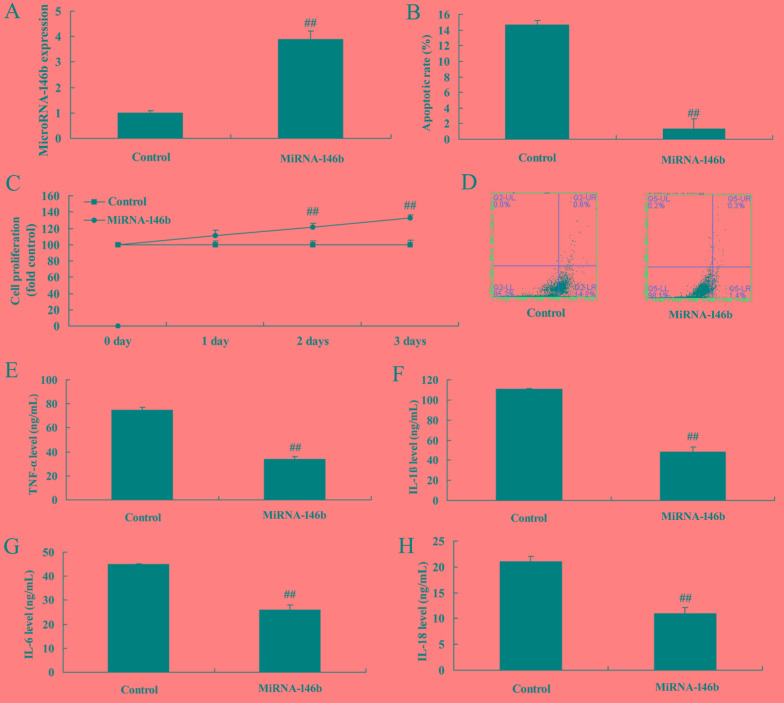
Upregulation of microRNA-146b decreases inflammatory factors and apoptosis in the in vitro model
There was a significant increase in the expression of microRNA-146b in the in vitro model following transfection with the microRNA-146b mimics, compared with the negative control group (Fig. 3A). The upregulation of microRNA-146b promoted cell viability, reduced apoptosis, decreased levels of inflammatory factors TNF-α, IL-1β, IL-6 and IL-18, and decreased apoptosis in the in vitro model, compared with the negative control group (Fig. 3B-H).
Figure 3.
Upregulation of miRNA-146b decreases inflammatory factors and apoptosis in an in vitro model. (A) Expression of miRNA-146b, (B) vascular apoptotic rate, (C), cell viability, and (D) vascular apoptosis, detected using flow cytometry, of myocardial infarction. Levels of (E) TNF-α, (F) IL-1β, (G) IL-6 and (H) IL-18 in the in vitro model. ##P<0.01, vs. Control group. Control, control negative group; miRNA-146b, microRNA-146b upregulation group; TNF-α, tumor necrosis factor-α; IL, interleukin.
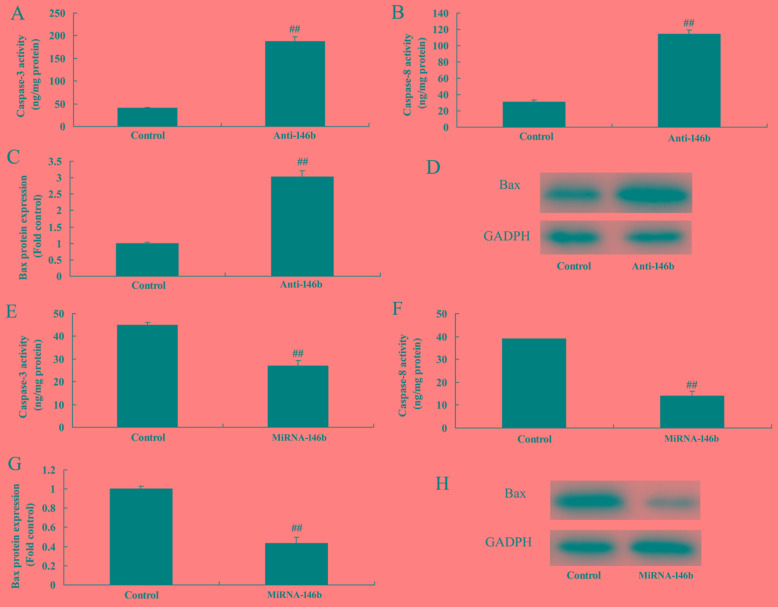
MicroRNA-146b regulates the Bax/caspase-8/caspase-3 signaling pathway in vitro
The present study also assessed whether microRNA-146b regulated the Bax/caspase-3/caspase-9 signaling pathway in the in vitro model. As shown in Fig. 4A-D, the downregulation of microRNA-146b significantly induced caspase-3/8 activity and the protein expression of Bax in the in vitro model, compared with the negative control group. The upregulation of microRNA-146b significantly suppressed the protein expression of Bax and activity of caspase-3/8 in the in vitro model, compared with levels in the negative control group (Fig. 4E-H).
Figure 4.
miRNA-146b regulates the Bax/caspase-8/caspase-3 signaling pathway in the in vitro model. Effects of downregulation of miRNA-146b on the activity of (A) Caspase-3 and (B) Caspase-8, and (C) protein expression of Bax, determined by statistical analysis of (D) western blot analysis of Bax. Effects of upregulation of miRNA-46b on the activity of (E) Caspase-3 and (F) Caspase-8, and (G) protein expression of Bax, determined by statistical analysis of the (H) western blot analysis of Bax. ##P<0.01, vs. Control group. Control, negative control group; Anti-146b, microRNA-146b downregulation group; miRNA-146b, microRNA-146b upregulation group. Bax, B-cell lymphoma 2-associated X protein.
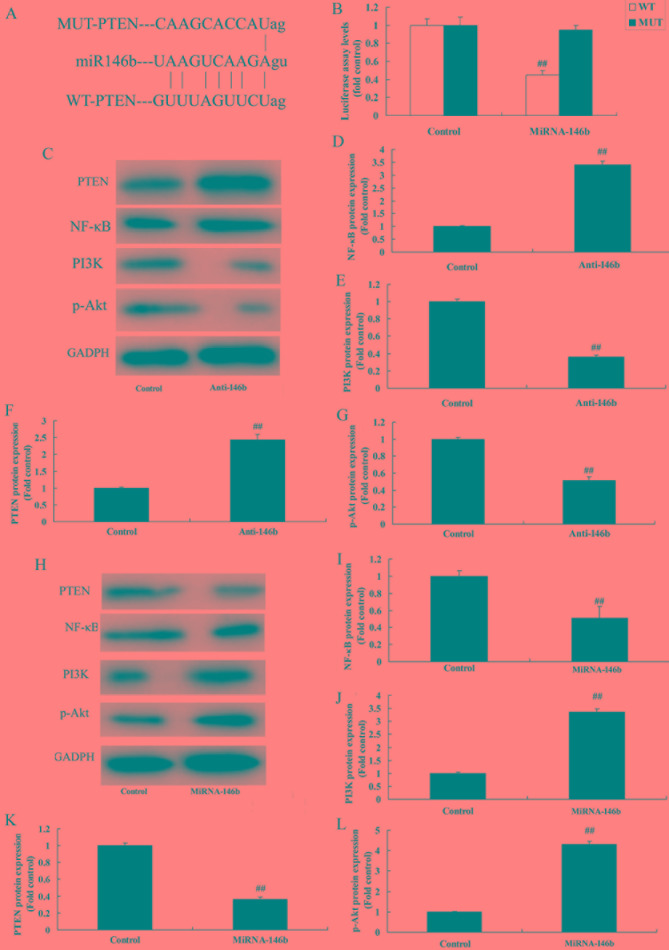
MicroRNA-146b regulates the PI3K/Akt/ NF-κB signaling pathway in vitro by PTEN
To evaluate the mechanism of microRNA-146b in myocardial infarction, the potential binding sites of microRNA-146b on the 3′-UTR of PTEN mRNA were examined (Fig. 5A). Luciferase activity levels were reduced in the group overexpressing microRNA-146b, compared with those in the negative group (Fig. 5B). The downregulation of microRNA-146b significantly induced the protein expression of PTEN and NF-κB, and suppressed the protein expression of PI3K and p-Akt in the in vitro model, compared with the levels in the negative control group (Fig. 5C-G). The upregulation of microRNA-146b significantly suppressed the protein expression of PTEN and NF-κB, and induced the protein expression of PI3K and p-Akt in the in vitro model, compared with the levels in the negative control group (Fig. 5H-L).
Figure 5.
miRNA-146b regulates the PI3K/Akt/NF-κB signaling pathway in an in vitro model by PTEN. (A) miRNA-146b potential binding sites on the 3′-untranslated region of PTEN mRNA. (B) Luciferase activity levels. (C) Western blot analysis of PTEN, PI3K, p-Akt and NF-κB, and statistical analysis of (D) NF-κB, (E) PI3K, (F) PTEN and (G) p-Akt under miRNA-146b downregulation. (H) Western blot analysis of PTEN, PI3K, p-Akt and NF-κB, and statistical analysis of (I) NF-κB, (J) PI3K, (K) PTEN and (L) p-Akt under miRNA-146b upregulation. ##P<0.01, vs. Control group. Control, negative control group; Anti-146b, microRNA-146b downregulation group; miRNA-146b, microRNA-146b upregulation group; PI3K, phosphoinositide 3-kinase; NF-κB, nuclear factor-κB; PTEN, phosphatase and tensin homolog; p-Akt, phosphorylated Akt.
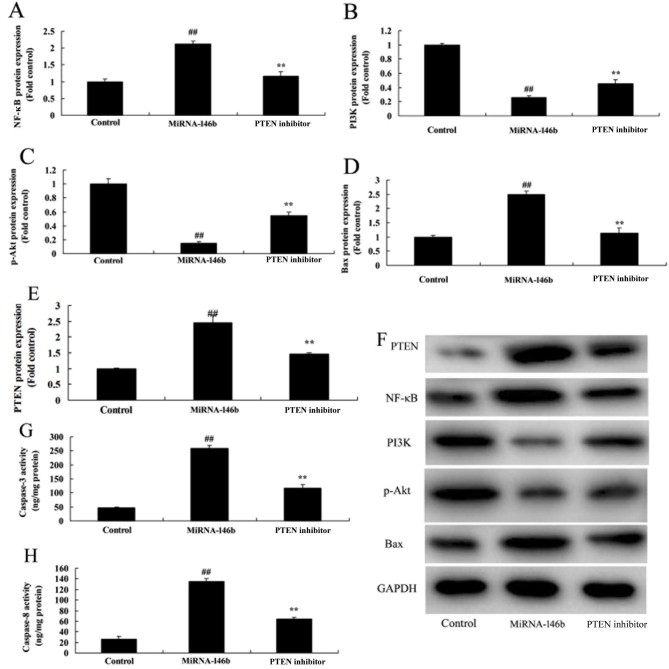
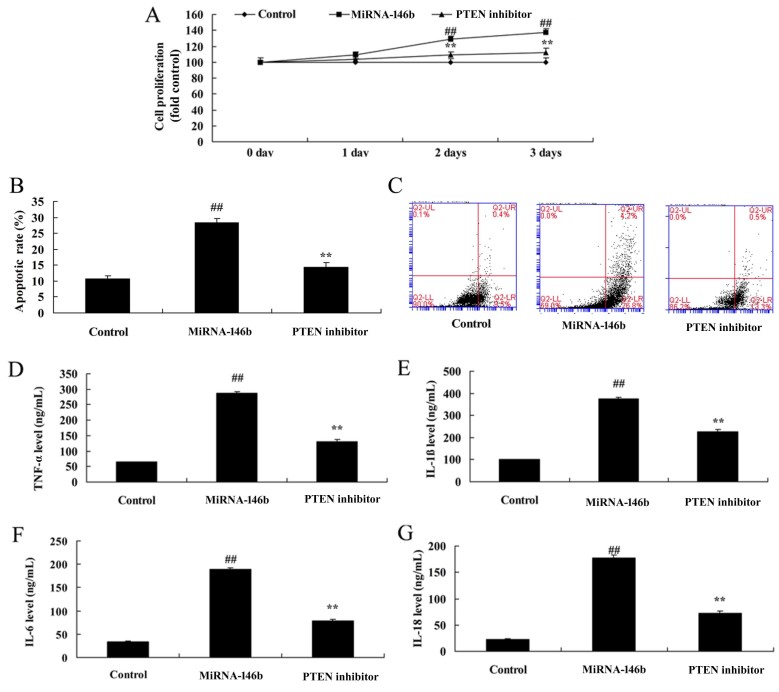
Inhibition of PTEN reduces the effect of microRNA-146b in myocardial infarction
In order to determine whether the PI3K is involved in the effect of microRNA-146b in myocardial infarction, the PTEN inhibitor, VO-Ohpic trihydrate (10 µM), was added to cells following microRNA-146b. As shown in Fig. 6, the PTEN inhibitor induced the protein expression of PI3K and p-Akt, and suppressed the protein expression of PTEN and NF-κB in the in vitro model following microRNA-146b, compared with the microRNA-146b only group. The inhibition of PTEN reduced the effect of microRNA-146b on the promotion of myocardial cell viability, the suppression of apoptosis, and inhibition of the levels of TNF-α, IL-1β, IL-6 and IL-18 in the in vitro model following microRNA-146b, compared with the microRNA-146b only group (Fig. 7A-G).
Figure 6.
Inhibition of PI3K reduces the effect of miRNA-146b on the PI3K/Akt/NF-κB signaling pathway. Statistical analysis of (A) NF-κB, (B) PI3K, (C) p-Akt, (D) Bax and (E) PTEN from the (F) western blot results of PI3K, p-Akt, NF-κB, Bax and PTEN. Activity of (G) Caspase-3 and (H) Caspase-8. ##P<0.01, vs. Control group; **P<0.01, vs. miRNA-146b group. Control, negative control group; miRNA-146b, microRNA-146b upregulation group; PTEN inhibitor, microRNA-146b upregulation and PTEN inhibitor group; PI3K, phosphoinositide 3-kinase; NF-κB, nuclear factor-κB; Bax, B-cell lymphoma 2-associated X protein; PTEN, phosphatase and tensin homolog; p-Akt, phosphorylated Akt.
Figure 7.
Inhibition of PTEN reduces the effect of miRNA-146b in myocardial infarction. (A) Cell viability, (B) vascular apoptotic rate, and (C) vascular apoptosis (determined using flow cytometry) of myocardial infarction. Levels of (D) TNF-α, (E) IL-1β, (F) IL-6 and (G) IL-18 in the in vitro model. ##P<0.01, vs. Control group; **P<0.01, vs. miRNA-146b up-regulation group. Control, negative control group; miRNA-146b, microRNA-146b upregulation group; PTEN inhibitor, miRNA-146b upregulation and PTEN inhibitor group; PI3K, phosphoinositide 3-kinase; TNF-α, tumor necrosis factor-α; IL, interleukin.
Discussion
Myocardial infarction is a common pathological process. It is also the core link in the pathogenesis of myocardial infarction, and in the myocardial revascularization treatment process (18). How the identification of effective myocardial protection measures to reduce myocardial ischemia/reperfusion injury has had remained a focus of interest for investigations (19). Studies have found that implementing a few brief ischemia/reperfusion events in a canine myocardial infarction model at the beginning of the reperfusion cycle can markedly reduce edema and inflammation in regions of post-reperfusion myocardial infarction in myocardial tissue. The concept of ischemic post-conditioning myocardial protection has also been proposed (18). A series of subsequent studies have shown that ischemic post-conditioning offers myocardial protection (5,20). Additionally, it can markedly reduce myocardial infarction in myocardial infarction models in mice, rats, rabbits, dogs and other species (21). In previous years, several studies have found that isoflurane inhalation anesthetic post-conditioning can simulate ischemic post-conditioning, protect against myocardial infarction, and function through a series of mechanisms. The present study showed that the expression of microRNA-146b was downregulated in a myocardial infarction rat model. Hendgen-Cotta et al (16) showed that miR-146b was inhibited in ischemia/reperfusion of acute myocardial injury in vivo.
Previous studies have shown the presence of myocardial cell apoptosis in myocardial infarction (20,22). Adjusting the marker protein of myocardial cell apoptosis can alleviate myocardial cell apoptosis and improve the left ventricular ejection fraction (20). These finding suggests that reducing myocardial cell apoptosis can improve cardiac function in heart failure.
Apoptosis is a form of programmed cell death, which is also an energy consumption process that can be regulated. The Caspase family and Bcl-2, to a certain extent, are important in the regulation of apoptosis (22). The activation of Caspase 3 can cause myocardial cell apoptosis, and the activation of PI3K signaling pathways can inhibit the activation of Caspase-3. Therefore, inhibiting the occurrence of apoptosis and providing a specific inhibitor of Caspase 3 can inhibit apoptosis and reduce cardiac remodeling (11). Lin and An (23), reported that the inhibition of miRNA-146b-5p promoted inflammation by targeting TNF receptor associated factor 6 in atherosclerosis-associated foam cell formation. In the present study, only the H9c2 cell line was used, which is a limitation of the study; another cell line is to be used to verify the results in further investigations.
NF-κB is a key transcription factor mediating the release of inflammatory factors, which is distributed in vascular endothelial cells, vascular smooth muscle cells and myocardial cells, and is involved in the genesis and development of cardiovascular disease (11). Under normal physiological conditions, it binds with the inhibitory protein, IκB, exists in the form of homodimer, and is under an inactive status (24). In the case of stimulation by multiple pathological factors, the bind between NF-κB and IκB breaks. NF-κB and IκB are activated by phosphorylation and transferred to the cell nucleus, bind with specific target genes, regulate target gene transcription, and release relevant inflammatory factors, including IL-6 and TNF-α (25). In this regard, the downregulation of microRNA-146b significantly induced the protein expression of PTEN and NF-κB, and suppressed the protein expression of PI3K and p-Akt in the in vitro model. Jiang et al (26) showed that miRNA-146b ameliorated high-fat diet-induced non-alcoholic fatty liver disease by directly suppressing NF-κB.
The PI3K/AKT signal pathway is an important intracellular signal transduction pathway, which exerts important biological functions in activities including cell apoptosis, survival and proliferation (7). It has been confirmed in experiments in vivo and in vitro that the PI3K/AKT signal transduction pathway is important in protecting from myocardial ischemia reperfusion injury (27) As is indicated in a number of studies, ischemic preconditioning or pharmacological preconditioning can activate the PI3K/AKT signal pathway in myocardial cells. This can induce a series of subsequent reactions, including alleviating cell apoptosis, eliminating intracellular reactive oxygen species, inhibiting activation and aggregation of neutrophils, and protecting mitochondrial functions. Therefore, it is decisive in the protective mechanism of myocardial ischemia reperfusion injury (28). The data in the present study provided support that the downregulation of microRNA-146b significantly suppressed the protein expression of PI3K and p-Akt in the in vitro model. Ramírez-Moya et al (15), showed that microRNA-146b promoted the PI3K/AKT pathway by targeting PTEN in hyperactivation and thyroid cancer progression.
PTEN is the negatively regulatory factor of the PI3K/AKT signaling pathway (14). It is a tumor suppressor factor that downregulates the expression of phosphatidyl triphosphate in multiple systems (14). In addition, it is vital in regulating embryonic development, cell growth, differentiation, apoptosis and migration. PTEN can antagonize the action of PI3K and promote myocardial apoptosis (12). In the present study, it found that the inhibition of PTEN reduced the effect of microRNA-146b on myocardial infarction. Ramirez-Moya et al (15), showed that microRNA-146b promoted PI3K/AKT pathway hyperactivation and thyroid cancer progression by targeting PTEN. The present study is the first, to the best of our knowledge, to report that microRNA-146b regulates the PI3K/AKT pathway to reduce vascular inflammation and apoptosis in myocardial infarction.
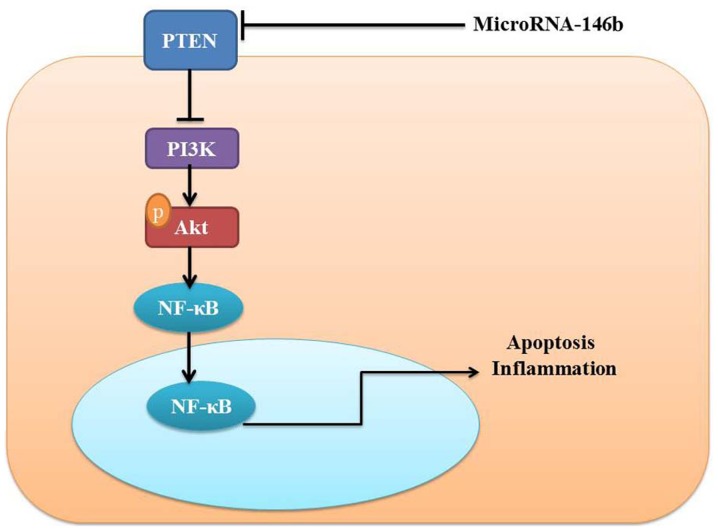
In conclusion, the present study demonstrated that microRNA-146b mediated vascular inflammation and apoptosis in patients with myocardial infarction, which may be associated with activatsion of the PI3K/Akt/NF-κB signaling pathway by PTEN (Fig. 8). Therefore, microRNA-146b may be a promising therapeutic target for the treatment of myocardial infarction, cardiac injury and heart failure.
Figure 8.
MicroRNA-146bb induces the PI3K/Akt/NF-κB signaling pathway to reduce vascular inflammation and apoptosis in myocardial infarction by targeting PTEN. PI3K, phosphoinositide 3-kinase; NF-κB, nuclear factor-κB; PTEN, phosphatase and tensin homolog.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.
Authors' contributions
Not applicable.
Ethics approval and consent to participate
All experimental manipulations were undertaken in accordance with the Guide for the Care and Use of Laboratory Animals by the National Institutes of Health, with the approval of the Animal Experimental Ethics Committee of Jining No. 1 People's Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Lavi S, Alemayehu M, McCarty D, Warrington J, Lavi R. One-year outcome of the sevoflurane in acute myocardial infarction randomized trial. Can J Anaesth. 2015;62:1279–1286. doi: 10.1007/s12630-015-0456-2. [DOI] [PubMed] [Google Scholar]
- 2.Galea N, Francone M, Zaccagna F, Ciolina F, Cannata D, Algeri E, Agati L, Catalano C, Carbone I. Ultra low-dose of gadobenate dimeglumine for late gadolinium enhancement (LGE) imaging in acute myocardial infarction: A feasibility study. Eur J Radiol. 2014;83:2151–2158. doi: 10.1016/j.ejrad.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Xu L, Cai Z, Xiong M, Li Y, Li G, Deng Y, Hau WK, Li S, Huang W, Qiu J. Efficacy of an early home-based cardiac rehabilitation program for patients after acute myocardial infarction: A three-dimensional speckle tracking echocardiography randomized trial. Medicine (Baltimore) 2016;95:e5638. doi: 10.1097/MD.0000000000005638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu M, Mao C, Li J, Han F, Yang P. Effects of the Activin A-Follistatin System on myocardial cell apoptosis through the endoplasmic reticulum stress pathway in heart failure. Int J Mol Sci. 2017;18 doi: 10.3390/ijms18020374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen TL, Zhu GL, He XL, Wang JA, Wang Y, Qi GA. Short-term pretreatment with atorvastatin attenuates left ventricular dysfunction, reduces infarct size and apoptosis in acute myocardial infarction rats. Int J Clin Exp Med. 2014;7:4799–4808. [PMC free article] [PubMed] [Google Scholar]
- 6.Boshra V, Atwa A. Effect of cerebrolysin on oxidative stress-induced apoptosis in an experimental rat model of myocardial ischemia. Physiol Int. 2016;103:310–320. doi: 10.1556/2060.103.2016.3.2. [DOI] [PubMed] [Google Scholar]
- 7.Cheng XY, Gu XY, Gao Q, Zong QF, Li XH, Zhang Y. Effects of dexmedetomidine postconditioning on myocardial ischemia and the role of the PI3K/Akt-dependent signaling pathway in reperfusion injury. Mol Med Rep. 2016;14:797–803. doi: 10.3892/mmr.2016.5345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li CM, Shen SW, Wang T, Zhang XH. Myocardial ischemic post-conditioning attenuates ischemia reperfusion injury via PTEN/Akt signal pathway. Int J Clin Exp Med. 2015;8:15801–15807. [PMC free article] [PubMed] [Google Scholar]
- 9.Lu C, Wang X, Ha T, Hu Y, Liu L, Zhang X, Yu H, Miao J, Kao R, Kalbfleisch J, et al. Attenuation of cardiac dysfunction and remodeling of myocardial infarction by microRNA-130a are mediated by suppression of PTEN and activation of PI3K dependent signaling. J Mol Cell Cardiol. 2015;89:87–97. doi: 10.1016/j.yjmcc.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li H, Song F, Duan LR, Sheng JJ, Xie YH, Yang Q, Chen Y, Dong QQ, Zhang BL, Wang SW. Paeonol and danshensu combination attenuates apoptosis in myocardial infarcted rats by inhibiting oxidative stress: Roles of Nrf2/HO-1 and PI3K/Akt pathway. Sci Rep. 2016;6:23693. doi: 10.1038/srep23693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raish M. Momordica charantia polysaccharides ameliorate oxidative stress, hyperlipidemia, inflammation, and apoptosis during myocardial infarction by inhibiting the NF-kappaB signaling pathway. Int J Biol Macromol. 2017;97:544–551. doi: 10.1016/j.ijbiomac.2017.01.074. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Xing R, Zhang X, Dong W, Zhang J, Yan Z, Li W, Cui J, Lu Y. miR-375 targets the p53 gene to regulate cellular response to ionizing radiation and etoposide in gastric cancer cells. DNA Repair (Amst) 2013;12:741–750. doi: 10.1016/j.dnarep.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Zhuo SM, Li SC, Lin YQ, Yu HB, Li N. The effects of anti-Fas ribozyme on T lymphocyte apoptosis in mice model with chronic obstructive pulmonary disease. Iran J Basic Med Sci. 2017;20:1102–1108. doi: 10.22038/IJBMS.2017.9367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang MJ, Su H, Yan JY, Li N, Song ZY, Wang HJ, Huo LG, Wang F, Ji WS, Qu XJ, Qu MH. Chemopreventive effect of Myricetin, a natural occurring compound, on colonic chronic inflammation and inflammation-driven tumorigenesis in mice. Biomed Pharmacother. 2018;97:1131–1137. doi: 10.1016/j.biopha.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Ramirez-Moya J, Wert-Lamas L, Santisteban P. MicroRNA-146b promotes PI3K/AKT pathway hyperactivation and thyroid cancer progression by targeting PTEN. Oncogene. 2018;37:3369–3383. doi: 10.1038/s41388-017-0088-9. [DOI] [PubMed] [Google Scholar]
- 16.Hendgen-Cotta UB, Messiha D, Esfeld S, Deenen R, Rassaf T, Totzeck M. Inorganic nitrite modulates miRNA signatures in acute myocardial in vivo ischemia/reperfusion. Free Radic Res. 2017;51:91–102. doi: 10.1080/10715762.2017.1282158. [DOI] [PubMed] [Google Scholar]
- 17.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 18.Boghdady A, Elbadry MI. Comparison of successful myocardial reperfusion and adverse events in patients with ST-Elevation myocardial infarction who underwent rescue percutaneous coronary intervention after failed fibrinolytic therapy with vs. without manual coronary thrombus aspiration. Am J Cardiol. 2015;116:1185–1192. doi: 10.1016/j.amjcard.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka S, Masuda T, Kamiya K, Hamazaki N, Akiyama A, Kamada Y, Maekawa E, Noda C, Yamaoka-Tojo M, Ako J. A single session of neuromuscular electrical stimulation enhances vascular endothelial function and peripheral blood circulation in patients with acute myocardial infarction. Int Heart J. 2016;57:676–681. doi: 10.1536/ihj.15-493. [DOI] [PubMed] [Google Scholar]
- 20.Song XJ, Yang CY, Liu B, Wei Q, Korkor MT, Liu JY, Yang P. Atorvastatin inhibits myocardial cell apoptosis in a rat model with post-myocardial infarction heart failure by downregulating ER stress response. Int J Med Sci. 2011;8:564–572. doi: 10.7150/ijms.8.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poss J, Desch S, Eitel C, de Waha S, Thiele H, Eitel I. Left ventricular thrombus formation after ST-segment-elevation myocardial infarction: Insights from a cardiac magnetic resonance multicenter study. Circ Cardiovasc Imaging. 2015;8:e003417. doi: 10.1161/CIRCIMAGING.115.003417. [DOI] [PubMed] [Google Scholar]
- 22.Roubille F, Combes S, Leal-Sanchez J, Barrère C, Cransac F, Sportouch-Dukhan C, Gahide G, Serre I, Kupfer E, Richard S, et al. Myocardial expression of a dominant-negative form of Daxx decreases infarct size and attenuates apoptosis in an in vivo mouse model of ischemia/reperfusion injury. Circulation. 2007;116:2709–2717. doi: 10.1161/CIRCULATIONAHA.107.694844. [DOI] [PubMed] [Google Scholar]
- 23.Lin N, An Y. Blockade of 146b-5p promotes inflammation in atherosclerosis-associated foam cell formation by targeting TRAF6. Exp Ther Med. 2017;14:5087–5092. doi: 10.3892/etm.2017.5121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun Y, Huang J, Song K. BET protein inhibition mitigates acute myocardial infarction damage in rats via the TLR4/TRAF6/NF-kappaB pathway. Exp Ther Med. 2015;10:2319–2324. doi: 10.3892/etm.2015.2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jin JL, Lv RG, Guo J, Liu XH, Liang YW, Wei JR, Wang L. Improvement of left ventricular remodelling by inhibition of NF-kappaB in a rat model of myocardial infarction. Heart Lung Circ. 2016;25:1007–1012. doi: 10.1016/j.hlc.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 26.Jiang W, Liu J, Dai Y, Zhou N, Ji C, Li X. MiR-146b attenuates high-fat diet-induced non-alcoholic steatohepatitis in mice. J Gastroenterol Hepatol. 2015;30:933–943. doi: 10.1111/jgh.12878. [DOI] [PubMed] [Google Scholar]
- 27.Lee TM, Chang NC, Lin SZ. Inhibition of infarction-induced sympathetic innervation with endothelin receptor antagonism via a PI3K/GSK-3beta-dependent pathway. Lab Invest. 2017;97:243–255. doi: 10.1038/labinvest.2016.138. [DOI] [PubMed] [Google Scholar]
- 28.Liu S, Ai Q, Feng K, Li Y, Liu X. The cardioprotective effect of dihydromyricetin prevents ischemia-reperfusion-induced apoptosis in vivo and in vitro via the PI3K/Akt and HIF-1alpha signaling pathways. Apoptosis. 2016;21:1366–1385. doi: 10.1007/s10495-016-1306-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.